Abstract
Telemedicine and tele-ophthalmology have been in existence since many years, but have recently gained more importance in the present scenario of pandemic COVID-19. The attitude and perception of the doctors and patients has been changing gradually. Telemedicine has many advantages including providing care in inaccesible areas.In the present scenario, tele-ophthalmology gives an oppurtunity to patient for seeking consultation while also protecting against the contagion. There are many barriers faced by the patients and doctors that have restricted use of this technology in the past. However, with a systematic approach to designing the best suited technology, these barriers can be overcome and user friendly platforms can be created. Furthermore, the demand and use of teleconsulation had increased presently in this area of pandemic. Recent survey conducted by the All India Ophthalmological Society also reveals that many ophthalmologists who have not used tele-ophthalmology in the past are more keen to use it presently. In this article, we have reviewed telemedicine and tele-ophthalmology literature on Google and PubMed to get a holistic idea towards teleconsultation, its advantages, increased importance and prefrence during COVID-19 pandemic and various barriers faced so that the known challenges can be understood, which can pave way for better understanding and future incorporation into practice.
Keywords: Barriers of tele-ophthalmology, pandemic, telemedicine guidelines, telemedicine, tele-ophthalmology
Telemedicine is diagnosis and treatment of health condition using telecommunication technology. One of the earliest and most famous uses of hospital-based telemedicine was in the late 1950s and early 1960s, when a closed-circuit television link was established between the Nebraska Psychiatric Institute and Norfolk State Hospital for psychiatric consultations.[1] Tele-ophthalmology exists since many years, but its application has been challenging because of its need for standardized and high definition digital images.[2]
In a pandemic like COVID-19, it is advised to decrease in-person consultation to maintain social distancing. Also, Teleconsultation decreases burden on healthcare system and currently is of paramount importance.
We conducted literature search on Google and PubMed to assess the attitude towards teleconsultation, its advantages and barriers, and its increased importance and preference during COVID-19.
Definition
World Health Organization (WHO) defines Telemedicine as “The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities”.[3]
Attitude towards Tele-Ophthalmology
To understand the attitude towards adopting tele-ophthalmology, an anonymous descriptive survey was conducted, to which 58 ophthalmologists responded. 71% of the respondents had not used telemedicine, but 82% were willing to participate in teleconsultation. However, 59% had low confidence in providing opinion on remote consultation. The survey revealed an inclination towards practicing telemedicine, especially by younger ophthalmologists,[4] emphasizing the requirement for good telemedicine platforms.
All India Ophthalmological Society (AIOS) recently conducted a survey to assess the attitude of ophthalmologists in India towards tele-ophthalmology. The results depicted a surge in attitude towards integration of tele-ophthalmology into practice. Out of a total of 1180 responses, only 17.5% were already using tele-ophthalmology. However, 98.6% of all participants showed interest to incorporate it into their practice and 98.8% of all participants were eager to adopt a dedicated mobile application (app) based teleconsultation. 93.1% were interested to use an affordable ophthalmology specific Electronic Medical Record (EMR) if AIOS was to develop it. 54.9% respondents had previously used EMR which would make adoption of this technology less challenging. These results demonstrate that demand for tele-ophthalmology has accelerated in this hour of need.[5]
These results are influenced by the fact that the survey was conducted during the times of lockdown where in-person consultations were not possible. It needs to be seen as to whether this remains a felt need even later when elective consultations are feasible. The findings have been summarized in Figs. 1-5.
Figure 1.
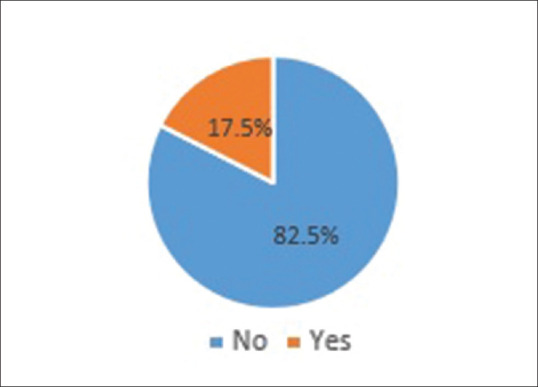
Current use of tele-ophthalmology in practice
Figure 5.

Respondents willing to use affordable ophthalmology specific EMR
Figure 2.

Interest to incorporate tele-ophthalmology into practice
Figure 3.
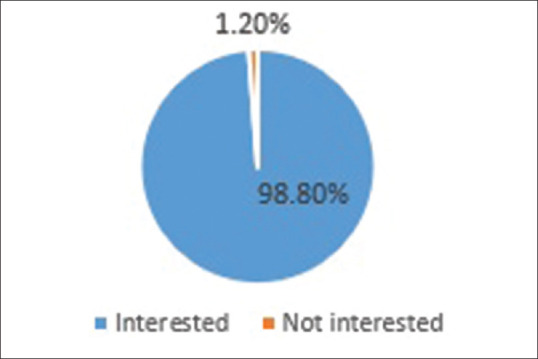
Interest to try mobile-app based tele-ophthalmology
Figure 4.
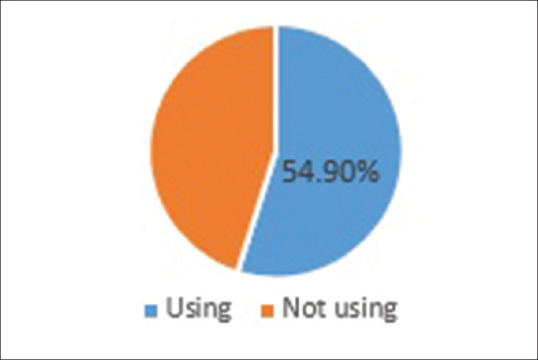
Use of electronic medical records in practice currently
Barriers and Solutions
Unfamiliarity with tele-ophthalmology
One vital barrier for use of tele-ophthalmology is unfamiliarity with its use for both the patient and doctor. Study conducted in United States (US) emphasizes that major patient barriers to use included unfamiliarity with tele-ophthalmology and logistical challenges whereas major facilitators were factors related to convenience and recommendation from doctor. Major barriers for doctors included difficulty in identifying when patients were due for consultation and unfamiliarity with tele-ophthalmology and major facilitators were ease of referral process and communication of screening results.[6]
Formal training of doctors and user-friendly platforms for patients can overcome this barrier. In the currently available platforms, the technology manages everything and the ophthalmologist has to only provide consultation.
Patient concern regarding accuracy
Another crucial barrier for doctors and patients towards telemedicine is their concern regarding its accuracy.
The Skyes survey in US for use of telemedicine in COVID-19 era found that 40% of respondents were concerned about the ability to get proper diagnosis or treatment in virtual setting.[7]
Solution for this is clear identification of conditions which should be adopted for teleconsultation in ophthalmology. The authors propose an 8 point plan for the same [Table 1].
Table 1.
