Abstract
Purpose:
To assess the perspectives of physicians in general and ophthalmologists in particular about restarting elective out-patient (OP) and operating (OT) services after relaxation of lockdown for COVID-19.
Methods:
An online survey, containing 31 questions, was conducted among medical doctors using a secure Google forms link. The survey was open for 48 hours from 16th-18th April 2020.
Results:
Responses were received from 556 physicians (including 266 ophthalmologists). About a third (n = 205) wanted to start OP immediately after lockdown. In OP, mask of any kind for patient (60.8%), 3-ply for assistants (52.7%) and N95 for doctors (72.7%) were most common preferences. In OP, 31.5% and 46.6% felt full PPE and gloves alone were sufficient respectively. Ophthalmologists were more likely to start immediately after lockdown compared to other specialists (P = 0.004). Among 299 surgeons, an almost equal number (27%) wanted to start routine OT services immediately and 2 weeks post lockdown. A large majority (76.9%) would mandate COVID-19 tests before elective surgeries. In OT, 34.1% wanted N95 for surgical team and 3-ply for patient, 23.4% wanted 3-ply masks for everyone. 40.5% felt additional personal protective equipment (PPE) is not required and 33.1% felt that full PPE is required for everyone in OT. Ophthalmic surgeons preferred 3-ply masks and were less inclined to use full PPE (P < 0.001).
Conclusion:
Perspectives of doctors vary, especially with regarding to timing of restarting services and precautions to be taken in the OT. Ophthalmologists may tend to err on the side of taking lesser stringent precautions when restarting services post lockdown.
Keywords: Corona virus, COVID-19, elective surgery, physician perspectives, restarting services, survey
The COVID-19 pandemic has led to an unprecedented health care crisis and crippled normal life, as we know it. India, with a population of 1.3 billion, leads the list of countries where movement of people has been restricted as a precautionary measure.[1] COVID-19, that stands for coronavirus disease 2019, was suggested by World Health Organization (WHO).[2] The enveloped single stranded RNA virus, officially called the 'Severe Acute Respiratory Syndrome Corona Virus 2' (SARS-CoV-2), has not been previously identified in humans.[3] Therefore, much of our knowledge about the properties of this pathogen is derived from other coronaviruses.[4] Knowledge is rapidly evolving and modalities to combat its transmission are constantly being updated by governments and scientific societies.[5,6,7]
A recent survey amongst Indian ophthalmologists done during the existing lockdown showed that majority were either not seeing patients at all or were seeing only emergencies while elective surgeries were postponed indefinitely.[8] In the absence of concrete guidelines, consensus statements have been issued by scientific bodies for various medical specialties.[4,6,9,10,11] Yet, it is unclear how practices will be affected when the lockdown is eased and how doctors will adopt these guidelines in their own settings to restart their out-patient (OP) and routine operating (OT) services. In this survey, we endeavored to assess doctors' perspectives about restarting their services after lifting of government-mandated lockdown and practice patterns they intend to follow with information available to them to ensure protection of patients and providers.
Methods
An online survey questionnaire was developed by the authors and assessed for its validity, question formation and options for each item by peer discussions and by piloting it amongst 5 peers. Before recruitment, participants were informed about the length of the study, its duration and purpose. For those who took the survey, consent was implied.
The electronic survey [Annexure 1] was hosted on Google forms platform. The survey was open for 48 hours from 16th to 18th April 2020, corresponding to the 25th day of lockdown in India. All participants were mandated to answer 19 questions. Further, 7 questions were mandated to be answered by surgeons alone. Finally, ophthalmologists were asked 5 additional questions before submission.
Chi-square test was used to estimate association between categorical variables. A P < 0.05 was considered statistically significant. Bonferroni correction with standardized residuals was applied where necessary. All statistical analysis was performed using SPSS 23 (SPSS Inc., Chicago, IL, USA).
Results
The study included responses from 556 physicians, of whom 266 (48%) were ophthalmologists. Most were in the age group of 31-40 years (n = 248, 44.6%) followed by those between 41-50 years (n = 174, 31.3%). About two-third of the responders were male (n = 377, 67.8%). In descending order, the commonest type of practice was private single practitioner (n = 226, 40.6%), corporate chain (n = 108, 19.4%), private group practitioners (n = 83, 14.9%), government (n = 75, 13.5%) and non-governmental institutes (n = 64, 11.5%). 326 (58.6%) participants had stopped all forms of medical service since implementation of lockdown.
