Abstract
Purpose:
The aim of this study is to describe the demographics and clinical profile of patients with ocular disorders presenting during the novel coronavirus (COVID-19) lockdown in India.
Methods:
This cross-sectional hospital-based study included patients presenting between March 23, 2020 and April 19, 2020. All patients who presented to the emergency department were included as cases. The data were collected using an electronic medical record system.
Results:
Overall, 1,192 patients (mean 42.57 per day) presented to the ocular emergency department and were included for analysis. The median age of the patients was 35 (Interquartile range, IQR: 20-52) years and they were mostly adults (77.85%). The majority of patients were male (62.16%) and presented from the local metropolitan region (56.21%). On triaging based on the ocular disorders at presentation, the majority of the patients were emergency related (65.02%), followed by urgent (8.14%) and routine (26.85%) in nature. The most common emergencies were microbial keratitis (23.74%), followed by corneal trauma (16.39%). There was an increasing trend seen in emergency patients (46.11%; week 1 to 71.78%; week 4) and a decreasing trend seen in routine patients (45%; week1 to 21.20%; week 4). A subset of patients (23.49%) underwent surgery where indicated and the most commonly performed procedures were vitreo-retinal procedures (32.86%) followed by trauma related (31.43%).
Conclusion:
The enforcement of the nationwide lockdown due to COVID-19 resulted in a fewer patients presenting to the hospital. The majority of them presented from the local metropolitan region and the common emergencies were microbial keratitis and corneal trauma. About one fourth required a surgical intervention which was most commonly a vitreo-retinal procedure.
Keywords: COVID-19, electronic medical records, eye care, India, SARS-CoV-2
The ongoing novel coronavirus (COVID-19) pandemic is shaping the world on an unprecedented scale affecting more than 2.7 million individuals.[1] The risk of transmission of the severe acute respiratory syndrome (SARS-CoV-2) virus has enforced strict protocols the world over with nationwide lockdown of populations in the hope of flattening the curve of COVID-19 cases. About a third of the world's population is estimated to be under some form of restriction. However, this is a constantly changing dynamic based on the current state of positive cases in that region.[2] India went into one of the largest lockdowns in the entire world from March 23rd 2020 with 1.3 billion people told to stay indoors for 21 days to halt the spread of the virus.[3] The implementation of social distancing to prevent community transmission has brought in new challenges for patients accessing health care services both due to the lockdown and the lack of access to transport to access the same. Relevant guidelines for providing clinical care to the patients are constantly evolving across different specialties in health care.[4,5,6] Emergency eye care is of utmost importance and must be provided to all patients in need. The imposed lockdown restrictions leading to decreased access to care due to the unfortunate circumstances of the pandemic only compounds the problem. Practice guidelines to consider during the lockdown period for ophthalmologists include triaging of patients to cater to emergencies, modified patient flow in the outpatient department and operation room, use of personal protective equipment, infection control, and management of manpower, among others.[7] The use of triaging systems helps to balance the delivery of eye care services while decreasing the risk of possible exposure. The authors describe their experience of the demographic and clinical profile of patients with ocular disorders who presented to the center of excellence of a large multi-tier ophthalmology network in India during the COVID-19 lockdown.
