Abstract
Background
Little is known about the damage to the respiratory system in asymptomatic patients with coronavirus disease (COVID-19).
Objective
Herein, we evaluate the findings of chest computed tomography (CT) and radiography in patients with COVID-19 who were asymptomatic.
Methods
We retrospectively investigated patients with a confirmed diagnosis of COVID-19 but who did not show any symptoms. Among the 139 patients with COVID-19 who were hospitalized in Yeungnam University Hopistal in Daegu, South Korea, 10 (7.2%) were asymptomatic. Their chest CT and radiographic findings were analyzed.
Results
In the results, all patients (100%) had ground-glass opacity (GGO) on chest CT. Further, the GGO lesions were predominantly distributed peripherally and posteriorly in all patients. In 9 (90%) patients, the GGO lesions were combined with reticular opacity. Air bronchogram due to bronchiolectasis surrounded by GGO was observed in 8 patients (80%). Additionally, the lung lesions were dominant on the right side in all patients.
Conclusions
In conclusion, considering our results that the lung is affected in asymptomatic patients, it will be necessary to extend the indications of COVID-19 testing for effective management of COVID-19 during the pandemic.
Keywords: COVID-19, Asymptomatic patient, Radiologic finding, Computed tomography, Radiography
Introduction
In December 2019, an outbreak of the coronavirus disease (COVID-19) occurred in Wuhan, China, and the disease subsequently spread to approximately 200 countries within 3 months [1]. This disease causes massive alveolar damage and progressive respiratory failure, with 2–6% of COVID-19 cases leading to death [2]. The fatality rate is higher in older individuals and individuals having underlying diseases. Because COVID-19 is highly infectious, individuals who come in close contact with COVID-19 patients and those who have a confirmed diagnosis of COVID-19 are placed in isolation to prevent secondary and tertiary infections. Typical symptoms of COVID-19 include fever, cough, sputum, chest pain, and muscle soreness. However, approximately 46% (95% CI 18.48–73.60) of patients with COVID-19 are reported to be asymptomatic [3, 4, 5, 6, 7]. Asymptomatic COVID-19 patients are unlikely to be tested and will remain unaware of the fact that they have infection. Therefore, asymptomatic patients with COVID-19 can be a source of the spread. Moreover, if asymptomatic patients are left untreated, then damage to the respiratory system may occur. However, little is known about the damage to the respiratory system in asymptomatic COVID-19 patients. Therefore, in the current study, we evaluated the findings of chest computed tomography (CT) and radiography in patients with COVID-19 who were asymptomatic.
Methods
Of the 139 confirmed COVID-19 patients admitted to our university hospital (a 930-bed, tertiary referral hospital) between February 18, 2020, and April 11, 2020, we retrospectively selected patients with confirmed COVID-19 who did not show any symptoms of COVID-19 at the initial diagnosis or during the treatment period. All of the included patients had their diagnosis confirmed through RT-PCR (AllplexTM 2019-nCoV Assay; Seegene®, South Korea) with a pharyngeal swab at our hospital.
In the early stages of the COVID-19 epidemic in South Korea, all patients who were determined to be positive by a COVID-19 RT-PCR test were hospitalized in a negative pressure room, even if they were asymptomatic, to prevent the spread of COVID-19 in the community. The asymptomatic patients included in our study were infected by novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the early stages of the COVID-19 epidemic in South Korea. Therefore, even though all of the patients in our study were asymptomatic, they were hospitalized. In all of the patients who were investigated in this study, chest CT and radiography were performed as a standard process during admission to our hospital.
Definition of Symptoms of COVID-19
Patients with COVID-19 were classified as symptomatic if they had had at least one of the typical or atypical symptoms of COVID-19; patients exhibiting typical symptoms, such as subjective fever or temperature >100.0°F (37.8°C), cough, or shortness of breath, were classified as symptomatic with typical symptoms [8]. Atypical symptoms included chills, malaise, increased confusion, rhinorrhea, nasal congestion, sore throat, myalgia, dizziness, headache, nausea, and diarrhea [8].
Patient Characteristics
Among the 139 patients with COVID-19 who were hospitalized, 10 (7.2%) were asymptomatic. Their mean age was 65 ± 12.8 years (range: 52–95), and the sex ratio was 6:4 (male:female) (Table 1). Five patients (50%) underwent tests for COVID-19 because they had a contact history or possibility of contact with COVID-19 patients, and 2 patients (20%) had COVID-19 tests as a routine laboratory test on admission for treating other underlying disorders. The other 3 patients (30%) underwent COVID-19 tests as a routine laboratory test before surgical operation. No patient had a history of pulmonary disorders, such as chronic obstructive lung disease, tuberculosis, or lung cancer. Only 1 patient (patient 9) had a smoking history of one pack of cigarettes per day for approximately 50 years. The other patients had no history of smoking.
