Abstract
Performing interstage home monitoring using digital platforms (teleIHM) is becoming commonplace but, when used alone, may still require frequent travel for in-person care. We evaluated the acceptability, feasibility, and added value of integrating teleIHM with synchronous telemedicine video visits (VVs) and asynchronous video/photo sharing (V/P) during the interstage period. We conducted a descriptive program evaluation of patient-families receiving integrated multimodality telemedicine (teleIHM + VV + V/P) interstage care from 7/15/2018 to 05/15/2020. First, provider focus groups were conducted to develop a program logic model. Second, patient characteristics and clinical course were reviewed and analyzed with univariate statistics. Third, semi-structured qualitative interviews of family caregivers’ experiences were assessed using applied thematic analysis. Within the study period, 41 patients received teleIHM + VV + V/P care, of which 6 were still interstage and 4 died. About half (51%) of patients were female and 54% were a racial/ethnic minority. Median age was 42 days old (IQR 25, 58) at interstage start, with a median of 113 total days (IQR 72, 151). A total of 551 VVs were conducted with a median 12 VVs (IQR 7, 18) per patient. Parents sent a median 2 pictures (IQR 0–3, range 0–82). Qualitatively, families reported an adjustment period to teleIHM, but engaged favorably with telemedicine overall. Families felt reassured by the oversight routine telemedicine provided and identified logistical and clinical value to VVs above teleIHM alone, while acknowledging trade-offs with in-person care. Integration of multimodality telemedicine is a feasible and acceptable approach to enhance in-home care during the interstage period.
Keywords: Telemedicine, Video visit, Interstage home monitoring, Remote patient monitoring, Advanced practice provider, Nurse coordinator
Introduction
Infants with single ventricle physiology (SVP) are medically fragile patients who require close surveillance between staged surgical palliations. Interstage home monitoring (IHM) of objective clinical parameters, such as daily weight, oxygen saturation, and enteral intake, has become a standard care strategy to minimize the morbidity and mortality of infants with SVP and other complex heart conditions between palliative interventions. [1–3] “TeleIHM,” which is the implementation of IHM using a remote patient monitoring digital platform, [4] has become increasingly widespread in the pediatric cardiology setting.
While teleIHM proactively tracks objective clinical parameters pertinent to a patient’s clinical status, teleIHM alone often excludes routine collection of contextual or subjective information (e.g., family perspective of how infant is doing, infant appearance) and by design typically occurs separately in time than other interactions with the health care team (i.e., asynchronously). Some platforms also allow for video/photo sharing (V/P), where a family can send a provider a photo or short video of their child, which also typically occurs in an asynchronous manner. So, while these tools provide important care delivery options, home surveillance based on asynchronous teleIHM and V/P sharing alone may still result in frequent patient travel for routine in-person evaluations or necessitate family-provider phone calls to discuss or clarify asynchronously collected information.
Video visits (VVs)—defined as real-time (i.e., synchronous) secure video conferencing between a health care provider and a patient and/or family caregiver [5]—provide another technological method to connect providers with family caregivers of affected infants. While VVs have become more common since the onset of the COVID-19 pandemic, the feasibility and acceptability of using these VVs along with teleIHM and V/P sharing as a scheduled method to enrich routine home surveillance during the interstage period remain mostly unexplored in the literature.
To improve this gap in the literature, we used program evaluation to explore our institution’s experience with integrating three telemedicine modalities (teleIHM, VV, and V/P sharing) during the interstage period. Program evaluation is an established public health method used to describe a program’s activities in a systematic way and assess its perceived value by end-users, in this case by patients and their families. [6, 7] Our goal in this manuscript was to use program evaluation to describe the acceptability, feasibility, and perceived added value of telemedicine, including its perceived impacts on patient care and the family experience.
Materials and Methods
Program Evaluation Approach
We conducted a descriptive evaluation of our single ventricle program’s use of three telemedicine modalities (teleIHM, VV, and V/P sharing) from 7/15/2018–5/15/20 using the Centers for Disease Control and Prevention (CDC) Framework for Program Evaluation. [6] We used the CDC’s mixed-methods approach of creating a logic model, engaging stakeholders through provider focus groups and family interviews to understand their experience of the program, and gathering evidence to summarize the key elements of the program (e.g., patient chart review) [6, 7].
The work was determined to be exempt by our Institutional Review Board as a program evaluation.
Program Logic Model Development
Focus groups were conducted with the interstage program providers and staff to develop a program logic model and care model diagram. [6, 8–10] The logic model synthesized the program’s elements into an outline of what was needed to make the program function. A care model diagram was then created to further describe the integration of telemedicine with in-person care.
Patient Characteristics
Data were extracted from the electronic health record to describe patient characteristics and clinical course. Collected data included basic patient demographics (e.g., age, sex, race/ethnicity), baseline cardiac physiology, type and dates of first and second procedure including discharge and admission dates, and feeding method. The total number of VVs, in-person clinic visits, emergency department (ED) visits, and planned and unplanned hospitalizations were totaled. TeleIHM data entry and adherence as well as use of V/P sharing were directly extracted from the teleIHM platform (LocusHealth ®, Charlottesville, VA). To evaluate the feasibility of teleIHM, adherence was defined as the total number of days of teleIHM data entry by the family (numerator) divided the total interstage days (denominator) times 100. Data were analyzed with univariate statistics using STATA (Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.). Results were presented using the median as the measure of central tendency given the non-normal distributions of most data.