Ophthalmological conditions suitable for teleophthalmology
| Ophthalmological conditions more suitable for TeleOphthalmology |
| 1st consultation- conditions which can be reasonably diagnosed on video consult viz. stye, chalazion, red eye with no loss of vision etc. |
| Follow up for medicine optimization |
| Follow up of surgery patients with no complaints (reduced number of visits) |
| Counselling- LASIK, diabetic retinopathy, glaucoma, cataract, computer vision syndrome etc. |
| Cross consultation between multidisciplinary super specialists and ophthalmologists |
| Trauma- first aid , tele triaging through health care worker |
| Consultation to patients in inaccessible areas |
| Consultation to patients in remote areas where optometrists are available |
*LASIK: Laser- assisted in situ keratomileusis. †Any telemedicine consultation can be converted to an in-person consultation if the ophthalmologist, as per his/her clinical judgment feels that more information is needed to diagnose and treat the condition
High cost of initial investment
Traditionally telemedicine was used in ophthalmology majorly for diabetic retinopathy (DR) screening and diagnosis. One of the barriers for diabetic retinopathy screening via tele-ophthalmology is high cost of initial investment incurred for installation of fundus camera. A Spanish study found that although direct fundus examination is less costly from public health system perspective due to less capital expenditure and maintenance costs, tele-ophthalmology is more economical from a global perspective due to lower travel costs and lost income for the patients.[8]
In the author's experience, the best platform for teleconsultation in present time is a dedicated mobile-based telemedicine app, which does not come with a very high cost.
Poor quality of images
Successful implementation of tele-ophthalmology in diabetic retinopathy was hampered because of ungradable images due to poor field definitions, small pupil size and media opacities. Due to higher frequency of cataract, tele-ophthalmology programs with non-mydriatic fundus camera have higher rate of ungradable images. In one study, ungradable images ranged from 3.1% to 10.6% for DR and 12.6% to 22.3% for macular edema.[9]
To reduce the incidence of ungradable images, authors advocate establishing comprehensive standard operating procedures. Adequate training of staff on image capture and upgrading of instruments is required.
Non-availability of trained staff
Technically challenged staff and resistance to change affect acceptance of teleconsultation significantly.[10] Appropriate implementation requires a structured organization, with a team comprising of a leader, a physician specially trained in telemedicine, trained para-clinical staff and tele-technician.[11]
According to the Indian guidelines for Telemedicine issued on 25th March 2020, a mandatory online course will be developed at a later date. Any Registered Medical Practitioner (RMP) wishing to practice telemedicine will have to undertake this course within 3 years of its notification. This would produce better trained teleconsultants.[12]
Lack of dedicated staff for telemedicine implementation
An Australian survey emphasizes on having 'Telehealth Champions' who are enthusiastic to initiate and promote uptake of telehealth services. 39 individuals involved in operation of 37 diverse telehealth services throughout Australia were interviewed. 25 of the 37 services were initiated by 'champions' who were involved in promotion of telehealth, acting as legitimators and to build relationship. The services were vulnerable to cessation when they lost interest or moved on.[13]
Hence, a dedicated onsite project coordinator is required who gives undivided attention to implementation and management of telemedicine services.
Policy barriers
Defined rules, regulations, procedures and protocols are required for proper functioning of telemedicine. Many practitioners fear legal issues related to malpractice, which has limited its acceptance.[11]
A pilot study in Ethiopia found that factors like e-government readiness, enabling policies, multi-sectoral involvement and capacity building processes affect successful implementation of telemedicine.[14]
Privacy and security concerns
There are privacy and security concerns associated with Telehealth that can adversely affect patients and clinicians level of trust and willingness to adopt and use the system. Privacy risks involve a lack of control over the collection, use and sharing of data. Also, smartphone apps may share sensitive data such as sensor data on location without the user's knowledge.[15] Thus, ensuring patient privacy and confidentiality is important to build trust between doctor and patient.
Other barriers
Software and hardware of the equipments needs to be regularly updated.[11]
Teleconsultation using mobile App or video call is possible only when reliable high speed internet is available.[11] Wherever its availability is limited, simple mobile call can be used as a method of teleconsultation.
An Ethiopian study shows that organizational barriers account for 48% of all barriers, whereas customer, staff and programmer's barriers represents 30% and 22%, respectively. Inadequate Information and communications technology (ICT) infrastructure including poor internet connection, e-health equipment and insufficient access to electric power for proper implementation of telehealth services were considered as the most common organizational barriers. The main consumer barriers affecting adoption of telemedicine are limitation of computer or e-Health literacy, internet bandwidth of dwelling, access to mobile phone, socioeconomic factors, cultural factors and unawareness of existence of telehealth services. Staff and programmer's barriers include technically-challenged staff, resistance to change, language problem, and anxiety.[16]
There is no perfect 'one size fits all' technology and so the use of combined interoperable applications, according to the local context is highly recommended.[14]
From experience, authors advocate identification of implementation strategies to directly address barriers and facilitators for tele-ophthalmology use. Also, the physician has to endorse teleconsultation and promote its use to their patients wherever possible.[17]
The barriers faced by the doctors and patients have been summarized in Table 2.
Table 2.
Barriers for adoption of telemedicine and teleophthalmology
| Barriers for Health care providers |
| Unfamiliarity with Tele-ophthalmology |
| Concern regarding accuracy |
| High cost on initial investment |
| Poor quality images |
| Non- availability of trained staff |
| Lack of dedicated staff for telemedicine implementation |
| Technically challenged staff |
| Resistance to change |
| Policy barriers |
| Regular upgradation of equipment |
| High speed internet |
| Inadequate ICT infrastructure |
| Privacy and security concerns |
| Barriers for Patients |
| Unfamiliarity with Tele-ophthalmology |
| Concern regarding accuracy |
| High speed internet |
| Preference for face to face consultation |
| Limited computer or technology use and knowledge |
| Limited access to mobile phones specially smart phones in rural areas |
| Socio-economic factors |
| Privacy and security concerns |
*ICT: Information and communications technology
Advantages of Teleconsultation
Extensive outreach
According to guidelines, RMP can provide teleconsultation anywhere within India.[12] Consultation can be provided in inaccessible areas also, thus, having an extensive outreach and leading to expansion of clinical practice.
Some of the successful ongoing tele-ophthalmology projects in India are SNTOP[18] (SankaraNetralaya Teleophthalmology Project), ATN (Aravind Tele Network),[19] KIDROP,[20] etc., SNTOP focuses on comprehensive eye examination in rural areas of South India. Customized mobile van unit equipped with ophthalmic examination unit and satellite connectivity is sent to villages. Preliminary examination and screening, including anterior and posterior segment imaging is done by optometrist. Data is subsequently transferred to expert in base hospital and real-time interaction via videoconferencing is done between the expert, examining optometrist and patient.[18]
EyeSmart EMR app for tele-ophthalmology consultations consists of video conferencing across the vision centers of LVPEI eye care network in India. 15,001 tele-ophthalmology consultations were provided to patients from vision centers from January 2017 to August 2018. They concluded that the use of technology played a vital role in appropriate medical management as it connected patients at rural areas and ophthalmologists at higher centers.[21]
Timely intervention in emergency situation
Through telemedicine timely access to appropriate intervention can be provided in emergency situation. In ophthalmology, chemical injury and trauma are prime emergencies. Non availability of ophthalmologist for emergency services causes delay in initiation of treatment and can impair long term visual potential. According to study published by Veterans Affairs Palo Health Care system in California, emergency ophthalmology coverage was available in 48.6% of rural facilities compared to 74.7% in non- rural facilities.[22] This study highlights existence of coverage gap for emergency eye care in rural facilities and establishes the importance of use of tele-ophthalmology.
