Abstract
We are reporting a rare case of collecting duct carcinoma in a 45years old male who was seeking for medical treatment of his persistent cough, dyspnea and weight loss. Chest x-ray revealed multiple focal opacities. Axial Contrast enhanced CT scan for the abdomen and pelvis showed right renal upper pole mass and D11 vertebral sclerotic metastasis. A core tissue biopsy for histopathology and immunohistochemistry was provisionally diagnosed as a clear cell carcinoma, however further immunohistochemical studies and histopathology consultation confirmed a Non-clear cell carcinoma, collecting duct carcinoma, that opens eyes on establishing earlier and accurate diagnosis of this rare tumor.
Keywords: Collecting duct carcinoma, Histopathology, Lung metastasis, Renal cell carcinoma
Introduction
Collecting duct carcinoma (CDC) is a rare malignant tumor arising from the distal part of the medullary collecting duct of the kidney, firstly described by Fleming S. & Lew H.J.E. on 1986. It accounts for less than 1% of all the other types of renal malignant tumors.1 It is an aggressively behaving tumor with a poor prognosis, most of the few previously reported cases showed a great tendency for metastasis and poor life expectancy, it is considered a rare entity as only few cases were reported in literature.2
Case presentation
A 45-year-old male, presented with a history of cough and dyspnea. The patient gave a history of gradual weight loss during the last six months. He received respiratory medical treatment for ten days with no response; chest x-ray was done and showed multiple focal opacities. Pelvi-abdominal ultrasound revealed a well-defined hypoechoic mass occupying the upper pole of the right kidney measured 6 × 3 cm likely neoplastic, but no other remarkable findings. Axial Contrast enhanced computed tomography scan for the abdomen and pelvis showed a right renal upper pole mass likely neoplastic and D11 sclerotic vertebral metastasis.
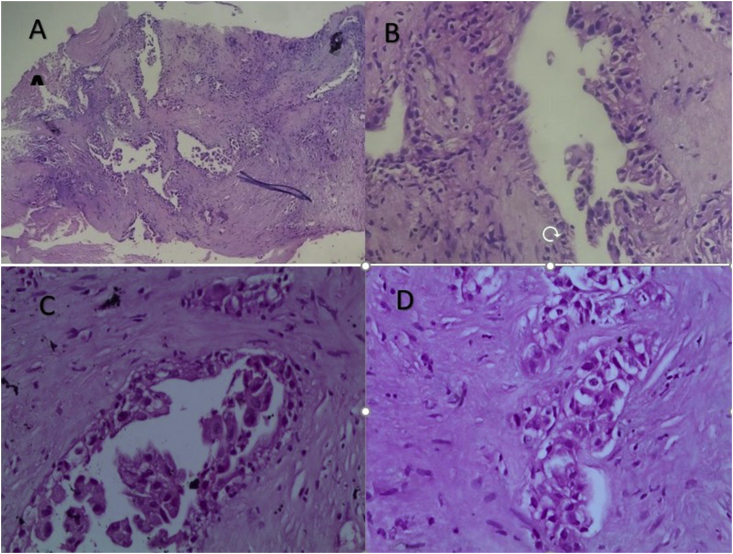
Core tissue biopsy was performed and prepared for histopathological examination. Upon the microscopic examination, a round to polygonal neoplastic cells with occasional prominent nucleoli and eosinophilic cytoplasm arranged in sheets and tubular pattern with occasional desmoplasia and necrosis was seen (Fig. 1). CD10 immunohistochemical staining was performed and provisional diagnosis of necrotizing clear cell type renal cell carcinoma (CCRCC) was done by two pathology trainees.
Fig. 1.
Histopathological features of tumor cells with mildly pleomorphic nuclei and eosinophilic cytoplasm arranged mainly in tubular pattern with surrounding desmoplasia (H&E stain; A: 4x B:20x. C,D: 40x).