Perspectives about non-emergency OP services
Immediately after lockdown, 205 (36.9%) participants wanted to resume their regular OP. An additional 98 (17.6%) participants responded that routine OP services were currently running at the time of this survey and 79 (14.2%) clinicians wanted to delay the start of OP for 2 weeks after lockdown ends. Of the remaining, 78 (14%) and 39 (7%) wanted to start OP 2 weeks and 1 month after no new cases were reported respectively in their locality. Majority of doctors wanted to divide their staff into 2 batches working on alternate weeks (n = 241, 43.3%) while 112 (20.1%) doctors did not prefer any change in schedule for their staff and 97 (17.4%) preferred to divide their staff into 3 batches to report once in 3 weeks.
To ensure social distancing in the OP, the preferred choices were placing chairs apart (n = 464, 83.5%), allowing only one attender (n = 445, 80%), restricting OP hours (n = 353, 63.5%), history taking over telephone (n = 244, 43.9%) and seeing patients only with prior appointment (n = 215, 38.6%). A majority (n = 454, 81.7%) would prefer to postpone OP consultation for a non-emergency case if the patient was from a government declared “hot-spot” and 371 (66.7%) planned to have a triage facility that screens patients before being seen by the primary clinician. Additionally, 449 (80.8%) doctors were in favor of having a declaration from the patient regarding possibility of COVID-19 transmission from the health care facility and 366 (65.8%) doctors planned to insist on online non-contact payment methods such as BHIM, Google Pay, Paytm etc. to avoid cash or card transfer between individuals. RT-PCR was considered the most reliable test for assessing the COVID-19 status of a patient by 443 (77.9%) physicians, followed by 92 (16.5%) who chose rapid test IgM antibodies and 31 (5.6%) who chose rapid test for IgG antibodies.
With respect to use of masks by the patient in OP, 338 (60.8%) doctors mandate a mask but were not particular about the type while 117 (31.8%) prefer a 3-ply mask. For hospital staff, 282 (52.7%) prefer a 3-ply mask and 211 (37.9%) would prefer an N95 mask. For doctors in OP, 404 (72.7%) would mandate an N95 mask and 126 (22.7%) would prefer 3-ply masks. In relation to use of personal protective equipment (PPE) in OP, 259 (46.6%) doctors felt that gloves are sufficient and full PPE was not required for both clinician and the assistants while 175 (31.5%) were of the opinion that complete PPE inclusive of gloves was required for both the doctors and assistants. An additional 81 (14.6%) responded that gloves and full PPE were required for the doctor while gloves were sufficient for the assistant and 41 (7.4%) remarked that both gloves and PPE are not required. In order to meet the extra costs arising from measures taken due to COVID-19, 281 (50.5%) doctors would prefer passing it on to those receiving care while 275 (49.5%) felt that these costs were inevitable in the present scenario and preferred to absorb the costs themselves.
Comparison of these perspectives between ophthalmologists and doctors of other specialties is given in Table 1. Ophthalmologists were less involved in clinical work during lockdown (P < 0.001), are more likely to start routine OP immediately after lockdown is lifted (χ2 [6] = 19.31, P = 0.004) and are more likely to seek a declaration from patients in OP (P < 0.001).
Table 1.
Physicians perspectives about precautions in the OPD
| Parameters | Ophthalmologists (n=266) | Other Physicians (n=290) |
|---|---|---|
| Starting routine OPD, n (%) | ||
| Presently running | 33 (12.4) | 65 (22.4) |
| Immediately after lockdown ends | 118 (44.4)** | 87 (30) |
| 2 weeks after lockdown ends | 32 (12) | 47 (16.2) |
| 1 month after lockdown ends | 8 (3) | 10 (3.4) |
| 2 weeks after zero transmission | 37 (13.9) | 41 (14.1) |
| 1 month after zero transmission | 16 (6) | 13 (7.9) |
| Other options | 22 (8.3) | 17 (5.9) |
| Hospital staff shifts, n (%) | ||
| Entire staff reports as usual | 54 (20.3) | 58 (20) |
| 2 batches reporting alternate weeks | 107 (40.2) | 134 (46.2) |
| 3 batches reporting once in 3 weeks | 42 (15.8) | 55 (19) |