Families Interviews
Qualitative semi-structured interviews were conducted with participating primary family caregivers (i.e., parents) to assess the acceptability, feasibility, and program value from the family perspective. Qualitative interviews are a method in medical research and program evaluation to “explore the experiences of participants and the meanings they attribute to them.” [8, 10] Participating family caregivers had to be legal guardians and proficient in either English or Spanish; temporary guardians of patients who were currently in custody of the state were excluded. Applied thematic analysis, a method to inductively identify themes expressed by interview participants, [11] was conducted using Dedoose software (V.8.3.17, Los Angeles, CA). Interviews were analyzed until the themes captured the majority of the data to describe the families’ experience with the program. [12].
Results
Program Description: Setting
The single ventricle program is part of the larger heart center within a freestanding quaternary care children’s hospital in the Midwest. Patients with a range of cardiac anatomy and physiology are followed in the program, and they typically include:
Infants with either single ventricle physiology such as hypoplastic left heart syndrome, tricuspid atresia, or double inlet left ventricle prior to bidirectional Glenn procedure; or
Infants with complex biventricular physiology requiring staged palliation with either ductal stent or aortopulmonary shunt placement prior to an eventual biventricular repair.
Patients are referred to the program at the time of diagnosis and followed throughout the “interstage period,” defined as the time from first discharge home to either bidirectional Glenn procedure or definitive biventricular repair. [3] Care for patients during the interstage period is coordinated through the single ventricle program’s high acuity clinic. The clinic is staffed by a dedicated registered nurse (RN) coordinator (A.S.), advanced practice nurse (APN) (M.S.), and four physicians including a dedicated medical director (K.A.).
Program Description: Use of Telemedicine Modalities
Since November 2016, all patients with single ventricle physiology whose parents were proficient in English or Spanish were trained in IHM prior to hospital discharge and sent home with home monitoring equipment, including a scale, pulse oximeter, and binder. Once home, the team’s dedicated RN coordinator and/or APN coordinated the IHM with oversight by the interstage cardiology attendings. In From July 2018 onward, families were assigned a tablet (iPad ® Cupertino, CA) to conduct VVs via a secure video-conference application (Polycom® RealPresence® system, Santa Cruz, CA). In September 2018, the program transitioned to teleIHM; so in lieu of a binder, the tablets were also loaded with the teleIHM platform (LocusHealth ®, Charlottesville, VA), which collects and displays information (e.g., heart rate, oxygen saturations, weight) entered by parents, provides V/P sharing, and offers access to pre-written materials (e.g., instructions, references) in both English and Spanish. Additionally, the tablets were loaded with supplementary applications, including an application to access their infant’s electronic health record (MyChart © Epic Systems Corporation, Verona, WI), applications for meditation and stress relief (Headspace © Headspace, Inc; Calm ©, Calm.com, Inc.), an application providing educational material on congenital heart conditions (Heartpedia ©, Cincinnati Children’s Hospital Medical Center), and an informational pop-up on cardiac catheterization written by the care team. For limited English Proficiency families, translation was provided by an interpreter who was placed on speaker phone by the cardiac provider during the VVs.
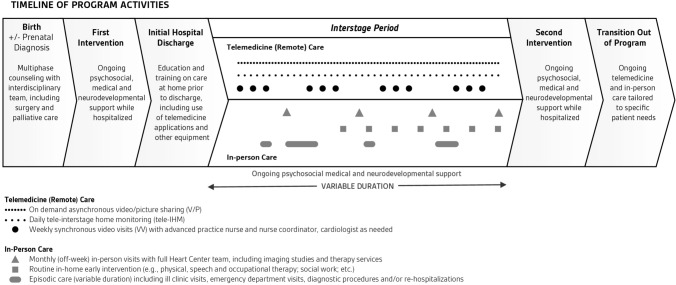
Program Description: Integrated Care Model Diagram
The Integrated Multimodality Telemedicine Care Model for Infants During the Interstage Period is shown in Fig. 1 demonstrating the high-level integration of VVs with teleIHM and V/P sharing for patients followed in the interstage program. Monthly clinic visits are conducted in-person with the cardiology providers and developmental team (speech, feeding, physical and occupational therapy) and typically include additional testing (e.g., echocardiogram, electrocardiogram). These in-person visits are supplemented with remote telemedicine care comprised of daily teleIHM data collection plus scheduled weekly VVs with the team’s APN or RN coordinator. For teleIHM, parents are required to document multiple daily elements that covered weight; heart rate; oxygen saturation; oxygen flow (if present); intake (feeding information, e.g., concentration, amount); outputs (stool, urine, and emesis); time to collect and input IHM, and presence/absence of parental concern. All are catalogued daily except for heart rate and oxygen saturation, which are documented twice per day. Optional data entry elements include topics such as breastfeeding and administration of Synagis. Family caregivers can additionally conduct asynchronous V/P sharing with the care team, on an as-needed basis. VVs are arranged weekly but are typically skipped during a week in which an in-person visit occurs. Additional VVs are scheduled more frequently if additional follow-up is desired. If available, therapists (e.g. speech/feeding) or nutritionists join the APN or RN coordinator in the VVs session. Following the end of the interstage period, the use of routine, scheduled VVs is determined on a per patient basis as needed and based on any protocols in place at the time of transition. TeleIHM with V/P sharing may also be utilized after the interstage period, if patients are experiencing significant heart failure, are medically fragile, or in the setting of ongoing, complex feeding regimens (e.g., nasogastric tube feed weaning).
Fig. 1.
