Abstract
Cataract is the second leading cause of preventable blindness on the globe. Several programs across the country have been running efficiently to increase the cataract surgical rates and decrease blindness due to cataract. The current COVID-19 pandemic has led to a complete halt of these programs and thus accumulating all the elective cataract procedures. At present with the better understanding of the safety precautions among the health care workers and general population the Government of India (GoI) has given clearance for functioning of eye care facilities. In order to facilitate smooth functioning of every clinic, in this paper, we prepared preferred practice pattern based on consensus discussions between leading ophthalmologists in India including representatives from major governmental and private institutions as well as the All India Ophthalmological Society leadership. These guidelines will be applicable to all practice settings including tertiary institutions, corporate and group practices and individual eye clinics. The guidelines include triage, use of personal protective equipment, precautions to be taken in the OPD and operating room as well for elective cataract screening and surgery. These guidelines have been prepared based on current situation but are expected to evolve over a period of time based on the ongoing pandemic and guidelines from GoI.
Keywords: Cataract, COVID-19, Pandemic, Phacoemulsification, SARS-CoV-2
Cataract is the second leading cause of preventable blindness on the globe. Among the global population (2015) with moderate or severe vision impairment and blind, cataract accounted for 52·6 million and 12·6 million, respectively. By 2020, among the global population with moderate or severe vision impairment and blindness the number of people with cataract is anticipated to increase to 57·1 million and 13·4 million respectively.[1,2,3] In order to decrease the burden of visual impairment or blindness due to cataract there has been a lot of emphasis on improving the cataract surgical coverage and cataract surgical rates in India by various national and international agencies.[4] In spite of the all these efforts, cataracts continue to be a major cause of visual impairment and blindness and due to rapidly aging population.[4]
Recent data (2018-2019) from National Programme for Control of Blindness (NPCB) shows that on an average about 557,568 cataract surgeries are performed per month in India. The recent onset of COVID-19 pandemic has led to the closing of the screening programme and surgical centres across the country thus further compromising the achievement of set goals.
India reported its first case of corona virus on 30th January 2020 and the number of positive cases kept on increasing over time which has led to the declaration of nationwide lockdown from 24th March 2020 affecting 1.3 billion population. The entire nation has shut all the elective medical care services with a lot of uncertainty. The entire health care fraternity and the government spent most of the time, energy and the resources in overcoming the current emergency situation. As of today (13th May 2020), India has been under lockdown for about 51 days and according to NPCB data (2018-2019) approximately 947,866 cataract surgeries which had to be performed have been pending.
In spite of phenomenal advances that humanity and technology have brought to our lives, we are still unable to predict the onset of new epidemics and pandemics of infectious diseases. These encounters would not only cause immediate changes, but also have long term socioeconomic impact on all affected countries. At this juncture it is important for us to ensuring skilled and trained ophthalmic HCWs at all levels of care to prevent transmission of the novel coronavirus. There are several things about the current COVID-19 pandemic that are not well understood and hence the guidelines have been evolving over a period of time. Different countries have adopted various strategies and these could lead to variation in the safety protocols. In India, with better understanding of the spread of the disease and after establishment of safety protocols to contain the disease, the Ministry of Health and Family Welfare (MoHFW) and Government of India (GoI) have released guidelines for restoration of medical services across the country.[5] Earlier necessary guidelines have been published for functioning of ophthalmic facilities.[6,7] In order to remain safe, investing in preparedness can mean little but can impact a lot of patients by restoring good vision. In this article, we are hereby attempting to propose guidelines that could be followed to start screening and operating on patients with cataracts.
Methods
These guidelines outline the infection prevention and control advice for ophthalmologists and health care workers (HCWs) involved in the treatment of patients for ophthalmic care. These guidelines are based on the available literature and guidelines issued from the MoHFW, GoI and Indian Council of Medical Research (ICMR). With the evolving situation on COVID-19, further updates may be made to this guidance as and when required. An invitation to review these guidelines was sent out by email to eminent ophthalmologists across India, including heads of the major teaching institutions, both in government and private sectors. The experts suggested several changes in the base document that was collated, and a consensus was arrived at. Disagreements on guidelines were resolved by discussion between members.