| 2-3 batches spread over the day | 41 (15.4) | 29 (10) |
| Other options | 22 (8.3) | 14 (4.6) |
| Mask for patient, n (%) | ||
| Mask not required | 2 (0.8) | 7 (2.4) |
| Mask required. Type not important | 169 (63.5) | 169 (58.3) |
| 3-ply | 78 (29.3) | 99 (34.1) |
| N95 | 17 (6.4) | 15 (5.2) |
| Mask for assistant, n (%) | ||
| Mask not required | 0 (0) | 2 (0.7) |
| Mask required. Type not important | 33 (12.4) | 28 (9.7) |
| 3-ply | 141 (53) | 141 (48.6) |
| N95 | 92 (34.6) | 119 (41) |
| Mask for clinician (s), n (%) | ||
| Mask not required | 1 (0.4) | 1 (0.3) |
| Mask required. Type not important | 12 (4.5) | 12 (4.1) |
| 3-ply | 58 (21.8) | 68 (23.4) |
| N95 | 195 (73.3) | 209 (72.1) |
| PPE for routine OPD, n (%) | ||
| Gloves & PPE for doctor and assistant | 79 (29.7) | 96 (33.1) |
| Gloves & PPE for doctor. Gloves for assistant | 50 (18.8) | 31 (10.7) |
| Gloves for doctor & assistant. PPE not needed | 121 (45.5) | 138 (47.6) |
| Gloves and PPE not needed | 16 (6) | 25 (8.6) |
| Most reliable COVID-19 test, n (%) | ||
| Rapid IgM antibody | 53 (19.9) | 39 (13.4) |
| Rapid IgG antibody | 21 (7.9) | 10 (3.4) |
| RT-PCR for viral antigen | 192 (72.2) | 241 (83.1)** |
OPD: Out patient department, PPE: Personal protective equipment, RT-PCR: Reverse transcriptase polymerase chain reaction, **P<0.001
Perspectives about elective surgeries
There were 299 (54%) surgeons of which 190 (63.5%) were ophthalmologists engaged actively with surgery. A similar number wanted to start routine OT immediately after lockdown was lifted (n = 80, 26.8%) and 2 weeks after lockdown was lifted (n = 82, 27.4%). Forty four (14.7%) surgeons wanted to start routine OT after 2 weeks of no new cases being reported in their locality, 42 (14%) planned to wait for 1 month of no new cases being reported and 36 (12%) would wait for 1 month after lockdown ends. Majority (n = 230, 76.9%) surgeons preferred to make it mandatory to conduct a COVID-19 laboratory test for each patient before an elective surgery.
When starting elective surgeries post lockdown, 102 (34.1%) participants wanted N95 masks for surgeon and assistant along with 3-ply mask for patient in the OT, another 70 (23.4%) wanted 3-ply masks for the surgeon, assistant and the patient, 56 (18.7%) wanted N95 masks for the surgeon and 3-ply masks for assistants and patient and 52 (17.4%) wanted N95 masks for surgeon, assistant and patient. A minority (19, 6.4%) felt that 3-ply masks for the surgeon and assistant were sufficient with no mask for the patient.
An overwhelming majority (n = 241, 80.6%) had not performed surgery with full PPE in the past. Regarding current PPEs, 163 (54.5%) felt that they were safe but uncomfortable, 75 (25.1%) mentioned that these were neither safe nor comfortable, 39 (13%) felt that PPEs available currently are both safe and comfortable and 22 (7.4%) responders opined that they were comfortable but unreliable. Concerning components of PPE usage, 121 (40.5%) felt that routine gloves and gowns were sufficient and additional PPE was not required, 99 (33.1%) felt that full PPE was required for the surgeon, assistant and all OT personnel, 65 (21.7%) were of the opinion that full PPE was needed for the surgeon and assistant while 14 (4.7%) opined that full PPE was necessary for the surgeon alone. Increased follow-up intervals after surgery was preferred by 226 (75.6%) surgeons.
Comparison of these perspectives between ophthalmic surgeons and surgeons of other specialties is given in Table 2. Eye surgeons had lesser experience in using PPE compared to other surgeons (P < 0.001) and are less likely to mandate a COVID-19 test before elective surgery (P = 0.006). Ophthalmic surgeons (n = 56, 29.5%) most commonly preferred 3-ply masks for the surgeon, assistant and the patient in OT whilst other surgeons preferred N95 masks (χ2[4] = 30, P < 0.001) for all these individuals (n = 32, 29.4%). Ophthalmologists opined that additional PPE was not required for surgery and other surgeons were of the opinion that full PPEs required for the surgeon, assistant and all OT personnel (χ2[3] = 33.46, P < 0.001). Ophthalmologists were less likely to consider RT PCR as the most reliable test (χ2[2] = 10.56, P = 0.005).
Table 2.
