Abstract
Objective
Mobile health platforms have become an important component of pain self-management programs and hundreds of mobile applications are commercially available for patients to monitor pain. However, few of these applications have been developed in collaboration with healthcare professionals or have been critically evaluated. Manage My Pain is a user-driven mobile health platform developed by ManagingLife in collaboration with clinician researchers. Manage My Pain allows patients to keep a “pain record” and supports communication of this information with clinicians. The current report describes a user engagement study of Manage My Pain among patients at the Transitional Pain Service (TPS) at Toronto General Hospital, a multidisciplinary clinic for patients at high risk of developing postsurgical pain.
Methods
Patients at the TPS were encouraged to register on Manage My Pain as one component of a larger, non-randomized prospective study of treatment predictors and treatment enhancement. Uptake of the application and rates of registration, use, and retention were tracked for 90 days.
Results
Of the 196 patients who consented to the larger study, 132 (67%) also provided consent to the Manage My Pain component, indicating that they found this to be an acceptable treatment adjunct, and 119 (61%) completed registration. Of those who used the app, 67.9% and 43.2% continued to use Manage My Pain beyond 30 and 90 days, respectively. On average, users engaged with the app for 93.14 days (SD = 151.9 days) logged an average of 47.39 total records (SD = 136.1).
Conclusions
Manage My Pain was found acceptable by a majority of patients at an academic pain management program. Rates of user registration and retention were favorable compared to those reported by other applications. Further research is needed to develop strategies to retain users and maximize patient benefit.
Keywords: Pain, mHealth, apps
Introduction
Self-management approaches are a mainstay of chronic pain programs and critical to long-term success.1 Over the past decade, mobile health platforms have become a frequent component of pain self-management.2 Generally, these applications are developed as an independent adjunct to medical treatment, designed to augment self-management practices such as tracking of pain intensity levels and communication with medical professionals.3 Use of such applications is increasingly called for to reduce the treatment gap, improve access to pain management, and support the efficacy of self-management interventions.4,5
This has led to a notable divide between commercially available apps that are easily accessible but have been developed without patient or provider input, and those developed in academic research settings which have been subjected to rigorous research but are not publicly available. Thousands of health management applications are currently available to the public through smartphone application stores.2,3 Notwithstanding their ubiquity, there are major limitations with these commercially-available applications, including lack of input from users (people with pain), researchers, or health care providers as well as lack of publicly-available research on app engagement or clinical outcomes associated with application use.3,6 In contrast, a recent meta-analysis of academically-driven apps supported the ability of these apps to reduce pain intensity and improve quality of life.2 However, none of the apps featured in the meta-analysis were commercially available and only one described plans for commercial development.7 This dichotomy highlights the need to identify applications that are both readily available to patients and developed with input from users, healthcare personnel, and researchers knowledgeable about pain.8
Manage My Pain (MMP) is a user-driven mobile health platform developed by ManagingLife.9–11 MMP was first developed as an independent, commercially-available application designed to allow users to track their pain on a daily basis and provide reports to facilitate communication of this information to healthcare providers. After over 100 iterations of the application, incorporating user beta-testing as well as user feedback and reviews, in 2016, ManagingLife partnered with the Transitional Pain Service (TPS) at the Toronto General Hospital, a multidisciplinary clinic dedicated to identification and treatment of individuals at risk of developing chronic pain after major surgery.12 This partnership facilitated further development and refinement of the application through creation of a scientific advisory committee consisting of clinical researchers with expertise in pain and focus group discussions with health care providers.9 After research ethics board approval and institutional approval regarding privacy issues, patients at the TPS were encouraged to use Manage My Pain throughout treatment as an adjunct to self-management and to aid with clinical decision making.
The current manuscript describes patient engagement during a pilot study examining the use of MMP in conjunction with clinical care at the TPS. At their initial visit to the TPS, patients were encouraged to sign up for the application at clinic intake and to use MMP throughout treatment. The aims of the current study were to evaluate the rate of uptake of the application in the TPS and to describe patterns of activity among MMP users.
Materials and methods
Participants
Data were collected on 196 consecutive patients who consented to participate in a prospective study of treatment predictors and MMP for treatment enhancement in the TPS. The study was approved by the research ethics board at the University Health Network (REB # 16-5109-AE). Participants were patients who had been referred to the TPS for management of postsurgical pain and complex chronic pain. Patients are referred to the TPS through one of the following care pathways: 1) prior to surgery due to risk factors for postsurgical pain and opioid use; 2) by the Acute Pain Service after surgery; 3) by surgeons or primary care physicians due to persistent postsurgical pain and complex chronic pain. Participants were recruited into the current study at their first encounter with TPS staff. Eligibility criteria included having a pain condition requiring management in the TPS and sufficient English fluency to engage with the app. The majority of participants identified as female (53.4%) and the average age was 47.6 (SD = 13.3). Data collection occurred between February 2017 and August 2019.
