Abstract
The COVID-19 pandemic has brought with it the huge burden of mortality and morbidity across the world and the added effects of the mandatory lockdown measures to try and control the spread. A number of aspects of healthcare including eye donation and eye collection require adequate safety precautions in place to keep both the involved healthcare workers and patients safe. This paper highlights the consensus-based guidelines by an expert panel on how to restart eye banking and eye collection services and carry out emergency corneal surgeries during this COVID-19 time. These guidelines will be applicable to all eye banks across the country and should help ophthalmologists and eye banking staff to restart eye banking while safeguarding themselves and their patients.
Keywords: Consensus, cornea guidelines, COVID-19, eye banking, ophthalmology, pandemic, precautions, preferred practice
The COVID-19 pandemic has affected people around the world and the medical fraternity in particular. It has made us change the way we function and in the aftermath of this pandemic, ophthalmologists will require practical guidelines based on advisories from national health departments on how to restart eye banking and cornea-related healthcare across the country.
As per the Ministry of Health and Family Welfare(MoHFW), hospitals can continue emergency services with adequate spacing in OPDs and personal protective equipment except in containment zones. Elective and non emergency follow ups and surgeries can be deferred.[1]
This paper highlights the consensus based guidelines by an expert panel comprising of representatives from the All India Ophthalmological Society (AIOS), Eye Bank Association of India(EBAI), Indian Society of Cornea and Keratorefractive surgeons (ISKRS), Cornea society of India(CSI) and major governmental and private ophthalmological institutions in India. These guidelines will be applicable to all eye banks across the country and should help ophthalmologists and eye banking staff to restart eye banking while trying to ensure the safety of their patients and themselves.
Methods
These guidelines outline the infection prevention and control advice for ophthalmologists and healthcare workers (HCWs) involved in the treatment of patients for ophthalmic care especially with regard to eye banking practices and cornea services. These guidelines are based on the available literature and guidelines issued from the MoHFW, Government of India, and Indian Council of Medical Research (ICMR). With the evolving situation on COVID-19, further updates may be made to this guidance as and when required. An invitation to review these guidelines was sent out by email to eminent ophthalmologists across India, including heads of the major teaching institutions, both in the government and private sectors. The experts suggested several changes in the base document that was collated, and the consensus derived. Disagreements on guidelines were resolved by discussion between members.
Practice Guidelines for Ophthalmologists with relevance to Eye Banking and Cornea
Advisory for resuming the eye banking activitiesa
All collected tissues should be quarantined for 48 h prior to the release of the tissue for usage for transplantation. Avoid immediate usage
The Eye Banking activities to be resumed through hospital cornea retrieval programme (HCRP) and to be from a hospital which is declared as non-COVID-19
Voluntary/Community donation and eye collection is more hazardous for the recovery team and to be put on hold for 2 weeks or until the fresh guidelines are circulated whichever is earlier
No eye banking activities to be started in the containment areas of red zones. Containment zones shall be demarcated within red (Hotspots) and orange Zones by State/UTs and District Administration based on the guidelines of MoHFW
The Recovery Technician/doctor to use personal protective equipment (PPE) -including N95 mask, cap, face shield/visor, gloves, gown, while recovering the donor tissue for 2 weeks or until the fresh guidelines are circulated whichever is earlier
The technicians and relevant staff must be given training about the PPE use and other precautions during retrieval to reduce the risk of acquiring or spreading the infection
Eye Bank Association of India recommends that the collection of a nasal swab of the deceased donor for RT-PCR COVID-19 testing may be done at the discretion of the hospital director.
The Eye Bank Association of India recommends that eye banks exclude the following potential donors for ocular tissue collection[2]
Tested positive for or diagnosed with COVID-19
Acute respiratory illness or fever 100.4°F (38°C) or at least one severe or common symptom known to be associated with COVID-19 (e.g., unexplained fever, cough, shortness of breath, diarrhea) with no other etiology that fully explains the clinical presentation Table 1
Individuals who have been exposed to a confirmed or suspected COVID-19 patient within the last 14 days, who have returned from nations which have more than 10 infected patients and those whose cause of death was unexplained should not be accepted as deceased donors.