Surgeons perspectives about precautions in the OT
| Parameters | Ophthalmic Surgeons (n=190) | Other Surgeons (n=109) |
|---|---|---|
| Starting elective surgeries, n (%) | ||
| Immediately after lockdown ends | 53 (27.9) | 27 (24.8) |
| 2 weeks after lockdown ends | 54 (28.4) | 28 (25.7) |
| 1 month after lockdown ends | 24 (12.6) | 12 (11) |
| 2 weeks after zero transmission | 22 (11.6) | 22 (20.2) |
| 1 month after zero transmission | 24 (12.6) | 18 (16.5) |
| Other options | 13 (6.8) | 2 (1.8) |
| Mandate COVID-19 testing for surgery, n (%) | 137 (72.1) | 93 (83.8)** |
| Masks in OT, n (%) | ||
| 3-ply for surgeon & assistant. No mask for patient | 15 (7.9) | 4 (3.7) |
| 3-ply for surgeon, assistant and patient | 56 (29.5)** | 14 (12.8) |
| N95 for surgeon. 3-ply for assistant and patient | 42 (22.1) | 14 (12.8) |
| N95 for surgeon and assistant, 3-ply for patient | 57 (30) | 45 (41.3) |
| N95 for surgeon, assistant and patient | 20 (10.5) | 32 (29.4)** |
| PPE in OT, n (%) | ||
| Additional PPE not required | 96 (50.5)** | 25 (22.9) |
| Full PPE for clinician | 11 (5.8) | 3 (2.8) |
| Full PPE for clinician and assistant | 41 (21.6) | 24 (22) |
| Full PPE for clinician, assistant & OT personnel | 42 (22.1) | 57 (52.3)** |
| Opinion on current PPEs, n (%) | ||
| Safe & comfortable | 30 (15.8) | 9 (8.3) |
| Unreliable but comfortable | 8 (4.2) | 14 (12.8)** |
| Safe but uncomfortable | 108 (56.8) | 55 (50.5) |
| Neither safe nor comfortable. Needs redesigning | 44 (23.2) | 31 (28.4) |
OT: Operation theatre, PPE: Personal protective equipment, **P<0.001
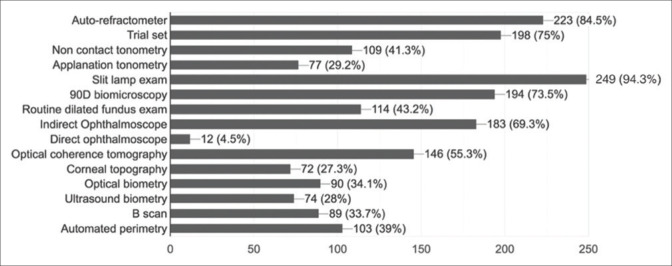
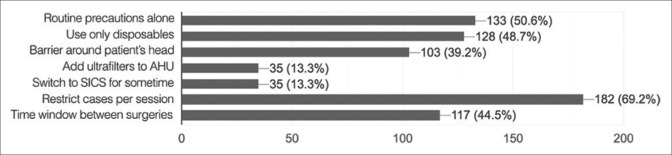
Ophthalmic practices
Ophthalmologists preferred to start using most OP instruments along with their OP consultation [Fig. 1]. An equal number of ophthalmologists (n = 70, 26.4%) preferred starting OP laser procedures immediately and 2 weeks after lockdown, 43 (16.2%) wanted to start l month after lockdown ends, 42 (15.8%) preferred to wait for 1 month and 40 (15.1%) preferred to wait for 2 weeks after no new cases are reported. Half the ophthalmologists (n = 132, 50.6%) considered phacoemulsification to be an aerosol generating procedure (AGP). Precautions that surgeons would like to follow for phacoemulsification are given in Fig. 2. In the spectacle dispensing unit, 78 (30.7%) responders preferred to switch to virtual devices for patients to try spectacles, 76 (29.9%) would restrict the number of frames tried on by the patient, 58 (22.8%) would ask patients to choose without trying on the frames and 20 (7.9%) would not take any special measures.
Figure 1.
Ophthalmologist's responses on instruments that can be used in OPD after lock down is lifted
Figure 2.