Avoiding unnecessary referrals
A study recognized that most patients referred for fundus examinations do not need specific treatment. This signifies that teleconsultation could be a viable tool in countries where healthcare assistance remains a challenge due to the size of the country and the dearth of doctors in certain areas.[23] Through tele-ophthalmology, we can select patients who require intervention, thus, reducing burden on healthcare system.
Saves cost, time and effort
Teleconsultation saves travel cost, time and effort of patients wherever in-person consultation is not mandatory. Economic review provides evidence of cost effectiveness of tele-ophthalmology for diabetic retinopathy and glaucoma.[24]
Health education
Via telemedicine, RMP can impart health education for disease prevention and health promotion.[12] Via tele-ophthalmology, patients can therefore be educated regarding contagious infections, eye rubbing, contact lens usage etc. Patients can be counseled for refractive procedures, cataract surgery, requirement of close follow up in DR, corneal ulcer etc.
Professional opinion
Through telemedicine another practitioner can be consulted e.g., one ophthalmologist can connect to another for professional opinion.[12] Interdisciplinary consultations can also be taken. For example, an ophthalmologist opinion for management of ophthalmic injuries in a case of poly-trauma.
Protection against infection
In today's time of an ongoing pandemic, where social distancing is an essential to control spread of the disease, teleconsultation is a channel for patients to consult their doctor while safeguarding themselves, doctor and other patients against the contagion.
Benefits of Teleconsultation to doctors and patients have been summarized in Table 3.
Table 3.
Benefits of telemedicine and teleophthalmology
| Benefits to Health care providers |
| Widespread outreach to patients and more extensive practice |
| Promotion of hospital |
| Medium for Health education |
| Medium for counselling |
| Professional opinion |
| Interdisciplinary consultation |
| Protection against contagious infections |
| Benefits at rural level |
| Better health care facility |
| Availability of expert opinion |
| Better outcome of patients |
| Benefits to patients |
| Access to care in inaccessible areas |
| Timely access to appropriate intervention in emergency |
| Saves travel cost |
| Saves time and effort |
| Avoids unnecessary referrals to tertiary centers |
| Protection against contagious infections |
Relevance in COVID-19 Era
Teleconsultation is suited in disasters and pandemics. It enables patients to access medical care without risking the spread of disease due to personal contact.
A cross-sectional hospital based study was conducted at a multi-tier ophthalmology hospital network during COVID-19 lockdown from March 23rd to April 19th 2020. 7,008 tele-calls were addressed of which 2,805 (40.02%) patients with a clinic-related query were included in the study. They found that the most common queries were related to redness, pain, watering, blurring of vision (31.52%) and usage of medications (31.05%). 34.15% queries were related to cornea, whereas 24.74% were that of retina. 16.08% people were from lower socio-economic class. One-fourth patients were new patients (23.96%). The most common advice given to the patient was related to management of medications (54.15%) followed by appointment related (17.79%). 16.36% emergency requests required further evaluation by an ophthalmologist. Thus, they concluded that tele-consultations helped give a timely response in an ongoing lockdown due to the COVID-19 pandemic. It also highlighted the possibility of managing follow-up visits of patients by teleconsultation.[25]
Skyes surveyed adults across US to gauge their perception of and experience with telehealth in era of COVID-19. Of the 2000 adults surveyed, 1441 responders were not familial with telehealth and were excluded. Of the remaining, only 19% had tried telehealth and were satisfied with the experience. 38% were interested to adopt teleconsultation in the present scenario to avoid being in the same room as another sick person. One-third respondents in age group of 55 years and more specified that they would never like to try telehealth. Two-thirds of those who already had a telehealth appointment have had more than one. 36% liked it for no need to travel for consultation and 12% liked it for the ability to schedule appointment for the same day. Nearly three-quarter respondents preferred to use telemedicine if they had COVID-19 symptoms. Two-thirds reported that COVID-19 has increased their willingness to try telehealth in future. Those in age group of 18-24 years were more receptive towards teleconsultation, but people across all age groups were willing to try it if number of COVID-19 patients increased.[7]
According to an article published in American Journal of Ophthalmology, there has been recent increase in patient and provider interest in telemedicine. The ongoing social distancing practices are compelling many ophthalmologists to consider virtualizing their services. They also enlist mean by which visual acuity and intra-ocular pressure can be checked by the patient themselves at home.[26]
The COVID-19 outbreak has forced changes in adoption of telemedicine throughout the world. The Korean government has temporarily relaxed restriction on telemedicine consultations due to the COVID-19 outbreak. In Daegu and Seoul, telemedicine centres have been established to provide free medical treatment for self-quarantined COVID-19 patients with minor symptoms.[27]
This underlines the accelerated acceptance of teleconsultation in present scenario. Due to rising number of cases in India also, patients are not inclined to visit hospital and endanger themselves. In such situation, through tele-ophthalmology treatment can be provided wherever in-person consultation is not required. It also enables the patients to access medical care for discomforting ocular conditions where teleconsultation is sufficient. It has also been speculated that post this pandemic, there will be a “new normal”. For ophthalmology, it will be tele-ophthalmology, wherein the patients will be more willing to adopt this approach.
Guidelines
Indian Telemedicine practice guidelines are included in Appendix 5 of Indian Medical Council (Professional Conduct, Etiquette and Ethics Regulation, 2002). New guidelines in association with NITI Aayog were released on 25th March 2020.[12]
Mandatory online course will be developed which would have to be taken by any RMP wishing to practice telemedicine, within 3 years of notification. In the interim period, teleconsultation can be provided according to the following guidelines
RMP can impart healthcare using telemedicine anywhere within India
-
Teleconsultation can be provided for both emergency and non-emergency care
- Non-emergency consultation: First consult or follow up consultation can be provided
- Emergency consultation: To provide first aid where immediate in-person consultation is not available and referral for detailed in-person examination thereafter if required.
-
Telemedicine has its own set of limitations for adequate examination. Wherever essential, depending on professional judgment, the RMP shall recommend:
- Video consultation
- In-person consultation
- Examination by another RMP/Health Worker.
-
Teleconsultation should not be anonymous. Both the doctor and patient should know each other's identity
- Identification of the patient has to be done accurately Patient's name, age, address, email id, phone number, registered identification proof or any other ID as deemed to be appropriate has to be taken
- Doctor's credentials and registration number should be displayed so that the patient can confirm the same if required.