Table 1.
Epidemiology of each patient
| Patient No. | Age, years | Sex | Time to initiation of treatment (admission) after COVID-19 confirmation, days | Time to check radiograph after COVID-19 confirmation, days | Time to check CT after COVID-19 confirmation, days | Reason for COVID-19 test |
|---|---|---|---|---|---|---|
| 1 | 63 | F | 12 | 20 | 19 | History of contact with COVID-19 patients |
| 2 | 59 | 9 | 19 | 10 | Routine check for operation | |
| 3 | 59 | 3 | 11 | 11 | History of contact with COVID-19 patients | |
| 4 | 95 | 0 | 2 | 1 | Routine check for admission | |
| 5 | 60 | M | 12 | 13 | 12 | Routine check for operation |
| 6 | 73 | 5 | 6 | 5 | Possible contact with COVID-19 patients | |
| 7 | 53 | 8 | 9 | 8 | Routine check for admission | |
| 8 | 62 | 8 | 9 | 8 | History of contact with COVID-19 patients | |
| 9 | 74 | 0 | 3 | 3 | Possible contact with COVID-19 patients | |
| 10 | 52 | 1 | 2 | 1 | Routine check for operation |
Chest CT Protocol
All images were obtained using a CT system (Siemens Healthineers, Germany) with patients in the supine position. The main scanning parameters were as follows: tube voltage, 120 kVp; automatic tube current modulation, 30–70 mAs; pitch, 0.99–1.22 mm; matrix, 512 × 512; slice thickness, 1.0 mm; and field of view, 350 × 350 mm.
Qualitative Image Analysis
One radiologist (W.L.), with 25 years of experience, checked and confirmed the radiologic findings. We reviewed the initial chest CT images and radiographies taken on admission for each patient. We checked the CT findings for the same parameters as those mentioned in the previously reported cases, i.e., number of affected lobes, presence of GGO, consolidation, halo or reversed halo signs, a crazy paving pattern, air bronchogram manifested as bronchiolectasis surrounded by GGO, reticular opacity suggesting interstitial thickening or fibrosis, a subpleural line, and other combined pathologies including lymphadenopathy and pleural effusion [9].
The definitions of each term for describing the CT findings were as follows [10]: consolidation; increased pulmonary parenchymal density that obscures the margins of underlying vessels and airway walls; GGO; hazy areas with a slightly increased density in the lungs without obscuration of bronchial and vascular margins; halo, nodules, or masses surrounded by ground glass; a reversed halo, a focal rounded GGO surrounded by a more or less complete ring-like consolidation; a crazy paving pattern, thickened interlobular septa and intralobular lines with superimposition on a GGO background, resembling irregular paving stones; reticular opacity, interstitial thickening, or fibrosis; a subpleural line; and a thin curvilinear opacity, 1–3 mm in thickness, lying less than 1 cm from and parallel to the pleural surface.
In addition, the extent of lung involvement on chest CT images was assessed according to a previous study by Zhou et al. [11]. Each side of the lung was divided into 3 zones as follows: upper (above the carina), middle (from the carina to the inferior pulmonary vein), and lower (below the inferior pulmonary vein) zones. Each zone was then divided into the following 2 areas: anterior (the area before the vertical line of the midpoint of the diaphragm in the sagittal position) and posterior (the area after the vertical line of the midpoint of the diaphragm in the sagittal position). Thus, the bilateral lungs were divided into 12 zones. The degree of involvement of each lung zone was scored as follows: 0, no involvement; 1, <25% involvement; 2, 25% to <50% involvement; 3, 50% to <75% involvement; and 4, ≥75% involvement. Scores were recorded and summed for each lung zone, and the maximal score was 48.
Statistical Analysis
We analyzed the prevalence of each chest CT finding (number of affected lobes, presence of GGO, consolidation, halo or reversed halo signs, crazy paving pattern, air-bronchogram manifested as bronchiolectasis surrounded by GGO, reticular opacity suggesting interstitial thickening or fibrosis, subpleural line, and other combined pathologies including lymphadenopathy and pleural effusion) in asymptomatic patients with COVID-19 [12, 13, 14]. We also analyzed the prevalence of abnormal chest radiograph findings in asymptomatic patients with COVID-19.