Cataract Surgery Guidelines
General safety involved in opting for health care
The most important factor preventing heath care workers form starting routine work is the risk of cross infection. COVID-19 is a highly contagious virus in humans and its basic reproduction number (R0- average number of people who will catch the disease from one infected person), was calculated to be between 2.24 and 3.58.[8] However, this could vary from country to country based on cultural profiles, stringent measures taken by the respective governments to prevent cross infection. Risk profiling of districts has been done by the MoHFW and GoI into red (hotspot), orange, and green zones.[5] This has been done based on the following guidelines:
Green Zones: Districts with zero confirmed case as of 1st May 2020 or districts with no confirmed cases in the last 21 days
Red zones/Hotspot districts: This is based on the total number of active cases, doubling rate of confirmed cases, extent of testing and surveillance feedback.
Orange Zone: Districts that are neither in green or red zones. In a district labelled as orange zone can have MC with no confirmed case in the last 21 days and these areas can be labelled as green zone.
Containment zone: These are the areas located in the orange or red zones and the district administration taking measures to make sure there is no movement of people unless an emergency.
The GoI has provided for some relaxation to the routine activities to restore normalcy based on the zones with necessary precautions. Except for in containment zones, medical facilities can function normally in the red, orange and green zones with necessary social distancing and safety precautions.[5]
Since there is a variability in the location of patient and the location of clinic/surgical center according to the recent risk profiling by the GoI, the probable risk of cross infection is possible when a patient from a red or orange zone travel to a surgical centre located in any zone. The possibility of cross infection may be least when a patient from a green zone opts for surgical care at a surgical centre in green zone [Fig. 1]. This risk profiling definitely emphasises the importance of safety precautions proposed for MoHFW for every patient irrespective of the zone they travel from or opt for health care in any zone.
Figure 1.
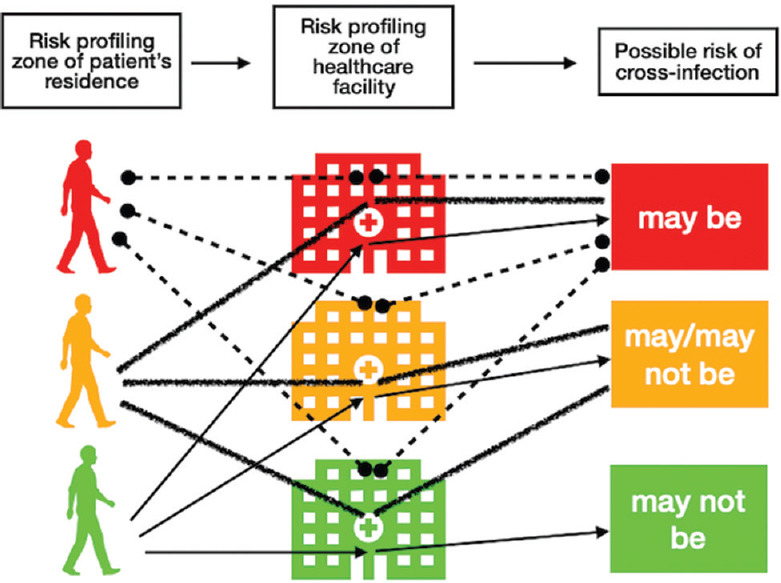
Picture showing a possible risk of cross infection with patients and health care facilities located in different risk profile zones
Prerequisites for functioning of the clinic
Planning
Identify minimum number of staff needed to function
Identify and physically delineate areas based on the flow of the patients
Availability of standard personal protective equipment (PPE)
Anticipate influx of patients from time to time.
It is very important to minimize the amount of time the patient spends in the clinic and also decrease the number of visits that the patient has to make to the clinic. The following measures may help in decreasing and minimizing waiting time and the number of visits to the clinic:
Fixing appointments and function with a fixed number of patients per hour to minimize the number of patients and their family in the waiting halls
To consider taking history of any symptoms of active COVID-19 and also of any contact primary/secondary contacts
Emphasize that the patient and the attendant are mandated to download the Aarogya Setu COVID-19 tracking app by the GoI and register with their mobile number for possible future digital tracking
Every patient and attendant should pass through the triage area with appropriate partition and every patient is assessed for the risk of being COVID-19 positive. If the patient has any symptoms or signs of COVID-19 they should be referred to designated COVID-19 hospitals. There may be a need for multiple stations based on number of patients seen
Temperature by non-contact method is recorded for every patient and attendant
Previous medical records can be shared over email prior to the appointment which could help the ophthalmologist to review the records without having contact of the same and also decrease the time in the clinic
Make provisions to implement social distancing at each time point (reception, waiting areas and pharmacy)
All elevators to have demarcation lines and ensure patients are standing facing walls. The number of people in each elevator at any given time can be decided based on the space available
Limit to one accompanying adult with the patient in waiting rooms or examination rooms
Online payment methods to be explored to minimize the contact with currency.