Integrated Multimodality Telemedicine Care Model for Infants During the Interstage Period. It shows the program’s integration of virtual visits (VVs), tele-interstage home monitoring (teleIHM), and video/picture (V/P) sharing with in-person care from prenatal diagnosis or birth through the interstage period
Program Description: Logic Model
The program logic model is shown in Fig. 2 demonstrating program inputs and activities as well as intended outcomes and goal impact. The teleIHM operates as a unique partnership between the APN (M.S.) and RN coordinator (A.S), who is specially trained and focused on interstage care, allowing her to independently monitor and triage asynchronous V/P data and conduct synchronous VVs with families. If concerning data findings arise, the RN coordinator has direct and immediate access to APN and physician staff.
Fig. 2.
Logic Model of Integrated Multimodality Telemedicine for In-Home Care of Infants During the Interstage Period. Demonstrates the programs’ inputs and activities as well as intended outcomes and goal impact
The APN and RN coordinators’ activities are divided between “off camera” activities and “on camera” interactions with families. “Off camera” activities include telemedicine training, teleIHM and V/P data review, and care coordination. During the actual “on camera” VVs, the RN or APN coordinator obtains an interim history, discusses teleIHM data, shares study or lab results, conducts a visual assessment of the patient, solicits family understanding, and reinforces and counsels on any new adjustments to the care plan. The providers document a patient’s overall appearance, work of breathing, color, presence of facial swelling or secretions, incision appearance, placement of nasogastric tube and oxygen nasal cannula, as applicable. Providers also observe feedings. Physician team members are available on-demand during VVs to address any acute concerns and help determine next steps in management and assessment as needed. Physician team members also routinely review teleIHM for all patients weekly and as needed to identify abnormal values or trends and coordinated regularly with the patient’s other cardiologist(s) to maintain inpatient/outpatient continuity of information. Together the team’s on and off camera activities are integrated with the in-person care visits, with the goal of maximizing patient growth and development while minimizing morbidity and mortality in a family-centered manner.
Key Programmatic Facilitators and Barriers
A key facilitator to program development was the institution’s willingness to support dedicated RN and APN coordinator time to conduct the non-billable VVs prior to COVID-19-related reimbursement. The integration of VVs into care was also made easier by the care and education processes already in place for teleIHM, including family training before discharge. VVs, in turn, supported the family’s adherence to teleIHM by keeping families engaged in the teleIHM data entry process during weekly VVs.
Program barriers included limited therapist co-participation in VVs (e.g., feeding therapy) due to their inability to bill directly for the encounter. The inability to easily integrate language interpretation into the VVs for families with limited English proficiency remains an ongoing barrier, both due to platform interface challenges and scheduling constraints. Lower health or technology literacy of family caregivers, which required additional education and training, was also noted. Families who had no or low WiFi access were provided data-enabled tablets paid for by institutional funds. A working billing model for the teleIHM and V/P sharing care application, which is currently supported by institutional funds, remains an additional ongoing limitation.
Participating Patient Characteristics and Clinical Course
At the end of the evaluation period, 41 infants had received the fully integrated multimodal telemedicine (teleIHM + VV + V/P) care, of which 31 had completed the interstage period, 6 were currently receiving interstage care, and 4 had died. Participating infant characteristics are shown in Table 1. Overall, 51% of infants were female and 56% were a racial or ethnic minority. Median age at discharge from 1st surgery (start of interstage) was 42 days old (IQR 25, 58). Overall the median number of interstage days was 113 (IQR 72, 151). Of the infants who died: one died during a planned cardiac procedure and the other three died after immediate triage from home to an ED and/or inpatient setting.
Table 1.
Patient demographics and clinical characteristics
| Total N = 41 | N (%) |
|---|---|
| Age in days at initial discharge [median (IQR)] | 42 days old (25, 58) |
| Number of interstage days [median (IQR)] | |
| All infants combined | 113 days (72, 151) |
| Infants who completed interstage | 125 days (86, 154) |
| Infants still actively in interstage | 95 days (52, 378) |
| Infants who died during interstage | 40 days (21, 81) |
| Sex | |
| Female | 21 (51%) |
| Male | 20 (49%) |
| Race/ethnicity | |
| Non-Hispanic White | 19 (46%) |
| Hispanic | 11 (27%) |
| Non-Hispanic Black | 6 (15%) |
| Other or mixed race/ethnicity | 5 (12%) |
| Preferred language for medical care | |
| English | 38 (93%) |
| Spanish | 3 (7%) |
| Insurance coverage | |
| Medicaid | 24 (59%) |
| Private only | 17 (41%) |
| Surgical intervention prior to interstage | |
| Norwood | 12 (29%) |
| PDA stent | 12 (29%) |
| Main pulmonary artery Bandband | 6 (15%) |
| No surgical intervention | 5 (12%) |
| Aortopulmonary shunt | 4 (10%) |
| Other | 2 (5%) |
| Nutrition type at start of interstage | |
| Part by mouth, part by tube | 19 (46%) |
| Fully tube fed | 11 (27%) |
| Completely by mouth | 11 (27%) |
Demographic and clinical characteristics of patients receiving integrated multimodality telemedicine during the interstage period
IQR Interquartile range
Participating families reported that teleIHM data collection and entry took a median 10 min (IQR 5, 20). Adherence-wise, families entered teleIHM on a median 87.5% (IQR 73.1%, 94.7%) of the interstage days.
