Abstract
The coronavirus disease (COVID-19) has become a global public health threaten. A series of strict prevention and control measures were implemented in China, contributing to the improvement of air quality. In this study, we described the trend of air pollutant concentrations and the incidence of COVID-19 during the epidemic and applied generalized additive models (GAMs) to assess the association between short-term exposure to air pollution and daily confirmed cases of COVID-19 in 235 Chinese cities. Disease progression based on both onset and report dates as well as control measures as potential confounding were considered in the analyses. We found that stringent prevention and control measures intending to mitigate the spread of COVID-19, contributed to a significant decline in the concentrations of air pollutants except ozone (O3). Significant positive associations of short-term exposure to air pollutants, including particulate matter with diameters ≤2.5 μm (PM2.5), particulate matter with diameters ≤10 μm (PM10), and nitrogen dioxide (NO2) with daily new confirmed cases were observed during the epidemic. Per interquartile range (IQR) increase in PM2.5 (lag0-15), PM10 (lag0-15), and NO2 (lag0-20) were associated with a 7% [95% confidence interval (CI): (4–9)], 6% [95% CI: (3–8)], and 19% [95% CI: (13–24)] increase in the counts of daily onset cases, respectively. Our results suggest that there is a statistically significant association between ambient air pollution and the spread of COVID-19. Thus, the quarantine measures can not only cut off the transmission of virus, but also retard the spread by improving ambient air quality, which might provide implications for the prevention and control of COVID-19.
Keywords: COVID-19, Air pollution, Quarantine, Time series, Short-term exposure, China
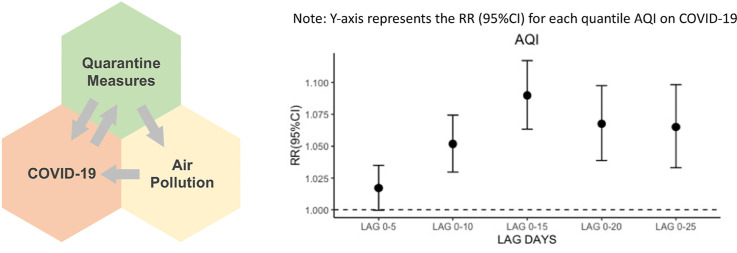
Graphical abstract
Short-term exposure to air pollutants, including PM2.5, PM10, NO2, may contribute to an increase in the counts of daily onset cases. Stringent prevention and control measures can not only cut off the transmission of virus, but also retard the virus spread by reducing air pollution, which might provide implications for the prevention and control of COVID-19.
1. Introduction
At the end of Dec. 2019, a novel coronavirus disease was first detected in Wuhan, Hubei Province, China. The pathogen had been identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the disease was officially named as coronavirus disease 2019 (COVID-19) by World Health Organization (WHO) (Qu et al., 2020). The COVID-19 epidemic in China is the largest outbreak of atypical pneumonia since the severe acute respiratory syndrome (SARS) outbreak in 2003 (Wang et al., 2020a). On Jan. 30th, 2020, WHO declared the COVID-19 outbreak to be an public health emergency of international concern (Mahase, 2020). As of Apr. 6th, 2020, there have been 1,210,956 confirmed cases and 67,594 deaths globally covered at least 215 countries and regions (WHO, 2020).
To retard the rapid spread of COVID-19, the China government have initiated the national public health response to the first level of emergency and implemented a series of strict prevention and control measures, such as self-quarantine, social distancing measures, traffic restrictions, and community containment (Deng and Peng, 2020; Wilder-Smith and Freedman, 2020). On Jan. 23rd, a lockdown was imposed in Wuhan and neighboring cities with travel restrictions, and within days, the quarantine was extended to all provinces in China. All of these interventions led to a reduced number of vehicles on the road and diminished factory production, contributing to the improvement of air quality (Chen et al., 2020; Wang et al., 2020b). Recent studies stated that significant declines of nitrogen dioxide were found during the lockdown in India (Shehzad et al., 2020), and fine particulate matter decreased in the 50 most polluted capital cities worldwide (Rodriguez-Urrego and Rodriguez-Urrego, 2020).
Ambient air pollutant, a mixture of chemicals, including carbon oxides (CO), nitrogen oxides (NOx), ozone (O3), sulfur oxides (SOx), and particular matters (PM), has been proven that can increase the probability of respiratory infections, by prolonging the aerosol transmission of viruses (Chen et al., 2010), or enhancing the ability of viruses to invade airway epithelial cells (Cruz-Sanchez et al., 2013). Exposure to ambient air pollutants may also aggravate respiratory symptoms by inhibiting the expression of key inflammatory mediators (Popovic et al., 2019), as observed in previous studies. Several studies have indicated that the diffusion dynamic of COVID-19 supposed be shaped by socioeconomic and health status, such as living conditions, migration scale and occupation (Bao and Zhang, 2020; Kaiser and Stathopoulos, 2020; Khalatbari-Soltani et al., 2020; Lau et al., 2020), and air pollution seems to play a role in aerosols transmission of SARS-CoV-2. Van Doremalen et al. has shown that SARS-CoV-2 could remain viable in aerosols for several hours, making airborne transmission plausible (van Doremalen et al., 2020). Fattorini and Regoli examined the association between COVID-19 spread and long-term exposure to air pollution, suggesting that chronic exposure to atmospheric contamination may represent a favorable context for the spread of SARS-CoV-2 (Fattorini and Regoli, 2020). Zhu et al. have investigated the association between short-term exposure to air pollutants and Covid-19 infection in 120 cities in China, finding that air pollution can be an important factor in COVID-19 infection (Zhu et al., 2020). Thus, it is reasonable to speculate that ambient air pollutants might affect the transmission of SARS-CoV-2.
A recent study from Heederik et al. (2020) argued that prognosis and confounder of geographical locations were not distinguished in previous studies, and the impact of the COVID-19 pandemic from air pollution can also be affected by the introduction of measures. Thus, the effects of the quarantine measures on the spread of COVID-19 as well as air pollution, the time lag of onset date and report date of new cases (Epidemiology Working Group for NCIP Epidemic Response, 2020), and more lag days of air pollution on COVID-19 infection should be considered in this study.
Although the spread of COVID-19 epidemic has significantly declined in some countries, e.g. China, the number of cases is still increasing rapidly from a global perspective. It is of great significance to clarify the possible influencing factors as air pollutants for COVID-19 epidemic. This study aims to describe the trend of air pollutants and incidence of COVID-19 during the epidemic and explores the association between air pollutants and daily confirmed cases of COVID-19 base on both onset and report dates. In order to assess the effects of air pollution on the transmission of COVID-19, time series data of main ambient air pollutants (PM2.5, PM10, NO2, CO, SO2 and O3) and meteorological variables (temperature, dew point temperature and wind speed) over the study period (Dec. 1st, 2019 to Apr. 6th, 2020), together with daily COVID-19 confirmed cases have been examined through generalized additive models (GAMs). In addition, the study and further assesses the effects of various prevention and control measures on the variation trend of COVID-19 and the association with air pollution in totally 235 cities in China.