Adequate patient privacy has to be ensured
-
Patients consent is necessary for any telemedicine consultation
- Implied consent: If the patient initiates consultation, then the consent is implied, similar to an in-person setting
- Explicit consent: It is required if a RMP, health care worker or caregiver initiates consultation. An explicit consent can be recorded in any form. Patient can send an email, text or audio/video message.
Teleconsultation holds as much responsibility as an in-person consultation. In case of any uncertainty, patient should be advised in-person consultation and virtual advice should not be given
Detailed classification of drugs into groups has been given and guidelines have been laid as to which medication can be provided in a given scenario. The authors recommend that in tele-ophthalmology, certain drugs like cycloplegics and steroids should be avoided. Cycloplegics can precipitate an attack of glaucoma in a patient with shallow anterior chamber angle. Similarly, giving steroids can be hazardous as a detailed anterior segment examination is not possible on video consultation
Patient has to be given a proper prescription. RMP shall provide photo, scan or digital copy of a signed prescription or e-Prescription to the patient via email or any messaging platform
Receipt/Invoice has to be given
Maintenance of records such as case history, investigations, images, reports etc., as deemed appropriate
RMPs are not permitted to solicit patients for telemedicine through any advertisements or inducements.
*However, as per ethics, announcing the telemedicine practice and giving information to patients via message and social media is allowed. Patients can be advised to contemplate the option of teleconsultation when enquiring to fix appointment.
The United States has made an amendment to their existing telemedicine guidelines on “temporary and emergency basis”. They have expanded telehealth Medicare coverage to enable access to wider range of health care services to decrease visit to health care facility.[28]
The telehealth guidelines issued by Medical Council of New Zealand in March 2020 are similar to those of India, except those related to scope of practice. The guidelines allow a RMP to practice telehealth outside their country and similarly a practitioner from another country can also practice telehealth in New Zealand provided due registration process has been completed.[29]
Modes
The various modes of communication available are audio, video or text.[12] Any mode of consultation that is used, should follow aforementioned guidelines for medico-legal safety. According to author's experience, a dedicated mobile App, based on above mentioned guidelines is the recommended modality.
Modes of consultation[12]
-
Video consultation:
- Advantages: It is closest to an in-person consultation. Patient identification is superior with video consultation. Furthermore, when the doctor and patient see each other, they develop a better rapport as compared to isolated audio and text consultation. Also, inspection is possible and visual cues can be perceived on a video consult which assists in making diagnosis
- Disadvantages: The need for high quality internet connection and risk of abuse/misuse. Thus, ensuring privacy is extremely paramount.
-
Audio consultation:
- Advantages: It is convenient, fast, has unlimited reach, suitable for urgent cases and privacy is ensured. It does not require any special infrastructure and thus is more economical
- Disadvantages: Patient identification needs to be clearer as there are greater chances of imposters. Visual inspection is not possible.
-
Text-based consultation:
- Advantages: It is convenient and quick
- Disadvantages: It is difficult to establish rapport with the patients. Audio and visual cues are also missed. Moreover, medico-legal aspects are not taken care of in most of the text consults, as formal platforms are not used.
Although not mentioned in the guidelines, –Smart Messaging Apps such as WhatsApp etc., offer a 4th mode i.e., the hybrid mode, which is a combination of video, audio, text and image sharing. This however, is different from the dedicated tele-consult App that integrates the clinical encounter keeping all the legal requirements in consideration. This 4th modality has been used extensively across various departments in medicine even before the arrival of COVID-19.
According to interaction between individuals involved
Patient can directly approach RMP
Caregiver can approach RMP. Caregiver can obtain consultation in case the patient is a minor or debilitated, in which case explicit consent has to be taken
In remote areas, a health worker can examine the patient and organize teleconsultation with RMP. It offers an advantage of having a trained personnel with the patient who can explain the medicines and/or precautions as advised by the RMP
RMP can consult another RMP for professional opinion.
According to time of information transmitted
Real time: The doctor and patient both are present at the time of consultation and can interact with each other e.g., video consultation
Asynchronous: The patient shares his complaint and/or documents with the doctor and the doctor replies later as per his/her convenience e.g., via text message, email etc.
Tele-Ophthalmology in Various Ocular Conditions
Tele-ophthalmology has opened new avenues in today's time. But its implementation may be more relevant for some particular ocular conditions than other. In the current scenario, when tele-ophthalmology appears to be the need of the hour, we reviewed the literature for ocular conditions which can be diagnosed and treated with tele-ophthalmology and challenges faced while doing so.
Tele-ophthalmology and adnexal and orbital diseases
Diagnosis and management of adnexal and orbital diseases is possible on video consultation as inspection can be done. In Chennai, 3497 patients were provided teleconsultation in remote areas of Tamil Nadu. 101 patients (2.88%) had adnexal or orbital diseases. 18 of 101 patients required further investigations at a tertiary care center, 13 required only medical treatment whereas 72 were advised surgery. They found it was feasible to utilize teleconsultation for patients with adnexal and orbital diseases.[30]
Tele-ophthalmology and lid, conjunctival and corneal diseases
Due to visual cues available during video consultation, lid conditions like stye, chalazion etc., can be diagnosed. However, due to inability to use fluorescein stain, certain anterior segment pathologies may be difficult to address unless they are grossly visible on external examination.
