Abstract
Introduction:
Mobile health is an emerging technology around the world that can be effective in cancer screening. This study aimed to examine the effectiveness of mobile health applications on cancer screening.
Methods:
We conducted a systematic literature review of studies related to the use of mobile health applications in cancer screening. We also conducted a comprehensive search of articles on cancer screening related to the use of mobile health applications in journals published between January 1, 2008, and January 31, 2019, using 5 databases: IEEE, Scopus, Web of Science, Science Direct and PubMed.
Results:
A total of 23 articles met the inclusion criteria and were included in the present review. All studies have identified positive effects of applications on cancer screening and clinical health outcomes. Furthermore, more than half of mobile applications had multiple functions such as providing information, planning and education. Moreover, most of the studies, which examined the satisfaction of patients and quality improvement, showed healthcare application users have significantly higher satisfaction of living and it leads to improving quality.
Conclusion:
This study found that the use of mobile health applications has a positive impact on health-related behaviours and outcomes. Application users were more satisfied with applying mobile health applications to manage their health condition in comparison with users who received conventional care.
Keywords: Early detection, neoplasms, mobile applications, telemedicine
Introduction
Mobile health (mHealth) has been developed as a component of electronic health (eHealth). mHealth involves the use of mobile communication technologies to promote health by supporting healthy practices (eg, delivery of healthcare information, health data collection or patient observation and provision of care).1 Furthermore, mHealth can improve continuous health monitoring of both populations and individuals. mHealth has the potential to improve health outcome, support chronic disease self-management, reduce cost, enhance efficiency and decrease the number of patient visits to healthcare facilities, and provide on-demand, localized and personalized interventions.2
In this age of advanced technologies and digital devices, physicians increasingly use electronic devices for patient care, clinical guidelines and education. Mobile applications (apps) are new tools that can be downloaded onto mobile devices such as tablet computers and smartphones. Many of them are targeted at medical providers. These apps may lead to enhanced patient care, increase efficiency or provide individualized learning for clinicians.3
mHealth enables the timely data collection, transmission, storage as well as data analyses, sharing and reporting.1 Besides, mHealth applications contribute to improving healthcare through monitoring, diagnoses and treatment.4 The advent of smartphone technologies that empower quick and easy access, transfer and tracking of data and information, as well as sharing, interactive displays and interventions that can be highly engaging, has promoted adoption. Furthermore, mHealth has increased accessibility to healthcare provider and services, improved quality of healthcare and reduced cost of healthcare.5
Cancer screening programmes aim to detect cancer precursors or cancers at an early stage before symptoms appear. Early detection is beneficial when cancer incidence or cancer death is prevented. Screening may be a system of checking for the presence or absence of disease. Cancer screening is effective in reducing cancer incidence and mortality.4,6 Health organizations recommend screening for cancers such as cervical cancer and breast cancer, and their recommendations have been adopted in many countries. Despite their success, population-based cancer screening programmes face the challenge of overcoming geographical barriers for rural and low-income healthcare centre which are often less likely to be reached by preventive healthcare services than urban healthcare centre.7 The number of cancer survivors continues to increase based on the growth and ageing of the population and improvements in early detection and treatment. mHealth technologies play an important role in helping cancer patients to become active participants in their care. Given the ubiquity of mobile devices and the omnipresent wireless connectivity, mHealth solutions have the capability to provide just-in-time support that is both adaptive and targeted to user needs. mHealth solutions can be used to generate and share patient-centred care planning, manage late effects with cancer and its treatments, promote lifestyle and behavioural changes and assist survivors with communication with healthcare providers. Mobile applications afforded cancer patients the ability to engage with their health providers and their support networks.8
The use of smartphones and mHealth applications is now almost universal. mHealth provides the opportunity to improve health communication, exchange medical information, educate target populations and record health data and support data collection, even in rural and remote areas. Countries with low medical resources need added support and assistance in the delivery of modern healthcare. The development of mHealth applications in cancer screening is a low-cost and easy-to-use strategy that appears to be appreciated by patients and caregivers, and which could potentially improve the quality of healthcare.9 The mHealth can measurably improve outcomes relating to health issues that commonly affect this population.10 Results of previous studies indicate the effectiveness of mHealth for self-management.10,11 This study aimed to examine the impact of mHealth applications on cancer screening.
Materials and Methods
Search strategy
We searched for articles published in electronic databases from January 1, 2008, to January 31, 2019, using 5 databases: IEEE, Scopus, Web of Science, Science Direct and PubMed.