2. Materials and methods
2.1. Study area
This study included 235 cities (4 municipalities and 231 prefecture-level cities) in China, dispersing over all provincial administrative regions. According to the National Health Commission, 81,740 COVID-19 confirmed cases have been documented in China as of April 6th, 2020. Our studied cities covered 82.8% of confirmed cases. We focused our analysis on these 235 cities because of the limitation of the air pollution data and meteorological data we have collected. In the descriptive analysis, the mainland China was divided into six geographic regions according to general classification, including central, east, southwest, north, northeast and northwest (Table S2).
2.2. COVID-19 data collection
From Dec. 31st, 2019, the centers of disease controls (CDC) at all levels in mainland China jointly launched the COVID-19 investigation. Data of COVID-19 cases in China were obtained from the reports released by the China National Health Commissions (CNHC, http://www.nhc.gov.cn/) and local health commissions on the official websites, including 31 health commissions of province-level. Daily-confirmed cases, recovered cases and deaths of city-level from Jan. 1st to Apr. 6th, 2020 were collected. Data of Hong Kong, Macao, and Taiwan were not included in this study, because the methods used for data collection were different in these areas.
2.3. Environmental data
The Daily ambient air pollution data for 367 Chinese major cities were collected at China’s National Environmental Monitoring Center from Dec. 1st, 2019 to Apr. 6th, 2020, via Qingyue Open Environmental Data Center, which publishes data of environmental quality. Daily (24-h) average concentrations of air quality index (AQI), carbon monoxide (CO), nitrogen dioxide (NO2), maximum 8-h average ozone (O3), particulate matter with diameters ≤2.5 μm (PM2.5) and particulate matter with diameters ≤10 μm (PM10) were calculated. Besides, we collected the air pollution data of past few years from 2016 to 2020 in 367 major cities of China from the monthly reports of Ministry of Ecology and Environment of the People’ s Republic of China (http://www.mee.gov.cn/, accessed September 30, 2020) and compared the mean ambient air pollutant concentrations of hibernal days (from last Dec. to Apr.) in Fig. S1.
Daily data of meteorological conditions, including mean temperature (°C), dew point temperature (°C) and wind speed (m/s), were also obtained from the National Oceanic and Atmospheric Administration Center (https://www.ncei.noaa.gov). All air pollution and meteorological data were collected from Qingyue Open Environmental Data Center.
2.4. Statistical analysis
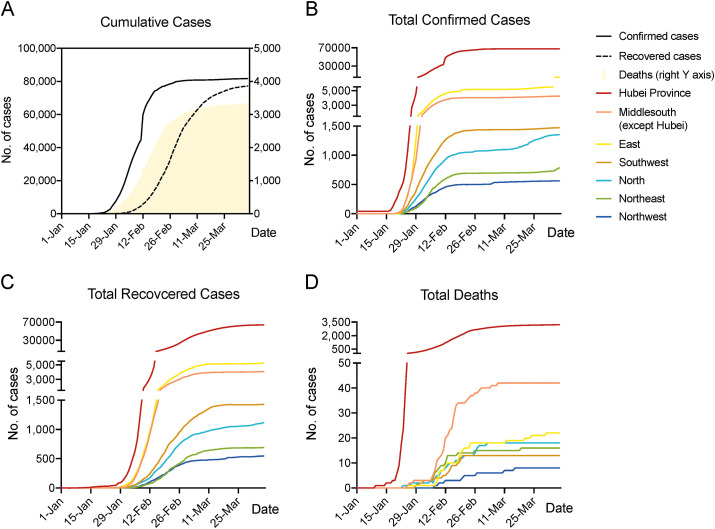
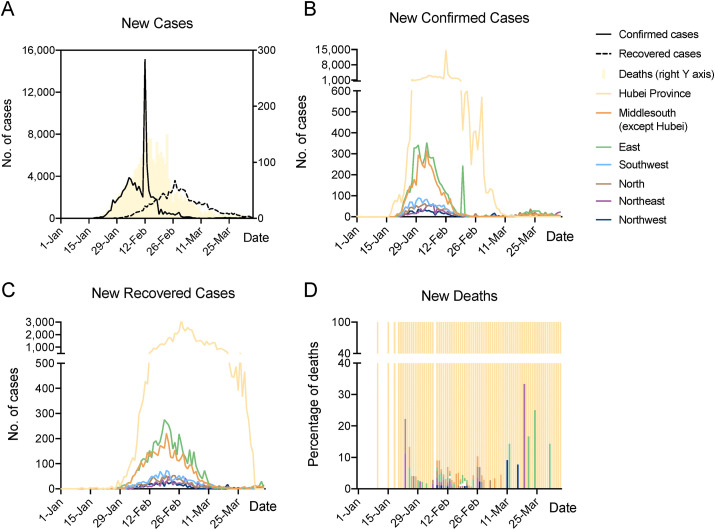
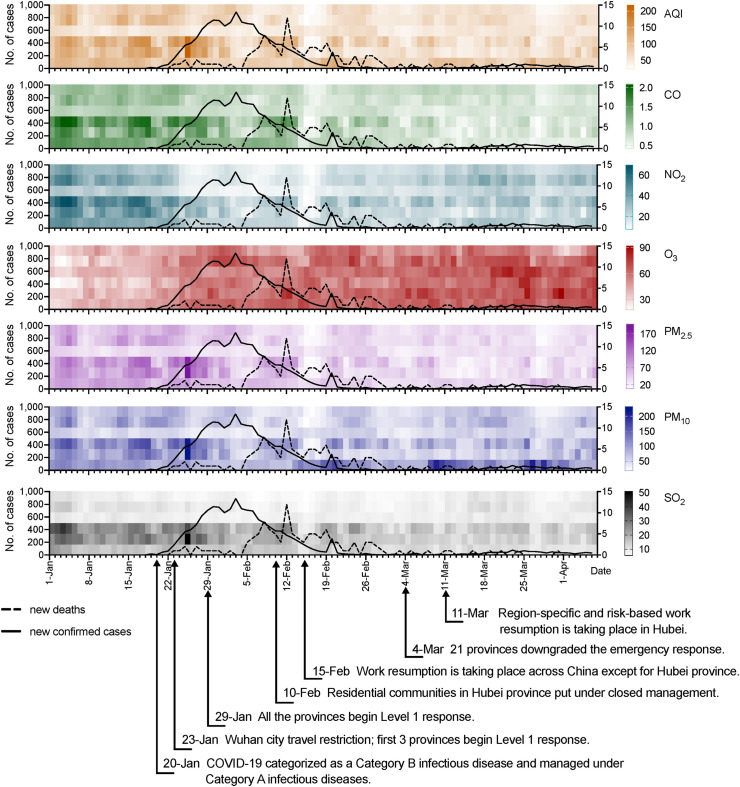
We demonstrated the original cumulative and new cases in the descriptive analysis (Fig. 1 & Fig. 2 ). Changes of daily COVID-19 cases were presented at national level and in 6 geographic regions of mainland China from Jan. 1st to Apr. 6th. Time-series heatmaps (Fig. 3 ) were used to plot AQI and concentrations of six ambient air pollutants in six geographic regions, combined with line-charts of daily confirmed cases and deaths outside Hubei.