University of Michigan evaluated diagnostic accuracy of detecting corneal diseases (corneal abrasion, scar, ulcer and pterygium) using photographs from two portable cameras. A cornea specialist provided Gold standard diagnosis on slit lamp and it was compared to responses from 3 cornea specialists via telemedicine. Sensitivity to detect anterior segment pathology ranged from 54% to 71% from iTouch and 66% to 75% for Nidek.[31]
Similar study done for Ocular Surface disorders found sensitivity and specificity for diagnosing conjunctival haemorrhage, zonal degeneration of cornea and eyelid tumor to be 100%. Sensitivity for pterygium, corneal scar and keratitis was 80% and specificity was 100%. For pingecula, conjunctivitis and corneal dystrophy, sensitivity was < 80%.[32]
A study in Indian Journal of Ophthalmology in 2020 studies the role of tele-ophthalmology in diagnosis and treatment of anterior segment disorders in rural areas. 5,604 patients were examined by vision technicians of which 6.9% patients were referred for teleconsultation. 45% of those who underwent teleconsultation had pathologies related to ocular surface, cornea, lid and adnexa.[33]
Tele-ophthalmology and diabetic retinopathy
Increasing burden of diabetes and its associated vision threatening complications has led to remote retinal imaging becoming one of the largest and most widely accepted applications of telemedicine principles in ophthalmology. Traditionally, retinal evaluation for diabetic retinopathy involves dilated fundus evaluation. Based on annual requirement for follow up of a patient with retinopathy and due to rapidly increasing global diabetic population, it is postulated that use of traditional method will cause time investment of over 4.5 million hours per year.[34]
Ocular images captured on fundus camera can be shared with ophthalmologists. In Chennai, non-mydriatic fundus camera were installed in diabetic clinics, general hospitals and testing centers. They used asynchronous tele-ophthalmology and found that in 80% of cases, doctors reported back within 30 minutes. Patient with diabetic retinopathy were referred to an ophthalmologist if any intervention was required.[35]
Multiple studies have reported that sensitivity (62.5% to 98.2%) and specificity (76.6% to 98.7%) for diagnosing DR using tele-ophthalmology was comparable to traditional clinical examinations.[36,37]
A study by Boucher and colleagues reported telemedicine as a reliable method for DR screening. 291 participants underwent both a complete ophthalmologic examination with pupil dilation with local ophthalmologists and non-dilated fundus imaging. 81.7% had images of sufficient quality for interpretation.[38] Using non-mydriatic fundus imaging, screening thresholds for ophthalmologic referral of mild non-proliferative DR (NPDR) and moderate NPDR had sensitivity of 97.1% and 53.3%, respectively, and specificity of 95.5% and 96.9% respectively. Eyes with severe NPDR were correctly identified 100% of the time using a screening threshold of mild retinopathy.[39]
In rural India, a cost-utility analysis was performed for DR screening using tele-ophthalmology. Patient and provider costs of DR screening via tele-ophthalmology and DR therapy were estimated through interviews with patients and hospital administrators. Findings indicated that the cost per quality-adjusted life-year (QALY) for tele-ophthalmology was cost-effective ($1320 per QALY) compared to no screening.[40]
Tele-ophthalmology and glaucoma
A study from Kenya found moderate agreement between the ability to diagnose glaucoma using tele-ophthalmology as compared to traditional examination.[41]
Meta-analysis studies reveal that tele-glaucoma can accurately discriminate between screen test results with greater odds for positive cases. It detects more cases of glaucoma than in-person examination. Thus, tele-glaucoma is an effective screening tool specifically for remote and under-served communities.[42]
Tele-ophthalmology and age related macular degeneration
Studies indicate that tele-ophthalmology for ARMD is as effective as in-person examination and increases patient participation in screening.[43] De Bats et al. reported ability of detecting ARMD using non-mydriatic digital fundus camera.[44]
Tele-ophthalmology and retinopathy of prematurity
Reviewed articles report that wide field digital imaging of premature infant retina is more competent than traditional bedside binocular ophthalmoscopy.[45] Additionally, it requires less time compared to bedside examination.[46]
The Stanford University network for Diagnosis of Retinopathy of Prematurity (SUNDROP) is an ongoing network in Northern America. A team of trained NICU nurses take infant retinal images as per recommendations and then send it for opinion. It showed sensitivity of 100% and specificity of 99.8%. It separates those without any ROP and with ROP not requiring treatment, from those with ROP that warrant intervention. The same is also used for follow-up.[47]
Karnataka Internet Assisted Diagnosis of Retinopathy of Prematurity (KIDROP) program is a well-structured tele-ROP tool in rural South India. Retinal imaging is performed by trained technicians who grade images and transfer them to experts with specially designed software to generate ROP report. The accredited technician determines on site whether the baby needs follow-up/treatment/discharge based on the triage algorithm created by experts. The rural multicenter study (2011–2015) demonstrated successful screening of 7,106 preterm infants (20,214 examination) from 36 rural NICUs in South India. The study reported that no infant in the study region developed unscreened stage 4 or 5 ROP.[20]
Tele-ophthalmology and emergency
Tele-ophthalmology has a cardinal role in emergency situations for diagnosis, treatment and prompt referral, especially in rural areas.[48] Use in emergency conditions has high sensitivity, specificity and accuracy.[49]
Tele-ophthalmology and post-operative patients
Most of the cataract patients are geriatric and have co-morbidities. In the present time, when the risk of exposure to coronavirus has accelerated, many post-operative patients may be non- compliant for follow-up.
According to previous studies, although, video consultation can detect edema at central cornea; detection of edema at corneal section and anterior chamber flare was found to be inconsistent. Descemet's membrane folds and anterior chamber cells could not be ascertained with certainty.[50] Thus, authors propose teleconsultation in asymptomatic post-operative cataract patients whereas in case of any complaints, in-person visit is required [Table 1].
Patient Satisfaction and Acceptability
Boucher and colleagues reported that patients find tele-ophthalmology to be a highly admissible method for DR screening. Patients were asked to answer questionnaire related to satisfaction after in-person consultation and after a teleconsultation. 99% were satisfied with their telemedicine experience. 82% preferred telemedicine over in-person consultation. The reasons enumerated were absence of pupil dilation, rapidity of the photographic examination, less annoyance and ease of accessibility. Only 3.2% did not trust the technology.[38]
Ease of use, low cost and decreased travel time are some factors that increase patient satisfaction while using telemedicine.[51] A study was conducted where video slit-lamp, automated perimeter, non-mydriatic fundus camera, videoconferencing system were installed in a healthcare center in rural area. While 29 patients were examined at rural center, 41 control patients were examined at city hospital. It was determined that patients in both groups were equally satisfied. 96% of the patients of rural clinic wanted follow-up at rural center only due to reduction in travelling, cost and time.[52]
Some studies suggest that patients prefer face to face care,[53] while others suggest that it is not a limiting factor for the patients.[54] Many patients prefer tele-ophthalmology as their choice of care[55] and prefer this method for future screening owing to convenience and decreased consultation time.[56]
Experience with App based Teleconsultation
An elaborate study published in 2017 was conducted in 2 phases. In the first phase, requirement analysis was done in which users' requirements were investigated. Data elements that were important as per the users were under 4 main categories: patient identifying information, patient clinical information, optometrist's information, and specialist's information. Patient clinical information includes disease history, family history, allergies and eye images. For optometrist's information, their medical council unique number and phone number were found to be necessary. For specialist's information, medical council unique number, phone number and workplace address were reported necessary. Similarly, the feasibility of uploading images, searching records and prescribing were considered necessary by most specialists. In the second phase, based on the results of the first phase a prototype was developed and usability testing was conducted. The study established that any teleconsultation mode that addresses the requirements of the care giver and is easy to operate will have a wider acceptability.[57]
EyeSmart EMR app for tele-ophthalmology consultations was provided to 15,001 patients from vision centers from January 2017 to August 2018 by LVPEI. They concluded that the use of technology played a vital role in appropriate medical management as it connected patients at rural areas and ophthalmologists at higher centers.[21]
In the current era, majority of the people are familiar with mobile phone and its applications. Online shopping, food delivery, cab booking, bill payments etc., is becoming the new norm. In the last five years, the Indian internet has matured both in terms of demography and geography.[58] India had 451 million monthly active internet users as on 31st March 2019, second only to China, according to a report by Internet and Mobile Association of India.[59] Population of above 25 years of age on the Indian web has grown from 40% in 2013 to 54% in 2018. The rural-urban divide seems to have blurred in terms of internet users. Penetration has increased, with rural and semi-urban audiences constituting 40-50% of user base, up from 29% 5 years ago.[58] According to Telecom Regulatory Authority of India (TRAI), there were 449 million mobile subscriptions in rural India as if June 2017 of which 109 million users owned smartphones. In 2013, smartphone penetration in India was at 6.3% and grew to 23.8% by end of 2018. It has been projected that 60% of country's population would have smartphones and fast & reliable data connectivity by 2025.[58] In terms of revenue the healthcare apps market in India was valued at INR 27.01 billion in 2018 and is estimated to reach INR 138.0 billion by 2024 expanding at a compound annual growth rate (CAGR) of approximately 31.61% during the 2019-2024 period.[60] This shows that the access to smart phones and internet connectivity has increased both in urban and rural areas. This means that the teleconsultation can be adopted more widely presently than earlier.