Safety precautions to be taken in the clinic
All planning bodies involved have been aiming at taking appropriate steps to slow the spread of the virus. The most important factor that can prevent cross infection is social distancing and it have been proven to reduce the severity of illness and mortality.[9] The current data suggests that the incubation period ranges from day 1-14 with peak being at 5-7 days. Patient may have the ability of transmitting the virus 1-2 days before the onset of symptoms. Hence, it is important to consider every patient having potential of spreading the virus.[10] It is mandatory to follow the necessary measures at every point of time in the clinic as well.[11]
Patient-related
Every patient should be informed about the importance of appointment time
All should have a mask or equivalent (patients & attendants)
All should use sanitizer to disinfect the hands at the entry
Minimize baggage to the clinic
Avoid touching face with hands
To be seated in designated seats only
Avoid talking to other patients/attendants
Age: It has been shown that elderly population and those with comorbidities had a very high mortality rate.[12] It would be appropriate to make sure that patient with coexisting comorbidities (uncontrolled blood pressure or diabetes, chronic lung disease, obesity, asthma, and those whose immune system is compromised such as by chemotherapy for cancer) are seen on priority to minimize their stay in the clinic
It is imperative that layered social-distancing interventions may be a more acceptable long-term solution to the current pandemic.
Employees
All staff should have the mask and hand gloves on at each time point. The use of face shield may aid in preventing direct spillage of aerosols[13,14,15,16]
Minimise onsite waiting time/patient journey time
Keep the doors open to allow free flow of air and minimize the contact with doorknobs
Avoid accompanying relatives in examination rooms unless absolutely necessary
Reduce workforce-patient contact time
Keep more than one meter away from patients except where clinical examination is performed
Avoid speaking at the slit lamp
Keep the examination brief and pertinent to the decision making required
Avoid re-examination of patients who have already been assessed
Avoid investigations unless critical to decision making
Use treatment changes that can reduce the frequency of required visits for the next few months
Clean all surfaces (chair units, stool, slit lamp, desk, keyboard, computer monitor, trial frame) with specified cleaning solution before starting clinics. Same should be repeated after each patient examination. Sodium hypochlorite solution in spray bottles to be sprayed on chair and stools as well as desks and alcohol swab for slit lamp, and keyboard)
Hand sanitizing protocol are followed without fail during the examination, and also in between patient examinations.
Screening patients for cataract surgery
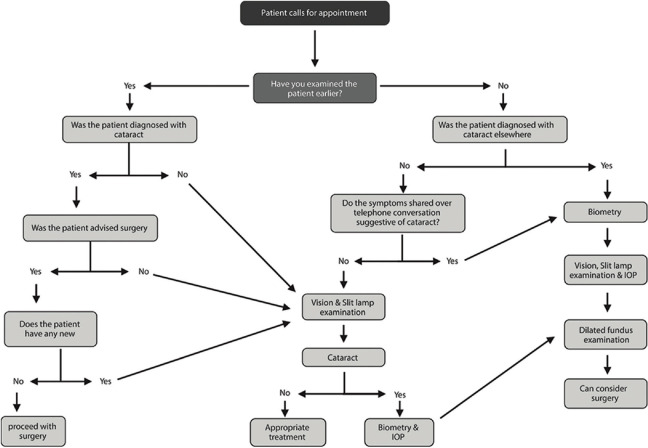
The lockdown was a decision that was announced with minimal time to plan as it was the need of the hour. Patients that had a prior ocular examination and are due for cataract surgery may be considered for surgery without the need for additional examination thus avoiding further contact. Further examination may be required in case the patients who had been examined earlier have symptoms that cannot be explained due to cataract. During telephone conversations, if the patient reveals of having been diagnosed of cataract or symptoms suggestive of cataract, then the patient may have biometry done and proceed further for ocular examination. If there is clarity of the presence of a cataract for a patient, it would be appropriate for them to be examined first before performing any diagnostic test [Fig. 2]. In every clinic, the responsibilities of the ophthalmologist, optometrist and technician should be clearly distributed and followed. The close contact to the patient and instillation of the drops should be done by only an ophthalmologist or a trained optometrist. It would be appropriate to avoid any trainees involved in the patient care for a next few weeks.
