Abstract
Vulvar pain is a common complaint in women during reproductive and post-reproductive years. A 70-year-old woman experienced severe intractable vulvar pain after bladder cancer surgery and adjuvant radiation therapy. We performed five fluoroscopy-guided pudendal nerve blocks. Her numeric rating scale decreased from 10 to 3, and after 5 months, her pain was controlled only with oral medication. Pudendal nerve block might stop ongoing sensitization which lead acute nociceptive vulvar pain into chronic neuropathic vulvodynia by attenuating nociceptive stimulation and inflammation.
Keywords: Vulvodynia, Nerve block, Radiotherapy, Acute pain
Introduction
Vulvar pain is a common gynecologic complaint that has devastating effects on a patient's quality of life. It is characterized as perceptions of burning, stabbing, tearing, aching, or irritating, and dyspareunia is nearly always present as well. Studies of the general population have estimated that vulvar pain is present in more than 8% of reproductive aged women.1
Vulvar pain is caused by multiple factors and management depends on each factor. In general, it requires a multidisciplinary approach including medical treatment, psychological therapy, physical therapy, nerve block and surgery.2 Among them, pudendal nerve block may be a suitable treatment for vulvar pain.
Here, the authors report a case of a patient who complained of severe intractable vulvar pain. Authors diagnosed her pain as vulvar pain caused by adjuvant radiotherapy after bladder cancer surgery through a thorough evaluation of her history. Authors treated her with pudendal nerve blocks under fluoroscopic guidance and it was successful.
Case presentation
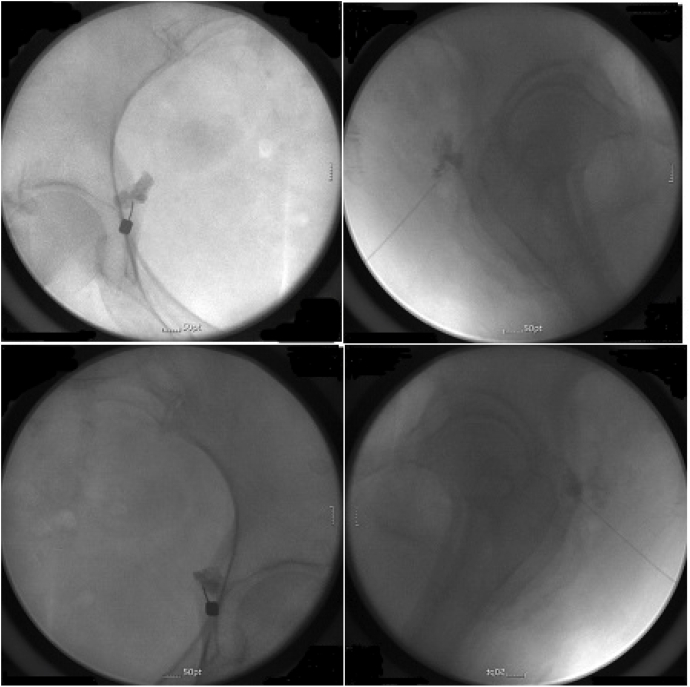
A 70-year-old woman was referred to the authors' pain clinic from the urologic department for severe intractable burning pain on the vulva and urethra. She got trans-urethral resection of bladder tumor(TUR-BT) 2 months prior to visiting our pain clinic and the result of biopsy showed that she had papillary urothelial carcinoma, high grade(1973 WHO histologic grade 3/3) and the muscle layer was invaded. She had received the adjuvant radiotherapy 22 times during a 2-month period. For the radiotherapy, radiation oncologic department used X-ray beam with dose of 66.6Gy in 37 fractions for targeting the bladder. After the 22nd radiotherapy, she suffered from a significant burning pain on her vulva and urethra. Numeric rating scale (NRS) was 10 out of 10. Her pain occurred spontaneously and persisted all day. It was so severe that she could not sit on the chair, lie down, and even sleep at night. In the pain clinic, the authors prescribed oral painkiller and buprenorphine transdermal patch to relieve her pain but it was not effective. Then, authors performed a caudal epidural block with a mixture of 0.5% bupivacaine 10mg(2ml), normal saline 8ml and triamcinolone 4mg but it was not successful. Thereafter, authors tried fluoroscopy-guided pudendal nerve blocks on both sides. The pudendal nerve block was performed in the prone position. A pillow was placed under the abdomen. A-P-Oblique view was taken to see the ischial spine optimally with C-arm. Skin entry point was just above the tip of the ischial spine. After local anesthetic infiltration, a 22-gauge spinal needle was advanced to the ischial spine and searched the point where she felt her original pain. Then, authors injected 1ml of non-ionic contrast medium and confirmed the correct position of the needle in A-P and lateral view (Fig. 1). Then, a mixture of 0.5% bupivacaine 10mg (2ml), normal saline 8ml and triamcinolone 8mg was administered. Even after the first pudendal nerve blocks, her pain was alleviated to 70%. After 2 weeks, the second pudendal nerve blocks were done and she told that she felt better than before and her pain decreased to 30%. Authors repeated the pudendal nerve blocks three times more, and thereafter, the burning pain on her vulva and urethra was well controlled with the medication and the transdermal patch. After 5 months, the pain was almost gone and authors decreased the dose of medication and even didn't give her a buprenorphine transdermal patch. After 6 months, she decided to get surgery for recurred bladder cancer in other hospital so authors could not follow up her anymore.