A total of 551 VVs were conducted with a median 12 VVs (IQR 7, 18) per infant. This equated to a median 3.4 VVs (IQR 3, 3.75) per month during the monitoring interstate period, excluding hospitalized time. A total of 154 in-person clinic visits occurred (median 4 (IQR 2, 5) per patient), which equated to a median of 1 (0.8, 1.3) in-person clinic visits per patient per month. A speech therapist joined in the care of 7 patients over 13 visits. Physical therapists joined one patient for a visit.
During the same period, 14 patients (34%) experienced an ED visit (total 22, range 1–4/patient). Twenty-five patients (61%) had a planned hospitalization (total 37, range 1–4/patient) and 23 patients (56%) experienced an unplanned hospitalization (total 44, range 1–11/patient). Overall, patients were hospitalized for a total of 298 days during the interstage monitoring period with a median of 4 (IQR 1, 11) hospitalization days per patient.
Most (n = 32, 78%) families used asynchronous picture sharing. However, picture sharing use ranged widely from 0 to 82 pictures shared per patient; with a median of 2 (IQR 1–20) pictures sent per patient. Fewer families (n = 8, 20%) used asynchronous video sharing; with a range of 0–19 videos shared per patient.
Family Interview Demographics
Out of thirty patient-families who were initially approached for an interview, 18 families participated while 2 actively declined, 6 passively refused (i.e., did not return call or email), and 4 were not reached. Two caregivers chose to participate within the same family (1 mother and 1 father); otherwise, only one family caregiver participated per child. All of the family participants were female (mothers), except the one male (father) who joined as an additional interviewee. Of the 18 mothers, 8 (44%) were non-Hispanic White and the remaining majority were a racial or ethnic minority. Three spoke Spanish. Mean age was 31 years old (SD 6.4) and 8 (44%) had less than a college degree (i.e., high school or trade school). All had experience with commercial video conferencing software (e.g., Facetime, Skype) prior to enrollment but only two had previous experience with virtual healthcare prior to their child’s interstage period.
Family Experience Themes
Eleven families reported experiencing a technological problem during VV care, but most problems were short-lived. One family had more long-standing problems with WiFi access due to their more rural locality. Another family had to swap out their tablet for a new one. VV scheduling was distributed evenly between morning and afternoon, with participants reporting timing was often based on a patient’s naptime.
Four general themes summarizing the family experience with the integrated multimodality telemedicine care are shown in Table 2 with illustrative quotes: 1) Adjustment Period, 2) Ease of Use, 3) Reassurance Provided by Remote Care, and 4) Tailoring of Care to Patient/Family. First, almost all families reported an adjustment period with the telemedicine activities, where they had to “get into a routine” with the daily teleIHM data collection and entry. Some reported adjusting quickly and reported it as “easy” and even “enjoyed” entering teleIHM data noting that they “liked being able to see the trends,” especially weight gain. A few families, however, found the daily teleIHM “time consuming and kind of stressful” and “a tad overwhelming,” primarily due to the amount of total care tasks they had to complete for their child while still recognizing the teleIHM was “for a good reason.” A few noted that this adjustment to the teleIHM occurred in conjunction with an emotional adjustment to being discharged home after sometimes long hospital stays, with parents noting that the VVs provided continuity with their in-person stay.
Table 2.
Family perceptions of the acceptability and feasibility of integrated multimodality telemedicine model of care
| Themes | Illustrative quotes |
|---|---|
| Adjustment period | |
| Adjustment to daily monitoring routine | "For me personally [teleIHM] was very complicated at first because it was a lot of things that I had to do at once. I had to do medication, I would write it down, then have to input into the iPad. But with time, one get’s used to multitasking.”—Parent 17 |
| Continuity with inpatient care | "I mean just that we were really grateful to have [the VV’s]. You know we didn’t know a lot about heart disease beforehand and …we were really grateful taking our first newborn home from the hospital and having someone like, two people to check in with [us] to kind of fill that void where nurses were taking care of a lot of stuff while we were in the hospital.”—Parent 8 |
| Easy Ease of use | |
| Ease of modality integration |
“[Doing both VVs and teleIHM was] fairly easy. I normally do her monitoring every morning and then right after that we normally have the [VV] ready.”—Parent 11 “I thought it was helpful that the nurses who I would speak to on the [VV] already had the data in front of us so they didn’t have to like ask me how it was going because they could see it for themselves.”—Parent 4 |
| Specific user-interface suggestions |
“Only I would change is let there be a notification in there when you need to update or if something is not being processed through. …You know like how on your phone like the settings on your phone indicate you need to update, I wish it had something like that.”—Parent 1 “I think maybe one thing I would say is so [my husband] would be at work usually during the calls and I’d [be] home with the baby. It would have been nice if there could have been some way for him to join the [VVs] also.”—Parent 9 |
| Adjunctive use of video/photo sharing |
“[My daughter] is has an NG (nasogastric) tube, so I [would] show [the providers] when she was eating by mouth like with a spoon or I show them like when she was like I took a picture like a birthday picture …Just multiple like things like you know milestones or like pictures that we were proud of… Like when they weren’t around, like when they were busy or have other calls … [V/P sharing] was easy to just you know reach out even when they’re busy, so like it was still convenient in a way.”—Parent 2 “I [shared] [my daughter] in her [holiday] outfit kind of thing, but I also took pictures …like you know different colors of her incision as she went through her healing process, you know just different things like that. She had some issues come up with her incision. She was slow to heal, so I had to take pictures and upload those.”—Parent 15 |
| Reassurance provided by remote care | |
| Integrated remote care provided “peace of mind” for families |