Figure 2.
A flow chart that would guide screening patients with cataract and their flow in the clinic
Examination protocols
Ophthalmologists/Optometrists are at a higher risk of being exposed to aerosolized particles from respiratory droplets of the patient due to close proximity during slit-lamp biomicroscopy examination.[17,18] We have lost eminent ophthalmologists like Dr Li Wenliang who were exposed to the virus after treating asymptomatic patients.[19] As of today, we have only anecdotal reports of presence of viral RNA.[19,20,21] The following safety protocols may aid in decreasing the possibility of developing cross infection.
-
History:
To maintain distance while talking to the patient and the mask may always be kept on while talking. Minimize the need to touch the documents from patient. One may ask patients to share the necessary documents through email before the appointment, if possible.
-
Visual Acuity:
Distance: When testing visual acuity, may start from the lowest achievable line to speed things up. Avoid using an occluder and request patients to close the non-testing eye with their palm after using sanitizer. At least one-meter distance from the patient should be maintained while assessing visual acuity
Near: One may hold the near vision chart with gloved hands at an appropriate distance instead of the patient holding it. Complete the procedure of assessing near vision while standing so that examiner is at a higher level compared to that of the patient
Manifest Refraction: It should be performed wherever necessary. Avoid touching the forehead of the patient to measure working distance. The trial frame, pinhole occluder and all lenses used should be wiped with alcohol swab before bringing the next patient and provide sufficient time to make surface of these instruments dry
Intraocular Pressure (IOP)[22]: IOP should be performed only there are signs of increased IOP or patient on steroids or planning cataract surgery. Using Shiotz tonometry or Icare tonometry or Goldmann applanation tonometry (GAT) or tonopen with disposable sleeves will minimize the risk of cross infection. The GAT prism to be wiped with alcohol between every case and with 1:10 sodium hypochlorite at the beginning and end of the day. Non-contact tonometry should be avoided as it is an aerosol-generating procedure
Gonioscopy should be avoided wherever possible. It should be performed only by an ophthalmologist. The lens should be washed with soap and water after every case and clean with alcohol wipe before performing the test
Slit lamp examination: It would be appropriate to minimize the number of HCWs coming on close proximity to the patient. Only one person should perform slit lamp examination. The breath shields available commercially will minimize the risk of aerosol contamination by acting as a barrier between patient and ophthalmologist. All the surfaces should be cleaned before examining the next patient
Lacrimal sac evaluation: It is important to check the patency of the lacrimac sac prior to cataract surgery. This can be tested by regurgitation on pressure over the lacrimal sac (ROPLAS) or a micro-reflux test using flourescein dye.[23,24] Both these tests require pressure on the lacrimal sac and hence it is very important to make sure gloves are used during these procedures. In cases of suspicious case of chronic nasolacrimal duct obstruction or chronic dacryocystitis, it is advisable to postpone cataract surgery. It is preferable to avoid lacrimal syringing as it is an aerosol generating procedure
Fundus examination: It should be performed prior to performing a cataract surgery and all patients postoperatively where a retinal pathology is suspected or if the retina was not visualized prior to the cataract surgery. Indirect ophthalmoscope with a breath shield should be considered. Central retina can also be examined using 90D or 78D lenses at the slit lamp. It is advisable to not to use a direct ophthalmoscope
Nd:YAG Capsulotomy: It can be considered wherever necessary. The breath shield should be installed as a barrier between the patient and the ophthalmologist.
Diagnostics in cataract surgery
General Guidelines:
Patient to be allowed into the diagnostic room only after wearing mask covering the nose and mouth of the patient
Hand sanitizer to be made available in the diagnostic room
Both the patient and the technician should sanitize hands before proceeding for the scan
Only one patient along with an attender to be allowed into the diagnostics room
All instruments preferably should have a breath shield attached with an opening for the eyes or around the instrument panel
All instruments in diagnostic area to be cleaned once in the morning before the start of OPD and once in evening after the completion of OPD. This includes the wire connection and the all instrument panel surfaces
Minimal touching of surfaces by the patient and attender in the diagnostic premises.
