Abstract
Coronavirus pandemic has strained the healthcare system with mortality and morbidity. A number of elective surgeries have come to standstill due to lockdown and movement restrictions. Refractive surgery being a purely elective procedure and quite a fresh subset of ophthalmology, there is a lack of unanimity as to what precautions should be followed to resume the practice of same. This article attempts to highlight simple guidelines in accordance with an expert panel, which can be followed by all those involved directly or indirectly in refractive surgery services while addressing safety of doctors, supporting staff as well as patients as a primary concern.
Keywords: COVID-19, preferred practice patterns, refractive surgery
We are in the midst of worldwide pandemic, with cities and even whole countries shutting down. In this crisis, the government, healthcare professionals, and researchers are doing their best to deliver the healthcare services. However, the uncertainty on delivering our services without getting impacted is the hardest thing to decipher. Change in our ways of functioning in inevitable and we will require practical guidelines as to how to we restart our practice of refractive surgery based on national advisories.
Refractive surgery being a relatively upcoming branch with rapid advancements, there is a lack of common consensus or direction on how do we resume our practices in this aftermath. To our knowledge, there is yet no set of guidelines for safe surgery practice in this domain. Refractive surgeries are elective procedures and are included in the non-urgent category of the recent COVID-19 related ophthalmic guidelines published by the Indian journal of Ophthalmology.[1] As per the Ministry of Health and Family Welfare (MoHFW)—all medical activities as deemed required by the hospital can be carried out by all hospitals except in containment zones with the necessary precautions.[2] COVID-19 testing for pre-operative patients is not mandatory[1] but may be done as per the hospital policy and anesthetist/doctor discretion even if the patient is asymptomatic. Few studies have reported low prevalence of SARS-CoV-2 Virus in tears.[3] Excimer laser ablation comprises a major part of refractive surgeries and excimer laser ablation of the cornea, in a human immunodeficiency virus (HlV)-infected or herpesvirus-infected patient, posing a health hazard to the operating surgeon has been shown to be highly unlikely.[4] This article highlights the consensus based guidelines by an expert panel comprising of leading ophthalmologists of India including representatives from major governmental and private institutions as well as the All India Ophthalmological Society leadership. These guidelines are comprehensive, simple to follow and can be easily reproduced in all centers across the country and should help ophthalmologists to restart refractive surgery practice while trying to ensure the safety of their patients and themselves.
Methods
These guidelines demarcate the infection control and prevention advice for ophthalmologists involved in Refractive surgery practice inclusive of LASIK (Microkeratome or Femtosecond assisted Laser in situ keraomileusis), Transepithelial PRK (Photorefractive keratectomy), SMILE (Small incision lenticule extraction), ICL (Implantable collamer lenses), laser treatments in Keratoconus, and crosslinking. These guidelines are based on the available literature and guidelines issued from the MoHFW, Government of India, and Indian Council of Medical Research (ICMR). These guidelines are dynamic and with the evolving situation on COVID-19, further refining may be done, as and when required. An invitation to review these guidelines was sent out by email to eminent ophthalmologists across India, including heads of the major teaching institutions, both in the government and private sectors. Disagreements on guidelines were resolved by discussion between members and a final set based on common consensus was made.
Practice Guidelines for Refractive Surgery Services
General measures to be taken in hospital
For patients[1]
All patients and attendants must wear a mask and use sanitizer at entry point.
Schedule appointments prior so as to avoid overcrowding.
To take history of any symptoms of COVID-19—this includes questions on travel, fever, cough, or recent onset difficulty in breathing, loss of smell or taste. It is relevant here to ask the same history for the attendant as well.
Temperature by non-contact method to be documented of both the patient and the attendant.
The patient and the attendant to be explained and mandated to download the Arogya Setu COVID-19 tracking App with their mobile number (location enabled) for future digital tracking.
Social distancing norms to be strictly followed in areas of movement like reception, pharmacy, waiting area.
All patients and attendees to fill the COVID-19 declaration form. [Supplementary Table 1 (837.4KB, pdf) ]
Online payment methods to be encouraged to minimize the contact with currency.
For employees
All staff involved to have mask, Protective eyewear, head cap, and gloves on at all times.
Hand sanitizing protocol to be followed during the examination and also in between patient examinations.
Greet patients with a Namaste instead of shaking hands.
Keep doors/windows open to allow free flow of air.
Clean all surfaces (chair units, tables, slit-lamp units, keyboard, computer monitor, trial frame, etc.) with appropriate cleaning solution before starting clinics and at periodic intervals.