Procedure
The current report details one aim of a larger, non-randomized, prospective study of treatment predictors and use of MMP for treatment enhancement in the TPS. Interested individuals were able to consent separately to each aim of the study, which included use of MMP, blood draws, and permission to link patient data with large, independent patient registries. Patients who consented to use MMP were provided with instructions on how to install and set-up the app and, when possible, were guided through this process by the research coordinator. Patients were also provided with a unique identifier within the application so that internal app records could be matched with participant IDs within the larger study. Patients were then encouraged to use the app during the course of standard treatment. All patient activity prior to each clinic visit, participant summaries from MMP covering the time since previous visit were shared with medical providers. Patient records from MMP were downloaded at the conclusion of the study and matched to demographic information (e.g. Age, Gender), collected as part of the larger study. All participants who used MMP agreed to share the data entered into the app with the clinical and research team. However, uptake of medical providers viewing this data via the monitoring portal features was not tracked in a systematic fashion.
Manage My Pain
MMP is a user-driven mobile health application designed by ManagingLife. There are three central features of MMP. The first is a “pain record” that asks users to complete a single pain intensity numerical rating scale (from 0, no pain, to 10, worst ever), presented on a slider, with the option of answering 8 additional questions regarding pain characteristics (Figure 1(a)). These questions are designed to take less than 60 seconds to complete and capture pain locations, associated symptoms, character of the pain, aggravating factors, ineffective treatments, alleviating factors, pain timing, and environmental factors. A second feature of the app is a “daily reflection record” that asks users “what did you do today that mattered to you?” and rate on a scale from 0, nothing, to 10, everything I wanted, the extent to which users engaged in meaningful activities that day, with the option to specify meaningful activities (Figure 1(b)). An important feature of MMP is the ability of users to share their app data via a randomized user ID with the clinical and research team, who can then access a summary of a patient’s ratings and activities (Figure 2).9 In the context of the current study, research staff accessed participant’s MMP summary and shared this with medical providers prior to visits.
Figure 1.
(a) Image of the pain record screen from Manage My Pain. (b) Image of the daily reflection record from Manage My Pain.
Figure 2.
Manage My Pain clinician report summary page.
Data analysis
Descriptive statistics were used to evaluate uptake of the application and user retention. Uptake was defined as the proportion of participants who consented to the MMP portion of the larger study. User retention was defined as the proportion of users who were still actively logging records in the app at 1 day, 7 days, 14 days, 30 days, and 90 days Users were defined as individuals who became active within the app (i.e. logged at least one record). Non-parametric correlations were used to examine bivariate relationships between duration of use and the number of records completed in the app.
Results
Uptake and registration
Figure 3 describes patient recruitment into the study, uptake of the application, and registration on the app. 382 consecutive patients were screened for the study. Of these, 196 provided consent to participate in any component of the larger study and 132 found MMP acceptable and consented to participate in the app component of the study. Of the 132 participants who consented to the MMP portion of the study, 119 successfully registered an account within the app. Of the 119 participants who registered for MMP, 81 (68%) became active users reflected by having completed at least one record (either pain record or daily reflection), reflecting that the app had been downloaded and used.
Figure 3.

Flow diagram of participants who became MMP users.
Duration and type of MMP use
Figure 4 depicts the proportion of participant users (i.e. those who downloaded and completed at least one record on the app) who continued to use the app after 1 day, 7 days, 14 days, 30 days, and 90 days. Overall, 35 participants (43.2% of users) were still using the app after 90 days. The periods of greatest attrition occurred at on-boarding, prior to any use (30 participants, 27%), between 1 day and 7 days (10 participants, 9%), and between 30 days and 90 days (20 participants, 18%) after registration. The median duration of activity was 56.5 days (IQR = 13.5 – 176).
Figure 4.
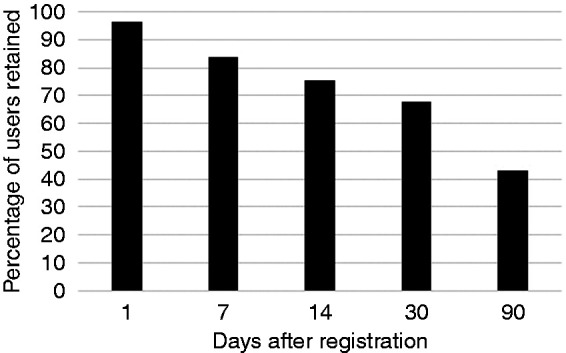
Percentage of users retained over the first 90 days after registration with MMP.