Ophthalmologist's perspectives of precautions to be taken in OT for cataract surgeries
Discussion
Doctors and other health care workers are at the highest risk of contracting COVID-19 in their practice. Besides transmission by aerosols and fomites, there is anecdotal evidence of transmission from individuals who are asymptomatic and have subclinical infection.[12,13] Of interest to ophthalmologists, actual viral shedding in tears has not been demonstrated although Xia et al. demonstrated viral antigens with RT-PCR.[14] Zhou and colleagues announced that, of 121 confirmed COVID-19 cases, 8 (6.6%) had ocular symptoms. In all, viral RNA was detected in conjunctival swabs of 3 (2.5%) patients.[15] On the other hand, Seah et al. have reported that viral antigens could not be detected by RT-PCR.[16] In summary, transmission of COVID-19 through the ocular route remains uncertain.[17]
We as doctors cannot expect an “all-clear” all of a sudden and return to resuming our medical practices the way we were used to before the pandemic.[7] It would likely be a few months before any semblance of “normalcy” is restored. In the meantime, it is up to individual practices to adapt and create their own strategies to resume services once lockdown has been lifted. Whilst general hand sanitizing measures, hospital disinfection and triage are more likely to be implemented uniformly, other aspects such as methods for social distancing, protocols in OPD and OT are not very clear. Although we are “locked down”, we continue to gather information about public health status and guidelines being issued by authorities. Doctors have formed some opinion about reopening their practices.
Reopening of regular OP services is a debated topic and doctors, across their type of practice, seem to be unsure of the way ahead. Responses vary widely among different specialists. As a collective group, ophthalmologists are more likely to be away from medical services during lockdown and prefer reopening services as soon as lockdown is lifted. Of importance, All India Ophthalmic Society (AIOS) Consensus Statement experts suggest postponement of routine OP and elective surgeries for 4 weeks or until the government provides guidelines.[6,9] Ophthalmologists are more divided amongst themselves with regard to offering elective laser procedures after lifting of lockdown. Most doctors prefer to split their staff into two groups and ask them to report on alternate weeks. There seems to be an agreement among doctors that, immaterial of type, all patients attending OPD need to wear a mask. 3-ply masks seem to be preferred for assistants in the OPD and N95 masks for doctors. Interestingly, close to 50% doctors felt that gloves alone are sufficient in the routine OPD and full PPE is not essential. In our survey, it was apparent that an overwhelming majority of doctors, and ophthalmologists in particular, had no experience using full PPE in the past and more than 50% doctors were of the opinion that PPEs are safe but uncomfortable to use. Training in proper donning and doffing of PPEs and safe behavior when using PPEs has to be imparted to doctors. With respect to PPEs, risk of exposure varies in different settings and no single strategy is without problems or benefits.[18] Different countries and practices have adopted protocols varying from strict “no-risk” approach employing full PPE to “mask and glove” only approach.[13] In relation to this, AIOS consensus statement recommends 3-ply masks for patients, full PPE and 3-ply or N95 mask for personnel at point of entry to the hospital and obtaining a declaration from the patient regarding the possibility of acquiring COVID-19 from the health care facility.
For a non-high risk patient with no COVID-19 symptoms undergoing a brief close contact OP procedure, like slit-lamp examination or prolonged close contact procedures like laser and injections, 3-ply masks with gloves, goggles and surgical scrub suits are recommended by AIOS consensus statement.[6] This assumes importance as more than 94% ophthalmologists in our survey indicated that they would use the slit lamp when restarting practice. The Royal College of Ophthalmologists recommends switching to indirect laser delivery for cases that require retinal laser therapy.[9] AGPs require the use of N95 masks along with the above mentioned equipment and a surgical gown over the surgical scrub suit.[4,6] Although there is no direct mention of phacoemulsification or vitrectomy being AGPs, any surgery that employs high speed devices can be considered an AGP.[9] It is also recommended that surgeries are performed under a negative pressure environment for patients suspected to have COVID-19.[19] In contrast to our study, Nair et al. reported that only 11.8% and 9.9% of ophthalmologists preferred starting surgeries immediately after lockdown and mandating COVID-19 tests before surgery, respectively.[8] This difference is possibly because of the timing of their survey that was conducted 5 days after lockdown was enforced. By 25 days, doctors had a different perception about the disease and their finances.
Social distancing is the key in limiting spread of COVID-19 and steps have to be taken to ensure it is adhered to once practices reopen.[20,21] Built environment ecosystems that humans have constructed around themselves have largely shaped how we interact with each other on a daily basis and has potential to enhance or curb COVID-19 transmission based on the way it is handled.[22] Higher numbers of patients and staff within the premises lead to increased occupant densities, enhanced levels of activity in a closed environment and inevitable contact with fomites - all of which play a role in virus transmission. In our survey, doctors favored social distancing in the OP by means of re-arranging chairs, limiting attenders and OP timings, moving to an appointment-only approach and insisting on non-contact online payment methods. There was a preference for workforce to be split into shifts to attend to their work on separate schedules, which can factor in the cumulative function for mean incubation period of 5.3 days.[23] Increasing interval between surgeries and avoiding frequent patient visits in the postoperative period are also methods that can be employed. In the spectacle dispensing unit, measures like use of virtual devices and restrict of number of frames tried on can be employed.