Fig. 1.
Fluoroscopic images of administration of pudendal nerve blocks: both AP and Lateral views.
Discussion
The classification system for vulvar pain of the International Society for the Study of Vulvar Disease (ISSCD) along with the International Society for the Study of Women's Sexual Health, and the International Pelvic Pain Society divides the vulvar pain conditions into 2 main groups: Vulvar pain and vulvodynia.3
In this case, the authors diagnosed her pain as vulvar pain, not vulvodynia because the duration of her pain is shorter than 3 months and there was a clear identifiable cause which is the radiotherapy. Radiotherapy affects both tumor tissue and surrounding normal tissue and it causes DNA damage and radiation-induced cell death. These lead to inflammation and eventually, tissue fibrosis and vascular damage, neural damage, and tissue necrosis may occur.4
We thought that irradiation of the bladder caused inflammatory process in the nervous system. This led to nociceptive pain near the pudendal nerve that is usually described as burning or stabbing in this case. Initially, a pudendal nerve block was performed to anesthetize the perineum during labor and the vagina for minor surgeries. Recently pudendal nerve block has been reported to be effective for relieving of pelvic pain.
Pain can be classified into two types which are nociceptive and neuropathic, even though some says both types are not distinct but different points on the continuing spectrum. The pathophysiology of neuropathic pain is complex after initial noxious stimuli. When stimuli persists, transition from nociceptive to neuropathic pain occurs through a cascade of biochemical and structural changes in nociceptive pathways of central and peripheral nervous system, which is called sensitization. The vulvar pain usually has an acute onset but in most cases, it is known to become a chronic condition lasting months to years.5
In authors' opinion, the curable ‘nociceptive’ vulvar pain may degenerate into the intractable ‘neuropathic’ vulvodynia without proper treatment due to the above mentioned ‘sensitization’. In this case, authors aimed for reducing nociceptive stimulation and inflammation which may potentially lead to sensitization near the pudendal nerves by performing pudendal nerve block in the early phase of inflammation before acute nociceptive pain became chronic neuropathic condition.
Conclusion
Similar to other pain conditions, vulvar pain can be intractable if proper therapy is not applied. Tissue injury causes inflammation that sensitizes nerves. If it persists, neuropathic change occurs in the peripheral and central nervous system which is very hard to recover. Therefore, as with other painful condition, vulvar pain should be treated with effective method to stop sensitizing nerves as soon as possible.
Financial conflict of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
References
- 1.Edwards L. Vulvodynia. Clin Obstet Gynecol. 2015;58:143–152. doi: 10.1097/GRF.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 2.Stenson A.L. Vulvodynia: diagnosis and management. Obstet Gynecol Clin N Am. 2017;44:493–508. doi: 10.1016/j.ogc.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Bornstein J., Goldstein A.T., Stockdale C.K. ISSVD, ISSWSH, and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. J Sex Med. 2015;13:607–612. doi: 10.1016/j.jsxm.2016.02.167. 2016. [DOI] [PubMed] [Google Scholar]
- 4.De Ruysscher D., Niedermann G., Burnet N.G., Siva S., Lee A.W.M., Hegi-Johnson F. Radiotherapy toxicity. Nat Rev Dis Primers. 2019;5:13. doi: 10.1038/s41572-019-0064-5. [DOI] [PubMed] [Google Scholar]
- 5.Fregoso G., Wang A., Tseng K., Wang J. Transition from acute to chronic pain: evaluating risk for chronic postsurgical pain. Pain Physician. 2019;22:479–488. [PubMed] [Google Scholar]