Various features need to be present in the mobile app based consultation that safeguards the interest of the doctor and patient. Current platforms facilitate patients for access to user friendly tele-ophthalmology. Technology helps in initial registration, procurement of identity, booking appointments, sending confirmatory messages and reminders. Part of the process that technology cannot do is done by the front desk like sending push messages and helping those who are not very familiar with use of technology. There is currently a surge of such solutions where the ophthalmologist is free to give only consultations and not be much involved in the technology. This is an ideal setting to get started with teleconsultation.
There are certain challenges present with the use of a telemedicine app. Although people are familiar with the use of mobile phones, but the use of telehealth related apps is new. Thus, lack of awareness poses difficulty to accept use of this technology. Thus, although the apps are self-explanatory, we recommend that a trained personnel at the front desk should explain the patients who visit for in-person consultation on how to register and use the teleconsultation app. This will increase the awareness and make patients more comfortable to use it in future for follow-up consultations. Also, in the present scenario of a pandemic, a pre-consultation screening video call can be done by the front desk to check for any history of travel, fever etc., On the same call, if the ophthalmologist is satisfied that the patient can be treated by teleconsultation, then in-person consult can be avoided.
Also, security and privacy of the patient has to be ensured. An agreement should be signed between the doctor and vendor to ensure no breach in confidentiality. Similarly, terms and conditions of using this mode of consultation also has to be displayed on the home page of the App and consultation given only after patient agrees with the terms. Thus, as far as possible, secrecy has to be maintained. According to the guidelines, RMP will not be held responsible for breach of confidentiality if there is a reasonable evidence to believe that patient's privacy and confidentiality has been compromised by technology breach or by another person. The RMPs should ensure that reasonable degree of care was undertaken during hiring such services.[11]
Good internet speed and quality is required for a satisfactory teleconsultation experience. But the option should be available in the app to convert a video consultation to audio consultation in case the video quality is not good due to poor quality internet.
Also, the patient's clinical information, reports, prescription etc., should be stored on the App. Also, the App should be linked with the hospital EMR so that the relevant information can be extracted whenever required.
Conclusion
Based on the review, we can conclude that lack of awareness and acceptance of new technology, both by the public and the professionals, is what is holding back wider use of tele-ophthalmology. According to the data, in India, there are 9 ophthalmologists for every million people in contrast to US, where there are 81 ophthalmologists for every million people.[35] Tele-ophthalmology is a solution for patients, who would otherwise not have access to an eye care professional, to be screened and treated earlier to prevent permanent visual complications. Earlier, telemedicine was developed as a model to provide health care to inaccessible areas; but now it encompasses both rural and urban areas. Due to less time consumption and convenience of seeking consultation, it has also improved compliance for follow-up.[61] Tele-ophthalmology can go a long way in providing care and consultation to patients in remote areas and in cases where in-person consultation is not indispensable.
The present review gives a holistic synopsis of the present attitude towards adoption of teleconsultation, its advantages and barriers.
Our review had some limitations. Articles in languages apart from English could not be reviewed. Also, there is dearth of articles on use of tele-ophthalmology specifically during COVID-19 pandemic. This is the first pandemic that we all are facing, thus for future preparedness, application of tele-ophthalmology in a pandemic needs to be evaluated in greater detail.
In the present scenario of COVID-19, tele-ophthalmology has a larger application. The current experience so far since the easing of the lockdown is the stark decline in the consults over the past 3 weeks. Patients are increasingly approaching the hospital instead of the remote consult due to its attending limitations. This will continue to evolve as the pandemic COVID-19 new cases wax and wane. Hospitals are at about 40% capacity already. Currently, the proportion of new patients seen through such a modality is 20%.
Ongoing social distancing practices is compelling ophthalmologists to consider virtualizing their practice. Implementation of systems to use it in the present scenario provides a means for providing care to patients and also gives an opportunity to get acquainted to it so that it can be used in the future also. Hopefully, in the future tele-ophthalmology will be utilized more and will reach its full potential.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nesbitt TS. The Evolution of Telehealth: Where Have We Been and Where Are We Going National Academies Press (US); 2012 Bookshelf ID: NBK207141 [Google Scholar]
- 2.Grisolia ABD, Abalem MF, Lu Y, Aoki L, Matayoshi S. Teleophthalmology: Where are we now? Arq. Bras Oftalmol. 2017;80:401–6. doi: 10.5935/0004-2749.20170099. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth [Internet] Geneva, Switzerland: World Health Organization; 2010. [Last accessed on 2020 May 14]. p. 93. (Global Observatory for eHealth Series) Available from: http://wwwwhoint/goe/publications/goe_telemedicine_2010pdf . [Google Scholar]
- 4.Woodward MA, Ple-Plakon P, Blachley T, Musch DC, Newman-Casey PA, De Lott LB, et al. Eye care providers' attitude towards tele-ophthalmology. Telemedicine J E Health. 2015;21:271–3. doi: 10.1089/tmj.2014.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.All India Ophthalmological Society. 2020 Survey on Telemedicine AIOS Teleophthalmology platform Unpublished data [Google Scholar]
- 6.Liu Y, Zupan NJ, Swearingen R, Jacobson N, Carlson JN, Mahoney JE, et al. Identification of barriers, facilitators and system based implementation strategies to increase teleophthalmology use for diabetic eye screening in a rural US primary care clinic: A qualitative study. BMJ Open. 2019;9:e022594. doi: 10.1136/bmjopen-2018-022594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siwicki B. [Last accessed on 2020 May 14];2020 April 03 Survey-americans- perceptions- telehealth-covid19-era. Available from survey-americans- perceptions-telehealth-covid19-era. [Google Scholar]
- 8.Gomez-Ulla F, Alonso F, Aibar B, Gonzalez F. A comparative cost analysis of digital fundus imaging and direct fundus examination for assessment of diabetic retinopathy. Telemed J EHealth. 2008;14:912–8. doi: 10.1089/tmj.2008.0013. [DOI] [PubMed] [Google Scholar]
- 9.Mansberger SL, Sheppler C, Barker G, Gardiner SK, Demirel S, Wooten K, et al. Long-term comparative effectiveness of telemedicine in providing diabetic retinopathy screening examinations: A randomized clinical trial. JAMA Ophthalmol. 2015;133:518–25. doi: 10.1001/jamaophthalmol.2015.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2016;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bali S. Barriers to development of telemedicine in developing countries. Telehealth. doi: 105772/intechopen 81723. [Google Scholar]
- 12.Board of Governors in supersession of the Medical Council of India. Telemedicine Practice Guidelines. 2020. Mar, [Last accessed on 2020 May 14]. Available from: https://wwwmohfwgovin/pdf/Telemedicinepdf .