In the survey, RT-PCR was chosen as the most reliable test to assess COVID-19 status of patients. The Indian Council of Medical Research has notified that RT-PCR is the gold –standard test for COVID-19 and that rapid antibody tests are useful for epidemiological and surveillance purposes.[24] The utility of rapid tests is evolving and results are also seen to be dependent on field conditions.[24] Independent review of these tests for reliability and accuracy are awaited.[4] In their recommended protocols for seeing patients, the American Academy of Ophthalmology has suggested consideration of preoperative testing (RT-PCR) of asymptomatic patients undergoing aerosol generating procedures.[4]
This survey may serve as a guide to authorities and scientific societies about perspectives of doctors in these troubled times. In due course, regular medical services will need to commence, albeit in a graded manner. Where necessary, steps can be taken to correct misperceptions in a targeted and evidence based manner so that safety of health care workers, patients and the community at large can be ensured.
Our study had a few limitations. Although it was circulated in closed groups alone, we could not identify if all responders were doctors. Its anonymous nature prevented us from assessing responses based on whether the participant was located in a hot spot or not. Since all specialists took part, perceptions varied widely for a few questions.
Conclusion
Pandemics such as COVID-19 dictate terms to humanity. Almost all industries and fields are affected and an overhaul of systems and procedures is necessitated. Health care, perhaps, is the first in line to experience dramatic changes as a result of this pandemic. These are challenging times and a 'new normal' should be expected and prepared for. Opportunities to learn more about infection control protocols and implement them have to be embraced. Information and knowledge gathered about the disease is fast changing and, as doctors, we should be equally quick in keeping abreast of developments and adapting as necessary if we are to ward off this threat and emerge without much damage to person and profession.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Annexure 1
Perspectives of physicians in general and ophthalmologists in particular about restarting services post-COVID-19 lockdown
For all physicians
-
Your age?
- 20-30 years
- 31-40 years
- 41-50 years
- 51-60 years
- 61-70 years
- 71 and above
-
Gender
- Male
- Female
-
Type of practice
- Government
- Private - single practitioner
- Private - multiple practitioners/Group practice
- Corporate hospital/chain
- Non-governmental institute
-
Have you been actively involved in OP or OT services of any kind since lockdown was enforced?
- Yes
- No
-
When would you like to start routine out-patient (OP) services?
- We are presently running routine OPD services
- The day lock down ends
- 2 weeks after lockdown ends
- 1 month after lockdown ends
- 2 weeks after no new cases are reported
- 1 month after no new cases are reported
- Others
-
How would your hospital staff report for work?
- Entire staff reports to work as usual
- Staff divided into 2 batches to report on alternate weeks
- Staff divided into 3 batches to report once in 3 weeks
- Staff divided into two to three batches spread over the day with increased OP timings
- Others
-
What are the methods you would employ to ensure social distancing once you start OP services? (Multiple selection possible)
- Chairs are spaced apart
- Only one Attender allowed
- OP hours are restricted
- History taking over telephone prior to giving an appointment
- Others
-
Would you postpone OP consultation for a non-emergency case based on whether his domicile is a hot-spot or not?
- Yes
- No
-
Would you have a triage facility where all patients are initially screened by a health care worker before being seen by the primary clinician?
- Yes
- No
-
Would you take a declaration from the patient regarding possibility of acquiring COVID-19 from the health care facility?
- Yes
- No
-
Would you insist on non-contact online payment methods (eg. BHIM, GPay, Paytm) to avoid cash or card transfer between individuals?
- Yes
- No
-
What is the mask you would mandate in the OP for the patient?
- Mask not required
- 3Mask mandatory. I am not particular about the type
- 3.ply mask
- N95 mask
-
What is the mask you would mandate in the OP for your assistants?
- Mask not required
- 3Mask mandatory. I am not particular about the type
- 3.ply mask
- N95 mask
-
15. What is the mask you would mandate in the OP for your doctors?
- Mask not required
- 3Mask mandatory. I am not particular about the type
- 3.ply mask
- N95 mask
-
What is the personal protective equipment (PPE) you would mandate in the OP for routine cases?