Methods
Study design, period, location and approval
This cross-sectional observational hospital-based study included all patients presenting between March 23, 2020 and April 19, 2020 to the center of excellence of a multi-tier ophthalmology network located in India.[8] A standard consent form for electronic data privacy was signed by the patient or the parents or guardians of the patient at the time of registration. None of the identifiable parameters of the patient information were used for analysis of the data. The study adhered to the Declaration of Helsinki and was approved by the Institutional Ethics Committee. The clinical data of each patient who underwent a comprehensive ophthalmic examination was entered into a browser-based electronic medical records system (eyeSmart EMR) using a standardized template by trained ophthalmic personnel and supervised by an ophthalmologist.[9]
Data retrieval and processing
A total of 1,192 patients of all ages presented to the center of excellence of the network during the study period and were included in this study. The data of these patients were retrieved from the electronic medical record database and segregated in a single excel sheet (Microsoft Excel®). Data on patient demographics, clinical presentation, ocular diagnosis and treatment modalities were used for analysis. The Excel sheet with the required data was then used for analysis using the appropriate statistical software. Standardized definitions were used for occupation, socio-economic status and geographic distribution.[10] The visual acuity was classified according to the WHO guidelines.[11] The ocular disorders of the patients were segregated into emergency, urgent and routine categories based on the published AIOS-IJO guidelines for India during the COVID-19 pandemic.[7] According to these guidelines, the urgency is determined by the ophthalmologist's judgment of the potential risk to vision, eye and life and impact on the quality of life if untreated, and also considered the age of the patient, disease laterality, geographic location, feasibility of follow-up and financial status for the triage classification. The preceding four weeks from February 24, 2020 to March 22, 2020 was considered as the pre-lockdown period and the demographic details of the 24,342 patients presenting during this time was used for comparative analysis.
Statistical analysis
Descriptive statistics using mean ± standard deviation and median with inter-quartile range (IQR) were used to elucidate the demographic and clinical data using Microsoft Excel 2019 (Microsoft Corporation, Redmond, USA).
Results
Overall, 1,192 patients presented during the study period and 912 (76.51%) were treated in the outpatient department and 280 (23.49%) underwent a surgical procedure. A total of 148 (12.42%) patients were referred to the center of excellence for further evaluation and management. The mean number of patients seen per day was 42.57 (1,192/28). This was significantly lower than the mean number of 869.35 (24,342/28) patients seen per day in the pre-lockdown period.
Age
The mean age of the patients was 35 ± 21.16 years while the median age was 35 (IQR: 20-52) years. There were 262 (22.15%) patients who were children (≤16 years) and 928 (77.85%) were adults. The most common age group at presentation was between 31-40 years with 242 (20.3%) patients. The adult: pediatric ratio was 3.54:1, as compared to 4.42:1 during the pre-lockdown period.
Gender
There were 741 (62.16%) male and 451 (37.84%) female patients. Among them, the mean and median age were 35.56 ± 20.3 and 37 (IQR: 21 to 50) years for men and 34.07 ± 22.43 and 34 (IQR: 12.5 to 55) years for women, respectively. The majority of the patients presenting to the outpatient department (60.96%; 556/912) and who underwent a surgical procedure (66.07%; 185/280) were male. The male: female ratio was 1.64:1 as compared to 1.4:1 during the pre-lockdown period.
Rural-urban-metropolitan distribution
There were 497 (41.69%) patients from the metropolitan region, 361 (30.29%) from rural districts and 334 (28.02%) from urban districts. Majority of the patients presenting to the outpatient department were from the metropolitan region (46.16%; 421/912) and who underwent a surgical procedure were from the rural districts (40.71%; 114/280). In contrast during the pre-lockdown period, there were 8,967 (36.84%) patients from the rural districts, 7,976 (32.77%) from urban districts and 7,399 (30.40%) from the metropolitan region.
Geographic distance and time of presentation
There were 670 (56.21%) patients from the local metropolitan region, 406 (34.06%) patients from the range of 50-250 kms and 84 (7.05%) patients from 250-750 kms and a minor subset of 32 (2.68%) patients from > 750 kms. The majority of the patients presenting to the outpatient department were from the local metropolitan region (61.18%; 558/912) and who underwent a surgical procedure were from the range of 50-250 kms (49.64%; 139/280). A significant proportion of 1,171 (98.24%) patients presented during the day (7 AM-7 PM) and a minority of 21 (1.76%) patients came during the night (7 PM-7 AM).
Socio-economic status
There were 326 (27.35%) patients from the lower socio-economic class, 825 (69.21%) from the lower middle class, 18 (1.51%) from the upper middle class and 23 (1.93%) from the upper class. The majority of the patients presenting to the outpatient department (72.59%; 662/912) and who underwent a surgical procedure (58.21%; 163/280) were from the lower middle class. In contrast during the pre-lockdown period, there were 6,739 (27.68%) patients from the lower socio-economic class, 15,952 (65.53%) from the lower middle class, 855 (3.51%) from the upper middle class and 796 (3.27%) from the upper class.