Fig. 1.
Daily Changes in cumulative confirmed cases, recovered cases and deaths of COVID-19 nationwide (A), and in different regions (B–D), from Jan.1st to Apr. 6th.
Fig. 2.
Daily Changes in new confirmed cases, recovered cases and deaths of COVID-19 nationwide (A), and in different regions (B–D), from Jan.1st to Apr. 6th.
Fig. 3.
Time series heatmap of air pollutants in different regions, combined with line chart of new confirmed cases and deaths outside Hubei province in China, From Jan. 1st to Apr. 6th. NOTE: X-axle of each heatmap from top to bottom: Central China, East China, North China, Northeast, Northwest, Southwest. Major epidemic response actions taken by the Chinese government are shown in the bottom.
Preliminary data edition was performed in association analysis to ensure that the authentic associations between air pollution and COVID-19 infection were emerged. Firstly, we shift the new confirmed cases to ten days earlier due to the country-level gap between the onset date and report date (Epidemiology Working Group for NCIP Epidemic Response, 2020). Concerning the potential lag effect between air pollution and infection, we calculated several combinations of moving average concentrations of air pollutants (lag0-5, lag0-10, lag0-15, lag0-20, lag0-25).
Specifically, new confirmed cases were calculated using (Nt – Nt-1) from cumulative cases and turned to negative in several days owing to the officially elimination after verifying. Those negative counts were conducted as missing value for the reason that the minus dependent variables were not allowed in Poisson regression. And the counts including clinical diagnosis and nucleotide-acid test in Hubei province between Feb. 12th and Feb.19th were conducted as missing value as well.
For the time-series analyses, Poisson regression models within GAMs were performed which were data-driven method designed to estimate the non-linear relation between explanative factors and dependent variables. Briefly, the model was demonstrated as follows:
| Log [E(Yt,i)] = α + β × pollutanti + s (datet, df1) + log [(Yt-1,i)+ 1] + s (temperaturet,i, df2) + dewpoint temperaturet,i + dowt + lockdownt + cityi |
E(Y t,i ) represented the expected (number + 1) of new confirmed cases count on day t in city i where i referred to different cities and t was the day of the COVID-19 onset and was log-transformed into log[E(Y t,i )] in Poisson regression automatically. α was the intercept. Pollutant i denoted the daily moving average concentration of the compositive AQI and six pollutants (PM2.5, PM10, NO2, CO, SO2, O3) in single-pollutant models; β referred to the coefficients of those pollutants in the models. In addition, several covariates entered the model adjusting for potential confounding: (1) a smoothing spline of calendar date t with 14 degrees of freedom (df1) per year controlled the potential long-term trend effect; (2) log-transformed new confirmed (cases + 1) on t-1 day entered the model controlling the serial correlation of the infectious disease (Liu et al., 2020); (3) meteorological factors were controlled for the possible confounding effect, including a smoothing spline of mean temperature t,i (°C) with 3° freedom (df2) and a linear term of mean dewpoint temperature t,i (°C); (4) day of week t was included as dummy variable to control for the week effect; (5) and lockdown t, effectively retarding the rapid spread of COVID-19, worked as categorical variable adjusting the national lock (since Jan 23rd, 2020) and unlock (until March 15, 2020) effect; (6) city i variable adjusted for the fixed effects such as spatial correlation and population density. S (.) mean the smoothing spline to control for the non-linear relationship. Besides, relative risks (RRs) and 95% confidence intervals (95%CIs) were calculated by the coefficients and standard variances from GAMs models.
Stratified analyses were conducted examining the modification effect by dividing the new cases into Hubei and other six Chinese natural areas (Middle south, East, Northeast, Southwest, Northwest, North).
The elimination of 10-day lag between COVID-19 onset day and report day was performed as sensitivity analyses to test the stability of the effects which was shown in supplementary. Furthermore, we adjusted a smoothing spline of mean wind speed t,i (°C) with 3° freedom in the Poisson model (Fig. S4).
All analyses conducted in R software (version 4.0.0) using mgcv packages. Statistically significance was considered as p < 0.05.
3. Results
In China, there have been 81,740 confirmed cases, 77,167 recovered cases and 3331 deaths of COVID-19 in China from Jan. 1st to Apr.6th (Figs. 1 and 2). Starting from Jan. 21st, the case number presented an explosive increase nationwide. Most cases (67,803 cases, 82.9%) were identified in Hubei Province, which was the hardest hit. Most of new confirmed cases in Hubei Province was found between Jan. 27th to Feb. 18th. Notably, on Feb. 12th, the abnormally higher number of cases due to a change of case definition in Hubei Province, which included clinical diagnosed cases with pneumonia imaging feature other than nucleotide-acid-test validation only. This additional inclusion of diagnostic criteria was only for Hubei Province, and was abolished in the updated version of diagnosis plan on Feb. 20th. Except for Hubei, East China and Central China were the major epidemic area, followed by Southwest China and North China. The peak of the number of new confirmed cases in provinces outside Hubei was from Jan. 29th to Feb. 6th, 2020. As of Apr. 6th, the overall case fatality rate was about 4.1% and 96.4% (3212 cases) of death occurred in Hubei Province. Patients in Hubei had a >5-fold higher case fatality rate at 4.7% compared to patients in other provinces (0.9%). In China, the COVID-19 pandemic was basically contained within about 5 weeks.
Table 1 provides summary statistics on daily AQI, CO, NO2, O3, PM2.5, PM10 concentrations, temperature, dew point temperature and wind speed at an average level in the first quarter of this year. Spearman correlations among AQI, all air pollutants and meteorological variables are shown in Table S1. In 235 urban areas, strong correlations were found for AQI and PM2.5 (Spearman’s correlation coefficient = 0.92), AQI and PM10 (coefficient = 0.96), PM2.5 and PM10 (coefficient = 0.84), reflecting the fact that particular matters were the major air pollutants during the COVID-19 epidemic.
Table 1.