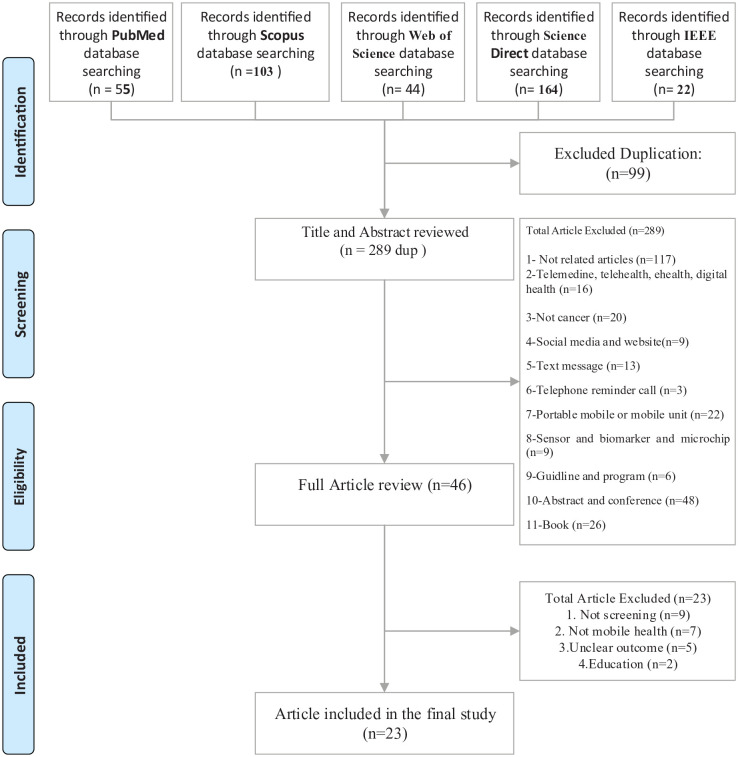
A researcher has conducted the research and found the related articles of the systematic review. The searches used the following keywords and medical subject heading (MeSH) terms in various combinations. We derived 2 broad themes that were then combined with the Boolean operator ‘AND’. The first theme in Mesh ‘mobile health’ was created by the Boolean operator ‘OR’ to combine text words (‘Mobile Health’, OR ‘mHealth’, OR ‘Smartphone*’, OR ‘Mobile app*’). The second theme ‘cancer screening’ was the broad aspect and created for the search strategy. In this study, to ensure the quality of this systematic review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used.12 This is a tool developed to confirm the quality of studies acquired during systematic reviews (see Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
IEEE indicates Institute of Electrical and Electronics Engineers.
Inclusion and exclusion criteria
We included papers with the following characteristics: (1) published in English, (2) published between 2008 and 2019, (3) papers were related to changes in cancer screening and (4) articles designed for app-based interventions to improve cancer screening. In this study, excluded criteria were qualitative studies, books, conference proceedings, dissertations, protocols, conference abstracts, protocol papers, editorials and commentary. Furthermore, unrelated subjects were excluded such as examining text messages and telephone reminder call, telehealth, telemedicine, eHealth, digital health, wearables, web, e-mails, twitter, social network services, vaccination, sensor, biomarker and microchip, scope, health marketing, biopsy, portable mobile or mobile unit, Personal Health Record (PHR) and Internet of Things (IoT). In this study, news, guidelines, booklet of conferences, magazine, educational programme and curriculum, Cancer programme, meeting, association (society), white paper report, bioinformatics and big data were excluded. We also excluded studies lacking indicators or outcomes for cancer screening, not using applications as the intervention tools or concentrating specifically on app design and development. Moreover, papers were removed if their content was unrelated to the research topic or insufficient and vague information existed.
Study selection
Three investigators independently reviewed papers based on titles and abstracts attributed to inclusion and exclusion criteria, and subsequently, the irrelevant studies have been removed. One reviewer (HS) conducted data extraction and other reviewers rechecked the accuracy of the results (NS, MA). The same researchers read and reviewed the entire texts to make the final decision. The reasons for inclusion and exclusion have been identified.
Data extraction and synthesis
An initial data extraction form was developed at this stage of the review. Data elements were extracted from each article that was organized in 2 sections: general items (study, year, country, cancer type, participants, intervention, follow-up, features, finding) and specific items (providing information, planning [goal-setting], education and training, positive feedback, remote clinical diagnosis, early detection, feasibility in low-resource setting or countries, availability and accessibility, clinical assistant, efficacy, effectiveness, ease of use and simplicity). The selected papers were summarized in the final step of our methodology and important factors were identified. Thus, the statistical results of systematic reviews were described for outcomes reported in the studies (see Tables 1 and 2).