Occupation
Of the 1,192 patients, 348 (29.19%) were professionals; 227 (19.04%) were homemakers; 213 (17.87%) were students; 126 (10.57%) were agriculture related; 90 (7.55%) were manual laborers; 52 (4.36%) were retired; and in the remaining 136 (11.41%) the occupational category was not applicable. The majority of the patients presenting to the outpatient department (30.92%; 282/912) and who underwent a surgical procedure (23.57%; 66/280) were professionals.
Emergency patients
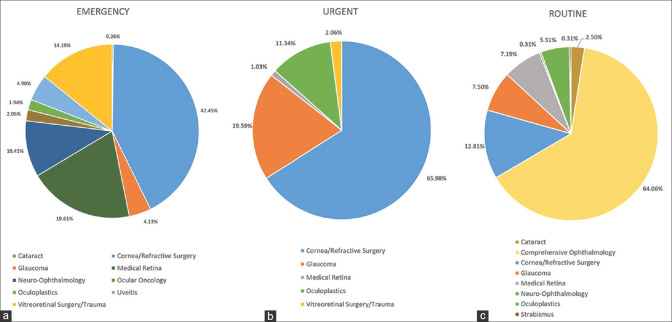
There were 775 (65.02%) patients who were triaged as an emergency. The most common ocular disorder was microbial keratitis in 184 (23.74%) patients, followed by corneal trauma in 127 (16.39%) and retinopathy of prematurity (ROP) screening in 69 (8.9%). The majority of patients were male (64%; 496/775), had unilateral affliction (77.03%; 597/775), visual impairment between > 20/400 to 20/1200 (26.32%; 204/775) and presented from the rural districts (36.13%; 280/775). There was an increase of emergency patients by 40.28% as compared to pre-lockdown period (24.74%). The detailed list of ocular disorders triaged as emergency are listed in Table 1 and depicted in Fig. 1a.
Table 1.
Distribution of the ocular disorders triaged as emergency category
| Emergency | n | % |
|---|---|---|
| Cataract | 2 | 0.26% |
| Traumatic Cataract | 2 | 0.26% |
| Cornea/Refractive Surgery | 329 | 42.45% |
| Microbial Keratitis | 184 | 23.74% |
| Corneal Trauma | 127 | 16.39% |
| Viral Keratitis | 6 | 0.77% |
| Steven Johnson Syndrome | 6 | 0.77% |
| Corneal Graft Rejection | 5 | 0.65% |
| Corneal Hydrops | 1 | 0.13% |
| Glaucoma | 32 | 4.13% |
| Phacomorphic Glaucoma | 17 | 2.19% |
| IOP >40 mm Hg | 10 | 1.29% |
| Acute Angle Closure | 4 | 0.52% |
| Primary Congenital Glaucoma | 1 | 0.13% |
| Medical Retina | 152 | 19.61% |
| ROP Screening | 69 | 8.90% |
| Proliferative Diabetic Retinopathy | 40 | 5.16% |
| Retinal Vein Occlusion | 14 | 1.81% |
| Central Retinal Artery Occlusion | 9 | 1.16% |
| Choroidal Neovascular Membrane | 5 | 0.65% |
| CMV Retinitis | 5 | 0.65% |
| Posterior Uveitis | 5 | 0.65% |
| Panophthalmitis | 4 | 0.52% |
| Retinitis | 1 | 0.13% |
| Neuro-Ophthalmology | 81 | 10.45% |
| Optic Neuritis | 25 | 3.23% |
| Papilledema | 18 | 2.32% |
| Neurological Diplopia | 14 | 1.81% |
| Retrobulbar Neuritis | 6 | 0.77% |
| Non-arteritic Ischaemic Optic Neuropathy | 6 | 0.77% |
| TRON | 5 | 0.65% |
| Acquired Nystagmus | 2 | 0.26% |
| Internuclear Ophthalmoplegia | 1 | 0.13% |
| Cerebral Sinus Venous Thrombosis | 1 | 0.13% |
| Total External Ophthalmoplegia | 1 | 0.13% |
| Homonymous Hemianopia | 1 | 0.13% |
| Hydrocephalus with Colloid Cyst | 1 | 0.13% |
| Ocular Oncology | 16 | 2.06% |
| Retinoblastoma | 16 | 2.06% |
| Oculoplastics | 15 | 1.94% |
| Eyelid Laceration | 10 | 1.29% |