- 13.Wade V, Elliot J. The role of the champion in telehealth services development: A qualitative analysis. J Telemed Telecare. 2012;18:490–2. doi: 10.1258/jtt.2012.gth115. [DOI] [PubMed] [Google Scholar]
- 14.Shiferaw F, Zolfo M. The role of information communication technology (ICT) towards universal health coverage: The first steps of a telemedicine project in Ethiopia. Global Health Action. 2012;5:1–8. doi: 10.3402/gha.v5i0.15638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall JL, McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff (Millwood) 2014;33:216–21. doi: 10.1377/hlthaff.2013.0997. [DOI] [PubMed] [Google Scholar]
- 16.Sagaro GGG, Battineni G, Amenta F. A Review on Barriers to Sustainable Telemedicine Implementation in Ethiopia. ResearchSquare. doi: 10.1089/tmr.2020.0002. doi: 1021203/rs 215424/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stumf SH, Zalunardo RR, Chen RJ. Barriers to Telemedicine Implementation. Healthc Inform. 2002;19:45–8. [PubMed] [Google Scholar]
- 18.John S, Sengupta S, Reddy SJ, Prabhu P, Kirubanandan K, Badrinath SS. The Sankara Nethralaya mobile teleophthalmology model for comprehensive eye care delivery in rural India. Telemed J E Health. 2012;18:382–7. doi: 10.1089/tmj.2011.0190. [DOI] [PubMed] [Google Scholar]
- 19.Prathiba V, Rema M. Teleophthalmology: A model for eye care delivery in rural and underserved areas of India. Int Fam Med. 2011;2011:683267. doi: 10.1155/2011/683267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vinekar A, Jayadev C, Mangalesh S, Shetty B, Vidyasagar D. Role of tele-medicine in retinopathy of prematurity screening in rural outreach centers in India – A report of 20,214 imaging sessions in the KIDROP program. Semin Fetal Neonatal Med. 2015;20:335–45. doi: 10.1016/j.siny.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Das AV, Mididoddi S, Kammari P, Deepthi Davara N, Loomba A, Khanna R, et al. App-based tele ophthalmology: A novel method of rural eye care delivery connecting tertiary eye care center and vision centers in India. Int J Telemed Appl. 2019;2019:8107064. doi: 10.1155/2019/8107064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wedekind L, Sainani K. Supply and Perceived Demand for Teleophthalmology in Triage and Consultations in California Emergency Departments. JAMA Ophthalmol. 2016;134:537–43. doi: 10.1001/jamaophthalmol.2016.0316. [DOI] [PubMed] [Google Scholar]
- 23.Torres E, Morales PH, Bittar OJNV, Mansur NS, Salomão SR, Belfort RJ. Teleophthalmology support for primary care diagnosis and management. Med Hypothesis DiscovInnov Ophthalmol. 2018;7:57–62. [PMC free article] [PubMed] [Google Scholar]
- 24.Sharafeldin N, Kawaguchi A, Sundaram A, Campbell S, Rudnisky C, Weis E. Review of economic evaluations of Tele ophthalmology as a screening strategy for chronic eye diseases in adults. Br J Ophthalmol. 2017;102:1485–91. doi: 10.1136/bjophthalmol-2017-311452. [DOI] [PubMed] [Google Scholar]
- 25.Das AV, Rani PK, Vaddavalli PK. Tele-consultations and electronic medical records driven remote patient care: Responding to the COVID-19 lockdown in India. Indian J Ophthalmol. 2020;68:1007–12. doi: 10.4103/ijo.IJO_1089_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saleem SM, Louis R, Sidoti PA, Tsai JC. Virtual ophthalmology: Telemedicine in a COVID-19 era. Am J Ophthalmol. 2020 doi: 10.1016/j.ajo.2020.04.029. doi: 101016/jajo 202004029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ellis D. Telemedicine- Necessity is the mother of adoption-But barriers remain. [Last accessed on 2020 May 14]. Available from: https://wwwmondaqcom/hongkong/healthcare/929614/telemedicine- necessity-is-the-mother-of-adoption- but-barriers-remain .
- 28.American Medical Association. March 19, 2020. Key changes made to telehealth guidelines to boost COVID-19 care. [Last accessed on 2020 May 14]. Available from https://www.ama-assn.org/delivering-care/public-health/key-changes-made-telehealth-guidelines-boost-covid-19-care .
- 29.Medical Council of New Zealand. March 2020. Telehealth. [Last accessed on 2020 May 14]. Available from: https://www.mcnz.org.nz/assets/standards/06dc3de8bc/Statement-on-telehealthv3.pdf .
