Abstract
Prostate cancer often spreads to bony sites, but other metastatic sites are exceptional. Brain localization accounts for less than 4% of postmortem cases.The cerebral metastases of a prostatic ADK are rare, the prognosis is unfortunate and the treatment is based on androgen deprivation and radiotherapy. We describe a case of orbital metastasis of prostatic adenocarcinoma and we highlight the diagnostic and therapeutic singularity of this affection.
Keywords: Prostate cancer, Brain metastasis, Orbital metastasis, Hormone therapy
Background
Prostate cancer is the second most common cause of cancer death in men after lung cancer and the most common in men after the age of 50.1 We report the exceptional case of a frontal brain, for which the patient was operated on and for which the immunohistochemical study of the surgical specimen was in favor of prostate adenocarcinoma.
Case presentation
68-year-old patient followed for hypertension for 6 years on calcium channel blocker and chronic smoking.
The patient reported symptomatology evolving over the past 6 months consisting of morning headache, vomiting, and decreased visual acuity associated with Lombosciatalgia, diffuse bone pain, and pollakiuria.
Clinical examination finds a patient in good general condition, PS: 2, apyretic, with the presence of a right exophthalmos. The Rectal examination found a hard prostate in its entirety, with a soft bladder base. The rest of the clinical examination is normal.
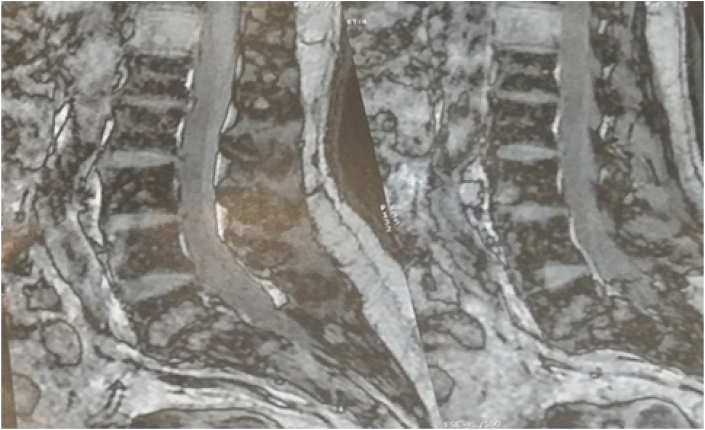
The patient benefited from a cerebral CT scan objecting to a frontal process. The patient's biology showed normal renal function and a PSA level of 495ng/ml. Prostate biopsy revealed a Gleason 9 (4 + 5) prostatic adenocarcinoma, spine radiology had shown diffuse vertebral bone demineralization confirmed by lumbar MRI which found a double dorsal T12 and sacral S2, S3 lesion with sacral intra-channel extension (Fig. 1).
Fig. 1.
Dorso-lumbar MRI objectifying the two lesions.
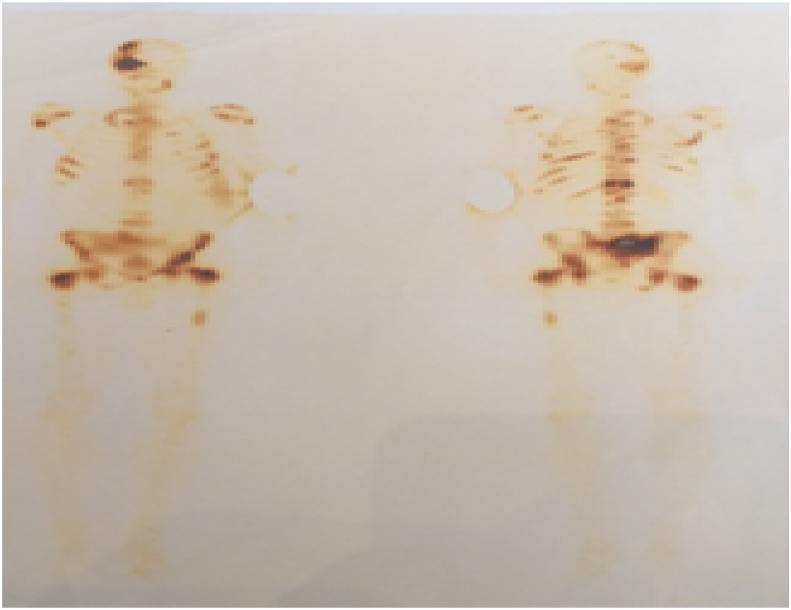
Bone scintigraphy showed several interesting areas of hyperfixation of different intensity and extent: the skull, face, cervical, dorsal, lumbar and sacral spine, femur, and sternum (Fig. 2).
Fig. 2.
Bone scan showing metastatic locations.