“Actually it made me feel like more comfortable with bringing her home knowing that in the beginning it was a weekly [VV] and the fact that we had to log all of that [teleIHM], even though it was overwhelming it made me feel more comfortable with the situation because I felt like we weren’t alone in you know trying to handle her medical issues, so yeah, it was actually kind of comforting having that.”—Parent 7 “I personally loved [the VVs]. I loved being able to touch base with our team every week. That was wonderful. And if I ever had any concerns, I knew that I was gonna be able to touch base with them and I mean just with like the complex needs of my son’s care. Like it was great to like always have the piece of mind to know that like I’m gonna get to touch base with them…—Parent 6 “I think it made me feel, I thought it made me feel a lot more comfortable just bringing him home. Everyone was, people were really accessible …I just thought it was helpful.” -Parent 9 |
| Tailoring care to patient need and family backgrounds or user preferences | |
| Desire to tailor data collection and visit frequency over time |
“I feel like once we got into our routine that it was very easy to log all of our daily information into the iPad. As far as our telehealth calls, I felt like [the providers] were always available to us… But I didn’t feel like they were necessary, you know as we got further out. … I felt like you know we had them I think once a month and that seemed to be very sufficient.”—Parent 15 "I just didn’t feel like things changed day to day that much and I already had so much to do that it was just one more thing to do and a lot of the times it was at the bottom of my list because there’s a lot more important things for me to do in my opinion… I don’t know if overwhelming is the right word, but it was hard for me to do … it was kind of, it was like very repetitive.”—Parent 6 |
| Preferences and ability gathering measurements |
“Sometimes it’s hard to remember [how much a child ate] after a whole day, so I think like if you just had to put it in almost after each feeding it would be a more accurate reading…”—Parent 13 “When I would take his oxygen, he would move his leg a lot. And sometimes he would move and I couldn’t take his oxygen. But then I would grab his leg or he would stop and everything was good.”—Parent 12 |
| Variable technology literacy and engagement |
“Well yeah, I had never done this before so I was afraid, right? What if I don’t do it right? This one time I did make a mistake, I didn’t do the password right and I locked the [tablet]. And my niece helped me and we unlocked it so we could continue to talk to the nurses.”—Parent 12 “I didn’t really pay attention to the [teleIHM] data that much unless something was like too alarming for me, but I think they were connected, yeah, because I think at [the hospital] they would look at the data and then let me know if something was off. They would let me know during the telehealth conference.”Parent 16 “I’m a very organized person when it comes to like having to have a schedule,..Like something was going on, it was detailed down to like the hour. … it took [the APN] to say you need to calm down, it’s okay if you do mid-day. It doesn’t have to be perfectly exact as we would like for it to be, but if you can do it mid-day, it’s okay. Just make sure you get a night one too.”—Parent 14 |
Illustrative quotes from family caregivers regarding their experience with the integration of video visits, interstage home monitoring, and video/audiopicture sharing for their children
Despite this adjustment, however, almost all interviewed families felt the telemedicine applications were “easy” to use. A few caregivers expressed stress and anxiety with the application interfaces during their first few uses. However, none of these challenges were sufficient enough for families to deter use and most issues resolved with some early trial and error. Some specific user-interface suggestions did arise for more “tech-savvy” families, most commonly the request for a notification/ or alarm for both teleIHM and VVs to remind parent about an upcoming data entry or a visit, respectively. One parent requested fewer “taps” to enter in data and the ability to view the rate of change in the data in addition to absolute values. Another wanted to customize some of her own data entry. One user noted that she would have liked to enter weight in pounds, not just kilograms. One family wished they had been offered the option of 3-way viewing to enable both parents to join in VVs when one parent was at work outside the home.
Families described the V/P sharing as a helpful adjunct to the more formal, scheduled VVs. They reported primarily using the photo function when they had specific questions about a rash, incision, or other skin finding. They also used this function for “social” and “fun” reasons, such as showing the child in a “cute” pose or outfit or on a milestone like a birthday, as a way to connect to the provider team. Some described liking the V/P sharing option because they knew it was sent and they “didn’t have to wait until our [scheduled VV] call,” but some of the families did not use the V/P sharing at all or only used it once or twice. Lastly, more than half of families reported positively engaging with supplementary applications;, but rarely described consistent long-term use.
Family caregivers did, however, consistently describe that the integrated telemedicine care provided them with “peace of mind,” “confidence,” “reassurance,” and/or “comfort” that the care team was making sure that they were not “missing anything” in their care at home which kept their “mind at ease.” Parents emphasized that consistent and routine communication through VVs and teleIHM provided reassurance that someone was keeping track of how their child was doing at home. Two even specifically noted that they felt that it eased the loss of bedside nursing care to which they had become accustomed while inpatient.
The family interviews also highlighted the need to tailor telemedicine care to the patient’s medical needs and the family literacy, preferences, and personalities. For example, a few families perceived that the frequency of teleIHM data collection and scheduled VVs could have decreased over time, noting it could often feel “repetitive,” and some parents reported different ability or preferences with the actual teleIHM data collection or measurement, such as feeling confident in how well they quantified oral intake or in using a pulse oximeter. One mother did not “pay attention” to the teleIHM data between visits and relied on VVs to discuss it, while others described expending a lot of time and emotional energy on data collection and review.