Descriptive statistics of daily air pollutants and meteorological variables in 232 Chinese cities, from Jan. 1st, 2020 to Apr. 6th, 2020.
| Variables | Air pollutants and meteorology |
||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Min | P25 | Median | P75 | Max | |
| AQI | 61.55 | 42.82 | 9.08 | 35.08 | 52.33 | 73.83 | 500.00 |
| Pollutants | |||||||
| CO (mg/m3) | 0.74 | 0.34 | 0.10 | 0.54 | 0.68 | 0.86 | 4.08 |
| NO2 (μg/m3) | 20.77 | 11.86 | 1.46 | 11.79 | 18.33 | 27.17 | 85.32 |
| O3 (μg/m3) | 59.33 | 19.50 | 3.88 | 35.73 | 59.38 | 72.29 | 153.39 |
| PM2.5 (μg/m3) | 38.45 | 34.78 | 1.29 | 18.72 | 30.75 | 47.63 | 1188.58 |
| PM10 (μg/m3) | 64.24 | 78.32 | 3.26 | 31.33 | 50.09 | 77.42 | 2767.83 |
| SO2 (μg/m3) | 10.21 | 6.99 | 1.14 | 5.79 | 8.17 | 12.29 | 94.00 |
| Meteorology | |||||||
| Temperature (°C) | 7.59 | 8.58 | −32.69 | 2.33 | 8.35 | 13.49 | 31.00 |
| Dew point temperature (°C) | −0.27 | 10.85 | −48.75 | −8.65 | 0.79 | 7.87 | 24.05 |
| Wind speed (m/s) | 2.59 | 1.40 | 0.00 | 1.64 | 2.28 | 3.19 | 15.14 |
Note: SD, standard deviation.
To show the joint distribution of daily confirmed and deaths cases and air pollutants, time-series heatmaps and line charts were used to plot the concentrations of air pollutants and new confirmed cases and deaths outside Hubei respectively. A timeline of control measures during the COVID-19 epidemics were added to visualize the contrast of air pollution and cases (Fig. 3). On Jan. 23rd, the travel restriction and some other control measures were declared in Hubei, and a few days later in other province. All the provinces began Level 1 response of public health emergency on Jan. 29th. During the quarantine (From Jan. 23rd to Mar. 11th), most regions witnessed substantial diminution of ambient air pollutants except for O3. The AQI decreased by 12.7%, and five air pollutants (ie. PM2.5, PM10, NO2, SO2 and CO) decreased by 13.4%, 19.4%, 43.1%, 15.9%, 10.8%, respectively. There was an obvious valley point for most regions from Feb. 14th to Feb. 17th. The concentration of air pollutants after quarantine were well below the China national air quality standards (Table S3). Moreover, we compared the ambient air pollution of winter in 367 major Chinese cities from 2016 to 2020 and a decline was shown since 2017 except PM10 and O3 (Fig. S1). However, 8-h average daily maximum concentration of O3 showed a rising trend during the study period, increased by 32.9%. On Feb. 15th, work resumption was taken place nationwide except Hubei, and on Mar. 4th, most provinces downgraded the emergency response to Level 2. Since there was a change of case definition, Hubei Province were not showed here.
Relative risk (RRs) and 95% confidence intervals (95%CIs) of air pollutants (per IQR increase) for COVID-19 new confirmed cases in single-lag models were presented in Fig. S2 The largest effect were found on lag 0–15 for AQI (RR, 1.09; 95%CI, 1.06–1.12), PM2.5 (RR, 1.07; 95%CI, 1.04–1.09), and PM10 (RR, 1.06; 95%CI, 1.03–1.08) respectively and such effects diminished along the time gradually. However, the association of NO2 and COVID-19 infection didn’t reach the top until lag 0–20 (RR 1.19; 95%CI 1.13–1.24), while the effects of rest gaseous pollutants (CO, SO2, O3) remained negative and reach summit on lag 0–25 with RR of 0.82(95%CI: 0.80–0.83), 0.81(95%CI: 0.78–0.85), and 0.82 (95%CI: 0.78–0.85) respectively (Table 2 ). In sensitivity analysis, the association between COVID-19 confirmed cases of report date and air pollution was shown (Fig. S3). Fig. S4 demonstrated the association which was additionally adjusted of wind speed and the result was quite stable.
Table 2.
RRs and 95% CIs of daily COVID-19 confirmed cases associated with per IQR increase in pollutant concentration (AQI, NO2, PM2.5, PM10, CO, SO2, O3) in single-lag models.
| Air Pollutants | Lag Days | RR | 95% CI |
|---|---|---|---|
| AQI | LAG 0-15 | 1.09 | 1.06–1.12 |
| CO | LAG 0-25 | 0.81 | 0.78–0.83 |
| NO2 | LAG 0-20 | 1.19 | 1.14–1.24 |
| O3 | LAG 0-10 | 0.96 | 0.93–1.00 |
| PM2.5 | LAG 0-15 | 1.06 | 1.03–1.08 |
| PM10 | LAG 0-15 | 1.07 | 1.04–1.09 |
| SO2 | LAG 0-25 | 0.82 | 0.78–0.85 |
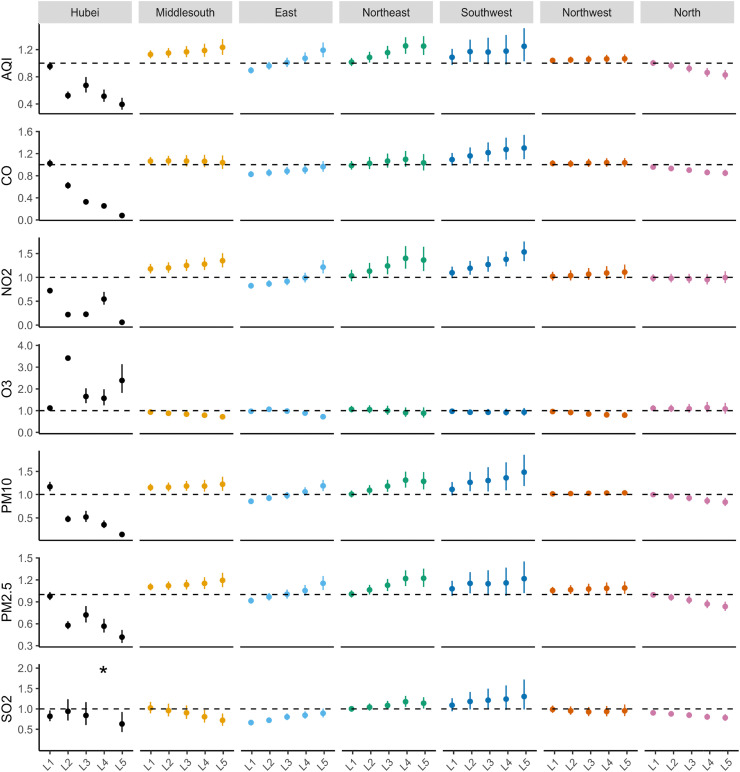
The stratified estimation by seven distinguished areas were showed in Fig. 4. In middle south, southwest and northwest of China, six air pollutants reached the largest effects on lag 0–25 which were not in accordance with the overall lag effects. And the effects of all gaseous pollution except for O3 in northeastern China showed the top on lag 0–20. In the eastern, the effects of PM2.5, PM10 and NO2 went through a transition from negative to positive and that of CO and SO2 remained negative with the decrease of RRs. In the northern, we saw an increase on association between concentrations of PM2.5, PM10, SO2 and CO and COVID-19 new cases resulting in the largest effects on lag 0–25. Besides, the significantly negative effect of O3 went summit on lag 0–25 in middle south, east and northwest part of China. However, no evident trend of air-pollutant effects in Hubei was found.