Table 1.
Summary characteristics of articles included.
| Study | Year | Country | Cancer type | Participants, the Sample size | Intervention | Follow-up | Features |
|---|---|---|---|---|---|---|---|
| Asgary et al13 | 2016 | Ghana | Cervical cancer | CHNs, 15 | Visual inspection of the cervix under the acetic acid | 3 months | Feasibility Efficacy Training Diagnosis Feedback |
| Tanaka et al14 | 2017 | California, USA | Cervical cancer | 20 patients with abnormal cervical cytology | Apple smartphone (Smartoscopy) | Uterine cervix captured by smartphone after application of the acetic acid. (1) CIN1, note 12 o’clock for the acetowhite* epithelium; (2) CIN2, mention the epithelium acetowhite at 12 noon and (3) CIN3, note the epithelium of acetowhite and the mosaic at 1 o’clock | Improve the quality of cervical cancer screening Assistance in their healthcare delivery Digital imaging |
| Uthoff et al15 | 2018 | India | Oral cancer | High-risk populations in remote areas with insufficient resources, younger than or equal to the age of 18 | Android application | 6 months | Low cost Portable Simple to use Auto-fluorescent imaging systems to detect oral cancer Earlier detection and diagnosis Minimizing the progression of the disease and, ultimately, reduction in rates of death from oral cancer and the cost of healthcare |
| Yeates et al16 | 2016 | Tanzania | Cervical cancer | Healthcare workers 1072 eligible women, age 25 to 49 years |
VIA via smartphone | 1 month | Improve the sensitivity of VIA Detect cervical cancer in low-resource settings Easily store and exchange images over time for training and mentorship as well as potential quality assurance reports Permanent medical record Feasibility and efficiency of using a smartphone camera to improve VIA by obtaining digital photographic images of the cervix (cervicography) Sharing images Continuous real-time mentoring to CCS providers |
| Peterson et al17 | 2016 | Kenya | Cervical cancer | Over the course of a week, 6 organizations conducting VIA used the EVA system to screen 824 patients and providers had their diagnoses and treatments recorded in the application | EVA system Smartphone Screening Programme Using a Decision Support Job Aid |
1 week | Improve nurse’s confidence Quality improvement Educations |
| March et al18 | 2015 | USA and Europe | Melanoma | Practical application for melanoma screening | Mobile smartphone application | Not mentioned | Facilitate early melanoma detection Help identify melanocytic Lesion Sensitivity Specificity Detecting melanoma Reduce detection time Facilitate mobile teledermatology Self-diagnosis Improve the detection rate And the efficiency of self-skin examination |
| Zhang et al19 | 2017 | Europe and Asia | Prostate cancer screening | Not mentioned | The specific application for risk calculators | Not mentioned | Risk calculator Avoid unnecessary interventions Easily accessible |
| Gallay et al20 | 2017 | Saint Damien Health Care Center, Ambanja, Madagascar | Cervical cancer | Women aged 30 to 65 years were recruited in Madagascar for a CC screening programme | Smartphone image application | Between May and November 2015 | Low-resource settings Good quality images for VIA/VILI diagnosis Images classification in a patient database Simple and intuitive use of the application Correct match between image file and identity of the patient |
| Catarino et al21 | 2015 | Geneva, Switzerland | Cervical cancer | Women aged 30 to 65 years | Smartphone image application | Between May and November 2015 | Simple Intuitive Classification Good quality Education Data collection and image capture |
| Loescher et al22 | 2013 | Arizona | Skin cancer | Review | All types of advanced technology in skin cancer | Not found | Classification the melanoma Physician assistant Nurse practitioner Effectiveness Guidance Education Early diagnosis Recommendations for SSE Helping patient living in geographically remote |
| Lee et al23 | 2018 | USA | Breast cancer | 14 Korean American immigrant women | Mobile App (mMammogram) |
Between June 2014 and February 2015 | It is a practical, efficient and appropriate tool Further insights into the assessment and feedback on a mobile phone text message programme were received by mMammogram |
| Szanto et al24 | 2017 | Not mentioned | Lung cancer | Moderate and high-risk groups 89 500 users in 23 different countries |
Smartphone application (app) (LungScreen) | In 2014 for 20 months | Increase awareness and provide a personal risk assessment for lung cancer |
| Tran et al25 | 2018 | Saint Damien Health Care Center in Ambanja, Madagascar | Cervical cancer | This included 125 consecutive HPV-positive women Nonpregnant women aged between 30 and 69 years were invited to perform self-sampling of HPV (selfHPV) |
Smartphone-based digital images | February and October 2015 | Designed to help to make an accurate clinical diagnosis and ensure no missing CIN2+ lesions Lower price An easy-to-use device The prospect of storing the photos and classifying them in the patient’s file, making them available for comparison during follow-up visits |