- 30.Verma M, Raman R, Mohan RE. Application of tele-ophthalmology in remote diagnosis and management of adnexal and orbital diseases. Indian J Ophthalmol. 2009;57:381–4. doi: 10.4103/0301-4738.55078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Woodward MA, Musch DC, Hood CT, Greene JB, Niziol LM, Jeganathan VSE, et al. Teleophthalmic approach for detection of corneal diseases: Accuracy and reliability. Cornea. 2017;36:1159–65. doi: 10.1097/ICO.0000000000001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liang QF, Li R, Pan ZQ, Deng SJ, Li JJ, Xu L, et al. The clinical specificity and sensitivity of tele-ophthalmology screening for ocular surface disease based on fundus photography. Research Gate. 2016;25:260–4. [Google Scholar]
- 33.Misra N, Khanna RC, Mettla AL, Marmamula S, Rathi VM, Das AV. Role of teleophthalmology to manage anterior segment conditions in vision centres of South India: EyeSmart Study 1. Indian J Ophthalmol. 2020;68:362–7. doi: 10.4103/ijo.IJO_991_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tayapad JB, Bengzon AU, Valero SO, Arroyo MH, Papa RTM, Fortuna EJS, et al. Implementation and pilot data on diabetic retinopathy in a teleophthalmology program at a multispecialty primary care clinic. Philipp J Ophthalmol. 2014;39:90–3. [Google Scholar]
- 35.Senthil T, Nainappan M. Tele-ophthalmology: A successful model to tackle diabetic retinopathy. TNOA J Ophthalmic Sci Res. 2017;55:131–3. [Google Scholar]
- 36.Surendran TS, Raman R. Teleophthalmology in diabetic retinopathy. J Diabetes Sci Technol. 2014;8:262–6. doi: 10.1177/1932296814522806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liesenfeld B, Kohner E, Piehlmeier W, Kluthe S, Aldington S, Porta M, et al. A telemedical approach to the screening of diabetic retinopathy: Digital fundus photography. Diabetes Care. 2000;23:345–8. doi: 10.2337/diacare.23.3.345. [DOI] [PubMed] [Google Scholar]
- 38.Boucher MC, Nguyen QT, Angioi K. Mass community screening for diabetic retinopathy using a nonmydriatic camera with telemedicine. Can J Ophthalmol. 2005;40:734–42. doi: 10.1016/S0008-4182(05)80091-2. [DOI] [PubMed] [Google Scholar]
- 39.Boucher MC, Gresset JA, Angioi K, Olivier S. Effectiveness and safety of screening for diabetic retinopathy with two nonmydriatic digital images compared with the seven standard stereoscopic photographic fields. Can J Ophthalmol. 2003;38:557–68. doi: 10.1016/s0008-4182(03)80109-6. [DOI] [PubMed] [Google Scholar]
- 40.Rachapelle S, Legood R, Alavi Y, Lindfield R, Sharma T, Kuper H, et al. The cost-utility of telemedicine to screen for diabetic retinopathy in India. Ophthalmology. 2013;120:566–73. doi: 10.1016/j.ophtha.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 41.Kiage D, Kherani IN, Gichuhi S, Damji KF, Nyenze M. The muranga tele-ophthalmology study: Comparison of virtual (teleglaucoma) with in-person clinical assessment to diagnose glaucoma. Middle East Afr J Ophthalmol. 2013;20:150–7. doi: 10.4103/0974-9233.110604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomas SM, Jeyaraman MM, Hodge WG, Hutnik C, Costella J, Malvankar-Mehta MS. The effectiveness of teleglaucoma versus in patient examination for glaucoma screening: A systematic review and meta-analysis. PLoS One. 2014;9:e113779. doi: 10.1371/journal.pone.0113779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kawaguchi A, Sharafeldin N, Sundaram A, Campbell S, Tennant M, Rudnisky C, et al. Tele-ophthalmology for age-related macular degeneration and diabetic retinopathy screening: A systematic review and meta-analysis. Telemed J E Health. 2018;24:301–8. doi: 10.1089/tmj.2017.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Bats F, VannierNitenberg C, Fantino B, Denis P, Kodjikian L. Age-related macular degeneration screening using a nonmydriatic digital color fundus camera and telemedicine. Ophthalmologica. 2014;231:172–6. doi: 10.1159/000356695. [DOI] [PubMed] [Google Scholar]
- 45.Sreelatha OK, Ramesh SV. Teleophthalmology: Improving patient outcomes? Clin Ophthalmol. 2106;10:285–95. doi: 10.2147/OPTH.S80487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richter GM, Sun G, Lee TC, Chan RV, Flynn JT, Starren J, et al. Speed of telemedicine versus ophthalmoscopy for retinopathy of prematurity diagnosis. Am J Ophthalmol. 2009;148:136–42e2. doi: 10.1016/j.ajo.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang SK, Callaway NF, Wallenstein MB, Henderson MT, Leng T, Moshfeghi DM. SUNDROP: Six years of screening for retinopathy of prematurity with telemedicine. Can J Ophthalmol. 2015;50:101–6. doi: 10.1016/j.jcjo.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 48.Kumar S, Yogesan K, Hudson B, Tay-Kearney ML, Constable IJ. Emergency eye care in rural Australia: Role of internet. Eye. 2006;20:1342–4. doi: 10.1038/sj.eye.6702104. [DOI] [PubMed] [Google Scholar]
- 49.Ribeiro AG, Rodrigues RA, Guerreiro AM, Regatieri CV. A teleophthalmology system for the diagnosis of ocular urgency in remote areas of Brazil. Arq Bras Oftalmol. 2014;77:214–8. doi: 10.5935/0004-2749.20140055. [DOI] [PubMed] [Google Scholar]
- 50.Smith LF, Bainbridge J, Burns J, Stevens J, Taylor P, Murdoch I. Evaluation of telemedicine for slit lamp examination of the eye following cataract surgery. Br J Ophthalmol. 2003;87:502–3. doi: 10.1136/bjo.87.4.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open. 2017;7:e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tuulonen A, Ohinmaa T, Alanko HI, Hyytinen P, Juutinen A, Toppinen E. The application of teleophthalmology in examining patients with glaucoma: A pilot study. J Glaucoma. 1999;8:367–73. [PubMed] [Google Scholar]
- 53.Lee JY, Du YE, Coki O, Flynn JT, Starren J, Chiang MF. Parental perceptions toward digital imaging and telemedicine for retinopathy of prematurity management. Graefes Arch ClinExp Ophthalmol. 2010;248:141–7. doi: 10.1007/s00417-009-1191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kumar S, Tay-Kearney ML, Constable IJ, Yogesan K. Internet based ophthalmology service: Impact assessment. Br J Ophthalmol. 2005;89:1382–3. doi: 10.1136/bjo.2005.072579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paul PG, Raman R, Rani PK, Deshmukh H, Sharma T. Patient satisfaction levels during teleophthalmology consultation in rural South India. Telemed J E Health. 2006;12:571–8. doi: 10.1089/tmj.2006.12.571. [DOI] [PubMed] [Google Scholar]
- 56.Kurji K, Kiage D, Rudnisky CJ, Damji KF. Improving diabetic retinopathy screening in Africa: Patient satisfaction with teleophthalmology versus ophthalmologist-based screening. Middle East Afr J Ophthalmol. 2013;20:56–60. doi: 10.4103/0974-9233.106388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ayatollahi H, Nourani A, Khodaveisi T, Aghaei H, Mohammadpour M. Teleophthalmology in practice: Lessons learned from a pilot project. Open Med Inform J. 2017;11:20–8. doi: 10.2174/1874431101711010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Economic Times. Feb 9, 2019. The changing face of the Indian Mobile User. [Last accessed on 2020 Jun 09]. Available from: https://meconomictimescom/small-biz/marketing-branding/marketing/the- changing-face-of-the-indian-mobile-user/articleshow/67912326cms .
- 59.Abhijit Ahaskar. 26 September 2019. India has second-largest population of monthly active internet users: Report. [Last accessed on 2020 Jun 09]. Available from: https://www.livemint.com/technology/tech-news/india-has-second-largest-population-of-monthly-activeinternet-users-report-1569500591581.html .
- 60.Research and markets. September 2019. Healthcare Apps Market in India 2019. [Last accessed on 2020 Jun 09]. Available from: https://www.researchandmarkets.com/reports/4988984/healthcare-apps-market-in-india-2019 .
- 61.Chin EK, Ventura BV, See KY, Seibles J, Park SS. Nonmydriatic fundus photography for teleophthalmology diabetic retinopathy screening in rural and urban clinics. Telemed J E Health. 2014;20:102–8. doi: 10.1089/tmj.2013.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]