Fig. 4.
The stratified estimation of seven distinguished areas of RRs and 95% CIs of daily COVID-19 confirmed cases associated with per IQR increase in pollutant concentration (AQI, NO2, PM2.5, PM10, CO, SO2, O3) in single-lag models. Note: the ∗ of SO2 in Hubei Province was 8.43 (95%CI: 5.76–12.34). L1-L5 related to Lag 0–5, Lag 0–10, Lag 0–15, Lag 0–20, Lag 0–25 respectively.
4. Discussion
This multicenter, time-series study demonstrated positive associations of short-term exposure to air pollutants (NO2, PM2.5, PM10) with daily new COVID-19 confirmed cases via GAM, in which the lag from onset date to report date were taken into account. However, the concentrations of CO, SO2, and O3 were negatively associated with increased risk of COVID-19. Furthermore, the stringent prevention and control measures intending to mitigate the spread of COVID-19, contributed to a significant decline in concentration of air pollutants except O3. And the decline of air pollution inversely protected against the transmission and invasion of coronavirus virus. Our stratified analysis showed differed associations in different geographic regions, which could be explained by the interaction effect of air pollution and spread of COVID-19.
Besides, we introduced lag effects between the COVID-19 onset date and report date. The median incubation period of coronavirus was 5.1 days as reported (Lauer et al., 2020) and the confirmation by nucleic acid test would cost several days which impacted the prompt confirmation of COVID-19 new onset cases. The largest lag effects of PM2.5, PM10 and NO2 were postponed to 10 days later and the lag of O3 was considered ten days ahead of the highest effect neglecting the report-date lag. Moreover, the largest association of SO2 and CO would be underestimated. The association of new confirmed of report date and air pollution was shown in sensitivity analysis (Fig. S3).
During the epidemic period, China has imposed a series of multifaceted public health measures to practice social distancing, so as to control the rapid dispersion of the virus. The implementation of stringent quarantines has improved the control of the COVID-19 outbreak in China, reducing the number of incident COVID-19 cases (Pan et al., 2020). Moreover, our results indicated that large quarantine in China contributed to a significant decline in concentration of air pollutants except O3. Starting from Jan. 23rd, the cities gradually entered level 1 of emergency response, carrying out epidemic prevention as well as control measures, including traffic restriction, community containment, personal protection, etc. Compared to the same hibernal period in 2019 (from Dec. 2018 to Apr. 2019), the ambient air pollutants’ concentrations reduced 9.31% for PM2.5, 14.49% for SO2, 11.54% for NO2, and 13.89% for CO respectively. However, the concentrations of the PM10 and O3 enriched 0.57% and 6.90% (http://www.mee.gov.cn/). During the quarantine period, the number of people and vehicles in public places were reduced, most industrial enterprises, construction site, entertainment and catering company were shut down, according to the compulsory measures. As a possible side effect of lockdown, many regions experienced an unprecedented reduction in ambient air pollution. A latest study illustrated that the traffic restriction taken in 44 cities in northern China in COVID-19 pandemic period reduced air pollution emissions significantly, with a 7.80% decrease of AQI (Bao and Zhang, 2020), close to the our results of a 12.7% decrease of AQI. Another study investigated the impact of reduced human activity on air quality over the Yangtze River Delta Region, finding that during the most stringent Level I response period, primary pollutants like SO2, NOx, PM2.5 and VOCs have been reduced by 26%, 47%, 46% and 57% (Li et al., 2020). Besides, due to the stringent lockdown measures, the O3 concentration increased by 32.9%. The increase of O3 attributed to the strong reduction in NOx emissions by transport, which caused a lower titration of O3 (Sicard et al., 2020). Chen et al. compared the changes in PM2.5 and NO2 in 2020 versus 2016–2019 during quarantine period, with those changes in the before quarantine period, suggesting that improved air quality avoided NO2-related and PM2.5-related deaths due to lockdown (Chen et al., 2020).
In the analyses of PM2.5 and PM10, we observed a 7% and 6% increase in COVID-19 morbidity per IQR increase in PM2.5 and PM10 concentration respectively, with a lag of 15 days. Recent studies have also found positive associations of PM2.5 and PM10 with the transmission dynamics of COVID-19 in China (Zhu et al., 2020), Italy (Zoran et al., 2020b) and the USA (Zoran et al., 2020b) by different means. There have been some studies demonstrating close associations between exposure to PMs and respiratory infectious diseases caused by some microorganisms. For instance, exposure to PM2.5 and PM10 have been proved to be associated with increased risk of drug resistant tuberculosis in a two-year study of 752 cases in Jinan, China (Yao et al., 2019), and increased risk of influenza in a six-year study in Taiwan (Chen et al., 2018). Besides, a former study reported significant short-term association between ambient PM levels and increased hospitalization for pneumonia by nationwide time-series study in China (Tian et al., 2019). It has also been verified that air pollutants emitted from vehicles and industries, including NOx and PMs, may affect viral transmission dynamics and increase the risks of hospital admissions due to respiratory virus bronchiolitis and asthma (Glencross et al., 2020; Sarmadi et al., 2020). Although the exact mechanisms for a causal association between PMs and SARS-CoV-2 transmission remains unclear, previous studies found that viruses are more likely to attached to suspended particles, rather than be airborne independently (Chen et al., 2010). Since the enveloped virion of SARS-CoV-2 measures as small as 50–200 nm (Xu et al., 2020b), the PM effect could occur if the virus associates physically with the particles, and the particles might prolong the aerosol transmission of viruses, thus increase the probability of infection. Recent studies revealed that the accelerated transmission dynamics of COVID-19 had a significant association with highly polluted cities, and transmission dynamics of COVID-19 is due to mainly to the mechanism of airborne viral infectivity rather than “human-to-human transmission” (measured with density of population) (Coccia, 2020), which might explain the possible mechanisms for the association.
Our results suggested that exposure to ambient NO2 may contribute to the spread of COVID-19. For per IQR increase in NO2 concentration, about 19% increase in COVID-19 morbidity were observed, with a lag of 20 days. Among all NO2 sources, motor vehicle emission and energy production are the most important. A systematic review confirmed that short-term increases in concentration of NO2, were associated with increases in hospital admissions due to pneumonia (Nhung et al., 2017). NO2 is an irritant of the respiratory system, and it has been verified that increases in viral clinical symptoms related to NO2 may due to the possible NO2 effects on host defenses that prevent the spread of virus (Becker and Soukup, 1999). What’s more, higher levels of ambient NOx were associated with prolonged exacerbations of likely viral etiology, which might increase susceptibility to infection (Pfeffer et al., 2019), supporting toxicological effects of air pollution.