| Tokosi et al4 | 2017 | Cape Town, South Africa | Breast cancer | Women aged 18 years and older | mHealth Interventions | Not mentioned | Suitable for targeted audiences Awareness Increased participation in breast cancer clinics Assist in determining whether mHealth has facilitated early detection and screening Increased enquiries about breast cancer through call centres, online forums and social media Improve healthy behaviours (eg, to improve awareness of breast cancer) Improve patient attendance (eg, increasing women’s participation in hospital workshops to enhance their knowledge of early detection, diagnosis, and treatment of breast cancer) |
| Ricard-Gauthier et al26 | 2015 | Ambanja, Madagascar | Cervical cancer | 300 females were screened primarily for HPV using self-collected vaginal specimens | Smartphone with a high-quality camera | Between July and November 2013 | Enhance visual images Feasibility Remote control The usefulness of the mobile phone High-quality image Improve screening strategy |
| Quercia et al9 | 2018 | Ambanja, Madagascar | Cervical cancer | Women aged 30 to 65 years participating in a screening campaign for cervical cancer in Ambanja, Madagascar | mHealth application | Between July and August 2016 | Improve quality Efficiency Transfer and collect data Supporting the role of EMR |
| Pereira-Azevedo et al27 | 2017 | Europe | Prostate cancer | Use algorithm and questionnaire All risk calculation algorithms used in the application were developed based on the ERSPC Rotterdam arm, using the clinical data and prostate biopsy results from 3624 previously unscreened men and 2896 men with previous negative prostate biopsy |
Mobile phone application | Not mentioned | Decision-making Provides supplementary information Increases predictive capability Optimizes prostate cancer screening Reduces unnecessary prostate biopsies while avoiding undiagnosis and preventing overtreatment of indolent prostate cancer mHealth offers the opportunity to transform the health services model, and prostate cancer, the world’s second most common cancer, must be included in this initiative High-quality health information |
| Owens et al28 | 2018 | USA and google search engine | Prostate cancer | 14 apps reviewed | Mobile phone applications | Between April and May 2017 | Provides general PrCA education by text only or video formats only News & Prevention Info Prostate Cancer Guidelines |
| Lee et al29 | 2017 | USA | Breast cancer | 120 Korean American women between the ages of 40 and 77 years | Mobile phone multilevel and multimedia messaging intervention | 6 months | Feasible, appropriate, acceptable and effective intervention Promotes breast cancer screening A flexible, easily tailored approach Greater improvement in ratings of breast cancer awareness and screening guidelines Provides high-quality health information |
| Gomes et al30 | 2017 | João Pessoa, northeastern Brazil | Oral cancer | A total of 55 people at high risk for developing oral cancer have been surveyed | Android system version 4.4.2, with JAVA language | Not mentioned | Sensitivity Specificity Accuracy Data collection Early diagnosis Providing noninvasive videos Good quality |
| Choi et al31 | 2018 | Korea | Skin cancer | Three electronic databases: PubMed, Web of Science and Embase We selected 18 studies that adhered to the review requirements for inclusion and exclusion |
mHealth app | 2007 and 2017 | Feedback Self-monitoring Availability |
| Birur et al32 | 2015 | Bangalore, India | Oral cancer | The study population (N¼3440) included a targeted cohort (n¼2000) and an opportunistic cohort (n¼1440), respectively, screened by FHW and dental professionals | Mobile phone cancer surveillance care programme | 12 months January to December 2010 |
Remote early detection Increased efficiency Feasible in low-resource settings |
| Birur et al33 | 2018 | India | Oral cancer | We conducted a pilot study in a targeted cohort screened by FHPs. FHPs and an opportunistic cohort screened by dentists There were 42 754 subjects screened and 5406 subjects with potentially malignant disorders identified |
mHealth-based approach | From 2010 to 2018 | Access to specialist care Make connections between specialist Provide widespread screening of underserved population relied on technical aspects to a great extent Cost-effective |
Abbreviations: CC, cervical cancer; CCS, cervical cancer screening; CHN, community health nurse; CIN, cervical intraepithelial neoplasia grade; EMR, electronic medical record; ERSPC, European Randomized Study of Screening for Prostate Cancer; EVA, enhanced visual assessment; FHP, frontline healthcare provider; FHW, frontline healthcare workers; HPV, human papillomavirus; PrCA, prostate cancer; SSE, skin self-examination; VIA, visual inspection under acetic acid; VILI, visual inspection with Iodine solution.