The specific “value-add” of VVs is summarized in Table 3 with illustrative quotes grouped by: 1) Logistical and Financial Value; 2) Clinical Value; and 3) Limitations/Other Considerations. Families reported a range of logistical advantages to VVs that included not just their time, but the cost of driving, stress of parking, and avoidance of foul weather exposure. Family caregivers recognized clinical value of VVs, including the avoidance of exposure to contagious illness and the ability of providers to visualize their child (e.g., breathing pattern). Families also felt that the VVs facilitated the opportunity to evaluate the teleIHM trends, including distinguishing any inconsistencies in the teleIHM data. Notably, this scheduled, summative discussion during VVs was reported as helpful both by family caregivers who described themselves as engaged heavily in the teleIHM (i.e., reviewed the teleIHM data trends actively on their own) and those who reported that they simply entered in data and only really reacted to alerts for out-of-range datum. Lastly, families reported that the use of VVs instead of in-person visits reinforced the infant’s normal biological sleep and feeding patterns, because they did not have to disrupt these patterns to travel to the clinic.
Table 3.
Summary of perceived added value and limitations of video visits during the interstage period
| Illustrative quotes | |
|---|---|
| Logistical and financial value | |
| Travel, parking, and wait time avoided | “I thought it was really convenient. We’re in the suburbs of [major urban city] but it still takes us like 2 h to get there and that was a really convenient way … to be able to get any changes to her treatment …I thought it was really helpful.”—Parent 13 |
| “I mean the calls, the video call seems way more efficient I guess because going in, seems like we always were stuck in a waiting room for almost like more than an hour usually between all the different visits we would do in a day. So a lot less wasted time traveling and parking, waiting.” -Parent 9 | |
| Travel cost avoided (e.g. gas, parking, missed work) |
“… my family as a whole, like the cost, like you pay, you have to pay to park, everything is a little more expensive because it’s downtown,..”—Parent 1 “Like coming in every week [for in-person visits], it’s money consuming, time consuming …”-Parent 2 |
| “[VVs] were pretty easy. I really liked [them]. We [could stay] home during cold months, so instead of going every single week to go see her often, like she was able to see him like through the screen.”-Parent 3 | |
| Clinical value | |
| Exposure to contagious illness avoided | “…I’d rather bring her in the hospital [only] once [by doing schedule VVs], especially we’re in the height of the flu season, … I would be risking her to get sick more than her being at home the majority [of the visits] and only having to come once a month.….”—Parent 1 |
| Allows for visual assessment of patient |
“I liked [the VVs] because you were able to interact and like [the providers] could, if there was something that was concerning throughout the week that I wasn’t comfortable with or you know I had to you know make some changes or I wanted them to see it you know for themselves, especially since I was doing both breastfeeding with the baby and feeding the baby through the tube, I wanted them to see how she was reacting and I think that helped because there were times where we were during the call that she was you know actively eating and they could see you know how everything was kinda going. …[and] like her breathing, like is she breathing okay?”—Parent 14 “You know with my daughter being a newborn, we would get her on the screen you know, just so that they could see her and kind of visualize you know here’s what we’re talking about with color or a change in this or her incision or something like that.”—Parent 15 |
| Facilitates discussion regarding teleIHM data trends, for family both more or less engaged in the teleIHM data |
“I really like that you can see any progress or like regression that was made on the [tablet]…[the VV’s] was actually one of the ways that they were able to see that she needed another surgery months earlier than they had originally thought.”—Parent 13 “I think the whole thing helped to keep everybody on the right track, so it was nice. You know having the [tablet] was amazing in the fact that I knew with confidence that I could log any information in there and then when we came for our visits, they could pull up all the graphs and the charts and the information and we often referred back to the data that was put in by my husband and I.”—Parent 15 |
| Disruption of infant biological patterns avoided (i.e. naps, scheduled feed |
“I think we mostly did [VVs] at 2:30. It was a time that just worked out between naps …”—Parent 6 “[In-person visits] would be a hassle because I had to put her on her feeding tube, like she was on a certain schedule. Sometimes the schedule would overlap right over like I was driving and I would have to feed her and she was one of those babies that was always throwing up throughout her feedings. …This was more convenient overall for us, for our family it just worked better.”—Parent 14 |
| Limitations/other considerations | |
| Trade off of longer in-person visits |
“I mean the longer in-person visits are challenging. They are really long. I think we spent over 6 h at the hospital one time or most times, and I mean this is minor but like stuff like not having time to eat lunch because all the back-to-back appointments and needing more supplies for him. Like they’re hard but at the same time I think doing an in-person visit every week would have been even harder. Going in every week would be even more time consuming.”—Parent 9 “… the only downside [to doing mostly VV’s with an occasional in-person visit] is sometimes there’s like a lot of waiting going on when we’re at [the in-person visits] but I’m not gonna complain about that (laughs) considering how few times we actually have to go there…”—Parent 7 |
| “Hands-on” evaluation still desired |
“Well in person it was different, because in person the nurses could see him, and touch him, and you can’t do that with the [VVs] so I think that’s different.”—Parent 12 "I guess in person you know [the providers] get to see my baby. They get to actually you know see her and if they want to examine her they can do that and then versus the [VV] they don’t have that option. But everything else is the same…”—Parent 11 “It’s always better in person for any details on medical questions of something that is more susceptible to the human eye than to a device.”—Parent 17 |
| Integration of interpreter services | “Because I understand English, I just don’t know how to express myself well in English. And some of the translator wouldn’t communicate things the way I was saying them. …because I understood the doctor. Not always, but sometimes. Or sometimes, their phone signal would drop, or their system, sometimes, the quality of their voice wasn’t good.”—Parent 18 |
Perceived value of video visits in addition to the other telemedicine modalities and in-person care, as reported by participating family caregivers. Limitations of video visits and other considerations when structuring virtual care are also noted
Family caregivers did recognize some limitations to VVs and its impact on their overall care experience. Most prominently, they recognized that having most of their visits virtually resulted in a much longer in-person visit in order to accommodate all the imaging and other hands-on evaluations that were not done in intervening weeks. When asked whether they would prefer fewer VVs in lieu of shorter in-person visits, all but one family preferred to continue to limit the number of longer in-person visits noting that the total time cost to them would still be less. The families did also recognize that the VVs were limited in their ability to perform every aspect of the physical exam, necessitating the option of some in-person care. Lastly, all three Spanish-speaking families reported phone interpretation as lower quality than in-person or video interpretation.