Ultrasound Biometry: The tip of the probe should be cleaned with alcohol swab after every case and sufficient time to dry should be given. In case of use of immersion scan, it may be advisable to use clean fluid and also clean the Prager shell along with the probe.
Keratometry: To measure the keratometry any keratometer can be used. The breath shield can be customized and placed as a barrier. The joystick, locking screw for the instrument base, head rest, chin rest, handlebar should be cleaned using alcohol swab after examining each patient.
Optical Biometry: It is the preferable method for measuring the eye. Clean the main instrument panel using a soft, lint-free cloth dampened with alcohol at maximum 70%. All necessary cleaning should be followed as per manufacturer's guidelines of each machine in order to avoid inadvertent damage by the cleaning solutions. Breath shields should be incorporated between the technician and the patient to prevent direct contact with the aerosols generated. Following parts to be cleaned with alcohol swab after every patient: joystick, locking screw for the instrument base, head rest, chin rest, handlebar which the patient holds, keyboard and touch display.
Additional Work-up: Necessary systemic workup can be requested at operating surgeon's/anaesthetist's discretion. Confirmatory tests for COVID-19 and chest X-ray may be requested at the discretion of the operating surgeon.
Counselling: It is advisable to facilitate the confirmation of surgery date, provide pricing details and also give clear instructions for surgery-day protocols. To minimise contact with papers, it would be appropriate to provide all the necessary details over phone or email or SMS. Special COVID-19 consents can be added to the preoperative protocol.[7]
Preparedness for opening the operating room: Fulfilment of ACAL (Assurance, Clinical, Administrative and Logistic) criteria
Assurance:
The pandemic in a nutshell has caused a significant psychological and economic distress to the humanity
It would take time for the population to revert back to completely normal pre-COVID-19 lifestyle
It is important for the health care facilities to provide adequate awareness to public of the use of infectious control measures and the safety involved in the elective consultation and surgery.
Clinical:
Check for the availability of personal protection equipment (PPE) and also follow the evolving policies for the health care workers and specific procedures
Waiting list- To assess the number of patients who have been examined earlier and are due for cataract surgery. Scheduling can be done based on available resources
Prioritization: Based on quantity of the backlog the surgeon can make a preference to the list of cataract surgeries (Immediate need- patients who need immediate cataract surgery in situations like lens induced glaucoma, one eyed patients with only seeing eye having cataract, bilateral dense cataracts and unilateral high myopes with one eye operated; delayed need- all other patients with cataracts)
Cleaning protocols: Cleaning in all areas should be addressed based on recommended protocols (e.g., preoperative, anaesthesia room, patient waiting room, ORs, changing rooms etc.).
Administrative:
Severity of the pandemic: It is important to assess the status of the pandemic locally, nationally and globally from time to time. The risk profiling zones would keep changing and hence monitoring the same would help in changing the hospital protocols
Capacity assessment: Before scheduling of cases it is important to assess the number of ORs that could be used immediately and also based on backlog plan the number of surgeries to be completed per day or week
Real-time decision making: In view of several new changes to the existing protocols built over the years may lead to development of new issues which could be collated and collectively addressed during the team huddle at the end of the day
Utilization/efficiency monitoring: Apart from ensuring the safety of patients and the health care workers, the utilization of the OR space and the efficiency of the staff should be monitored to maintain economic stability
OR schedules: The schedules could be staggered over a period of time and the team/facility should be ready to accommodate the rapid influx of cases. The scheduling efficiency can be improved by opening up extended hour and weekend working schedules
Logistics:
Accessibility: The risk profiling zones created by the GoI has definitely led to difficulties for patients travelling to seek health care. It is important for health care facility to engage the patient by being accessible through appropriates technologies like teleconsultation, social media, etc.