Preoperative guidelines
Wearing of appropriate mask for the patient as well for the examiner throughout all the tests is mandatory. In addition, it is recommended that the examiner wear gloves, protective glasses, and a protection gown.
Change of gloves between each patient is recommended.
While performing refraction, avoid touching the forehead of the patient to measure working distance. The Trial frame, pinhole occluder, and all lenses used should be wiped with alcohol swab appropriately and sanitized between patients with sufficient time provided for surface drying of the instruments.
Measurement of IOP using Goldmann applanation tonometry (GAT) may be done. The GAT prism to be wiped with alcohol between every case and with 1:10 sodium hypochlorite at the beginning and end of the day.
Use of commercially available breath shields for slit lamp is encouraged as it acts as barrier between the patient and examiner. Surface cleaning of the slit lamp chin rest, forehead resting bar should be done with alcohol-containing disinfectants between patients.
To decrease the risk of spread via aerosols, examiner should inform the patient that they will speak as little as possible during the slit-lamp examination and request that the patient also refrain from talking.
Corneal topography is an indispensable part of the pre-operative work-up. It is a quick, non-aerosol generating and non-contact procedure entailing a negligible risk of transmitting the virus to the patient. Additionally, applications of breath shields and cleaning of the device by alcohol in-between two patients should be followed to be extra-precautious. The examiner must give clear, concise instructions to minimize touching the patient for positioning.
Intraoperative precautionary measures
General etiquettes to be followed
Use of personal protection equipment according to general OT guidelines. N 95 mask/triple layered mask, surgical scrubs, cap, sterile gloves, protective goggles and/or glasses and sterile linen gown/disposable gown to be used while operating. This should be an accepted norm not only for the surgeon but also the assistant.
It is recommended that the patient changes into a disposable gown to avoid spread via fomites. Because of prolonged proximity of the eye surgeon to the patient, the patient should also wear a surgical mask.
Regardless of the prevalence of COVID-19 in your area, the waiting room should be kept as empty as possible, advice seated patients to maintain social distance. As much as possible, one patient (wearing appropriate protective gear) at a time in the waiting area.
Assisting team handling the patient must wear gloves, a gown, and a mask.
COVID-19 consent form for surgery to be duly signed.
Following are the recommended guidelines for selective procedures. The description is in reference to LASIK surgery. Besides the common steps to be followed, we have outlined additional precautions for specific surgeries as well.
Intraoperative guidelines
Ocular surface wash with 0.25% Povidone-Iodine 10 min prior to surgery ensures adequate holding time. This is virucidal with no untoward effect to the corneal surface.[5]
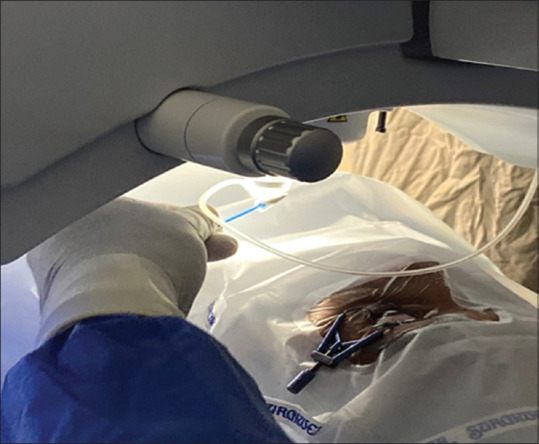
Patient should be well-draped under aseptic precaution with adequate exposure of the surgical area. [Fig. 1]
One of the crucial points is filling the eye drape pouch with 10 ml of 5% Povidone-Iodine solution [Fig. 2]. This ensures sterilization of saline solution used to wash the stromal bed post excimer laser ablation and any secretions from ocular surface, which may get washed into the pouch. This will also help protect the healthcare workers involved in disposal of drapes.
Minimal instruments as per the requirement to be kept on the surgical trolley. [Fig. 3]
The refractive suite may be covered with screens that can be easily sterilized without damaging the surface of the machine. Sterile plastic cover/shield may be placed between the surgeon and the patient while maneuvering the microscope.
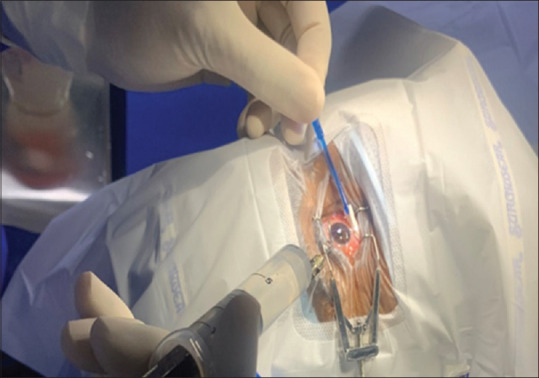
Drying ocular surface thoroughly using sterile dry swab before starting the surgical procedure to avoid pooling of secretions and tears [Fig. 4]. Pooled secretions could be a potential source of aerosols and should be avoided at any instance.