- Gloves and full PPE for clinician and assistant
- Gloves and full PPE for clinician and gloves for assistant
- Gloves for clinician and assistant
- Gloves and PPE not required, only mask is sufficient
-
In your opinion, which test is most reliable in assessing COVID.19 status of a patient?
- Rapid test IgM
- Rapid test IgG
- RT.PCR
-
How to you plan to meet the extra costs arising out of all the measures taken due to COVID.19?
- Inevitable hence will absorb the costs in the existing packages
- Will pass on the additional costs to the patients
-
What is your area of specialization?
- Medicine and allied specialties
- Surgery and allied specialties
- Dental
- Ophthalmology
-
Do you perform surgeries?
- Yes
- No
For surgeons
-
When would you like to start elective surgeries?
- As soon as lock down ends
- 2 weeks after lockdown ends
- 1 month after lockdown ends
- 2 weeks after no new cases are reported
- 1 month after no new cases are reported
- Others
-
What is the mask you will use in the OT?
- 3-ply masks for surgeon and assistant. No masks for patient
- 3-ply masks for surgeon, assistant and patient
- N95 mask for surgeon, 3-ply masks for assistant and patient
- N95 mask for surgeon and assistant, 3-ply mask for patient
- N95 masks for surgeon, assistant and patient
-
What is the personal protective equipment (PPE) you would mandate in the OT for routine and emergency surgeries?
- Additional PE not required
- Full PPE for clinician
- Full PPE for clinician and assistant
- Full PPE for clinician, assistant and other OT personnel.
-
Would there be a change in protocol for your post operative follow-ups?
- Yes. Increased interval between reviews.
- No. I intend to follow my routine schedule.
-
Have you seen OP or operated with a full PPE before?
- Yes
- No
-
What is our take on the current PPEs available
- Safe and comfortable to use
- Unreliable but comfortable to use
- Safe but uncomfortable to use
- Not safe nor comfortable. Needs redesigning.
-
Would you make COVID-19 testing compulsory for an elective surgery?
- Yes
- No
For Ophthalmologists
-
What are the OP equipment you would begin to use once you start OP (multiple responses can be selected)?
- Auto-refractometer
- Trial set
- Non contact tonometry
- Applanation tonometry
- Slit lamp exam
- 90D biomicroscopy
- Routine dilated fundus exam
- Indirect Ophthalmoscope
- Direct ophthalmoscope
- OCT
- Corneal topography
- Optical biometry
- Ultrasound biometry
- B scan
-
When would you like to start out patient elective interventional procedures like laser therapy?
- As soon as lock down ends
- 2 weeks after lockdown ends
- 1 month after lockdown ends
- 2 weeks after no new cases are reported
- 1 month after no new cases are reported
-
Do you consider phacoemulsification surgery to be an aerosol generating procedure (AGP)?
- Yes
- No
-
What additional precaution(s) do you intend to follow when performing routine phacoemulsification?
- Routine universal precautions
- Use only disposables
- Barrier around the patients head to prevent aerosol dispersion
- Addition of Ultra filters to the AHU
- Switch to Small incision cataract surgery for sometime
- Others
-
What are the precautions you would follow in your spectacle dispensing unit?
- No special precautions
- Restrict the number of frames tried by the patient
- Ask the patient to chose without trying on frames
- Switch to virtual devices to try on eye wear
- Others
References
- 1.Chart: What Share of the World Population Is Already on COVID-19 Lockdown? | Statista. [Last accessed on 2020 Apr 24]. Available from: https://www.statista.com/chart/21240/enforced-covid-19-lockdowns-by-people-affected-per-country/
- 2.WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. [Last accessed on 2020 Apr 24]. Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 .
- 3.COVID-19. Eur Cent Dis Prev Control. [Last accessed on 2020 Apr 24]. Available from: https://wwwecdceuropaeu/en/covid-19-pandemic .
- 4.Important coronavirus updates for ophthalmologists. Am Acad Ophthalmol. 2020. Apr, [Last accessed on 2020 Apr 24]. Available from: https://www.aao.org/headline/alert-important-coronavirus-context .
- 5.Ministry of Health and Family Welfare, Govt. of India. [Last accessed on 2020 Apr 24]. Available from: https://www.mohfw.gov.in/
- 6.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society – Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Returning to Ophthalmology Practice. Am Acad Ophthalmol. 2020. Apr, [Last accessed on 2020 Apr 24]. Available from https://wwwaaoorg/about/governance/academy-blog/post/returning-to-ophthalmology-practice . Available from https://wwwaaoorg/about/governance/academy-blog/post/returning-to-ophthalmology-practice .