| Orbital Cellulitis | 3 | 0.39% |
| Severe Thyroid Eye Disease | 1 | 0.13% |
| Orbital Fracture | 1 | 0.13% |
| Uveitis | 38 | 4.90% |
| Acute Anterior Uveitis | 34 | 4.39% |
| Intermediate Uveitis | 4 | 0.52% |
| Vitreoretinal Surgery/Trauma | 110 | 14.19% |
| Retinal Detachment | 44 | 5.68% |
| S/p Vitreo Retinal Surgery | 40 | 5.16% |
| Acute Endophthalmitis | 23 | 2.97% |
| Dislocated IOL | 3 | 0.39% |
| Grand Total | 775 | 65.02% |
Figure 1.
Clinical distribution of triage categories during the COVID-19 lockdown in India. Cornea/Refractive Surgery accounted for the highest number of cases in emergency (1a; 42.45%) and urgent (1b; 65.98%) cases while Comprehensive Ophthalmology was highest among routine (1c; 64.06%) cases
Urgent patients
There were 97 (8.14%) patients who were triaged as urgent. The most common ocular disorder was corneal foreign body in 24 (24.74%) patients, followed by corneal abrasion in 18 (18.56%) and closed globe injury in 17 (17.53%). The majority of patients were male (64.94%; 63/97), had unilateral affliction (82.47%; 80/97); visual impairment of <20/70 (48.45%; 47/97) and presented from the metropolitan region (53.6%; 52/97). There was a decrease of urgent patients by 8.95%, as compared to pre-lockdown period (17.09%). The detailed list of ocular disorders triaged as urgent are listed in Table 2 and depicted in Fig. 1b.
Table 2.
Distribution of the ocular disorders triaged as Urgent category
| Urgent | n | % |
|---|---|---|
| Cornea/Refractive Surgery | 64 | 65.98% |
| Corneal Foreign Body | 24 | 24.74% |
| Corneal Abrasion | 18 | 18.56% |
| Closed Globe Injury | 17 | 17.53% |
| Herpes Zoster Ophthalmicus | 5 | 5.15% |
| Glaucoma | 19 | 19.59% |
| IOP >30 mm Hg | 12 | 12.37% |
| Secondary Glaucoma | 7 | 7.22% |
| Medical Retina | 1 | 1.03% |
| Familial Exudative Vitreo-Retinopathy | 1 | 1.03% |
| Oculoplastics | 11 | 11.34% |
| Proptosis | 6 | 6.19% |
| Acute Dacryocystitis | 3 | 3.09% |
| Preseptal Cellulitis | 1 | 1.03% |
| Facial Cellulitis | 1 | 1.03% |
| Vitreoretinal Surgery/Trauma | 2 | 2.06% |
| Subhyaloid Haemorrhage | 1 | 1.03% |
| Horse Shoe Tear | 1 | 1.03% |
| Grand Total | 97 | 100.00% |
Routine patients
There were 320 (26.85%) patients who were triaged as routine. The most common ocular disorder was conjunctivitis in 76 (23.75%) patients, followed by postoperative follow-up in 64 (20%) and allergic conjunctivitis in 21 (6.56%). The majority of patients were male (56.87%; 182/320), had unilateral affliction (70.31%; 225/320); visual impairment of <20/70 (55%; 176/320) and presented from the metropolitan region (54.37%; 174/320). There was a decrease of routine patients by 31.32% as compared to pre-lockdown period (58.17%). The detailed list of ocular disorders triaged as routine are listed in Table 3 and depicted in Fig. 1c.