Acetowhite: staining and its significance in the diagnosis of oral mucosal lesions in women with genital HPV infections.
Table 2.
Summary of the positive impact of mobile health on cancer screening.
| Impact of mobile health | No. (%) |
|---|---|
| Providing information | 9 (39.13) |
| Planning (goal-setting) | 2 (8.69) |
| Education/training | 7 (30.43) |
| Positive feedback | 4 (17.39) |
| Remote clinical diagnosis | 7 (30.43) |
| Early detection | 8 (34.78) |
| Feasibility in low-resource setting or countries | 7 (30.43) |
| Availability and accessibility | 4 (17.39) |
| Clinical assistant | 5 (21.73) |
| Efficacy | 7 (30.43) |
| Effectiveness | 11 (47.82) |
| Ease of use and simplicity | 5 (21.7) |
Results
Characteristics of included studies
In this review, in terms of the intervention duration, the longest study duration was 20 months.24 Furthermore, the shortest study duration was 1 week.17 In terms of the populations and regions, 7 studies (30.4%) had a significant number of mHealth usage in remote regions with limited infrastructure for high-risk populations, remote clinical diagnosis and remote patient monitoring.9,15,22,26,30,32,33 The remote mHealth approach is a step towards a more successful oral cancer screening programme32 and also maintenance of patient records for follow-up.33 Seven studies (30.4%) had reported that mHealth improves healthcare quality in remote regions.14 Three studies (13%) had indicated that mHealth increases efficacy9,13,20,28,29,32,33 and 12 studies (52.1%) had shown that mHealth increases effectiveness.9,16,21-24,27,29,30-33 Participants in 5 studies (21.7%) provided positive feedback of using a smartphone.13,14,23,24,31 In terms of the type of interventions, 3 studies (13%) included the mHealth intervention with video systems.14,28,30 The comprehensive characteristics of included papers are summarized in Table 1.
The 23 selected studies were analysed in this systematic review, and the following 6 themes related to cancer screening were created: 39.1% cervical cancer,9,13,14,16,17,20,21,25,26 17.3% oral cancer,15,30,32,33 13% prostate cancer,19,27,28 13% skin cancer,18,22,31 13% breast cancer4,23,29 and 4.3% lung cancer.24 The cancer types are shown in Figure 2.
Figure 2.
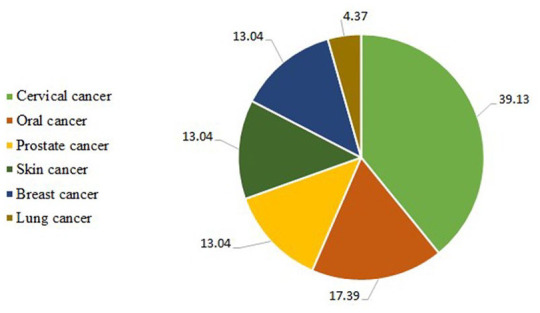
Cancer types screening by mobile health.
Content characteristics and positive impact factors of apps
Some app characteristics of contents and features were categorized according to the functions and impacts:17 These are providing information (39.1%),4,9,17,19,21,24,27,29,31 planning (goal-setting) (8.6%),13,24 positive feedback (17.3%),14,23,24,31 monitoring and evaluation (8.6%),9,17 decision-making (26%),1,9,17,20,21,27 education and training (30.4%),9,17,20-22,24,28 health awareness information (8.6%),4,24 remote clinical diagnosis (30.4%),9,15,22,26,30,32,33 feasibility in low-resource setting or countries (30.4%),15,16,20,21,25,26,32 early detection (34.7%),4,15,18,22,25,26,30,32 efficacy (30.4%),9,13,20,28,29,32,33 effectiveness (47.8%),14,16,21,23,24,27,29,30,32,33 ease of use and simplicity (21.7%),16,20,21,29,31 availability and accessibility (17.3%)9,25,28,31 and clinical assistance (21.7%).4,14,22,24,31
Furthermore, additional app characteristics, such as self-monitoring and self-diagnosing18,31 accuracy,30 enhanced visual image and high-quality image, improved screening strategy,26 transfer and collect data,9 increased health behaviour management,4 personal risk assessment,24 recommendations,22 classifications,20,21,22 flexibility,29 interaction and supporting job aid,17 medical records,16 avoidance of unnecessary interventions and biopsy,19,27 risk calculator,19 reduced time to detect, mobile teledermatology,18 and low cost and portable,15 were extracted from this study.