Availability of staff and training: The entire multidisciplinary cadres (surgery, anaesthesia, nursing, biomedical, housekeeping) of OR staff should be mobilized and trained with the most updated protocols. Mock drills should be done to assess their acquaintance with new protocols before commencing the OR
Inventory: It is important to ensure that all the necessary consumables required for cataract surgery are available and also making sure that a constant supply of these would be happening as the demand surges through different vendors
Medical equipment: Most of the equipment (surgical microscopes, phacoemulsification platforms, Femtosecond lasers, etc.) have not been used for several days and is important to get all these functioning and calibrated as per standards proposed by the manufacturer
Operating room: There has been a lot of discussion on the reversing of negative flow ORs for COVID-19 to positive flow ORs for surgery. The whole thought process behind this is to ensure the virus laden airborne particles do not move out of the room occupied by COVID-19 positive patient and also maintaining the concentration of virus laden particles inside the room at a minimum to protect health care workers. These precautionary measures are made when a patient with active virus is staying in the room or being operated in the OR. Most of the ophthalmic OR complexes would have a positive pressure wherein the air flows from in the room to adjacent areas (i.e away from the patient) whereas in negative pressure system the air flows into the room (i.e. towards the patient). The current HVAC (heating, ventilating air conditioning) system works on the recirculatory mechanism wherein the air in the OR is recirculated from the AHU (air handling unit). The positive pressure system can be converted to the negative pressure system by blocking the return air vents in the OR. The AHU should have access to surplus outdoor air supply. To extract the room air into the atmosphere exhaust blowers should be placed. At all-time points the exhaust air quantity should be greater than the inflow air quantity to maintain preferably >5 Pa in the room.[25,26] All these changes are required in situation of a patient having active COVID-19 disease, but the patients that are operated are not positive and the duration of surgery is also less (15-20 minutes). In the absence of any definite evidence for the need to change the operating environment for cataract surgeries, the current OT facility may be continued till definitive guidelines are issued by the GoI.
Flow of patients in the operating room
One day prior to surgery patient should be contacted to understand if the patient or any family members have symptoms of COVID-19 or any history of recent travel to hotspots/containment zone
Entry through triage area for temperature check
Only one attendant is allowed
Patients should change their cloths before entering OR complex. Disposable clothing is preferred but in case of linen cloth one should plan for proper handling protocols.
Both patient and attendant to wear mask all through and sanitize hands
Ensure safe distancing at each time point
Space out surgery appointments to avoid overcrowding.
On the day of cataract surgery:
Operating Room:
PPE (surgeon/assistant/scrub nurse)
Surgical scrubs, cap, footwear cover
N 95 mask/triple layered mask to be used at all times
Visor/face shield/protective goggles when not operating
Protective goggles and/or prescription glasses during surgery
Gloves (unsterile) to be used when not scrubbed
Gloves (Sterile) to be used while operating
Sterile linen gown/disposable gown may be used during the surgery.
Anesthesia
Topical anesthesia is preferred, wherever appropriate
Local anesthesia (Peribulbar anesthesia/retrobulbar) can be administered with the following safety measures:
Use gloves and other PPE as appropriate
Mark the eye
Instill topical anesthetic drops, 5% povidone iodine eye drops (2 minutes contact time) in the eye to be operated
Povidone iodine paint applied to the operating eye and the adnexa
Care to prevent spillage of body fluid on surgeon/anesthetists/staff or floor
To avoid the use of pinkie rubber ball for pressure or to consider proper cleaning/drying methods before using the same for subsequent patients. Instead using intermittent gentle digital massage may be appropriate
If the number of patients is limited, the Peribulbar anesthesia/retrobulbar anesthesia should be administered directly on the operating table.
During surgery
General Precautions
Maintain safe distance from assisting nurse/trainees/technicians as much as possible
Scrub and put on sterile linen gown and gloves or disposable scrubs may be considered
Brief the patient about the steps involved and approximate duration of surgery as this will help him to remain calm
To instruct patient not to talk during the procedure and avoid exertion specially for heavily built patients
Instill povidone iodine 5% in the operating eye (2 minutes of contact time) before applying sterile drapes
10% povidone iodine skin preparation and wait until the surface is completely dry
Ensure proper draping and no escape of exhaled air happens through the gaps in the drape
To spread viscoelastic over the cornea which will avoid need for frequent instillation of balanced salt solution (BSS) or ringer lactate (RL) over the cornea. The viscoelastic also replaces the tear film of the patient, thus minimizing the contact of instruments with the patient's tears
Handle equipment carefully so as to avoid injury with sharps to self and others
Avoid spillage of body fluid or blood particularly when squirting BSS/RL/viscoelastic from syringes
At the conclusion of the surgery, discard used disposable instruments following biomedical waste policy
Assisting team must handle patient with gloved hands wearing the mask and a linen/disposable gown. Protective goggles or visor/face shield can also be considered
All material proposed to be used for single use by the manufactures should be discarded after the procedure
Preferably a new tip and sleeve or a sterilized one should be used for every case
Avoid having observers sitting at the observer scope.