Practice social distancing from the machine, the patient, amongst assistants; and keep a one hand distance from the platform even while operating.
It is preferable to use the monitor for visualization of flap creation instead of looking through the microscope. Use the monitor also while excimer laser firing to avoid exposure to aerosols generated by plumes of laser.[6]
While washing the bed, practice simultaneous drying of the ocular surface with other hand using a sterile merocel swab to avoid pooling of solution. [Fig. 5]
Immediately post usage, immerse the instruments and used swabs in disinfectant solution like lysoformin (7.5 g glyoxal, 9,5 g glutaral, 9.6 g didecyl dimethyl ammonium chloride) for 15 minutes [Fig. 6]. Note that this is an additional procedure and not a substitute for the sterilization of instruments as per general guidelines. The swabs can be discarded after this as per the biomedical waste policy. At the conclusion of the surgery, use sanitizer to disinfect the gloves and practice.
Inward out removal of gloves so that the used surface of the gloves is unexposed and discarded, for the safety of the staff handling the waste.
Descrub after every case. If a disposable gown is being used, it should be discarded after every case.
Ensure change of sheets and through cleaning of patient bed with disinfectant with a holding time of 15 minutes. The surrounding floor should be wiped and allowed to dry after surgery.
Wait for 20 minutes between surgeries and rescrub thus allowing adequate time for the disinfectant to act and surfaces to dry.
Removal of the patient gown after surgery before the patient leaves the OT premises to prevent cross-contamination.
Preferable for the surgeon to take a shower post OT schedule to avoid carrying aerosols, if any, to OPD or other sections of the hospital.
Figure 1.
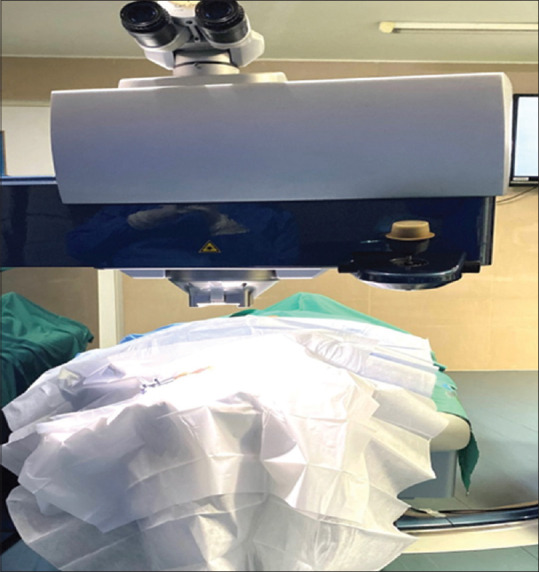
A Well Draped Patient
Figure 2.
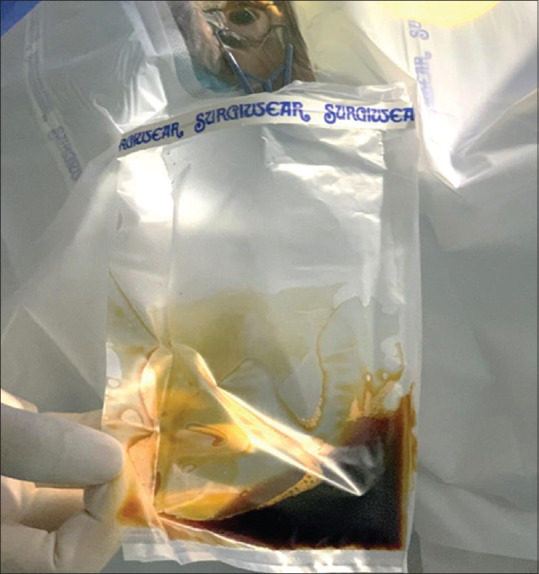
Povidone-Iodine filled draining pouch
Figure 3.