In the analysis of CO, SO2 and O3, protective effects were observed, which lowered the morbidity risk for 18%, 19%, 18% per IQR increase respectively, different from some previous findings (Szyszkowicz et al., 2018; Tao et al., 2014; Zhu et al., 2020). Yet prior studies have given some evidence suggesting a protective role of low-concentration exposure of gaseous pollution on respiratory diseases as well as asthma (Cai et al., 2015; Kim et al., 2020; Tian et al., 2013). In particular, the 24-h concentrations of CO, SO2 and maximum 8-h average O3 were below the China national air pollution standard of 4 mg/m3, 50 μg/m3 and 100 μg/m3, respectively. However, we speculated that confounders especially control measures during pandemic period might still play a major role. Besides, during the outbreak of COVID-19, the new confirmed cases rocketed while the concentrations of air pollutants dived with the strict national lockdown. The authentic association might be overwhelmed by the overspread epidemic situation if the relations were tiny enough due to the statistical defect that multi risk factors could not be explained.
In stratified analyses, Hubei province was separated from other part of nation and demonstrated a respectively violent risk ratio change on several lag days. Fewer cities included and diminishment cases on rise period in model would increase the statistical uncertainty in estimations of the effect. Moreover, the real relation between air pollution and coronavirus infection would be exaggerated and concealed due to the fact that the count of confirmed cases in Hubei was way much higher than other areas which means little change in concentration of air pollutants came along with great fluctuation in new confirmed cases. Thus, it might explain the positive relation between O3 and coronavirus new cases on account of the gentle rise of ozone shown in Fig. 3. What’s more, a significant adverse effects of air pollutants and number of daily confirmed cases were observed in North China. The probable interpretation might be that strict lockdown policies in North China resulted in a sharp decrease of air pollutant concentration, which may affect the supposed effect. The North China is considered as one of the most polluted regions in China and smog events have occurred frequently (Song et al., 2017). It is reasonable to speculate that control measures contributed to a more significant decline in North China compared to other regions. Additional research is needed to determine the biological mechanisms behind this phenomenon. In addition, the effects of CO and SO2 in northeast and southwest of China remained positive while the eastern and northern part of China showed a negative relation between those gaseous pollutants and COVID-19 infection. The discordance resulted in the overall negative association came from differed measures of control and diversity of population density and medical resource in disparate areas.
To date, several studies have examined the association between ambient air pollution and the incidence or mortality of COVID-19 around world, through time-series, regression or correlation test (Table 3 ). Although the studies has some notable differences as compared to our work, sepecially in the statistic model, the results from different countries and regions, including China (Xu et al., 2020a; Zhu et al., 2020), the USA (Bashir et al., 2020; Hendryx and Luo, 2020) and Italy (Fattorini and Regoli, 2020; Ogen, 2020; Zoran et al., 2020a, b), are similar to ours and generally point to positive association between air pollution and risk of COVID-19.
Table 3.
Summary of studies on associations between exposures to air pollution and COVID-19 incidence or mortality in different regions.
| Study | Study location | Time period | Methodology | Statistics | Air pollutants | Estimate |
|---|---|---|---|---|---|---|
| Zhu et al. (2020) | 120 cities in China | Jan. 23 to Feb. 29, 2020 | Time series, Generalized Additive Model (GAM) | Percentage daily confirmed cases change of 10-μg/m3 increase on lag 0-14 | PM2.5 | 2.24% (95% CI: 1.02 to 3.45) |
| PM10 | 1.76% (95% CI: 0.89 to 2.63) | |||||
| NO2 | 6.94% (95% CI: 2.38 to 11.51) | |||||
| O3 | 4.76% (95% CI: 1.99 to 7.52) | |||||
| SO2 | 7.79% (95% CI: −14.57 to −1.01) | |||||
| Xu et al. (2020) | 33 cities in China | Jan. 29 to Feb. 15, 2020 | Time-series Poisson regression model | RR on confirmed cases for each unit on lag 3 | AQI | 1.0008 (95% CI:1.0003, 1.0012) |
| Bashir et al. (2020) | California, USA | Mar. 4 to Apr. 24, 2020 | Spearman rank correlation tests | Correlation coefficient (R) on daily confirmed cases and deaths | PM2.5 | −0.267a; −0.350b |
| PM10 | −0.339a; −0.429b | |||||
| NO2 | −0.485a; −0.731b | |||||
| SO2 | −0.309a; −0.397b | |||||
| Hendryx and Luo (2020) | 3143 counties in the US | Data up to May 31, 2020 | Linear multiple regression | Estimate (SE) on prevalence and death rates | PM2.5 | Prevalence: 23.5 (10.3) ∗ Death rates: 1.08 (0.54) ∗ |
| Fattorini and Regoli (2020) | 71 provinces in Italy | Data up to Apr. 27, 2020 | Pearson correlation | coefficient of determination (R2) | PM2.5 | 0.340∗∗ |
| PM10 | 0.267∗ | |||||
| NO2 | 0.247∗∗ | |||||
| O3 | 0.264∗ | |||||
| Zoran et al. (2020) | Milan, Italy | Jan. 1 to Apr. 25, 2020 | Pearson coefficient correlation | Coefficient (R) on daily new cases | PM2.5 | 0.25 |
| PM10 | 0.35 | |||||
| Zoran et al. (2020) | Milan, Italy | Jan. 1 to Apr. 30, 2020 | Pearson coefficient correlation | Coefficient (R) on daily new cases | NO2 | −0.35∗∗ |
| O3 | 0.50∗∗ | |||||
| Ogen (2020) | 66 regions in European countries (Italy, Spain, France and Germany) | up to Mar. 19, 2020 | Ecological, descriptive analysis | / | NO2 | 83% of all fatalities were associated with NO2 > 100 μmol/m2 |
NOTE: a: on daily confirmed cases; b: on deaths; ∗: p < 0.05; ∗∗: p < 0.01.
Thus, the ambient air pollution would have effect on COVID-19 morbidity and the quarantine measures could decline the concentration of gaseous pollutants inversely. Our multicity time-series analysis provided evidence on positive associations between short-term exposure of air pollutants (AQI, PM2.5, PM10, NO2) and daily new COVID-19 confirmed cases. The negative relations between CO, SO2, O3 and coronavirus require further validation. Besides, we introduced the ten lag days from onset date to report date which helped to reveal the true lag effects for those air pollutants (Heederik et al., 2020). The lag effects of PM2.5, PM10 and NO2 might be postponed to 10 days later while those of O3 might be considered 10 days ahead and the largest association of SO2 and CO would be underestimated if neglecting the report-date lag. The association of new confirmed of report date and air pollution was shown in sensitivity analysis. In addition, the adjustments for lockdown and a range of confounders at the city level were considered.