As India itself is a country where COVID-19 pandemic is spreading rapidly, any patient who lives or has visited the red zone as defined by the Ministry of Health and Family Welfare vide D.O. No. Z.28015/19/2020-EMR dated 30.04.2020 will be considered as a risk and must be assessed for the clinical symptoms and avoided for eye donation
Evidence of conjunctivitis
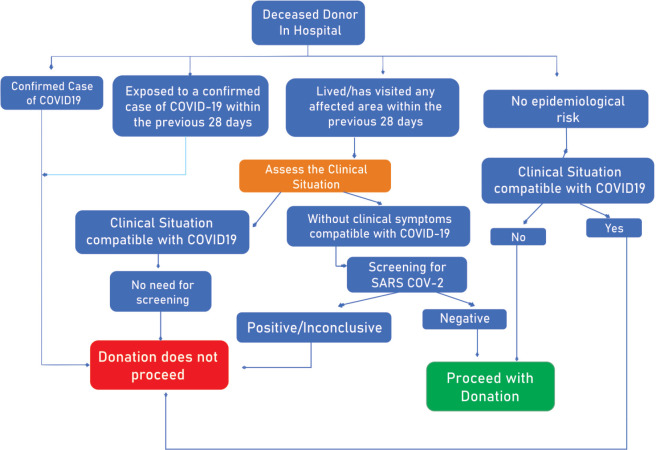
ARDS, pneumonia, or pulmonary computed tomography (CT) scanning showing “ground-glass opacities” (regardless of whether another organism is present) ([Fig. 1 - Algorithm to follow for Deceased Tissue Donation).[3]
Table 1.
COVID-19 symptoms[2]
| COVID-19 Symptoms | ||
|---|---|---|
| Severe | Common | Less Common |
| Difficulty in breathing | Fever | Myalgia |
| Chest Pain | Dry Cough | Fatigue |
| Confusion | Shortness of breath | Headache |
| Bluish lips or face | Hemoptysis | |
| Unresponsiveness | Diarrhoea | |
| Sore Throat | ||
| Rhinorrhea | ||
| Wet Cough | ||
| Loss of smell and test | ||
Figure 1.
Algorithm to follow for Deceased Tissue Donation
General functioning guidelines
Eye banks should document the risk assessment of the deceased by taking a relevant history from attender or family members and ensure that all staff are aware of the above
It is recommended that only corneal scleral rim excision be performed and avoid the whole eyeball enucleation
Use intermediate preservative media for the preservation of corneas
Donor corneas in intermediate preservation media if not utilized should be shifted to glycerol on the last day of preservation and kept in a deep freezer for future use for tectonic purposes
Recovery procedures mandatorily require double contact of povidone-iodine to ocular tissue before retrieval[4]
The entire disposable PPE kit to be removed immediately after tissue retrieval, properly packaged to avoid cross-infection and disposed off after reaching the hospital as per the guidelines
As a precaution use double-layered bags (using 2 bags) for collection of waste (blood sample/Cornea) to ensure adequate strength and no leaks[5]
Non-disposable parts of the PPE like goggles/visor to be cleaned with spirit or 1% sodium hypochlorite immediately after returning to the hospital
Clean all external surfaces of MK Medium/Cornisol bottles, flask, ice gel packs, instrument tray, stainless steel bin with surgical spirit, alcohol wipes, or freshly prepared 1% sodium hypochlorite after recovery and repeat it at Eye Bank
All the donor forms and documents are to be exposed to Ultraviolet light in the Laminar flow hood for 30 min immediately after the team arrives at the eye bank. (Expose both sides of forms -30 min +30 min)
The technicians who handled the tissues and materials, to wash hands thoroughly with soap and water for about 30 s up to elbow before handling any other work in the eve bank. (Staff should occupy only their dedicated chair and should not sit in somebody's chair)
Each eye bank should monitor and consult local THOTA/NOTTO/SOTTO/ROTTO/State health authority/NPCB for daily or weekly reports
Eye Donation Counsellor/Eye Recovery Technicians may be asked to be on call with limited movement in the hospital
Eye bank-related officials must disclose the history of a hospital visit in the past 14 days (Verify papers for the cause of visit)
The Eye Banks must follow the instructions of local State Government for starting of services.
Cleaning of the eye bank
The floor of the eye bank and laboratory areas MUST be cleaned with 1% Sodium Hypochlorite every 2 hourly
Deep cleaning to be done anytime there is any contamination
Door handles, side rails on stairs, high touch surface like reception counter, help desk, gate with 1% Sodium Hypochlorite (4 Times/Day)
Chair in the waiting area (head end, armrest etc.), electronic/IT equipment like monitor, keyboard, mouse, etc. must be done with alcohol swab every 2 h.
