Abstract
we presented a case of drug-induced interstitial nephritis in a 43-year-old woman, having the history of renal calculi, as a result of sodium valproate and triamterene. Renal biopsy was used to confirm the diagnosis, however, due to poor prognosis along with discontinuation of drugs, she was treated with corticosteroids.
Keywords: Interstitial nephritis, Renal, Sodium valproate, Triamterene
Introduction
Interstitial nephritis can be caused by infections and hypersensitivity to drugs like methicillin, phenobarbital, diazepam, sodium valproate, diuretics, proton pump inhibitors, H2 receptor antagonists and nonsteroidal anti-inflammatory drugs.1,2 Drug-induced acute interstitial nephritis (DI-AIN) is associated with acute renal injury marked with increased creatinine levels and eosinophilia and is commonly diagnosed with renal biopsy. Infiltration of lymphocytes and macrophages, tubular atrophy and fibrosis are common findings from biopsy3 and is reported in 0.5–3% of renal biopsies.2 Discontinuation of drugs is an important step for the management of AIN. It is recommended that patients presented with acute kidney injury should be suspected for AIN.2 Herein, we presented a case of drug-induced interstitial nephritis in a 43-year-old woman, having the history of renal calculi, as a result of sodium valproate and triamterene. Renal biopsy was used to confirm the diagnosis, however, due to poor prognosis along with discontinuation of drugs, she was treated with corticosteroids.
Case presentation
A 43-year-old woman was reported to our center with muscle weakness, sharp clamping pain, muscle ache and swelling, shortness of breath and pain in the limbs. The patient had a history of bilateral renal calculi (kidney stones) for which she was hospitalized and underwent Trans Urethral Lithotripsy (TUL). For depression and obesity, she was under a number of medications including metformin, sodium valproate, fluoxetine, propranolol and triamterene-H while fenofibrate was added to her regime two weeks before her referral.
At the time of referral to the emergency department, her hemodynamic were stable: blood pressure 110/70, rate of respiration 16 and temperature 38.7 °C. Her labs showed: low density lipoprotein (LDH) > 5,000, creatine phosphokinase (CPK) > 18,000, creatinine (cr) > 6, blood urea nitrogen 128 mg/dl, white blood cell (WBC) 20,000/μl with eosinophils ≥ 500μl and increased liver enzymes and urine volume and reduced glomerular filtration rate. Her urinary sedimentation was clear and she had skin rashes on her arms and around wrist while her renal sonography was normal.
Due to increased nausea and vomiting, and shortness of breath, for which she underwent temporary thoracotomy. Additionally, she underwent 15 sessions of hemodialysis, where her nausea and vomiting improved along with urine output. However, her creatinine was still 234 μmol/L (2.65 mg/dL) and the blood urea 14 mmol/L.
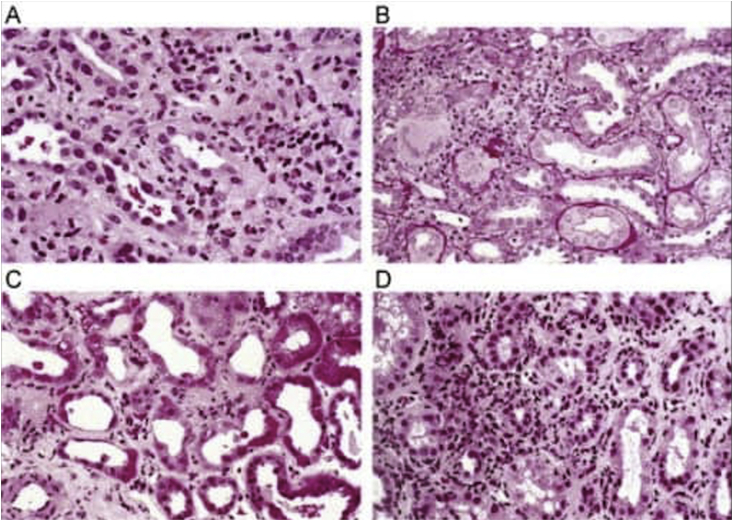
She underwent renal biopsy which showed interstitial inflammation and infiltration leukocytes, neutrophils, monocytes and eosinophils(Fig. 1). The epithelial cells showed necrosis and were mixed with lymphocytes. Invasion of inflammatory cells were also seen in the tubular basement membrane (tubulitis). All 16 glomeruli were normal along with vessels.
Fig. 1.
Drug-induced renal failure.
She was treated with prednisone with an initial bolus of 30 mg/kg methylprednisolone for two weeks and sodium valproate and triamterene-H were discontinued. Her 4 months follow-up labs showed serum cr 130μmol/l (1.47mg/dl) and eosinophils 300/μl.
Discussion
In this case report, patients was presented with DI-AIN as a result of sodium valproate and triamterene H, a thiazide diuretic. Magil, Ballon4 presented three cases reports of DI-AIN patients as a result of hydrochlorothiazide and triamterene. These patients were presented with a severe increase in blood urea nitrogen and creatinine and eosinophilia, similar the patient in this report. DI-AIN was confirmed with biopsy. They were presented with fever, anorexia, malaise and hypertension. The patients presented here had fever, rashes, nausea and vomiting and dyspnea.
Hypersensitivity to several different types of drugs have been correlated with acute renal failure as a result of immunological reactions. Plasma cells and monocytes infiltration is usually correlated with a late-type hypersensitivity.4 Similarly, Yoshikawa, Watanabe1 reported a case of DI-AIN as a result of sodium valproate in a young, who was presented with seizures, fever, metabolic acidosis, hyperuricemia, proteinuria and aminoaciduria. Her symptoms were overlapping with that of Fanconi Syndrome. However, AIN was confirmed with renal biopsy. Sodium valproate is also commonly known to be associated with renal tubular dysfunction, which is characterized with hypocarnitinemia, contrary to AIN.
Conclusion
Prolonged drug-induced hypersensitivity can lead to poor prognosis. Patients on DI-AIN causing drugs presented with acute kidney injury should be suspected for AIN and are likely to require renal biopsy for confirmation. Discontinuation of drugs can improve the symptoms whereas, corticosteroid are required in moderate to severe cases.
Contributors’ statement
Dr. Ziba Aghsaeifard: conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. Designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript.
Dr. Reza Alizadeh: Coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Declaration of competing interest
The authors deny any conflict of interest in any terms or by any means during the study.
References
- 1.Yoshikawa H., Watanabe T., Abe T. Tubulo-interstitial nephritis caused by sodium valproate. Brain Dev. 2002;24(2):102–105. doi: 10.1016/s0387-7604(02)00007-4. [DOI] [PubMed] [Google Scholar]
- 2.Nast C.C. Medication-induced interstitial nephritis in the 21st century. Adv Chron Kidney Dis. 2017;24(2):72–79. doi: 10.1053/j.ackd.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Krishnan N., Perazella M.A. Drug-induced acute interstitial nephritis: pathology, pathogenesis, and treatment. Iranian journal of kidney diseases. 2015;9(1):3. [PubMed] [Google Scholar]
- 4.Magil A.B. Acute interstitial nephritis associated with thiazide diuretics. Clinical and pathologic observations in three cases. Am J Med. 1980;69(6):939–943. doi: 10.1016/s0002-9343(80)80023-4. [DOI] [PubMed] [Google Scholar]