Upon the histopathology consultation; CD10 immunohistochemical staining was seen cytoplasmic and not membranous that lead to exclude the diagnosis of CCRCC and considering the differential diagnosis of Renal pelvis urothelial carcinoma (RPUC), Metastatic carcinoma and collecting duct carcinoma.
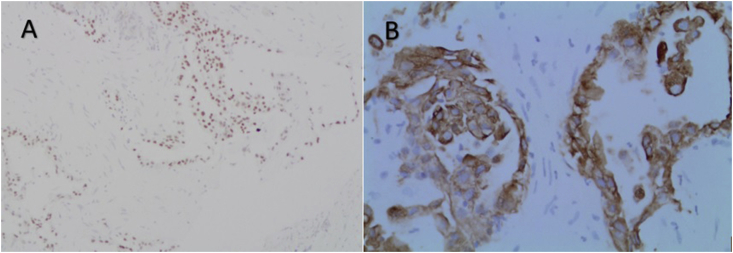
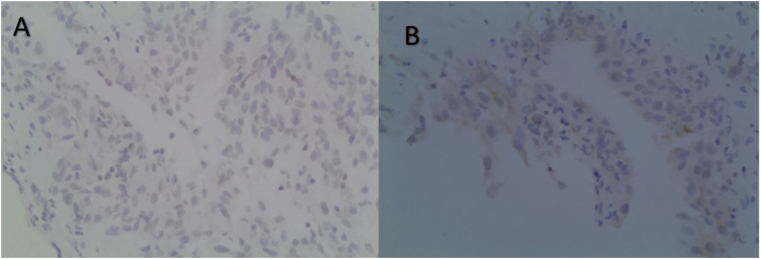
Further immunohistochemical analysis showed negative staining of P63, CDX2 and TTF1 and positive staining of PAX8 and the high Molecular weight Cytokeratin (HMWCK) (Fig. 2 and Fig. 3) which suggested primary renal cell tumor. The surgical pathology report was issued showing a final diagnosis of “collecting duct carcinoma with suggestive lung and vertebral metastasis”. However the examined material was very small, the staining negativity of CDX2 (ruling out colonic metastasis), TTF1 (ruling out both lung and thyroid carcinomas) and P63 (excluding RPUC) supported reaching out this final diagnosis.
Fig. 2.
Immunohistochemical stain of PAX8 showing nuclear staining (A), and HMWCK showing membranous staining (B).
Fig. 3.
Negative Immunohistochemical staining of P63 and TTF1.
The tumor appeared inoperable and the patient was referred to the oncologist but deteriorated and died six months later.
Discussion
The recent WHO classification of the renal tumor in 2016 refers to malignant types according to predominant cytoplasmic, architectural and anatomic features, correlation with a specific renal disease background as well as molecular alterations. CDC is a malignant tumor originating from the distal part of the collecting ducts.3
CDC usually presented by abdominal pain, flank mass and haematuria. It is more likely to present as advanced stage metastatic disease. The lung is the most common site (57%), followed by lymph nodes (48%) and osteoblastic bony metastasis.4 The Patient, in this case, was presented by non-specific pulmonary symptoms manifested as cough and dyspnea. Metastasis was suggested by radiology in lung and bone after the detection of a large kidney mass.