Results
Treatment of Asymptomatic Patients with COVID-19
Although there were no symptoms in the COVID-19 patients included in this study, all 10 asymptomatic patients were treated with either hydroxychloroquine sulfate (Oxiklorine® at 400 mg/day q.d.) alone or a combination of hydroxychloroquine sulfate (Oxiklorine® at 400 mg) and lopinavir/ritonavir (400 mg/100 mg/day b.i.d.; Kaletra®) based on the abnormal chest CT findings. All 10 patients were admitted for at least 2 weeks and did not show any symptoms of COVID-19 until they were discharged home after being cured. The patients were judged to be completely cured if 2 RT-PCR tests were negative at 24-h intervals after at least 2 weeks since the initial diagnosis [15].
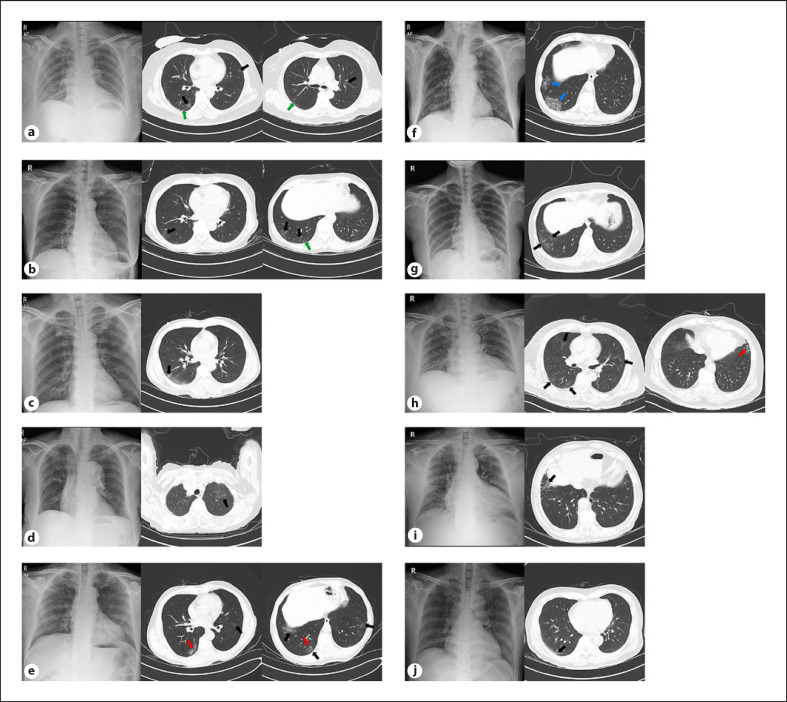
Findings of CT
The findings of chest CT and radiography in each patient are summarized in Table 2. Representative CT and radiographic images of each patient are presented in Figure 1. In the 10 asymptomatic patients, the median (range) number of affected lobes was 2.5 (range: 1–5). Three (30%) patients had 1 affected lobe, 2 (20%) patients had 2 affected lobes, and 4 (40%) patients had 3 affected lobes, while 1 (10%) patient had 5 affected lobes. Also, we scored the involvement of each patient's lungs according to a previous study by Zhou et al. [11] (Table 3).
Table 2.
Chest CT and radiographic findings for each patient
| Patient No. | CT |
Chest radiography | |||||
|---|---|---|---|---|---|---|---|
| GGO | Reticular opacity | Crazy paving | Air bronchogram | Subpleural line | others | ||
| 1 | RLL, LUL | RLL | RLL | RUL, RLL | Unremarkable | ||
| 2 | RLL | RLL | RLL | Unremarkable | |||
| 3 | RLL, LLL | RLL, LLL | RLL | Unremarkable | |||
| 4 | LUL | RLL, LUL, LLL | LLL | RLL | Unremarkable | ||
| 5 | RUL, RML, RLL, LUL, LLL | RLL, LLL | RLL, LLL | Unremarkable | |||
| 6 | RML, RLL, LLL | RML, RLL, LLL | RLL | RML, RLL, LLL | Patchy GGO at RLLF | ||
| 7 | RLL, LLL | RLL, LLL | RLL, LLL | Unremarkable | |||
| 8 | RUL, RLL, LUL | RUL, RLL, LUL | LUL | Bronchiectasis | Unremarkable | ||
| 9 | RML | RML | RML | Mild emphysema and bronchiectasis | Unremarkable | ||
| 10 | RLL | Mild emphysema | Unremarkable | ||||
RLL, right lower lobe; LUL, left upper lobe; RUL, right upper lobe; LLL, left lower lobe; RML, right middle lobe; RLLF, right lower lung filled.