Human resource
Eye banks should consider reorganization of the activities, introducing work shifts and batches and the personnel from one shift to not get in touch with the other shift to minimize the possibility of cross-infection. If a team gets quarantined due to any reason, then the other one can still continue to perform eye banking functions
PPE at the workplace should include mask (N95/other approved masks), gloves and visor (face shield) and regular apron. Usage, sterilization/disposal of masks as per protocol for each mask
All Eye Bank Staff should be provided with sufficient number of masks, gloves, single-use plastic aprons, with hand sanitizers
Frequent hand washing and use of hand sanitizer are recommended and sanitizer should be readily available with all team members during their duty timings
Mask is mandatory in the presence of other persons
Separation of office workstations
Maintain 1.5 m physical distance at all times
If staff suspected of contact but asymptomatic, quarantine for a minimum of 14 days and test as per protocols and symptomatology
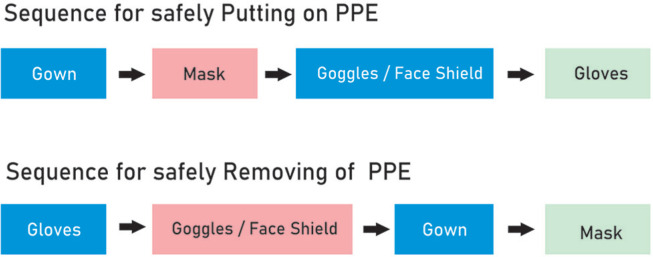
Fig. 2- Sequence for safely putting on and removing PPE
Wash hands or use an alcohol-based hand sanitizer immediately after removing all PPE.
Figure 2.
Sequence for safely putting on and removing PPE
All the staff members are advised to follow the below steps while going back home from eye bank/hospital[6]
Ring up home when you start form office
Someone at home should keep the front door open (so that you don't have to touch the calling bell or door handle) and a bucket of water with washing soap powder or bleaching powder added to it at the front door
Keep things (vehicle keys, pen, sanitizer bottle, phone) in box outside the door
Wash your hands in the bucket and stand in the water for a few minutes. Meanwhile use tissue and sanitizer and wipe the items you have placed in the box
Wash your hands with soap water again
Now enter the house without touching anything
The bathroom door is kept open by someone and a bucket of detergent soap water is ready
Take off all the clothes and soak inside the bucket
Take head bath with shampoo and body with soap
Wash your clothes and dry clothes in direct sunlight.
Staff training
A training program May be organized for all the staff of the eye bank, covering all the above guidelines and proper usage of doffing and donning of PPE by the medical director/eye bank manager. Nasopharyngeal swab may be taken by appropriately trained personnel.
Prioritize surgeries as per their level of medical urgency—For corneal transplants: Tectonic and therapeutic corneal transplants to be done on priority over optical and lamellar corneal transplants. Special consents can be added to the preoperative protocol for COVID-19 time. There are a number of other procedures and surgeries which may be required on emergency and semi-urgent basis and can be prioritized and undertaken with necessary care and precautions [Table 2].
Table 2.
Urgency wise list of corneal procedures
| Emergency procedure | Semi-emergency procedures | Elective procedure |
|---|---|---|
| Corneal Tear repair/Open Globe injury: Repair±Anterior Chamber reconstruction±Traumatic cataract Surgery±Anterior Vitrectomy, etc. Lid laceration repair |
*Keratoplasty for bilaterally blind/paediatric | *All keratoplasties |
| Wound Dehiscence Repair- Post Penetrating Keratoplasty (PK)/Post Therapeutic PK/Post Deep Anterior Lamellar Keratoplasty |
Closed Globe injury: Paracentesis/Hyphema drainage, Traumatic intumescent cataract Anterior Lens Capsule tear |
|
| *Therapeutic/Tectonic keratoplasty | Shield Ulcer debridement Supratarsal steroid |
All Ocular Surface surgeries |
| Emergency Perforation repair - Tenons patch/Amniotic Membrane Graft/Tissue adhesive+BCL |
Emergency tarsorrhaphy | Corneal collagen cross linking (C3R/CXL) |
| Ulcers - Corneal scrapings /AC tap /wash/Intracameral Injection/Tarsorrhaphy | Pseudomembrane peeling for Epidemic Keratoconjunctivitis (Precautions to ensure it is not COVID-19 conjunctivitis but adequate protection to be maintained) |
Pseudomembrane peeling for Epidemic Keratoconjunctivitis |
| Broken/Loose suture: Removal Epilation of Trichiatic lashes |
Acute hydrops: Intracameral C3F8 injection±Compression sutures | |
| SubTenon/Peribulbar injection of steroid or IVMP injection if required in Corneal graft Rejection | ||
| Management of Acute Stevens Johnson Syndrome/Ocular Burns as per protocol |
Management of Stevens Johnson Syndrome/Ocular Burns as per protocol |
|
| Foreign Body Removal: Surface or Intracameral | ||
| Surgery for Ocular Surface Squamous neoplasia (OSSN) |
Conclusion