Half of these apps provide multiple functions for managing behaviours related to health. The most common functions of mHealth apps were providing the opportunity for education or training, remote clinical diagnosis, providing information, early detection, efficacy and effectiveness. All participants underwent usual or standardized care in the control groups. Table 2 gives an overview of the positive impact of mHealth from 2008 to 2019.
Discussion
It seems that mHealth apps are widespread and their effectiveness is increasing promptly.13,14,16,21,23,24,27,29,30,32,33 In this study, 23 studies had been selected to evaluate mHealth influence on cancer screening. Most studies indicated a positive contribution to the adoption of the smartphone. Participants launched the application on iOS or Android devices and had access to cancer screening applications. With the widespread use of smartphones in user’s daily lives, it is highly recommended to use mHealth apps for managing user’s health.
The important role of mobile devices is providing access to accurate and timely cancer data while emphasizing on the importance of data privacy and security during data transmission.34 mHealth-enabled telemedicine demonstrated the potential role of mHealth in supporting screening and diagnosis of cancers.35
The major barriers to mHealth are data security, confidentiality and ownership. Thus, the consideration of the ethical-legal aspects is of paramount importance when handling data in the mHealth field for cancer care.36 In whatever way, 3 studies had some limitation to use mHealth. Tran et al25 found that the smartphone’s image quality is probably not as good as those obtained with colposcopy. In addition, Quercia et al9 found that 1 of the problems faced by the on-site caregivers was the language barrier when trying to explain the study inclusion criteria, but once patients accepted to attend the screening, the use of the application instead of written paper records was no longer a limitation to the screening visit.
Lee et al29 reported that the lack of considerable differences in these results, such as the social desirability effects along with spillover effects or prospective contamination and social desirability, affects the results of the study. There are multiple potential confounding factors that are believed to have influenced the receipt of mammography in both groups, 1 of which is monthly phone calls to verify the receipt of mammogram over the 6-month follow-up. Owens et al,28 in addition, reported the lack of instructions available for education.
Nevertheless, it is hard to evaluate the impact of apps according to the findings of 1 single study. So, it is essential to have further studies on this issue. Eventually, this study, in which the results of reviewed studies have been considered, has indicated more reliable proof to show the influence of smartphone apps. More than half of the reviewed studies were about common cancers in women (cervical and breast cancer). In addition, the longest study duration was 20 months.24 Furthermore, the shortest study duration was 1 week.17 Five studies (22%) reported users’ satisfaction of using the smartphone app.9,13,28-30
According to Pereira-Azevedo et al,27 the mobile application has been designed to not only give patients support but also to help healthcare specialists in the process of the decision-making. The application seems to be easy to work with; hence, it is very useful in the everyday care of patients. It could be also used in a clinical setting to avoid unnecessary biopsies and decrease the risk of prostate cancer, and as a result, it can diminish overdiagnosis and overtreatment. Furthermore, Tokosi et al4 reported that the screening system has increased attendance at breast cancer clinics and promoted early detection and screening.
In the present research, half of the studies showed great effectiveness (47%).13,14,16,21,23,24,27,29,30,32-33 It could be presumed that as the application used in users’ daily lives is highly feasible and acceptable, the rate of retention is high. Therefore, it is possible to adapt mHealth apps significantly so that cancer screening outcomes in users can be promoted largely by monitoring, managing and assisting them. In this review, some studies9,17,24,31,32 considered apps that perform multiple functions, such as providing information, planning, feedback, monitoring, evaluation, decision-making, education and health awareness information. In contrast, other studies15,17,25,32 considered apps for telehealth services. This means that there are many unconditional features belonging to the apps that may not be able to work congruously. So, there is a need to have an efficient app to meet the users’ needs and intentions. Hence, by giving users the right feedback, mHealth app is able to prepare personalized information. In this review, there were several limitations. First, despite the reporting time limits, this systematic review was restricted to published articles from 2008 to 2019. Second, we surveyed published papers on 5 main databases. Therefore, this study can be a landscape for prospective studies. Third, in this review, the impact of mHealth intervention was included, but documents related to gamification and telehealth were not examined in this research. Fourth, we excluded other types of papers such as opinion pieces, editorials, viewpoints and publications in languages other than English. It will not be possible to provide an overview of all studies and all cancers around the world given our limited resources. That is why it is not appropriate to generalize these findings to other developing countries. Fifth, in this study, we did not consider phases of screening such as early diagnosis, early detection and screening test.