Discussion
This evaluation found that the integration of scheduled, routine VVs with remote home monitoring (teleIHM) through a multidisciplinary advanced practice model can feasibly enhance the care of in infants during the interstage period with overall high family acceptability. The death of four infants during the interstage period is consistent with the published norms for this population, but also highlights the high-risk nature of this cohort. [13–16] While one infant died during a planned cardiac procedure, the other 3 were outpatients who were rapidly triaged from home to higher-level care based using information obtained in part from the program’s telemedicine modalities. These are infants that might otherwise have died at home due to unrecognized subtle clinical changes.
While the use of VVs has long been described in adult health care [17, 18] and a range of pediatric populations [19], this evaluation provides new, detailed information about the specific experience for infants during the interstage period and their families. This work also highlights the roles of the APN and RN coordinator in facilitating the use of integrated telemedicine between in-person visits. As our logic model shows, these care providers conduct a diverse range of activities both on and off camera that streamline the coordination of care between the home, clinic, and hospital setting.
Given that this program was in place prior to the COVID-19 pandemic, care to patients was minimally disrupted when stay-at-home orders were announced and outpatient clinics had to adjust to new care restrictions. With the ensuing Executive Order that relaxed telemedicine regulations and expanded reimbursement for VVs, the program was then able to start billing for visits. While it is unknown at this time whether reimbursement for VV care will continue in the post-COVID era, the general expansion of VVs across institutions nationally [20, 21] may launch news models of care for patients, including outside of the interstage period.
One consideration from our study is how patients during the interstage period require care that is similar or different to other high-risk cardiac populations (e.g., early post-transplant, status post ventricular assist device, pulmonary hypertension) and how this model could be applied more broadly. As our findings show, family costs regarding the time and effort required for remote data collection (teleIHM) and provider time interpreting data must be weighed against the utility of the clinical information obtained between visits. These costs should be balanced against the costs of in-person health care appointments and both medical and family costs such as transportation and missed workdays. Additional consideration must be given to the strain and disruption of travel on the infants themselves, which is compounded by a child who may be on nasogastric feedings or require frequent medication dosing. These patient and family costs of care should not be underestimated given the increasing evidence that they are quantifiable barriers to health care access and optimal health outcomes, especially for disadvantaged groups including those with lower health literacy and/or limited English proficiency. [22–24] As the care of children with cardiac conditions continues to evolve, we should be vigilant to develop care models that do not necessarily remove but rather optimize in-person care. These considerations may be particularly beneficial for chronically ill patients with relatively rare diseases who may receive care at regional children’s hospitals far from home.
Expansion of integrated telemedicine modalities should also consider the individual needs of families including their technology preferences, health literacy, and access to digital platforms (e.g., WiFi access, digital internet). Published reports during the expansion of telemedicine during COVID-19 have highlighted the concern for inequities in the use of telemedicine-based care [25, 26], and programs should address these barriers during design and implementation. Our findings suggest that the initial training of families, adjustment period at home, and access to cellular data or WiFi are key areas of support.
Limitations and Future Work
As with any retrospective chart review, not all relevant data are available which limits the completeness of the evaluation and our sample size was relatively small. While this evaluation incorporates the viewpoints of Spanish-speaking families that are often left out of many evaluations, families and patients who were non-English/Spanish speaking were excluded from interviews. Given historical changes within the program and the fact that this program was rolled out to all patients, we did not have a pre or concurrent group with which to compare clinical outcomes. Therefore, future work should include rigorous evaluation of the application of integrated telemedicine models on interstage duration and unplanned health care and other clinical outcomes, including family stress, using quasi-experimental design. Also, given that families still recognize the value of the physical exam, the use of peripheral telemedicine devices such as digital stethoscopes to supplement VVs may also provide additional reassurance to families and clinical information to care providers between in-person visits.
Conclusions
This evaluation provides a transportable framework for the use of integrated scheduled VVs with teleIHM and V/P sharing as one potential solution to decreasing familial and patient cost of in-person evaluations in children during the interstage period. Our evaluation showed that scheduled VVs enrich teleIHM care from the family perspective, by providing reassurance and aiding in clinical care through visualization of the patient and connection with the family.
Acknowledgements
We thank Luis Morales for his assistance with interviewing Spanish-speaking families for this project.
Abbreviations
- CDC
Centers for Disease Control
- TeleIHM
Tele-interstage home monitoring
- SVP
Single ventricle physiology
- VVs
Video visits
- V/P
Video/photo sharing
- ED
Emergency department
- APN
Advanced practice nurse
- RN
Registered nurse
Authors’ contributions
Dr. Foster conceptualized the evaluation, oversaw data collection, conducted data coding and analysis, drafted the initial manuscript, and edited the final manuscript. Ms. Steltzer, Ms. Snyder, and Dr. Allen conceptualized the evaluation, aided in data collection, participated in data analysis, and reviewed and edited the manuscript. Ms. Helner conducted data collection, participated in data coding and analysis, and reviewed and edited the manuscript. Ms. Alden, Dr. Schinasi, and Ms. Bohling aided in conceptualizing the evaluation, participated in data review, and reviewed and edited the manuscript. All authors approved the final manuscript as written.