It is a fact that no CT or MRI findings can allow differentiating CDC from other renal tumors variants. Histopathological examination of the tissue remains the only precise diagnostic tool; hence percutaneous core biopsy was the option to obtain a confirmed diagnosis directing towards the most appropriate form of treatment in metastatic diseases.1,2
Due to the rarity of the CDC and the early age presentation of the case, it is necessary to exclude the possible other common renal cell tumors. The conventional type of clear cell carcinoma is the most prevalent renal tumor, needed to be excluded in our case. CD10 stain was performed to differentiate CCRCC from non-CCRCC which gives a positive membranous pattern of staining.1,5
There are different histologic patterns could be seen in CDC including tubulopapillary and glandular structures with high nuclear grade and stromal desmoplasia. Infrequently, focal necrosis was reported. Urothelial adenocarcinoma invading the renal parenchyma may elicit a desmoplastic response and mimic collecting duct carcinoma which was excluded in our case due to the negative staining of p63 and positive PAX8.5
The late presentation of CDC is carrying poor prognosis and short life expectancy post-diagnosis. A retrospective study of Ciszewski et al. group included 1042 cases of renal neoplasm from 1999 to December 2013 identified 10 cases (0.96%) of CDC. The median overall survival was 7.6 months, and only 2 patients survived more than 2 years after nephrectomy.2
More recent, in the cohort study reported by Qian et al., 12 cases of CDC out of 2200 renal malignancies diagnosed from 2007 to 2017 which is considered the largest number of cases reported in the literature during 10 years showed 11 months median survival rate, and only 1 patient survived for more than 5years even post-surgical treatment by nephrectomy.1
Conclusion
Collecting duct carcinoma can be misdiagnosed as a clear cell carcinoma in case of having only small necrotizing renal tissue core stained only by H&E and CD10 and examined by a non-expert pathologist, so considering a panel of immunohistochemical stains and uropathology consultation is recommended. This CDC can present late by metastasis carrying poor prognosis. As the number of diagnosed cases is rising, accumulation of data is necessary for establishing earlier accurate detection and possible treatment of cases.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
The conception and design of the case report: Abdulkarim Hasan and Amal Ismail.
Acquisition of the clinical presentation: Hesham Abozied and Ahmed Youssef.
Radiology analysis: Sherif Fayad.
Interpretation and analysis of histopathology and immunohistochemistry: Abdulkarim Hasan and Amal Ismail.
Literature search: Amal Ismail, Abdulkarim Hasan and Hesham Abozied.
Drafting the case report: Abdulkarim Hasan, Amal Ismail, Hesham Abozied, Ahmed Youssef and Sherif Fayad.
Final revision: Abdulkarim Hasan and Amal Ismail.
Declaration of competing interest
The all authors declare no any competing interests of this article.
Acknowledgment
The authors would like to thank Dr. Samy El-Hakim and Dr Gamal Dawood (professors and former heads of pathology department at Al-Azhar University Hospitals) for their expert opinion and insightful advice for this case.
Contributor Information
Abdulkarim Hasan, Email: doctorabdulkarim7@gmail.com.
Hesham Abozied, Email: aboziedhesham@gmail.com.
Ahmed Youssef, Email: ahmedyoussef664@gmail.com.
Sherif Fayad, Email: dr.sheriffayad@gmail.com.
Amal Ismail, Email: amal.zumrawy2012@gmail.com.
References
- 1.Qian X., Wang Z., Zhang J., Wang Q. Clinical features and prognostic outcome of renal collecting duct carcinoma: 12 cases from a single institution. Canc Manag Res. 2020;12:3589–3595. doi: 10.2147/CMAR.S244094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ciszewski S., Jakimów A., Smolska-Ciszewska B. Collecting (Bellini) duct carcinoma: a clinical study of a rare tumour and review of the literature. Can. Urol. Assoc. J. 2015;9(9-10):E589. doi: 10.5489/cuaj.2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moch H., Cubilla A.L., Humphrey P.A. The 2016 WHO classification of tumours of the urinary system and male genital organs—part A: renal, penile, and testicular tumours. Eur Urol. 2016;70(1):93–105. doi: 10.1016/j.eururo.2016.02.029. [DOI] [PubMed] [Google Scholar]
- 4.Mathisekaran T., Raghavan D., Muthu R. Collecting duct carcinoma of kidney: masquerading as genitourinary tuberculosis-Lessons learnt. Urol. Case Rep. 2020;29:101100. doi: 10.1016/j.eucr.2019.101100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu Q., Cao Q., Liu N. Renal collecting duct carcinoma with extensive coagulative necrosis mimicking anemic infarct: report of a case and the literature review. Diagn Pathol. 2013;8(1):119. doi: 10.1186/1746-1596-8-119. [DOI] [PMC free article] [PubMed] [Google Scholar]