Fig. 1.
Chest CT and radiographic images of each patient. Patient No. 1–10 (a–j, respectively). Black arrows: GGO and/or reticular opacity. Red arrows: air bronchogram (bronchiolectasis with surrounding GGO and/or reticular opacity). Blue arrows: crazy paving appearance. Green arrows: subpleural linear opacity. Red arrow: GGO in chest radiographs.
Table 3.
The extent of involvement of each patient’s lungs on chest CT images
| Patient No. | RUA | RUP | RMA | RMP | RLA | RLP | LUA | LUP | LMA | LMP | LLA | LLP | Sum of scores |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 6 |
| 2 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| 3 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
| 4 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 4 |
| 5 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 6 |
| 6 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 4 |
| 7 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
| 00 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 5 |
| 9 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 10 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
RUA, right upper anterior; RUP, right upper posterior; RMA, right middle anterior; RMP, right middle posterior; RLA, right lower anterior; RLP, right lower posterior; LUA, left upper anterior; LUP, left upper posterior; LMA, left middle anterior; LMP, left middle posterior; LLA, left lower anterior; LLP, left lower posterior.
Regarding chest CT findings, in all 10 asymptomatic patients, findings of consolidation and halo or reversed halo signs were not observed. All patients (100%) showed GGO on chest CT. Further, the GGO lesions were predominantly distributed peripherally and posteriorly in all patients. The GGO lesions of 9 (90%) patients were combined with reticular opacity of intralobular septal thickening, and air bronchogram due to bronchiolectasis surrounded by GGO was observed in 8 patients (80%). A definite crazy paving pattern appeared in only 1 patient (10%). Three patients (30%) showed subpleural lines. Additionally, the lung lesions were dominant on the right side in all patients (Tables 2, 3).
Findings of Chest Radiographs
On chest radiographs, 1 patient (10%) had subtle GGO. The other 9 patients' radiographs revealed no specific abnormal findings.
Discussion
Among the 139 patients with COVID-19 who were hospitalized, 10 (7.2%) were asymptomatic. In previous reports, 4–25% of people testing positive for COVID-19 have been reported to be asymptomatic [11, 16, 17]. The widely heterogeneous percentage of asymptomatic patients in previous studies may be due to different support systems for the cost of COVID-19 testing and different policies on screening in each country.
In this study, unlike in chest radiography, where only 10% were positive, all asymptomatic patients showed abnormal findings on their CT scans. Considering these false-negative results of chest radiography, CT scans must be recommended to confirm lung involvement in asymptomatic patients with COVID-19. In previous studies, 83.9–88.7% of symptomatic COVID-19 patients have shown abnormal CT findings [11, 18, 19]. In this study, however, all patients showed abnormal CT findings despite having no symptoms. Our results may be due to the fact that we did not check the chest CT immediately after diagnosis but rather a few days later after confirmation of COVID-19 (median: 8 days; range: 1–19). We hypothesize that SARS-CoV-2 was not allowed enough time to damage the patients' lungs in previous studies.
In this study, the CT scans showed increasing involvement of the peripheral and posterior distributions in asymptomatic patients with COVID-19, which is consistent with the CT findings of a previous study in symptomatic patients with COVID-19 [11, 18]. Zhou et al. [11] reported that lesions had a characteristic multifocal distribution in the middle and lower lung regions and in the posterior lung area as noted in the CT scans of symptomatic patients with COVID-19. Guan et al. [18] reported that more than 70% of CT scans in symptomatic patients with COVID-19 showed lesions in the lower lobe. In all of our patients, the right lung was predominantly involved. This finding was also consistent with that reported in a previous study [11]. Zhou et al. [11] reported that, of 10 patients with a single lesion, 9 (90.0%) had lesions that were initially located in the right lung and 1 (10.0%) had a lesion in the left lung. These results may be due to the innate anatomic features of the right inferior lobar bronchus. The bronchus of the right lower lobe of the lung is steeper and straighter than the left bronchial branches, and the angle between the right lower lobe and the long axis of the trachea is smaller; hence, in the early phase of COVID-19, the virus is more likely to invade the branches of the right inferior lobar bronchus and cause infection [11].
Regarding the change in CT findings according to the progression of COVID-19, Zhou et al. [11] showed the differences between abnormal CT findings in the early phase (≤7 days after symptom onset) and those in the advanced phase (8–14 days after symptom onset) of COVID-19 in 62 patients with COVID-19. In their study, they observed many GGO findings in the early phase (47.5 vs. 27.3%) and then an increase in GGO with reticular opacity (50.0 vs. 86.4%) and air bronchogram (62.5 vs. 90.9%) in the advanced phase [4]. Considering these results, in our study, the incidence rate of GGO with reticular opacity and air bronchograms was 90 and 80%, respectively; accordingly, CT patterns were somewhat similar to those in the advanced stage despite being asymptomatic.