Table 3.
Distribution of the ocular disorders triaged as Routine category
| Routine | n | % |
|---|---|---|
| Cataract | 8 | 2.50% |
| Total Cataract | 8 | 2.50% |
| Comprehensive Ophthalmology | 205 | 64.06% |
| Conjunctivitis | 76 | 23.75% |
| Post-operative Visit | 64 | 20.00% |
| Allergic Conjunctivitis | 21 | 6.56% |
| Episcleritis | 11 | 3.44% |
| Internal Hordeolum | 9 | 2.81% |
| Migraine | 6 | 1.88% |
| Subconjunctival Haemorrhage | 5 | 1.56% |
| Scleritis | 3 | 0.94% |
| Aphakia | 3 | 0.94% |
| Flashes/Floaters | 3 | 0.94% |
| Microphthalmos | 2 | 0.63% |
| Coloboma | 1 | 0.31% |
| Episcleritis | 1 | 0.31% |
| Cornea/Refractive Surgery | 41 | 12.81% |
| S/p PRK | 13 | 4.06% |
| Keratoconus | 7 | 2.19% |
| Phlyctenular Keratoconjunctivitis | 4 | 1.25% |
| S/p PK | 4 | 1.25% |
| S/p LASIK | 2 | 0.63% |
| Severe Dry Eye | 2 | 0.63% |
| Adherent Leucoma | 2 | 0.63% |
| Keratoglobus | 1 | 0.31% |
| Sclerocornea | 1 | 0.31% |
| Contact Lens User | 1 | 0.31% |
| Corneal Scar | 1 | 0.31% |
| Peters Anomaly | 1 | 0.31% |
| Anterior Staphyloma | 1 | 0.31% |
| Pseudophakic Bullous Keratopathy | 1 | 0.31% |
| Glaucoma | 24 | 7.50% |
| PACG | 13 | 4.06% |
| POAG | 8 | 2.50% |
| JOAG | 3 | 0.94% |
| Medical Retina | 23 | 7.19% |
| Choroiditis | 8 | 2.50% |
| Hypertensive Retinopathy | 4 | 1.25% |
| Lattice Degeneration | 3 | 0.94% |
| Central Serous Chorioretinopathy | 3 | 0.94% |
| Coats Retinopathy | 1 | 0.31% |
| Chorioretinitis | 1 | 0.31% |
| Vasculitis | 1 | 0.31% |
| Choroideremia | 1 | 0.31% |
| Idiopathic Polypoidal Choroidal Vasculopathy | 1 | 0.31% |
| Neuro-Ophthalmology | 1 | 0.31% |
| Optic Atrophy | 1 | 0.31% |
| Oculoplastics | 17 | 5.31% |
| PANDO | 11 | 3.44% |
| CNLDO | 3 | 0.94% |
| Ptosis | 1 | 0.31% |
| Conjunctival Granuloma | 1 | 0.31% |
| Orbital Myositis | 1 | 0.31% |
| Strabismus | 1 | 0.31% |
| Esotropia | 1 | 0.31% |
| Grand Total | 320 | 100.00% |
Surgical management
The most common surgical procedures were related to vitreo-retinal in 92 (32.86%) patients, trauma like corneal/scleral/eyelid tear repair in 88 (31.43%), cornea and anterior segment in 37 (13.21%), cataract extraction in 16 (5.71%), examination under anesthesia in 14 (5%), oculoplastic procedures like evisceration/enucleation/orbitotomy in 11 (3.93%) and therapeutic keratoplasty in 9 (3.21%) patients. ROP Laser was performed in 13 (4.64%) patients. Among the 92 vitreo-retinal procedures, the most common was retinal detachment surgery in 44 (47.83%) patients, endophthalmitis related in 23 (25%) patients and intraocular anti-VEGF injection were given in 18 (19.57%) patients.