The COVID-19 pandemic has had a huge impact on healthcare both by the direct mortality and morbidity associated and the indirect effects of lockdown and social distancing measures to control the infection spread. The death toll around the world has risen steadily and the challenges faced by the healthcare systems is manifold.[7] Due to the close contact with patients, procedures which generate aerosols and potential risk of presence of virus in tears there was a fear that ophthalmologists and eye-related HCWs are at a slightly higher risk of developing the infection.[8,9] However there is no proven consensus on this matter.[10] It is important to use preferred practice guidelines so that we can exert extra care to restart eye banking and do at least the emergency surgeries without facilitating disease transmission and keeping ourselves safe. We hope that these eye banking guidelines are useful to ophthalmologists around the country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Ministry of Health and Family Welfare, Government of India
Eye Bank Association of India
Indian Society of Cornea and Keratorefractive surgeons
Cornea society of India
National Programme for Control of Blindness
Footnotes
Disclaimer
The expert panel would like to declare that this document contains guidelines based on information issued by various relevant organizations, and State and Central Governments as on the date of their release. The current outbreak is unpredictable and adherence to any recommendations included in this document may not ensure a successful outcome in every situation. Furthermore, the recommendations contained in this document should not be deemed inclusive of all proper methods of care nor exclusive of other methods of care reasonably directed to obtaining the same results. These guidelines reflect the best available information at the time the document was prepared. If widespread community-transmission occurs, healthcare infrastructure and capacity issues may have a further impact on donation and transplantation. These recommendations will be regularly updated to account for the changing epidemiology and new information regarding treatment and testing. The guidelines do not replace or override existing national/regional/local statutory requirements. All transplant units and eye banks must be aware of national and local government guidance. The ultimate judgment regarding the propriety of any specific therapy must be made by the physician and the patient considering all the circumstances presented by the individual patient, and the known variability and biological behavior of the medical condition. This expert panel does not warrant the accuracy or completeness of the guidance and assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this guidance or for any errors or omissions. No suit or legal proceedings shall lie against any person for anything done or intended to be done in good faith under this suggestions/advisory unless proved otherwise.
References
- 1.Ministry of Health and Family welfare- [Last accessed on 2020 Mar 20]. Available from: https://www.mohfw.gov.in/pdf/AdvisoryforHospitalsandMedicalInstitutions.pdf. Advisory for Hospitals and Medical Institutions .
- 2.COVID-19 Updated Guidance and Screening Recommendations by Eye Bank Association of America dated 14th April 2020. [Last Accessed May 2020]. Available from: https://restoresightorg/covid-19-updates/
- 3.Spanish recommendations to manage organ donation and transplantation regarding the infection associated with the new coronavirus (SARS-Cov-2) producer of COVID-19 dated 27th March 2020. [Last Accessed May 2020]. Available from: https://wwweatborg/images/COVID-19_Summary_of_Spanishpdf .
- 4.Regulatory updated by Eye Bank Association of America dated 29th April 2020. [Last Accessed May 2020]. Available from: https://restoresightorg/covid-19-updates/
- 5.Guidelines for Handling. Treatment and Disposal of Waste Generated during Treatment/Diagnosis/Quarantine of COVID-19 Patients dated 25th March 2020. [Last Accessed May 2020]. Available from: https://wwwmohfwgovin/pdf/63948609501585568987wastesguidelinespdf .
- 6.Advisory by Office of Minister of Health, Power, PWD, Home, UD. Water, I & FC & Industries, Govt. of Delhi: Delhi Secretariat No. minhealth/2020/1108 dated 7th April 2020 [Google Scholar]
- 7.Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020 doi: 10.1002/jmv.25757. doi: 101002/jmv25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28:391–5. doi: 10.1080/09273948.2020.1738501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang L, Wu P. There may be virus in conjunctival secretion of patients with COVID-19. Acta Ophthalmol. 2020;98:223. doi: 10.1111/aos.14413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seah IYJ, Anderson DE, Kang AEZ, Wang L, Rao P, Young BE, et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.03.026. doi: 10.1016/j.ophtha.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]