Our study still has several limitations. First, although 235 cities were covered in our analysis, considering the different control measures the findings cannot be completely interpreted as extent to other countries. Secondly, our study is an ecological study, which relied on aggregate data and did not contain the demographic information. Thus, the problem of ecological fallacy was inevitable. Also, our ecological study just performed statistical associations where the cause-effect relationship was shown restrictedly. Thirdly, in the epidemic prevention, controls such as suspend of public transport and outdoor activity with masks could inflect the airborne transmission of virus.
5. Conclusion
Our study finds that there is a significant decline in the concentrations of air pollutants except O3 during COVID-19 quarantine, and the association between air pollution and the spread of COVID-19 is statistically significant. Short-term exposure to air pollutants, including PM2.5, PM10, NO2, may contribute to an increase in the counts of daily onset cases. Our analysis provides quantitative assessments regarding links between air quality, COVID-19 and the quarantine measures, suggesting that stringent prevention and control measures can not only cut off the transmission of virus, but also retard the virus spread by reducing air pollution, which might provide implications for the prevention and control of COVID-19. This study may serve as a reference to better understand the factors affecting the diffusion and transmission of COVID-19. Furthermore, the findings suggest that ambient air quality should be attached more importance to, as it would reduce the spread of infectious diseases such as COVID-19. Thus, since resumption of work, production and activities has taken place in some regions, the significance of environmental protection should also be paid close attention to. An integrated strategy to prevent future epidemics similar to COVID-19 should be designed not only in medicine and health term, but also in terms of sustainability science and environmental science.
Credit author statement
Xinhan ZHANG: Methodology, Software, Validation, Formal analysis, Investigation, Writing - Original Draft, Visualization. Mengling TANG: Conceptualization, Methodology, Validation, Resources, Writing - Review & Editing, Supervision, Project administration. Fanjia GUO: Methodology, Software, Validation, Formal analysis, Investigation, Writing - Original Draft, Visualization. Fang WEI: Methodology, Resources, Formal analysis. Zhebin YU: Methodology, Resources, Formal analysis. Kai GAO: Investigation, Resources. Mingjuan JIN: Supervision, Project administration. Jianbing WANG: Supervision, Project administration. Kun CHEN: Conceptualization, Supervision, Project administration.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We want to thank all the medical workers for their great contribution and sacrifice during COVID-19 epidemics. Thanks to Qingyue Open Environmental Data Center (https://data.epmap.org) for support on Environmental data processing. This research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors.
Footnotes
This paper has been recommended for acceptance by Dr. Da Chen.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2020.115897.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Bao R., Zhang A. Does lockdown reduce air pollution? Evidence from 44 cities in northern China. Sci. Total Environ. 2020;731:139052. doi: 10.1016/j.scitotenv.2020.139052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B.J., Bilal Komal B., Bashir M.A., Farooq T.H., Iqbal N., Bashir M. Correlation between environmental pollution indicators and COVID-19 pandemic: a brief study in Californian context. Environ. Res. 2020;187:109652. doi: 10.1016/j.envres.2020.109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S., Soukup J.M. Effect of nitrogen dioxide on respiratory viral infection in airway epithelial cells. Environ. Res. 1999;81:159–166. doi: 10.1006/enrs.1999.3963. [DOI] [PubMed] [Google Scholar]
- Cai J., Chen R., Wang W., Xu X., Ha S., Kan H. Does ambient CO have protective effect for COPD patient? Environ. Res. 2015;136:21–26. doi: 10.1016/j.envres.2014.09.039. [DOI] [PubMed] [Google Scholar]
- Chen C.W.S., Hsieh Y.-H., Su H.-C., Wu J.J. Causality test of ambient fine particles and human influenza in Taiwan: age group-specific disparity and geographic heterogeneity. Environ. Int. 2018;111:354–361. doi: 10.1016/j.envint.2017.10.011. [DOI] [PubMed] [Google Scholar]
- Chen K., Wang M., Huang C., Kinney P.L., Anastas P.T. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. The Lancet Planetary Health. 2020 doi: 10.1016/S2542-5196(20)30107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P.-S., Tsai F.T., Lin C.K., Yang C.-Y., Chan C.-C., Young C.-Y., Lee C.-H. Ambient influenza and avian influenza virus during dust storm days and background days. Environ. Health Perspect. 2010;118:1211–1216. doi: 10.1289/ehp.0901782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729:20. doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Sanchez T.M., Haddrell A.E., Hackett T.L., Singhera G.K., Marchant D., Lekivetz R., Meredith A., Horne D., Knight D.A., van Eeden S.F., Bai T.R., Hegele R.G., Dorscheid D.R., Agnes G.R. Formation of a stable mimic of ambient particulate matter containing viable infectious respiratory syncytial virus and its dry-deposition directly onto cell cultures. Anal. Chem. 2013;85:898–906. doi: 10.1021/ac302174y. [DOI] [PubMed] [Google Scholar]
- Deng S.-Q., Peng H.-J. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J. Clin. Med. 2020;9 doi: 10.3390/jcm9020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epidemiology Working Group for NCIP Epidemic Response, C.C.f.D.C.a.P [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China] Chin. J. Epidemiol. 2020;41:145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264:5. doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glencross D.A., Ho T.R., Camilla N., Hawrylowicz C.M., Pfeffer P.E. Air pollution and its effects on the immune system. Free Radic. Biol. Med. 2020;151:56–68. doi: 10.1016/j.freeradbiomed.2020.01.179. [DOI] [PubMed] [Google Scholar]