Weekly trends
In the 4 week period, the number of patients was 180 (15.10%) in week 1 from March 23rd-March 29th, 193 (16.19%) in week 2 from March 30th-April 5th, 121 (10.15%) in week 3 from April 6th-April 12th and 698 (58.56%) in week 4 from April 13th-April 19th as depicted in Fig. 2. There was increasing trend seen in emergency patients (46.11%; week 1 to 71.78%; week 4) and a decreasing trend seen in routine patients (45%; week 1 to 21.20%; week 4). A description of the various triage categories and their trend over the 4 weeks is detailed in Fig. 3. A comparison of all the parameters between the pre-lockdown and lockdown period is detailed in Table 4.
Figure 2.
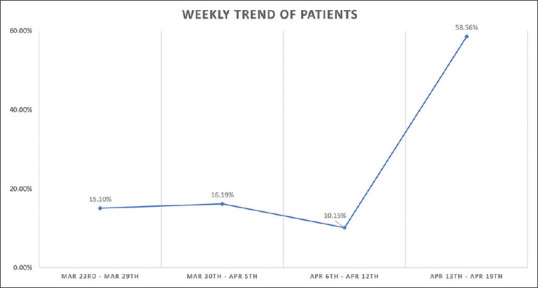
Weekly distribution of patients with ocular disorders presenting during the COVID-19 lockdown in India. The number of patients steadily decreased to a minimum of (10.15%) in week 3 and increased to (58.56%) in week 4
Figure 3.
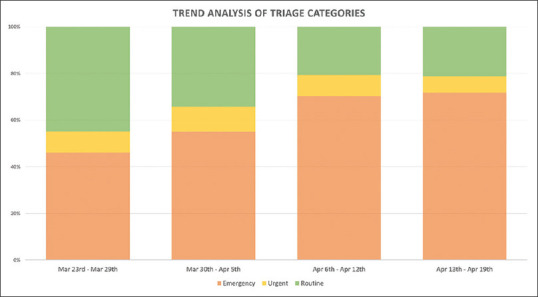
Weekly trends of triage categories during the COVID-19 lockdown in India. There was increasing trend seen in emergency patients (46.11%; week 1 to 71.78%; week 4) and a decreasing trend seen in routine patients (45%; week1 to 21.20%; week 4)
Table 4.
Comparison of patient profile between pre-lockdown and lockdown period
| Parameter | Pre-Lockdown* | Lockdown* | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Male | 14236 | 58.48% | 741 | 62.16% | 0.203001 |
| Female | 10106 | 41.52% | 451 | 37.84% | 0.100424 |
| Adult | 19853 | 81.56% | 928 | 77.85% | 0.299285 |
| Paediatric | 4489 | 18.44% | 264 | 22.15% | 0.00874 |
| Urban | 7976 | 32.77% | 334 | 28.02% | 0.013262 |
| Rural | 8967 | 36.84% | 361 | 30.29% | 0.001384 |
| Metropolitan | 7399 | 30.40% | 497 | 41.69% | <0.00001 |
| Higher SES* | 17603 | 72.32% | 866 | 72.65% | 0.919344 |
| Lower SES* | 6739 | 27.68% | 326 | 27.35% | 0.848832 |
| Emergency | 6023 | 24.74% | 775 | 65.02% | <0.00001 |
| Urgent | 4159 | 17.09% | 97 | 8.14% | <0.00001 |
| Routine | 14160 | 58.17% | 320 | 26.85% | <0.00001 |
| Total Patients | 24342 | 1192 | |||
*SES - Socio Economic Status. *Pre Lockdown - Feb 24th - Mar 22nd, 2020. *Lockdown - Mar 23rd - Apr 19th, 2020
Discussion
This study sought to describe the demographics and clinical profile of patients with ocular disorders presenting during the novel coronavirus (COVID-19) lockdown in India. The findings of this study suggest that the increased enforcement of the social distancing measures resulted in a decreased footfall of patients to the hospital. The patients were predominantly males and adults. They presented more commonly from the local metropolitan region and surrounding locations due to the travel restriction of the lockdown. On triaging the ocular disorders at presentation based on national guidelines, the majority were emergency related and were due to microbial keratitis followed by corneal trauma. About one fourth of the patients were routine cases and could have been managed by tele-consults where relevant. One fourth of the patients underwent a surgical procedure which was most commonly related to the vitreo-retina.