Specific Precautions:
Cataract surgery including phacoemulsification has not been proven to be an infective aerosol generating procedure till date. In phacoemulsification the aqueous in the anterior chamber is replaced by viscoelastic/BSS/RL at different points of the surgery. During the delivery of ultrasound energy, the BSS/RL may get aerosolized and not patient's aqueous humour. Thus, the risk of aerosolized virus would be very low[27]
Fashion the paracentesis and main wound appropriately to prevent excessive escape of fluid, and also avoid the need for suturing
Minimize the number of attempts of entry into the anterior chamber
Avoid switching on irrigation outside the anterior chamber
Avoid delivering of ultrasound energy when the phacoemulsification probe is not in the anterior chamber
Manual small incision cataract surgery: In general, to avoid blood or excess fluid spilling. Peritomy of the desired size should be made and adequate amount cauterization may be done to work under bloodless field. Blumenthal technique would involves the use of excessive amount of fluid. Hence the surgeon or the assistant should be more vigilant with the amount of fluid drained out so as to prevent spillage
Ensure that all the fluid is collected in the pouch and not spilled on the floor
At the end of the procedure, instillation of 5% povidine iodine solution in the cul-de-sac
All sheets on the operation table should be changed in between patients and the tables should be sanitized using appropriate disinfectants
At the conclusion of the surgery discard used disposable instruments following biomedical waste policy.
Special situations:
A. Femtosecond laser-assisted cataract surgery
Ensure povidone iodine (5%) drops 5 minutes prior to docking
Use new syringe and water for injection in every case to drop saline in suction cup (liquid optic interface-based platforms)
Wash excess drops before docking
Patient wears mask all through
All surfaces patient touches during procedure cleaned with alcohol swabs
Surgeon wears gloves all through along with other PPE
Touch screen covered by clingfilm - dispose after each procedure
Disposable plastic glove placed over patient bed joystick - changed after every case.
B. Toric IOL marking
Non-contact automated toric alignment platforms may be preferred for intraocular lens alignment wherever possible over manual marking
In situations of use of manual marking to consider using sterile toric marker and new marking pen for each patient
Povidone Iodine (5%) eye drops to be instilled prior to the marking
Ensure mask for patient
If the slit lamp is used for making to make sure the breath shields are kept as barrier between patient and surgeon. To make sure the slit lamp is cleaned after every case. Avoid talking while at slit lamp.
Postoperative care and follow-up
In order to avoid for the patient to travel and have multiple visits to the hospital the number of postoperative visits can be reduced for the patients who underwent an uneventful phacoemulsification. A few follow ups can be completed using teleophthalmology or over the phone discussion with the patient. The postoperative prescription and follow-ups can vary from cases to case as per surgeon's discretion. Patients should be advised to avoid travel and minimize contacts with individuals other than family members during the first 2 weeks after cataract surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990-2020: A systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–34. doi: 10.1016/S2214-109X(17)30393-5. [DOI] [PubMed] [Google Scholar]
- 2. [Last accessed on 2020 May 08]. Available from: https://www.iapb.org/knowledge/what-is-avoidable-blindness/cataract/
- 3.Nangia V, Jonas JB, George R, Lingam V, Ellwein L, Cicinelli MV, et al. Prevalence and causes of blindness and vision impairment: magnitude, temporal trends and projections in South and Central Asia. Br J Ophthalmol. 2019;103:871–7. doi: 10.1136/bjophthalmol-2018-312292. [DOI] [PubMed] [Google Scholar]
- 4.Rao GN, Khanna R, Payal A. The global burden of cataract. Curr Opin Ophthalmol. 2011;22:4–9. doi: 10.1097/ICU.0b013e3283414fc8. [DOI] [PubMed] [Google Scholar]
- 5. [Last accessed on 2020 May 08]. Available from: https://static.mygov.in/rest/s3fs-public/mygov_15883406691.pdf .
