Abstract
A 28-year-old female came to us one month after retinal detachment surgery with a sudden painless drop in vision. The condition gradually worsened with ongoing treatment so she was taken up for lensectomy with silicone oil removal and intravitreal antibiotics and steroids. The microbiological analysis of silicone oil revealed Mycobacterium complex and gene sequencing isolated Mycobacterium abscessus, which showed antibiotic sensitivity to only piperacillin-tazobactam. Repeated intravitreal injections of the same led to the resolution of infection. This case report highlights the impact of sparsely used piperacillin-tazobactam in cases of Mycobacterium positive endophthalmitis, and the role of gene sequencing.
Keywords: Endophthalmitis, gene sequencing, mycobacterium, piperacillin-tazobactam, polymerase chain reaction
Mycobacterium abscessus is a rare ubiquitous organism known to cause endophthalmitis and is commonly found in bioaerosols, exogenous materials like intraocular lenses, irrigating solutions, buckles, silicone oil, or perfluorocarbons.[1] Rapidly growing non-tuberculous mycobacterium complex comprises of M. chelonae, M. fortuitum, and M. abscessus.[2] Endophthalmitis caused by the first two is relatively common and well described in literature, but M. abscessus is quite rare and potentially devastating, as it has a slow and delayed course of onset, multiple recurrences, and grave prognosis, which we describe in our case report.[3]
Case Report
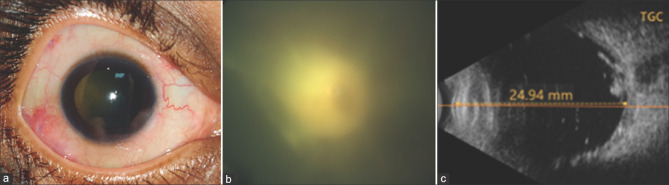
A 28-year-old young healthy female presented with sudden onset decrease in vision in the right eye for the past two days. She underwent retinal detachment surgery elsewhere in the right eye one month (Vitrectomy + Endolaser + Silicone oil injection) and she felt subjective improvement following surgery. Best-corrected visual acuity in right and left eye were hand movement and 20/20 (-6.0 DS) and intraocular pressures were 12 and 14, respectively. The anterior chamber (AC) in the right eye showed a severe reaction, small keratic precipitates inferiorly, and an early posterior subcapsular cataract [Fig. 1a]. Fundus examination of the right eye revealed attached retina, peripheral laser marks, and oil meniscus in situ [Fig. 1b]. Spectral-Domain Optical Coherence Tomography [Fig. 1c] (SD OCT, Spectralis, Heidelberg Engineering, Germany) raster scan passing from fovea showed multiple stalagmite-like pre-retinal deposits, silicone oil reflex, maintained fovea contour, and loss of outer retinal integrity at fovea. The patient was started on topical medications (moxifloxacin, tobramycin, prednisolone, and homatropine eye drops) and an AC tap was simultaneously performed, which revealed no growth. Thus, topical treatment was continued.
Figure 1.

Imaging at presentation. (a) is slit lamp photograph showing AC reaction, small keratic precipitates inferiorly and an early posterior subcapsular cataract. (b) is an Optos image showing mild vitreous haze, attached retina, peripheral laser marks and oil meniscus inferiorly (white arrow). (c) is SD OCT image showing multiple stalagmites like pre-retinal deposits (white arrow), silicone oil reflex, maintained fovea contour and loss of outer retinal integrity at fovea (white circle)
Two days later, the vision dropped to perception of light with the development of streak hypopyon and severe vitreous haze leading to a significantly decreased fundus view. Lensectomy and silicone oil removal (sent for microbiological examination) with intravitreal injection (vancomycin 1 mg/0.1 ml, ceftazidime 2.25 mg/0.1 ml, and dexamethasone) were performed. Intraoperatively post surgery, the retina was found to be attached with multiple superficial hemorrhages along the vascular arcades and perivascular sheathing. There was typically a sheath-like membrane over the posterior pole, and the disc was barely visible. This membrane was so strongly adherent to the underlying retinal surface that a plane for dissection could not be obtained, hence it was left untouched.
The antibiogram of aspirated oil showed sensitivity to piperacillin-tazobactam antibiotics, and hence intravitreal injection of the same (225 μgm/0.1 ml) with dexamethasone was repeated every 48 hours for the next eight days. On postoperative day nine, the vision improved to counting finger 2 meters, and there was resolving fibrin in the AC with a clear cornea [Fig. 2a]. Fundus [Fig. 2b] showed a contracting membrane, typically showing a centripetal crumpling pattern, and the second-order blood vessels were visible.
Figure 2.
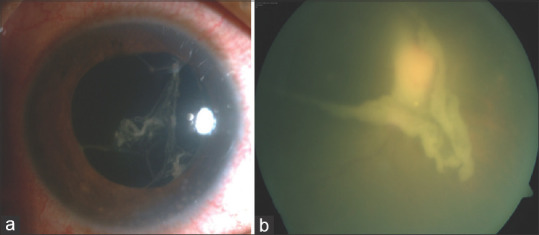
Post op day-9. (a) showing resolving fibrin in AC with a clear cornea. (b) showing a contracting membrane, typically showing a centripetal crumpling pattern, and visible second order blood vessels
Three days later, the patient presented back with a drop in vision to counting finger 1 meter. The anterior chamber was quiet, but the fundus showed a dull red glow with severe haze [Fig. 3a and b]. Ultrasound [Fig. 3c] revealed minimal low reflective dot echoes, attached retina, and a hyperreflective non-mobile membranous echo over the optic nerve head with small extensions in all quadrants, which corresponded with the contracting membrane visualized earlier. The patient was continued on a repeated dose of intravitreal injection. At one month post-op, the patient's vision improved to 20/200, and the anterior and posterior chamber was quiet. The membrane had significantly contracted and was visible over the disc [Fig. 4a]. The PCR report showed acid-fast bacilli, culturally and morphologically resembling rapid growers of Mycobacterium complex isolated in culture [Fig. 4b and c]. Gene sequencing was performed and Mycobacterium abscessus was isolated. Eventually, the patient was tapered off all topical medications over the next two weeks, and the patient's vision was maintained at three months post-op.