There are many important socio-determinants of health that need to be identified among the vulnerable groups such as children, elderly, women, lower socioeconomic strata of patients and residence in a geography with limited access to care.[12] In our study, we found the vulnerable groups to access care in this time of crisis were female gender (37.84%), pediatric age of ≤16 years (22.15%), elderly of ≥60 years (12.25%), lower socioeconomic strata (27.35%) and living in a location away of ≥250 kms from the point of care (9.73%). This lends insight into how we may be better prepared to ensure equitable care to these vulnerable groups in the event of challenges such as nationwide lockdowns. These vulnerable sections must be approached proactively to ensure we take care of the individuals that might be in need of eye care services. Our study highlights the disparity in the access to care in emergency situations and reinforces the need to provide equitable access to all those in need. The distance also was a limiting factor to travel to the center of excellence as the travel restrictions were imposed as the lockdown progressed. The government of India suspended both air, train and bus travel across the nation brining to halt air services that catered to 13 million passengers a month, the Indian Railways running 13,500 passenger trains a day and all local transport bus services till March 31st, 2020.[13] This did have an impact on the patient footfall as it reached the lowest in the third week (10.15%). However, we did a surge in patients in the fourth week (58.56%) possibly because of increasing need for care and the local government also allowed patients to visit the hospitals for emergency care as per the need. The decreasing trend of the patients from the local metropolitan region would have possibly been to an understanding of the patients to go to the hospital only in the event of emergency care. This was evident by the increasing trend of the emergency patients and the decreasing trend of the routine patients seen from the first week to the fourth week during the study period.
The majority of the patients also presented to the hospital due ocular disorders that were triaged as emergency (65.02%) or urgent (8.14%). About one-fourth of the patients were routine (26.85%) cases. In our experience of one month of a nationwide lockdown, we have found ocular infections and ocular trauma to be the most common emergency causes presenting to the hospital for care. ROP screening and ocular oncology cases were also catered to during the lockdown period. About one-fourth underwent a surgical procedure and the most common surgical procedures were related to vitreo-retina followed by trauma. National published guidelines serve as a very important measure to have clarity in triaging patients in times of crisis such as this.[7] There is a similar guideline published for Ophthalmology from experience from the epicenter of the COVID-19 outbreak in Europe from the city of Bergamo.[14] It is very important to balance the provision of patient care services and minimize the risk of exposure to the hospital staff from suspected COVID-19 positive patients. Analysis of the electronic medical records of the current distribution of patients presenting with various ocular disorders lends valuable insight to strategize the plan for future eye care services. We will be able to allocate the right amount of resources both in the outpatient department and operation rooms based on the nature of the patients. In our hospital, we sized down our clinical and non-clinical support staff into 3 teams that rotated twice a week and continued to provide care to all the patients presenting to the hospital during the lock down period. There should be every effort made possible to minimize the hospital visits of the routine non-emergency patients till the stabilization of the COVID-19 crisis and the use of telemedicine protocol is encouraged by eye care institutions to continue to provide timely advice to our patients.[15] The authors also have described their experience of providing teleconsultations to the patients calling the hospital during the lock down period and have managed the care through remote consults with access to the clinical history of the patient through electronic medical records system.[16] This has enabled an effective triage system to identify the patients with an emergency who were asked to report to the hospital immediately and also manage the post-operative patients who required advise about the use of medications and minor ocular symptoms among follow-up patients.