- 6.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. All India Ophthalmological Society-Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. [Last accessed on 2020 May 08]. Available from: https://aios.org/pdf/OPHTHALMIC-PRACTICEGUIDELINES-IN-THE-CURRENT-CONTEXT-COVID19.pdf .
- 8.Ashour HM, Elkhatib WF, Rahman MM, Elshabrawy HA. Insights into the recent 2019 Novel Coronavirus (SARS-CoV-in light of past human coronavirus outbreaks. Pathogens. 2020;9:1–15. doi: 10.3390/pathogens9030186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith R. Social measures may control pandemic flu better than drugs and vaccines. BMJ. 2007;334:1341. doi: 10.1136/bmj.39255.606713.DB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–9. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Coronavirus disease (COVID-19) advice for the public WHO. 2020. [Last accessed on 2020 Mar 17]. Available from: https://wwwwhoint/emergencies/diseases/novel-coronavirus-2019/advic e-for-public .
- 12.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China] Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145–51. [Google Scholar]
- 13.Lai TH, Tang EW, Chau SK, Fung KS, Li KK. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2020;258:1049–55. doi: 10.1007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai TH, Tang EW, Fung KS, Li KK. Reply to “Does hand hygiene reduce SARS-CoV-2 transmission.”? Graefes Arch Clin Exp Ophthalmol. 2020;258:1135. doi: 10.1007/s00417-020-04653-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tang GC, Steel DH, Li KK. Why ophthalmologists should mask: A perspective from Hong Kong [published online ahead of print, 2020 29] Eye (Lond) 2020:1–2. doi: 10.1038/s41433-020-0916-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wong DH, Mak ST, Yip NK, Li KK. Protective shields for ophthalmic equipment to minimise droplet transmission of COVID-19 [published online ahead of print, 2020 Apr 22] Graefes Arch Clin Exp Ophthalmol. 2020:1–3. doi: 10.1007/s00417-020-04683-y. doi: 101007/s00417-020-04683-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARSCoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou Y, Zeng Y, Tong Y, Chen C. (2020) Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctiva. medRxiv. doi: 10.1101/2020.02.11.20021956. [Google Scholar]
- 19.Parrish RK, 2nd, Stewart MW, Duncan Powers SL. Ophthalmologists are more than eye doctors: In memoriam Li Wenliang. Am J Ophthalmol. 2020;213:PA1–2. [Google Scholar]
- 20.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020 doi: 10.1002/jmv.25725. doi: 10.1002/jmv. 25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seitzman GD, Doan T. No Time for Tears. Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.03.030. S0161-6420; 30314-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ng VWK, Tang GCH, Lai THT, Tang EWH, Li KKW. Intraocular pressure measurement during COVID pandemic. Indian J Ophthalmol. 2020;68:950–1. doi: 10.4103/ijo.IJO_723_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas R, Thomas S, Braganza A. Evaluation of the role of syringing prior to cataract surgery. Indian J Ophthalmol. 1997;45:211–4. [PubMed] [Google Scholar]
- 24.Camara JG, Santiago MD, Rodriguez RE. The micro-reflux test: A new test to evaluate nasolacrimal duct obstruction. Ophthalmology. 1999;106:2319–21. doi: 10.1016/S0161-6420(99)90533-X. [DOI] [PubMed] [Google Scholar]
- 25.Malhotra N, Joshi M, Datta R, Bajwa SJS, Mehdiratta L. Indian Society of Anaesthesiologists (ISA National) Advisory and Position Statement regarding COVID-19. Indian J Anaesth. 2020;64:259–63. doi: 10.4103/ija.IJA_288_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agarwal A, Nagi N, Chatterjee P, Sarkar S, Mourya D, Sahay RR, et al. Guidance for building a dedicated health facility to contain the spread of the 2019 novel coronavirus outbreak. Indian J Med Res. 2020 doi: 10.4103/ijmr.IJMR_518_20. doi: 10.4103/ijmrIJMR_518_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. [Last accessed on 2020 May 15]. Available from: https://www.aao.org/headline/specialconsiderations-ophthalmic-surgery-du ring-c .