Funding
None.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ghanayem NS, Hoffman GM, Mussatto KA, et al. Home surveillance program prevents interstage mortality after the Norwood procedure. J Thorac Cardiovasc Surg. 2003;126(5):1367–1377. doi: 10.1016/S0022-5223(03)00071-0. [DOI] [PubMed] [Google Scholar]
- 2.Oster ME, Ehrlich A, King E, et al. Association of interstage home monitoring with mortality, readmissions, and weight gain: a multicenter study from the National Pediatric Cardiology Quality Improvement Collaborative. Circulation. 2015;132(6):502–508. doi: 10.1161/CIRCULATIONAHA.114.014107. [DOI] [PubMed] [Google Scholar]
- 3.Rudd NA, Ghanayem NS, Hill GD, et al. Interstage home monitoring for infants with single ventricle heart disease: education and management. J Am Heart Assoc. 2020;9(16):e014548. doi: 10.1161/JAHA.119.014548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shirali G, Erickson L, Apperson J, et al. Harnessing Teams and Technology to Improve Outcomes in Infants With Single Ventricle. Circ Cardiovasc Qual Outcomes. 2016;9(3):303–311. doi: 10.1161/CIRCOUTCOMES.115.002452. [DOI] [PubMed] [Google Scholar]
- 5.American Telemedicine Association. About telemedicine: what is telemedicine? https://www.americantelemed.org/main/about/about-telemedicine/telemedicine-faqs. Accessed 12 April 2018.
- 6.Centers for Disease Control and Prevention (1999) Framework for program evaluation in public health. Morbidity Mortality Weekly Report Recommendations Rep. 48(Rr-11):1–40. [PubMed]
- 7.CDC Evaluation Working Group. Summary of the Framework for Program Evaluation Morbidity and mortality weekly report Recommendations and reports. 1999;48(Rr-11):1–40. [PubMed]
- 8.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 9.Cohen DJ, Crabtree BF. Evaluative criteria for qualitative research in health care: controversies and recommendations. Ann Fam Med. 2008;6(4):331–339. doi: 10.1370/afm.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Britten N. Qualitative interviews in medical research. BMJ (Clin Res Ed) 1995;311(6999):251–253. doi: 10.1136/bmj.311.6999.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guest G. Applied thematic analysis. Thousand Oaks: SAGE; 2014. [Google Scholar]
- 12.Guest G. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. doi: 10.1177/1525822X05279903. [DOI] [Google Scholar]
- 13.Ohye RG, Sleeper LA, Mahony L, et al. Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. 2010;362(21):1980–1992. doi: 10.1056/NEJMoa0912461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azakie T, Merklinger SL, McCrindle BW, et al. Evolving strategies and improving outcomes of the modified norwood procedure: a 10-year single-institution experience. Ann Thorac Surg. 2001;72(4):1349–1353. doi: 10.1016/S0003-4975(01)02795-3. [DOI] [PubMed] [Google Scholar]
- 15.Tweddell JS, Hoffman GM, Fedderly RT, et al. Patients at risk for low systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg. 2000;69(6):1893–1899. doi: 10.1016/S0003-4975(00)01349-7. [DOI] [PubMed] [Google Scholar]
- 16.Hehir DA, Dominguez TE, Ballweg JA, et al. Risk factors for interstage death after stage 1 reconstruction of hypoplastic left heart syndrome and variants. J Thorac Cardiovasc Surg. 2008;136(1):94–99. doi: 10.1016/j.jtcvs.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 17.Finkelstein SM, Speedie SM, Lundgren JM, Demiris G, Ideker M. Telehomecare: virtual visits from the patient home. Home health care management & practice. 2001;13(3):219–226. doi: 10.1177/108482230101300307. [DOI] [Google Scholar]
- 18.Jerant AF, Azari R, Nesbitt TS. Reducing the cost of frequent hospital admissions for congestive heart failure: a randomized trial of a home telecare intervention. Med Care. 2001;39(11):1234–1245. doi: 10.1097/00005650-200111000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Burke BL, Jr, Hall RW. Telemedicine: pediatric applications. Pediatrics. 2015;136(1):e293–308. doi: 10.1542/peds.2015-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc JAMIA. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc JAMIA. 2020;27(7):1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolfe MK, McDonald NC, Holmes GM. Transportation barriers to health care in the United States: findings from the National Health Interview Survey, 1997–2017. Am J Public Health. 2020;110(6):815–822. doi: 10.2105/AJPH.2020.305579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lion KC. Caring for Children and Families With Limited English Proficiency: Current Challenges and an Agenda for the Future. Hosp Pediatr. 2017;7(1):59–61. doi: 10.1542/hpeds.2016-0186. [DOI] [PubMed] [Google Scholar]
- 24.DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(Supplement 3):S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 25.Zhai Y. A call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychother Psychosom. 2020;2020:1–3. doi: 10.1159/000509000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rajasekaran K. Access to telemedicine—are we doing all that we can during the COVID-19 pandemic? Otolaryngology. 2020;163(1):104–106. doi: 10.1177/0194599820925049. [DOI] [PubMed] [Google Scholar]