Conclusion
In this study, a summary of the features and advantages of the mHealth app in cancer screening outcomes has been given. Most of the employed mHealth technologies reported positive outcomes across the continuum of cancer screening. Along with the studies done previously, this study indicates that the use of mHealth apps can influence cancer screening positively, knowledge enhancement related to screening, presenting information, goal-setting or planning, reminding, monitoring, giving feedback, evaluation, support job aid, integration, decisions, education, interaction and health awareness information. Finally, mHealth interventions have demonstrated potential impacts on addressing various challenges facing cancer screening, even in low-resource settings, hence a promising field for supporting cancer care. In addition, most apps are proven to have a better function in improving cancer screening outcomes. Compared with conventional care users, most app users seem to be pleased with the use of mHealth. Although most studies taken into account suggested particular positive impact on health improvement, there is a great need to have other studies in which larger samples are used and more lengthy interventions are applied to confirm the positive effects of mHealth applications. Further study is needed to consider the health app’s impacts in larger detail.
Footnotes
Author Contributions: HS, MA and NS independently reviewed papers based on titles and abstracts attributed to inclusion and exclusion criteria and, subsequently, the irrelevant studies have been removed. HS conducted data extraction. NS and MA rechecked the accuracy. MA provided guidance on the article.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Hosna Salmani  https://orcid.org/0000-0001-8403-6673
https://orcid.org/0000-0001-8403-6673
References
- 1. Leon N, Schneider H, Daviaud E. Applying a framework for assessing the health system challenges to scaling up mHealth in South Africa. BMC Med Inform Decis Mak. 2012;12:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kumar S, Nilsen WJ, Abernethy A, et al. Mobile health technology evaluation: the mHealth evidence workshop. Am J Prev Med. 2013;45:228-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Perry R, Burns RM, Simon R, Youm J. Mobile application use among obstetrics and gynecology residents. J Grad Med Educ. 2017;9:611-615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tokosi TO, Fortuin J, Douglas TS. The impact of mHealth interventions on breast cancer awareness and screening: systematic review protocol. JMIR Res Protoc. 2017;6:e246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boudreaux ED, Waring ME, Hayes RB, Sadasivam RS, Mullen S, Pagoto S. Evaluating and selecting mobile health apps: strategies for healthcare providers and healthcare organizations. Transl Behav Med. 2014;4:363-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen TH, Yen AM, Fann JC, et al. Clarifying the debate on population-based screening for breast cancer with mammography: a systematic review of randomized controlled trials on mammography with Bayesian meta-analysis and causal model [serial online]. Medicine (Baltimore). 2017;96:e5684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mema SC, Yang H, Elnitsky S, Jiang Z, Vaska M, Xu L. Enhancing access to cervical and colorectal cancer screening for women in rural and remote northern Alberta: a pilot study. CMAJ Open. 2017;5:E740-E745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Geng Y, Myneni S. Patient engagement in cancer survivorship care through mHealth: a consumer-centered review of existing mobile applications. AMIA Annu Symp Proc. 2015;2015:580-588. [PMC free article] [PubMed] [Google Scholar]
- 9. Quercia K, Tran PL, Jinoro J, et al. A mobile health data collection system for remote areas to monitor women participating in a cervical cancer screening campaign. Telemed e-Health. 2018;24:277-282. [DOI] [PubMed] [Google Scholar]
- 10. Hernandez Silva E, Lawler S, Langbecker D. The effectiveness of mHealth for self-management in improving pain, psychological distress, fatigue, and sleep in cancer survivors: a systematic review. J Cancer Surviv. 2019;13:97-107. [DOI] [PubMed] [Google Scholar]