As described above, the app prompts participants to complete a pain record and daily reflection record every day. Combined, participants logged a median of 8 total records (IQR = 3–41.25). The median number of pain records completed was was 7 (IQR = 2.75–33.5) and the median number of daily reflections was 2 (IQR = 0–9). The number of days of app use was positively correlated with total number of records (Spearman’s ρ = 0.86, p < 0.001), number of pain records (Spearman’s ρ = 0.85, p < 0.001), and number of daily reflection records (Spearman’s ρ = 0.75, p < 0.001).
Discussion
The current report details the usage of Manage My Pain (MMP), a user-driven mobile health pain self-management application, amongst patients at the Transitional Pain Service (TPS), an academic pain treatment program designed to treat individuals at high risk for the development of chronic postsurgical pain and/or prolonged opioid use. Of the participants who agreed to participate in the larger study, 67% found the app to be an acceptable addition to treatment and 61% proceeded to register for the application. More than half of those who registered for MMP continued to use the app for at least 30 days.
The rates of user retention described in the current report are similar to those reported in other studies of health applications. In general, there is both low uptake and high rates of attrition for all applications, regardless of focus (e.g., media, retail, lifestyle, etc.). Indeed, recent industry reports indicate that it is not unusual for more than 70% of app users to disengage within 90 days,13 and that this rate may be as high as 85% for health related apps.14 In that respect, rates of disengagement from MMP are lower than the larger population of app users. In empirical reports, rates of user retention after 90 days for mobile health applications range greatly, from as low as 10% of users retained, to over 90% retention.15,16 Thus, in comparison to other health applications, MMP has generally favorable uptake and attrition rates.
There are several factors specific to the TPS that could be barriers to user retention with MMP. The TPS is a tertiary care, academic medical clinic located in a large urban center that serves a large catchment area and diverse patient population. Physical or socioeconomic barriers may have limited patient ability to engage with MMP. Furthermore, the fast-paced clinical environment of the TPS and the Toronto General Hospital may have limited time available to fully instruct the patient on the app or provide education as to the benefits of MMP.
Future research should examine strategies to enhance patient motivation to use MMP or other mobile health applications. Recent reviews have highlighted the need to align mobile health applications with formal theories of motivation and health behavior change.4,15,17 For instance, the addition of motivational enhancement components to a mobile health application has recently been linked to improved engagement.18 Although further study of engagement moderators is needed to identify promising intervention targets, the inclusion of educational materials focused on promoting self-management or interventional components to enhance perceived app utility may bolster engagement. Such strategies could be facilitated either by clinical staff or through application development. Moreover, these issues might benefit from targeted intervention delivered soon after registration. In the current study the largest drop off was between registration and 7 days post-registration. Educational or motivational materials that are included in the registration process or delivered shortly after registration may efficiently reduce attrition.
It is clear that times are changing. Digital information collection and management have the potential to reduce the treatment gap and optimize and transform healthcare.5 Patients are more and more ready to engage with mobile technology and web-based interfaces as part of their healthcare utilization. However, hospitals are large and complex organizations, and personal health information is very sensitive – so in this context, the shift to digital information management is challenging and slow. Barriers to integration of digital solutions into health care will need to be addressed at the institutional level. In addition, a key question that will need to be addressed is whether this new digital health architecture works best when patients or medical providers are custodians of patients’ personal health information. The advantages of settling these questions and finding ways to integrate hospital care and mobile/web based technologies are clear. For example, patients who live in remote areas, in particular, may benefit from the increased visibility afforded by data that can be collected between hospital visits. For this approach to be successfully implemented, health care providers must also be ready to embrace change; educating patients on the benefits of mobile health solutions, and reviewing remote data that is collected between visits. In summary, while digital innovations such as MMP have great potential, there are major issues to be addressed at the institutional, health provider, and patient level in order to make the leap to the digital future of health care.
Conclusion
In summary, MMP was an acceptable treatment adjunct for the majority of patients in the TPS and rates of user retention at 30 and 90 days were as favorable as those reported by other mobile health applications. Further research is needed on strategies to retain users and motivate app engagement. Manage My Pain, developed through collaboration among industry, academia, and healthcare providers, is a promising pain self-management application that is both acceptable and easily available to patients and positioned to undergo rigorous scientific evaluation.
Acknowledgements
We would like to thank research staff in the Toronto General Hospital Department of Anesthesia and Pain Management for their support on this project.
