Abstract
Eosinophilic cystitis is a rare form of interstitial cystitis. It can be chronic and debilitating due to urinary frequency, dysuria, incontinence, and frequent urinary tract infections. Prior attempts at treatment have included oral and intravesical steroids, antispasmodics, and antibiotics when indicated. Treatment of eosinophilic disorders has recently been improved with the use of monoclonal antibodies directed at interleukin 5. We report here a case of eosinophilic cystitis treated with the interleukin 5 antagonist, benralizumab. The patient had significant improvement in both quality of life measures and biopsy findings.
Keywords: Eosinophilic cystitis, Benralizumab, Interstitial cystitis, Monoclonal antibodies
Introduction
Eosinophilic cystitis (EoC) is a rare form of interstitial cystitis characterized by eosinophilic infiltration of the bladder wall. As with other forms of interstitial cystitis, it can lead to significant morbidity and quality of life (QoL) impairment. Urinary frequency and urgency can be debilitating in some cases, with dysuria, incontinence, hematuria, and pelvic pain as common presenting symptoms.1 The etiology of EoC is for the most part unknown, although some reports have been ascribed to medications, infection, bladder trauma, or hypereosinophilic syndrome. Due to the rarity of this condition, most of the literature is restricted to small case studies or single case reports. A larger pooled analysis of 135 cases published in 2000 found peripheral eosinophilia in 43% of cases and positive urine cultures in 26% of patients.2 Currently, there is no consensus about EoC treatment. Symptomatic management has consisted of oral and intravesical corticosteroids, antihistamines, antispasmodics, antibiotics, leukotriene antagonists, immunosuppressives, and in severe cases, surgical intervention.1, 2, 3
The treatment of eosinophilic disorders has recently been revolutionized by the arrival of monoclonal antibodies (mAbs) directed at interleukin-5 (Il-5), a chemotactic cytokine for eosinophils. Busse et al. mentioned EoC as a possible candidate for anti-Il-5 mAbs in 2010, but to our knowledge, no studies have been reported for this condition.4 We hypothesize that the Il-5 receptor blocker, benralizumab, may be an effective treatment for EoC by reducing eosinophilic infiltration of the bladder and improving QoL.
Case presentation
We report here the case of a 78-year-old woman referred to the allergy/immunology practice by her urologist. She had a two-year history of extreme dysuria, urgency, frequency, incontinence, pelvic pain, and hematuria. Notably, her symptoms included painful voiding every 20 minutes during the day and up to 20 times at night. This resulted in severe sleep disruption, subsequent depression, and social disturbance. She was essentially homebound. The patient had a long urologic history. A right nephrectomy was performed in 1997 for renal cell carcinoma. Subsequently, she was treated for recurrent urinary tract infections and interstitial cystitis. CT imaging demonstrated bladder wall thickening of 8mm at the fundus. A bladder biopsy was performed, and the bladder wall was found to have eosinophilic infiltrates at up to 100 eosinophils/high power field (Fig. 1). She had no peripheral eosinophilia. When seen initially in the allergy clinic, her skin prick tests were negative for inhalants and common allergenic foods. Previous pharmacologic treatments included oral corticosteroids, antihistamines, monteleukast, antispasmodics, antibiotic suppressive therapy and antibiotic treatment when indicated by dipstick and culture results. Despite these interventions, her symptoms were unrelieved and her self-reported QoL continued to diminish. We administered a validated questionnaire instrument, the Urogenital Distress Inventory (UDI-6) short form5 and found her pretreatment scores to be markedly elevated at 58. Following informed consent for off-label use of a biologic intervention benralizumab, the patient was started at 30mg subcutaneously every four weeks. The patient has been followed monthly to assess clinical response.
Fig. 1.
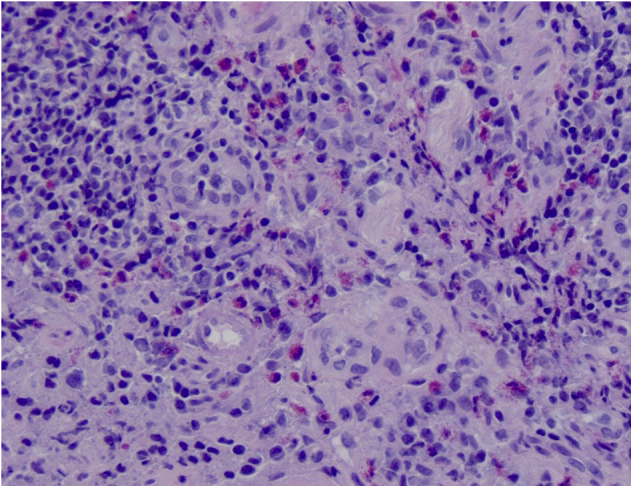
Bladder biopsy at presentation showing numerous eosinophils and eosinophilic microabscess.