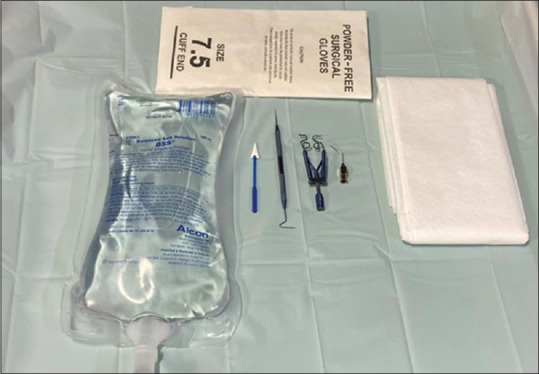
Minimal instruments on surgical trolley
Figure 4.

Drying the cul-de-sac with dry sponge
Figure 5.
Simultaneous drying of ocular surface during bed wash
Figure 6.

Immersing instruments in disinfectant solution
Additional precautions: Femtosecond-assisted LASIK
Once flap creation is completed, remove the suction cup gently and discard the used tubings and suction cup after disinfecting them with lysoformin [Fig. 7] or an appropriate OT disinfectant solution. Avoid keeping them on the platform only to be discarded later.
Figure 7.

Discarding the tubes after Surgery
Additional precautions: Microkeratome
Microkeratome assisted flap creation has more aerosol dispersion as compared to Femtosecond laser assisted Flap creation, which has negligible aerosols. Hence, one may use a larger protective shield (approximately A1 size) between the patient and the surgeon while operating.
Ensure adequate drying of the ocular surface to avoid splashing of saline while flap creation.
Change gloves after operating each eye.
Use a new blade and new set of tubings for each case.
Dry the ocular surface thoroughly before excimer laser ablation. Use the monitor for viewing ablation progression instead of using the microscope.
Additional precautions: SMILE
Use swab soaked in betadine to clean the suction cone before discarding at the end of the surgery [Fig. 8].
Figure 8.
Use of Povidone-Iodine soaked sponge on SMILE Suction cone after surgery
Additional precautions: Photorefractive keratectomy (PRK)
Transepithelial PRK/Phototherapeutic Keratectomy (PTK) + PRK recommended over the conventional methods of manual removal or using 20% alcohol for epithelial debridement. It has been shown that excimer laser ablation generates plumes which may have aerosols.[7] However, the spread of these aerosols thus generated is limited to short distances which might be shorter as compared to the dispersion of aerosol generation during wash. Thus, using transepithelial laser/PTK + PRK may be considered over manual removal of epithelium for PRK.
Use monitor to visualize the treatment progression while maintaining one arm distance from the platform.
Observe caution and gently remove the bandage contact lens after epithelial healing. The examiner should wear N95 mask, protective eye gear, and sterile gloves while doing so. Proper disposal of BCL as per biomedical waste policy to be followed.
Additional precautions: Corneal collagen crosslinking
While doing the collagen cross linking (KXL) the UV-A light head should be covered with a sterile transparent drape/plastic cover [Fig. 9]. The plastic cover to be sterilized using sodium hypochlorite or ETO.
One patient per OT rule to be followed.
Post-operatively, avoid using a bandage to patch the eye while the healing of epithelium is awaited. Prefer a bandage contact lens over the use of pad and bandage.
The KXL equipment for administering the UVA light should be cleaned with solution as per the manufacturer's recommendation.
Figure 9.

Covering the UV-A light head during Crosslinking
Post-operative care
Routine post-operative instructions and medications to be followed.
Can consider early tapering of steroids.
If IOP measurement is needed, consider using GAT and avoid Non-contact tonometry.
Consider keeping post-operative follow-up visits to minimal. Patients can be encouraged for scheduling video-consultation for any post-surgical problems.
Additional precautions: Phakic intraocular lens
Pre-operative Precautions
To be followed as in refractive surgery section mentioned above.
Operating room etiquettes to be followed (Refer to guidelines by Cataract Society of India)
PPE to be worn by both the surgeon and assistant.
N 95 mask/triple layered mask to be used at all times.
Sterile gloves and sterile gown/disposable gown to be used while operating.
Protective head gear/glasses with a side protective patch to be used throughout the surgery.
Anesthesia
Use topical anesthesia or block anesthesia, as per the surgeon preference.
Other guidelines for using anesthesia should be the same as other ocular procedures.
Intra-operative precautions
Use gloves and PPE as recommended in the operation theater.
Mark the eye.
Instill topical anesthetic eye drops, 5% povidone iodine eye drops (2 minutes contact time) in the eye to be operated.
Povidone iodine paint applied to the operating eye and the adnexa.
Care to prevent spillage of body fluid on surgeon/anesthetists/staff or floor.
Sub tenon or intracameral anesthesia can be given during the procedure, if required.
During surgery
Scrub and put on sterile linen gown/disposable gowns and gloves.