Figure 3.
Post op day-12. (a) showing quite anterior chamber. (b) showing dull red glow with minimal view of fundus details. (c) is ultrasound B scan image showing minimal low reflective dot echoes, attached retina and a hyperreflective non mobile membranous echo over the optic nerve head with small extensions in all quadrants; correspondingly well with the contracting membrane visualized earlier
Figure 4.

Post op-1 month. (a) is Optos image showing significantly contracted membrane visible just over the disc area with well attached retina and visibility of peripheral laser marks. (b) showing Acid Fast bacilli in direct smear Acid fast staining on 100X. (c) showing growth of Mycobacterium colonies from the specimen on Chocolate Agar after 3 days of incubation
Discussion
M. abscessus, a notorious organism, tends to form a biofilm, hence becomes highly resistant to antibiotics.[1] The chief complaint of the patient in most cases is the loss of vision, owing to severe anterior and posterior segment reaction. Redness, hypopyon, and pain are relatively uncommon, and the onset of the symptoms in typically after 2-6 weeks post intraocular procedure.[4]
Diagnosis of mycobacterium can be achieved with reverse transcription-polymerase chain reaction (RT-PCR) analysis, which specifically targets the m-RNA, and can detect the load of live organisms.[3] Gene sequencing methods help to distinguish between the subspecies of mycobacterium, as they tend to find out the order of DNA nucleotides or bases, which makes up the organism's DNA.[5,6] In our case too, with gene sequencing methods, M. abscessus was isolated.
The antibiogram sensitivity chart targeted towards M. abscessus showed sensitivity to piperacillin-tazobactam, rest all antibiotics were found to be resistant. Piperacillin is a semi-synthetic ureidopenicillin antibiotic, which has a broad-spectrum antibiotic coverage against gram-positive, negative, and anaerobes. Tazobactam is a beta-lactamase inhibitor antibiotic, which helps in preventing the hydrolysis of piperacillin, if used in combination.[7] We used a dose of 250 μg/0.01 ml, which was repeated every 48 hours, and a total of five doses were given. The non-improvement of vision more than 20/200 could also be attributed to the loss of outer retinal architecture at the fovea, which was distinctively evident in the OCT scan.
Conclusion
This case gives us clues in diagnosing mycobacterium endophthalmitis, highlights the importance of gene sequencing, and thus aids in providing targeted chemotherapy. Also, it illustrates the importance of piperacillin-tazobactam, which may be a new, potentially vital drug in the treatment of endophthalmitis resistance to multiple drugs, as it has an extensively broad antimicrobial spectrum.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank Dr. Parthopratim Majumdar for helping us in editing this manuscript.
References
- 1.Hung JH, Huang YH, Chang TC, Tseng SH, Shih MH, Wu JJ, et al. A cluster of endophthalmitis caused by Mycobacterium abscessus after cataract surgery. J Microbiol Immunol Infect. 2016;49:799–803. doi: 10.1016/j.jmii.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Shah M, Relhan N, Kuriyan AE, Davis JL, Albini TA, Pathengay A, et al. Endophthalmitis caused by non-tuberculous mycobacterium: Clinical features, antimicrobial susceptibilities and treatment outcomes. Am J Ophthalmol. 2016;168:150–6. doi: 10.1016/j.ajo.2016.03.035. [DOI] [PubMed] [Google Scholar]
- 3.Rolfe NE, Garcia C, Widen RH, Taylor SP. Rapid diagnosis of Mycobacterium abscessus endophthalmitis. J Med Microbiol. 2013;62:1089–91. doi: 10.1099/jmm.0.051771-0. [DOI] [PubMed] [Google Scholar]
- 4.Paulose RM, Joseph J, Narayanan R, Sharma S. Clinical and microbiological profile of non-tuberculous mycobacterial endophthalmitis- experience in a tertiary eye care centre in Southern India. J Ophthalmic Inflamm Infect. 2016;6:27. doi: 10.1186/s12348-016-0096-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipworth S, Hough N, Leach L, Morgan M, Jeffery K, Andersson M, et al. Whole-Genome Sequencing for Predicting Clarithromycin Resistance in Mycobacterium abscessus. Antimicrob Agents Chemother. 2018;63:e01204–18. doi: 10.1128/AAC.01204-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hung JH, Ko WC, Chen CY, Lin SH, Wu CL, Hsu SM, et al. Postoperative Mycobacteroides abscessus subsp abscessus endophthalmitis: Clinical analysis of 12 clustered adults and a proposed therapeutic algorithm. J Microbiol Immunol Infect. 2019 doi: 10.1016/j.jmii.2018.12.011. pii: S1684-1182(18)30349-9. [DOI] [PubMed] [Google Scholar]
- 7.Ozkiriş A, Evereklioglu C, Kontaş O, Oner AO, Erkiliç K. Determination of nontoxic concentrations of piperacillin/tazobactam for intravitreal application. Ophthalmic Res. 2004;36:139–44. doi: 10.1159/000077326. [DOI] [PubMed] [Google Scholar]