In this unprecedented time of change, where we are challenged to adapt to the delivery of eye care services to our patients, we need to utilize insights from data and base our decisions and strategy on the same. With the modification of guidelines of the lockdown and the possibility of multiple cycles of the same being brought into force based on the current scenario, it is important to follow standard triaging protocols for eye care. This will enable the provision of excellent, equitable and efficient eye care to all those in need in the time of the COVID-19 crisis.
Conclusion
In conclusion, the authors present their experience in the management of patients with ocular disorders presenting to the center of excellence of a multi-tier ophthalmology network in India during the COVID-19 lockdown period. An understanding of the demographic and clinical profile of the patients helps to plan our resources better after the lockdown as we all prepare to adapt to a new way of eye care delivery in the days to come, safe guarding the health of our patients and also our care givers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–4. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Business Insider [Internet]. c2020 [Cited 2020 Apr 24] Available from: https://www.businessinsider.com/countries-on-lockdown-coronavirus-italy-2020-3?r=DE&IR=T .
- 3.Prime Minister India [Internet] c2020. Cited 2020 Apr 24. Available from: https://wwwpmindiagovin/en/news_updates/pm-calls-for-complete-lockdown-of-entire-nation-for-21-days/
- 4.Kowalski LP, Sanabria A, Ridge JA, Ng WT, de Bree R, Rinaldo A, et al. COVID-19 pandemic: Effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020;42:1259–67. doi: 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mak ST, Yuen HK. Oculoplastic surgery practice during the COVID-19 novel coronavirus pandemic: Experience sharing from Hong. Kong Orbit. 2020:1–3. doi: 10.1080/01676830.2020.1754435. doi: 101080/0167683020201754435. [DOI] [PubMed] [Google Scholar]
- 7.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society-Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rao GN, Khanna RC, Athota SM, Rajshekar V, Rani PK. Integrated model of primary and secondary eye care for underserved rural areas: The L V Prasad Eye Institute experience. Indian J Ophthalmol. 2012;60:396–400. doi: 10.4103/0301-4738.100533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das AV, Kammari P, Vadapalli R, Basu S. Big data and the eyeSmart electronic medical record system-An 8-year experience from a three-tier eye care network in India. Indian J Ophthalmol. 2020;68:427–32. doi: 10.4103/ijo.IJO_710_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Das AV, Podila S, Prashanthi GS, Basu S. Clinical profile of pterygium in patients seeking eye care in India: Electronic medical records-driven big data analytics report III. Int Ophthalmol. 2020;40:1553–63. doi: 10.1007/s10792-020-01326-3. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization [Internet] Change the Definition of Blindness. c2008. Cited 2020 Apr 24. Available from: th e%20Definition%20of%20Blindnesspdf">https://wwwwhoint/blindness/Change%20th e%20Definition%20of%20Blindnesspdf .
- 12.Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P Consortium for the European Review of Social Determinants of Health and the Health Divide. WHO European review of social determinants of health and the health divide. Lancet. 2012;380:1011–29. doi: 10.1016/S0140-6736(12)61228-8. [DOI] [PubMed] [Google Scholar]
- 13.Live Mint [Internet] c2020. Cited 2020 Apr 25. Available from: https://wwwlivemintcom/news/india/coronavirus-impact-centre-suspends-train-metro-bus-services- till-31-march-11584875782117html .
- 14.Romano MR, Montericcio A, Montalbano C, Raimondi R, Allegrini D, Ricciardelli G, et al. Facing COVID-19 in Ophthalmology Department. Curr Eye Res. 2020;45:653–8. doi: 10.1080/02713683.2020.1752737. [DOI] [PubMed] [Google Scholar]
- 15.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A call to action. JMIR Public Health Surveill. 2020;6:e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Das AV, Rani PK, Vaddavalli PK. Tele-consultations and electronic medical records driven remote patient care: Responding to the COVID-19 lockdown in India. Indian J Ophthalmol. 2020;68:1007–12. doi: 10.4103/ijo.IJO_1089_20. [DOI] [PMC free article] [PubMed] [Google Scholar]