- 8.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey. Indian J Ophthalmol. 2020;68:725–30. doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Opthalmologists TRC of. COVID-19 clinical guidance for ophthalmologists. R Coll Ophthalmol. 2020. Apr, [Last accessed on 2020 Apr 24]. Available from: https://www.rcophth.ac.uk/2020/04/covid-19-update-and-resources-for-ophthalmologists/
- 10.Akladios C, Azais H, Ballester M, Akladios C, Azais H, Ballester M, et al. Recommendations for the surgical management of gynecological cancers during the COVID-19 pandemic - FRANCOGYN group for the CNGOF? J Gynecol Obstet Hum Reprod. 2020:101729. doi: 10.1016/j.jogoh.2020.101729. doi: 10.1016/j.jogoh. 2020. Epub ahead of print. PMID: 32247066; PMCID: PMC7118621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Givi B, Schiff BA, Chinn SB, Clayburgh D, Gopalakrishna Iyer N, Jalisi S, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg Published online March 31, 2020. doi: 10.1001/jamaoto.2020.0780. doi: 101001/jamaoto20200780. [DOI] [PubMed] [Google Scholar]
- 12.Chang D, Xu H, Rebaza A, Sharma L, Dela Cruz CS. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. doi: 10.1016/S2213-2600(20)30066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olivia Li J-P, Shantha J, Wong TY, Mehta J, Lin H, Lin X, et al. Preparedness among Ophthalmologists: During and beyond the COVID-19 pandemic. Ophthalmology. 2020;127:569–72. doi: 10.1016/j.ophtha.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection [published online ahead of print, 2020 Feb 26] J Med Virol. 2020 doi: 10.1002/jmv.25725. 101002/jmv 25725 doi: 101002/jmv25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou Y, Duan C, Zeng Y, Tong Y, Nie Y, Yang Y, et al. Ocular findings and proportion with conjunctival SARS-COV-2 in COVID-19 patients [published online ahead of print, 2020 Apr 21] Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.04.028. doi: 10.1016/j.ophtha.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seah IYJ, Anderson DE, Kang AEZ, Wang L, Rao P, Young BE, et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients [published online ahead of print, 2020 Mar 24] Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.03.026. doi: 10.1016/j.ophtha. 2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu AY, Tu R, Shao X, Pan A, Zhou K, Huang J. A comprehensive Chinese experience against SARS-CoV-2 in ophthalmology [published online ahead of print, 2020 Apr 07] Eye Vis. 2020 doi: 10.1186/s40662-020-00187-2. doi: 10.1186/s40662-020-00187-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Odor PM, Neun M, Bampoe S, Clark S, Heaton D, Hoogenboom EM, et al. Anaesthesia and COVID-19: Infection control [published online ahead of print, 2020 April 08] BJA Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.03.025. doi: 10.1016/j.bja.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Balas M, Al-Balas HI, Al-Balas H. Surgery during the COVID-19 pandemic: A comprehensive overview and perioperative care [Epub ahead of print] Am J Surg April. 2020 doi: 10.1016/j.amjsurg.2020.04.018. doi: 10.1016/j.amjsurg. 2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study [published online ahead of print, 2020 Apr 17] Lancet Public Health. 2020 Apr; doi: 10.1016/S2468-2667(20)30090-6. doi: 10/1016/S2468-2667(20) 30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kabesch M, Roth S, Brandstetter S, Häusler S, Juraschko E, Weigl M, et al. Successful containment of COVID-19 outbreak in a large maternity and perinatal center while continuing clinical service [published online ahead of print, 2020 Apr 22] Pediatr Allergy Immunol Off Publ Eur Soc Pediatr Allergy Immunol. 2020 Apr; doi: 10.1111/pai.13265. doi: 10.1111/pai13265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dietz L, Horve PF, Coil DA, Fretz M, Eisen JA, Van Den Wymelenberg K. 2019 Novel Coronavirus (COVID-19) pandemic: Built environment considerations to reduce transmission. mSystems. 2020;5:e00245–20. doi: 10.1128/mSystems.00245-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koo JR, Cook AR, Park M, Sun Y, Sun H, Lim JT, et al. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study? Lancet Infect Dis. 2020;20:P678–88. doi: 10.1016/S1473-3099(20)30162-6. doi: 10.1016/S1473-3099(20)30162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.COVID-19 | Indian Council of Medical Research | Government of India. [Last accessed on 2020 Apr 24]. Available from https://wwwicmrnicin/content/covid-19 .