- Heederik D.J.J., Smit L.A.M., Vermeulen R.C.H. Go slow to go fast: a plea for sustained scientific rigor in air pollution research during the COVID-19 pandemic. Eur. Respir. J. 2020 doi: 10.1183/13993003.01361-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendryx M., Luo J. COVID-19 prevalence and fatality rates in association with air pollution emission concentrations and emission sources. Environ. Pollut. 2020;265:115126. doi: 10.1016/j.envpol.2020.115126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser J.C., Stathopoulos G.T. Socioeconomic correlates of the SARS-CoV 2 and Influenza H1N1 outbreaks. Eur. Respir. J. 2020 doi: 10.1183/13993003.01400-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalatbari-Soltani S., Cumming R.C., Delpierre C., Kelly-Irving M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J. Epidemiol. Community Health. 2020;74:620–623. doi: 10.1136/jech-2020-214297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim A.M., Kang S., Park J.H., Kim Y. Regional variation of hospitalization rates for asthma in Korea: association with ambient carbon monoxide and health care supply. Int. J. Environ. Res. Publ. Health. 2020;17 doi: 10.3390/ijerph17041244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau M.S.Y., Grenfell B., Thomas M., Bryan M., Nelson K., Lopman B. Characterizing superspreading events and age-specific infectiousness of SARS-CoV-2 transmission in Georgia, USA. Proc. Natl. Acad. Sci. U. S. A. 2020 doi: 10.1073/pnas.2011802117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., Azman A.S., Reich N.G., Lessler J. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172:577–582. doi: 10.7326/m20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L., Li Q., Huang L., Wang Q., Zhu A., Xu J., Liu Z., Li H., Shi L., Li R., Azari M., Wang Y., Zhang X., Liu Z., Zhu Y., Zhang K., Xue S., Ooi M.C.G., Zhang D., Chan A. Air quality changes during the COVID-19 lockdown over the Yangtze River Delta Region: an insight into the impact of human activity pattern changes on air pollution variation. Sci. Total Environ. 2020;732:139282. doi: 10.1016/j.scitotenv.2020.139282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Hou X., Ren Z., Lowe R., Wang Y., Li R., Liu X., Sun J., Lu L., Song X., Wu H., Wang J., Yao W., Zhang C., Sang S., Gao Y., Li J., Li J., Xu L., Liu Q. Climate factors and the East Asian summer monsoon may drive large outbreaks of dengue in China. Environ. Res. 2020;183:109190. doi: 10.1016/j.envres.2020.109190. [DOI] [PubMed] [Google Scholar]
- Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- Nhung N.T.T., Amini H., Schindler C., Kutlar Joss M., Dien T.M., Probst-Hensch N., Perez L., Künzli N. Short-term association between ambient air pollution and pneumonia in children: a systematic review and meta-analysis of time-series and case-crossover studies. Environ. Pollut. 2017;230:1000–1008. doi: 10.1016/j.envpol.2017.07.063. [DOI] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO(2)) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q., Huang J., He N., Yu H., Lin X., Wei S., Wu T. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeffer P.E., Donaldson G.C., Mackay A.J., Wedzicha J.A. Increased chronic obstructive pulmonary disease exacerbations of likely viral etiology follow elevated ambient nitrogen oxides. Am. J. Respir. Crit. Care Med. 2019;199:581–591. doi: 10.1164/rccm.201712-2506OC. [DOI] [PubMed] [Google Scholar]
- Popovic I., Soares Magalhaes R.J., Ge E., Marks G.B., Dong G.-H., Wei X., Knibbs L.D. A systematic literature review and critical appraisal of epidemiological studies on outdoor air pollution and tuberculosis outcomes. Environ. Res. 2019;170:33–45. doi: 10.1016/j.envres.2018.12.011. [DOI] [PubMed] [Google Scholar]
- Qu Y., Yang B., Lin S., Bloom M.S., Nie Z., Ou Y., Mai J., Wu Y., Gao X., Dong G., Liu X. Associations of greenness with gestational diabetes mellitus: the guangdong registry of congenital heart disease (GRCHD) study. Environ. Pollut. 2020;266:115127. doi: 10.1016/j.envpol.2020.115127. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Urrego D., Rodriguez-Urrego L. Air quality during the COVID-19: PM2.5 analysis in the 50 most polluted capital cities in the world. Environ. Pollut. 2020;266:115042. doi: 10.1016/j.envpol.2020.115042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmadi M., Marufi N., Kazemi Moghaddam V. Association of COVID-19 global distribution and environmental and demographic factors: an updated three-month study. Environ. Res. 2020;188:109748. doi: 10.1016/j.envres.2020.109748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehzad K., Sarfraz M., Shah S.G.M. The impact of COVID-19 as a necessary evil on air pollution in India during the lockdown. Environ. Pollut. 2020;266:115080. doi: 10.1016/j.envpol.2020.115080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sicard P., De Marco A., Agathokleous E., Feng Z., Xu X., Paoletti E., Rodriguez J.J.D., Calatayud V. Amplified ozone pollution in cities during the COVID-19 lockdown. Sci. Total Environ. 2020;735:139542. doi: 10.1016/j.scitotenv.2020.139542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song C., Wu L., Xie Y., He J., Chen X., Wang T., Lin Y., Jin T., Wang A., Liu Y., Dai Q., Liu B., Wang Y.-N., Mao H. Air pollution in China: status and spatiotemporal variations. Environ. Pollut. 2017;227:334–347. doi: 10.1016/j.envpol.2017.04.075. [DOI] [PubMed] [Google Scholar]
- Szyszkowicz M., Kousha T., Castner J., Dales R. Air pollution and emergency department visits for respiratory diseases: a multi-city case crossover study. Environ. Res. 2018;163:263–269. doi: 10.1016/j.envres.2018.01.043. [DOI] [PubMed] [Google Scholar]
- Tao Y., Mi S., Zhou S., Wang S., Xie X. Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ. Pollut. 2014;185:196–201. doi: 10.1016/j.envpol.2013.10.035. [DOI] [PubMed] [Google Scholar]
- Tian L., Qiu H., Pun V.C., Lin H., Ge E., Chan J.C., Louie P.K., Ho K.F., Yu I.T. Ambient carbon monoxide associated with reduced risk of hospital admissions for respiratory tract infections. Am. J. Respir. Crit. Care Med. 2013;188:1240–1245. doi: 10.1164/rccm.201304-0676OC. [DOI] [PubMed] [Google Scholar]
- Tian Y., Liu H., Wu Y., Si Y., Li M., Wu Y., Wang X., Wang M., Chen L., Wei C., Wu T., Gao P., Hu Y. Ambient particulate matter pollution and adult hospital admissions for pneumonia in urban China: a national time series analysis for 2014 through 2017. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1003010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet (London, England) 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Yuan Y., Wang Q., Liu C., Zhi Q., Cao J. Changes in air quality related to the control of coronavirus in China: implications for traffic and industrial emissions. Sci. Total Environ. 2020;731:139133. doi: 10.1016/j.scitotenv.2020.139133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . WHO; 2020. Coronavirus Disease (COVID-2019) Situation Reports. [Google Scholar]
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Trav. Med. 2020;27 doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Yan C., Fu Q., Xiao K., Yu Y., Han D., Wang W., Cheng J. Possible environmental effects on the spread of COVID-19 in China. Sci. Total Environ. 2020;731:139211. doi: 10.1016/j.scitotenv.2020.139211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Chen P., Wang J., Feng J., Zhou H., Li X., Zhong W., Hao P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020;63:457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao L., LiangLiang C., JinYue L., WanMei S., Lili S., YiFan L., HuaiChen L. Ambient air pollution exposures and risk of drug-resistant tuberculosis. Environ. Int. 2019;124:161–169. doi: 10.1016/j.envint.2019.01.013. [DOI] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between ground levels of ozone (O(3)) and nitrogen dioxide (NO(2)) with coronavirus (COVID-19) in Milan, Italy. Sci. Total Environ. 2020;740:140005. doi: 10.1016/j.scitotenv.2020.140005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020;738:12. doi: 10.1016/j.scitotenv.2020.139825. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.