Assisting team handling the patient must wear gloves, mask and a linen/disposable gown.
Maintain safe distance from assisting nurse/trainees/technicians as much as possible.
Instill povidone iodine 5% in the operating eye (2 minutes of contact time) before draping as it inactivates any virus in tear film.
Fill the draining pouch with 10 ml of 5% Povidone-Iodine solution prior to procedure to ensure disinfection of the draining fluid.
Drape the eye taking care that the draining pouch is open and not leaking.
It is preferable to use viscoelastic over cornea instead of using Balanced salt solution or Normal saline.
Minimum handing of instruments by assistant to avoid any injury by sharps.
Avoid spillage of body fluid or blood particularly when squirting ringer/viscoelastic from syringes.
Assisting team must handle patient with gloved hands wearing the mask and a linen gown.
Ensure that all the fluid is collected in the pouch and not spilled on the floor.
All sheets on the operating table to be changed in between patients and the tables should be sanitized using appropriate disinfectants. Drying of the floor with a mop for any fluid spilled accidently during surgery before next surgery.
Post-operative care
Routine care and medications to be advised.
Use GAT for IOP measurement. Avoid the use of non-contact tonometry.
Non-contact procedure for vault measurement to be preferred over contact procedures like ultrabiomicroscopy (UBM) for ICL.
Conclusion
COVID-19 pandemic is straining the healthcare systems worldwide and in these scenario healthcare workers are an indispensable resource of every country. Because of the close contact with patients, procedures which generate aerosols and potential risk of presence of virus in tears there was a fear that ophthalmologists and eye related healthcare workers are at a slightly higher risk of developing the infection.[8,9] While we have attempted to make this an all-inclusive document, these guidelines are subject to change as per the rules and regulations laid down by local government authorities. Refractive surgery is an elective procedure and it is indisputable that resumption of our services may not be effective immediately in certain areas. Though eventually we will come out of this crisis, but with fundamental changes in our way of practice and following these simple guidelines will ensure a defence against the spread of transmission and help in protecting ourselves, our staff, our families and our patients. Practising discipline and mindfulness can be our armor against this chaos.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration Form for COVID-19 Infection
References
- 1.Sengupta S, Honavar SG, Sachdev MS, Sharma N, Kumar A, Ram J, et al. Writing Committee on behalf of the All India Ophthalmological Society-Indian Journal of Ophthalmology Expert Group for COVID-19 Practice Guidelines; Composition of the All India Ophthalmological Society-Indian Journal of Ophthalmology Expert Group for COVID-19 Practice Guidelines includes the Writing Committee (as listed) and the following members (in alphabetical order by the first name).All India Ophthalmological Society-Indian Journal of Ophthalmology consensus statement on preferred practices during the COVID-19 pandemic. Indian J Ophthalmol. 2020;68:711–24. doi: 10.4103/ijo.IJO_871_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sachdev M, Sharma N, Sinha R. Ophthalmic Practice Guidelines In The Current Context of COVID-19 Aiosorg. 2020. [Last accessed on 2020 May 31]. Available from: https://aiosorg/pdf/OPHTHALMIC-PRACTICE-GUIDELINES-IN-THE-CURRENT-CONTEXT-COVID19pdf .
- 3.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–8. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hagen KB, Kettering JD, Aprecio RM, Beltran F, Maloney RK. Lack of virus transmission by the excimer laser plume. Am J Ophthalmol. 1997;124:206–11. doi: 10.1016/s0002-9394(14)70785-8. [DOI] [PubMed] [Google Scholar]
- 5.Kariwa H, Fujii N, Takashima I. Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents. Dermatology. 2006;212(Suppl 1):119–23. doi: 10.1159/000089211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glickman RD, Liu Y, Mayo GL, Baribeau AD, Starck T, Bankhead T. Composition of the excimer laser-induced plume produced during LASIK refractive surgery. Proc SPIE Int Soc Opt Eng. 2003;4951:124–32. [Google Scholar]
- 7.Krueger RR, Krasinski JS, Radzewicz C, Stonecipher KG, Rowsey JJ. Photography of shock waves during excimer laser ablation of the cornea. Effect of helium gas on propagation velocity. Cornea. 1993;12:330–4. doi: 10.1097/00003226-199307000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28:391–5. doi: 10.1080/09273948.2020.1738501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang L, Wu P. There may be virus in conjunctival secretion of patients with COVID-19. Acta Ophthalmol. 2020;98:223. doi: 10.1111/aos.14413. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Declaration Form for COVID-19 Infection