In addition, for patients 9 and 10, we could not rule out the possibility of incidentally observed interstitial lung abnormalities. In our study, because we evaluated the chest CT findings in asymptomatic patients, even when subtle abnormal findings were observed, we described them as meaningful. Also, if previous studies reported some findings in chest CT as manifestations of COVID-19, we considered them to be findings associated with COVID-19. On the basis of the results of previous studies [12, 13, 14], findings such as GGO, subpleural lines, and intralobular septal thickening were described as COVID-19-related chest CT findings.
Our study has shown that asymptomatic COVID-19 patients also suffer significant lung damage. Although the prognosis of untreated patients with COVID-19 has not been reported, our results show that active screening may be necessary to detect asymptomatic patients with COVID-19 and manage them appropriately. Our study is the first to analyze the CT findings of asymptomatic patients with COVID-19. However, the present study has 2 limitations. First, changes in CT over the course of COVID-19 pneumonia have not been fully tracked and described for all patients. Second, we recruited a relatively small number of subjects. In the future, further studies to compensate for our limitations are required.
Statement of Ethics
Ethical approval was obtained from the IRB of Yeungnam University Hospital.
Conflict of Interest Statement
The authors have no conflict of interests to declare.
Funding Sources
This work was supported by the Research Program of Medicity Daegu Council funded by Daegu Metropolitan City (fund code: COVID19_DM19).
Author Contributions
Min Cheol Chang: data curation and writing of the original draft of this work. Jian Hur: data curation, conceptualization, and methodology. Donghwi Park: conceptualization, methodology, writing (review and editing), and supervision. Wonho Lee: data curation.
References
- 1.Singhal T. A Review of Coronavirus Disease-2019 (COVID-19) Indian J Pediatr. 2020 Apr;87((4)):281–6. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020 Apr;8((4)):420–2. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nishiura H, Kobayashi T, Miyama T, Suzuki A, Jung SM, Hayashi K, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020 May;94:154–5. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, et al. Public Health - Seattle & King County. CDC COVID-19 Investigation Team Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020 Apr;69((13)):377–81. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020 Mar;25((10)) doi: 10.2807/1560-7917.ES.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020 Apr;369:m1375. doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- 7.He W, Yi GY, Zhu Y. Estimation of the basic reproduction number, average incubation time, asymptomatic infection rate, and case fatality rate for COVID-19: meta-analysis and sensitivity analysis. J Med Virol. 2020 May;:jmv.26041. doi: 10.1002/jmv.26041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, et al. Public Health–Seattle and King County and CDC COVID-19 Investigation Team Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility. N Engl J Med. 2020 May;382((22)):2081–90. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest Radiographic and CT Findings of the 2019 Novel Coronavirus Disease (COVID-19): Analysis of Nine Patients Treated in Korea. Korean J Radiol. 2020 Apr;21((4)):494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008 Mar;246((3)):697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 11.Zhou S, Wang Y, Zhu T, Xia L. CT Features of Coronavirus Disease 2019 (COVID-19) Pneumonia in 62 Patients in Wuhan, China. AJR Am J Roentgenol. 2020 Jun;214((6)):1287–94. doi: 10.2214/AJR.20.22975. [DOI] [PubMed] [Google Scholar]
- 12.Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020 Jun;30((6)):3306–9. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020 Aug;30((8)):4381–9. doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang X, Song W, Liu X, Lyu L. CT image of novel coronavirus pneumonia: a case report. Jpn J Radiol. 2020 May;38((5)):407–8. doi: 10.1007/s11604-020-00945-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.European Centre for Disease Prevention and Control . Guidance for discharge and ending isolation in the context of widespread community transmission of COVID-19: first update. Solna: ECDC; 2020. [Google Scholar]
- 16.Zhou X, Li Y, Li T, Zhang W. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin Microbiol Infect. 2020 Jul;26((7)):957–9. doi: 10.1016/j.cmi.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020 Jun;20((6)):689–96. doi: 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan CS, Lv ZB, Yan S, Du YN, Chen H, Wei LG, et al. Imaging Features of Coronavirus disease 2019 (COVID-19): evaluation on Thin-Section CT. Acad Radiol. 2020 May;27((5)):609–13. doi: 10.1016/j.acra.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020 Aug;296((2)):E32–40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]