- 11. Yi JY, Kim Y, Cho YM, Kim H. Self-management of chronic conditions using mHealth interventions in Korea: a systematic review. Healthc Inform Res. 2018;24:187-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis: the PRISMA statement. BMJ. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Asgary R, Adongo PB, Nwameme A, et al. mHealth to train community health nurses in visual inspection with acetic acid for cervical cancer screening in Ghana. J Low Genit Tract Dis. 2016;20:239-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tanaka Y, Ueda Y, Okazawa A, et al. ‘Smartscopy’ as an alternative device for cervical cancer screening: a pilot study. BMJ Innov. 2017;3:123-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Uthoff RD, Song B, Sunny S, et al. Point-of-care, smartphone-based, dual-modality, dual-view, oral cancer screening device with neural network classification for low-resource communities. PLoS ONE. 2018;13:e0207493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yeates KE, Sleeth J, Hopman W, et al. Evaluation of a smartphone-based training strategy among health care workers screening for cervical cancer in northern Tanzania: the Kilimanjaro method. J Glob Oncol. 2016;2:356-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Peterson CW, Rose D, Mink J, Levitz D. Real-time monitoring and evaluation of a visual-based cervical cancer screening program using a decision support job aid. Diagnostics. 2016;6:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. March J, Hand M, Grossman D. Practical application of new technologies for melanoma diagnosis: part I. Noninvasive approaches. J Am Acad Dermatol. 2015;72:929-941. [DOI] [PubMed] [Google Scholar]
- 19. Zhang K, Bangma CH, Roobol MJ. Prostate cancer screening in Europe and Asia. Asian J Urol. 2017;4:86-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gallay C, Girardet A, Viviano M, et al. Cervical cancer screening in low-resource settings: a smartphone image application as an alternative to colposcopy. Int J Womens Health. 2017;9:455-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Catarino R, Vassilakos P, Scaringella S, et al. Smartphone use for cervical cancer screening in low-resource countries: a pilot study conducted in Madagascar. PLoS ONE. 2015;10:e0134309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Loescher LJ, Janda M, Soyer HP, Shea K, Curiel-Lewandrowski C. Advances in skin cancer early detection and diagnosis. Semin Oncol Nurs. 2013;29:170-181. [DOI] [PubMed] [Google Scholar]
- 23. Lee HY, Lee MH, Gao Z, Sadak K. Development and evaluation of culturally and linguistically tailored mobile app to promote breast cancer screening. Clin Med. 2018;7:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Szanto Z, Benko I, Jakab L, Szalai G, Vereczkei A. The use of a smartphone application for fast lung cancer risk assessment dagger. Eur J Cardiothorac Surg. 2017;51:1171-1176. [DOI] [PubMed] [Google Scholar]
- 25. Tran PL, Benski C, Viviano M, et al. Performance of smartphone-based digital images for cervical cancer screening in a low-resource context. Int J Technol Assess Health Care. 2018;34:337-342. [DOI] [PubMed] [Google Scholar]
- 26. Ricard-Gauthier D, Wisniak A, Catarino R, et al. Use of smartphones as adjuvant tools for cervical cancer screening in low-resource settings. J Low Genit Tract Dis. 2015;19:295-300. [DOI] [PubMed] [Google Scholar]
- 27. Pereira-Azevedo N, Osorio L, Fraga A, Roobol MJ. Rotterdam prostate cancer risk calculator: development and usability testing of the mobile phone app. JMIR Cancer. 2017;3:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Owens OL, Beer JM, Reyes LI, Thomas TL. Systematic review of commercially available mobile phone applications for prostate cancer education [published online ahead of print December 7, 2019]. Am J Mens Health. doi: 10.1177/1557988318816912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lee H, Ghebre R, Le C, Jang YJ, Sharratt M, Yee D. Mobile phone multilevel and multimedia messaging intervention for breast cancer screening: pilot randomized controlled trial. JMIR Mhealth Uhealth. 2017;5:e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gomes MS, Bonan PR, Ferreira VY, et al. Development of a mobile application for oral cancer screening. Technol Health Care. 2017;25:187-195. [DOI] [PubMed] [Google Scholar]
- 31. Choi J, Cho Y, Woo H. mHealth approaches in managing skin cancer: systematic review of evidence-based research using integrative mapping. JMIR Mhealth and Uhealth. 2018;6:e164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Birur PN, Sunny SP, Jena S, et al. Mobile health application for remote oral cancer surveillance. J Am Dent Assoc. 2015;146:886-894. [DOI] [PubMed] [Google Scholar]
- 33. Birur NP, Patrick S, Bajaj S, et al. A novel mobile health approach to early diagnosis of oral cancer. J Contemp Dent Pract. 2018;19:1122-1128. [PMC free article] [PubMed] [Google Scholar]
- 34. Mohammadzadeh N, Safdari R, Rahimi A. Cancer care management through a mobile phone health approach: key considerations. Asian Pac J Cancer Prev. 2013;14:4961-4964. [DOI] [PubMed] [Google Scholar]
- 35. Halake D, Ogoncho I. The role of mobile health in supporting cancer prevention, detection, treatment and palliative care in low and middle income countries: a scoping review. J Public Health Res. 2017;7:123-135. [Google Scholar]
- 36. Mechael P, Batavia H, Kaonga NN, et al. , eds. Barriers and gaps affecting mhealth in low and middle income countries: policy white paper. http://www.globalproblems-globalsolutions-files.org/pdfs/mHealth_Barriers_White_Paper.pdf. Updated 2010.