Discussion
Following the third dose, the patient's UDI-6 score was reduced to 20, demonstrating a 64% improvement in her subjective symptoms and QoL. The daytime voiding interval increased to 3 h and her sleep disruption was significantly improved to 4 to 8 nocturia events per night. She reported no longer feeling “hopeless and housebound.” No adverse effects from the benralizumab were noted. Three separate urine cultures obtained over the next 6 months were positive for group B strep and Klebsiella species. These were treated with appropriate antibiotics. Her urinary frequency increased during these infections, but subsequently decreased again with antibiotic therapy. Antispasmodics have been continued. Voiding diaries and patient reports demonstrate that urinary frequency and incontinence events begin to increase about three weeks after each benralizumab injection. At 9 months the urine has remained sterile, and she continues to void between 4 and 8 times at night. A repeat biopsy was obtained 9 months after initiating treatment. The biopsy showed continued cystitis, but only rare eosinophils were seen (Fig. 2). After the eleventh dose, the UDI-6 total score was 38, which demonstrates a 34% improvement in the patient's QoL, when compared to the pretreatment score.
Fig. 2.
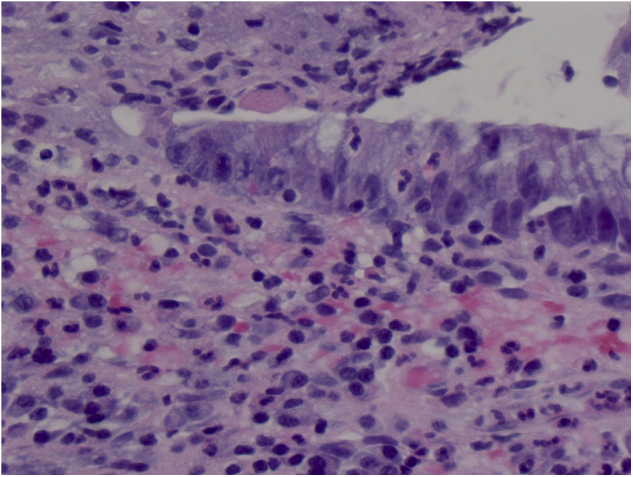
Bladder biopsy after 9 months of treatment showing urothelium and cystitis but no eosinophils.
Conclusion
We describe the successful use of the Il-5 receptor antagonist, benralizumab, in our patient with EoC. She had both improved QoL as measured by the UDI-6, symptomatic relief, and histologic resolution of her eosinophilic infiltration. We believe this is the first report of the use of the biologic benralizumab in this condition. Our patient demonstrates the possibility that biologic intervention with Il-5 antagonists may be a new paradigm in the treatment of EoC, and one that ideally should be further addressed in formal clinical trials.
Acknowledgements
The authors wish to thank Drs. Francisco Carpio and James Brennan for urologic care and Dr Trent Pansze for pathology.
References
- 1.Marcu I., Campian E., Tu F. Interstitial cystitis/bladder pain syndrome. Semin Reprod Med. 2018;36:123–135. doi: 10.1055/s-0038-1676089. [DOI] [PubMed] [Google Scholar]
- 2.Van den Ouden D. Diagnosis and management of eosinophilic cystitis: a pooled analysis of 135 cases. Eur Urol. 2000;37(4):386–394. doi: 10.1159/000020183. Apr. [DOI] [PubMed] [Google Scholar]
- 3.Mosholt K.S., Dahl C., Azawi N.H. Eosinophilic cystitis: three cases, and a review over 10 years. BMJ Case Rep. 2014 doi: 10.1136/bcr-2014-205708. Oct 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Busse W.W., Ring J., Huss-Marp J., Kahn J.E. A review of treatment with mepolizumab, an anti-Il-5 mAb, in hypereosinophilic syndromes and asthma. J Allergy Clin Immunol. 2010;125(4):803–813. doi: 10.1016/j.jaci.2009.11.048. Apr. [DOI] [PubMed] [Google Scholar]
- 5.Naughton M.J., Donovan J., Badia X. Symptom severity and qol scales for urinary incontinence. Gastroenterology. 2004;126(1 Suppl 1):S114–S123. doi: 10.1053/j.gastro.2003.10.059. Jan. [DOI] [PubMed] [Google Scholar]