Contributorship
TJ, AW, JK, and HC conceived and designed this study. MP, SK, and ST provided administrative support on the study. YK, VM, AMB, JF, RK, DT, KM, MK, AH, SK, ST, and HC provided study materials and participants for the study. PS, MP, SK, and ST were involved in assembly of data. PS, MP, TJ, SK, ST, AW, JK, and JC were involved in data analysis and interpretation. PS wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and provided approval for the final version of the manuscript.
Declaration of conflicting interests
JK is supported by a Canadian Institutes of Health Research Canada Research Chair in Health Psychology at York University. TJ is the founder and CEO of ManagingLife, Inc. JK and HC are unpaid members of the ManagingLife Advisory Board, providing guidance on the product and the company’s research initiatives.
Ethical approval
The research ethics board at the University Health Network approved this study (REB # 16-5109-AE).
Funding
This work was supported by the Ontario Centres of Excellence Advancing Health Grant awarded to TJ, JK, and HC.
Guarantor
HC.
Peer review
This manuscript was reviewed by reviewers who have chosen to remain anonymous.
ORCID iDs
P Maxwell Slepian https://orcid.org/0000-0003-0435-4191
Hance Clarke https://orcid.org/0000-0003-4975-3823
References
- 1.Hooten WM, Timming R, Belgrade M, et al. Assessment and management of chronic pain. Report, Institute for Clinical Systems Improvement, USA, November 2013. [Google Scholar]
- 2.Thurnheer SE, Gravestock I, Pichierri G, et al. Benefits of mobile apps in pain management: systematic review. JMIR mHealth uHealth 2018; 6: e11231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lalloo C, Shah U, Birnie KA, et al. Commercially available smartphone apps to support postoperative pain self-management: scoping review. JMIR mHealth uHealth 2017; 5: e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ankawi B, Kerns RD, Edmond SN. Enhancing motivation for change in the management of chronic painful conditions: a review of recent literature. Curr Pain Headache Rep 2019; 23: 75. [DOI] [PubMed] [Google Scholar]
- 5.Kazdin AE. Addressing the treatment gap: a key challenge for extending evidence-based psychosocial interventions. Behav Res Ther 2017; 88: 7–18. [DOI] [PubMed] [Google Scholar]
- 6.de la Vega R, Miró J. mHealth: a strategic field without a solid scientific soul. A systematic review of pain-related apps. PLoS One 2014; 9: e101312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Irvine AB, Russell H, Manocchia M, et al. Mobile-Web app to self-manage low back pain: randomized controlled trial. J Med Internet Res 2015; 17: e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao P, Yoo I, Lancey R, et al. Mobile applications for pain management: an app analysis for clinical usage. BMC Med Inform Decis Mak 2019; 19: 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weinrib A, Azam MA, Latman VV, et al. Manage My Pain: a patient-driven mobile platform to prevent and manage chronic postsurgical pain. In: Morr CE (ed) Novel applications of virtual communities in healthcare settings Hershey, PA: IGI Global, 2018, pp.93–126.
- 10.Rahman QA, Janmohamed T, Pirbaglou M, et al. Defining and predicting pain volatility in users of the Manage My Pain app: analysis using data mining and machine learning methods. J Med Internet Res 2018; 20: e12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahman QA, Janmohamed T, Pirbaglou M, et al. Patterns of user engagement with the mobile app, Manage My Pain: results of a data mining investigation. JMIR mHealth uHealth 2017; 5: e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz J, Weinrib A, Fashler SR, et al. The Toronto general hospital transitional pain service: development and implementation of a multidisciplinary program to prevent chronic postsurgical pain. J Pain Res 2015; 8: 695–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perro J. Mobile apps: what’s a good retention rate? Localytics 2018; https://info.localytics.com/blog/mobile-apps-whats-a-good-retention-rate (2018, accessed 14 September 2020).
- 14.Adjust Inc. Global App Trends 2019: Global Benchmarks Report. Report, Adjust Inc., Berlin, DE, 2019.
- 15.Druce KL, Dixon WG, McBeth J. Maximizing engagement in mobile health studies: lessons learned and future directions. Rheum Dis Clin North Am 2019; 45: 159–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crouthamel M, Quattrocchi E, Watts S, et al. Using a ResearchKit smartphone app to collect rheumatoid arthritis symptoms from real-world participants: feasibility study. JMIR mHealth uHealth 2018; 6: e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohr DC, Siddique J, Ho J, et al. Interest in behavioral and psychological treatments delivered face-to-face, by telephone, and by internet. Ann Behav Med 2010; 40: 89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shrier LA, Burke PJ, Kells M, et al. Pilot randomized trial of MOMENT, a motivational counseling-plus-ecological momentary intervention to reduce marijuana use in youth. Mhealth 2018; 4: 29–29. [DOI] [PMC free article] [PubMed] [Google Scholar]