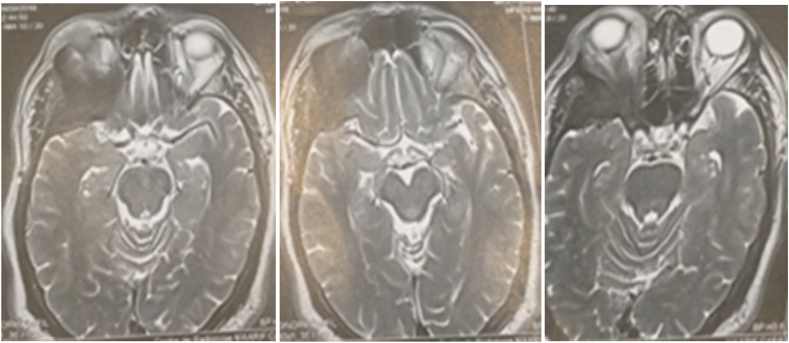
A cranio-orbital MRI showed a right sphenoidal process with hyposignal T1 at the postero-external wall of the orbit responsible for an exophthalmos. This process exerts a mass effect with compression and repression of the external orbital muscle and the optic nerve. The lesion measures 32/24 mm axially and 49/32 mm sagittally. This aspect was in favor of right spheno-orbital plate brain metastases responsible for exophthalmos (Fig. 3).
Fig. 3.
Cranio-orbital MRI objectiving the spheno-orbital process.
After The Multidisciplinary Concertation Meetings (MCM) and discussion with the patient, it was decided to start a hormonal treatment composed of a complete androgen blocking, associating a GnRH analog, and a non-steroidal anti-androgen as well as first line chemotherapy combined with analgesic radiotherapy for bone metastasis.
The evolution was marked by a drop in the PSA level to 65 ng/ml after one year and 3 months. Five months later, the patient's follow-up was marked by his death.
Discussion
The secondary cerebral localization of prostatic adenocarcinoma is exceptional, while the lymph node and bone involvement remains the most common.
Cerebral metastases are secondary to either hematogenous dissemination or contiguity of a bony location of the skull.1 In the CHUNG et al. series, cerebral metastases of prostate ADK represent only 0.6% of cases. Usually, these metastases are only discovered postmortem.2
In our patient, the cerebral localization would be secondary to the metastasis localized in the skull found on bone scan and brain MRI.
The clinical symptomatology is variable depending on the intra-parenchymal location and may manifest itself as agitation, confusion, decreased visual acuity, jet vomiting, and headaches grouped in the intracranial hypertension syndrome, which was found in our patient.
MRI is the main paraclinical examination to look for metastatic brain localization, while stereotactic biopsy allows us to have a histological confirmation. In our case, the patient was operated for a meningioma and an immunohistochemical study was completed which was in favor of a cerebral metastasis of a prostatic ADK.3
Management is based on corticosteroids and diuretics to treat intracranial hypertension and analgesics for diffuse bone pain. The etiological treatment is based on androgen blockade combined with cerebral radiotherapy.4
In the case of a single accessible metastasis, surgery can be indicated and improves the median survival.
A retrospective study on brain metastases of all tumors, carried out by HALL, found that brain metastases secondary to prostatic ADK and bladder tumors had a poor prognosis, with a median survival rate lower than that of other metastatic tumors.5
Conclusion
Cerebral metastases secondary to prostate cancer pose a diagnostic problem with primary brain tumors. The clinical picture shows signs of neurological appeal and MRI allows the diagnosis to be suspected. These are generally of poor prognosis; their treatment is based on androgen deprivation and radiotherapy.
Declaration of competing interest
The authors state that they do not have competing interests.
Acknowledgments
We thank Dr. Jihane El Habnouny for this contribution in writing and editing the article.
Abbreviation
- PS
Performance status
- CT
computed tomography
- PSA
prostate-specific antigen
- MRI
Magnetic Resonance Imaging
Ethical approval and consent to participate
Not available.
Consent to publication
The consent to publish this information was obtained from study participants. We confirm that written proof of consent to publish study participants are available when requested and at any time.
Availability of data and material
The datasets in this article are available in the repository of the urology database, Chu Ibn-Rochd Casablanca, upon request, from the corresponding author.
Funding
Not applicable.
Author's contributions
Dr. IJ, Dr. Dr. YL and Dr. AM analysed and performed the literature research, Pr. MD, Pr. AD, Pr. RA performed the examination and performed the scientific validation of the manuscript. Issam Jandou was the major contributors to the writing of the manuscript. All authors read and approved the manuscript.
References
- 1.Ameur A., Touiti D., El Mostarchid B., El Alami M., Jira H., Abbar M. Métastase cérébrale D'UN cancer de La prostate : régression sous traitement hormona. Prog Urol. 2001;11:1298–1301. [PubMed] [Google Scholar]
- 2.Capito P.R., Wang H., Brem H., Ahn H.S., Bryan R.N. Magnetic resonance imaging diagnosis of an intracranial metastasis of adenocarcinoma of the prostate : case report. Md Med J. 1991;40:113–115. [PubMed] [Google Scholar]
- 3.Chang D.S., Hwang S.L., Howng S.L., Chai C.Y. Prostatic carconoma with brain metastatis presenting as a tumor hemorrhage. Kao Hsiung I. Hsueh. Tsa Chih. 1998;14:247–250. [PubMed] [Google Scholar]
- 4.Gupta A., Baidas S., Cumberlin R.K. Brain stem metastasis as the only site of spread in prostate carcinome : a case report. Cancer. 1994;74:2516–2519. doi: 10.1002/1097-0142(19941101)74:9<2516::aid-cncr2820740920>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 5.Mseddi M.A., Bouassida M., Chaabouni A. Mhiri Métastase orbitaire d’un adénocarcinome prostatique: à propos d’un cas.Service d’urologie. CHU Habib Bourguiba. Sfax Tunisie. Afr J Urol. 2014 doi: 10.1016/j.afju.2014.03.036. [DOI] [Google Scholar]