Abstract
Nephrogenic adenoma (nephrogenic metaplasia) is a rare benign urological condition, which may present with hematuria, dysuria, and urinary frequency. In the prostatic urethra, it can be misdiagnosed as adenocarcinoma of the prostate. Risk factors for prostatic NA include trauma, infection and prior endourological procedures. We report a case of prostatic NA, presenting with isolated macroscopic hematuria in a man with a history of laser therapy of the prostate for benign prostate hyperplasia, and review the recent literature on the subject.
Keywords: Nephrogenic adenoma, Laser therapy, Benign prostatic hyperplasia, Hematuria, Transurethral resection
Introduction
Nephrogenic adenoma of the prostate is a rare benign condition of the prostate that may mimic adenocarcinoma. It is usually found in pathologic reports following transurethral resection (TUR) of the prostate or prostatic adenomectomy for benign prostatic hyperplasia (BPH). As risk factors, inflammation and previous endourological procedures are listed in the very few cases described in the urological literature.1,2 We present a case report of a nephrogenic adenoma of the prostate in a patient presenting with macroscopic hematuria and with a history of laser evaporation of the prostate, discussing the clinical and pathological aspects involved.
Case presentation
A 67 years-old male presents with an episode of isolated asymptomatic macroscopic hematuria which resolved spontaneously a few days ago. The patient had not experienced hematuria before, had never smoked, and did not have a personal or family history of urolithiasis. Urinalysis was normal, and urine culture was negative. The patient had undergone a transurethral laser photovaporization of the prostate four years earlier, for obstructive symptoms of the lower urinary tract. An abdominal computerized tomography (CT) revealed a 2.5 cm solid renal lesion in the lower pole of the left kidney. A cystoscopy was scheduled under anesthesia to complete the evaluation of the hematuria: anterior urethra was normal, but there were small papillary lesions in the prostatic urethra, and obstructive lateral lobes (Fig. 1). The bladder was normal. A transurethral resection of the prostate was performed, and pathology revealed the presence of cystic urethritis and mesonephric rests (nephrogenic adenoma) in the prostatic urethra (Fig. 2), along with BPH. The patient recovered uneventfully. A month later, a laparoscopic left partial nephrectomy was performed, revealing a 2.3 cm clear cell carcinoma of the kidney Fuhrman I, with negative surgical margins. The patient had a full, uneventful recovery.
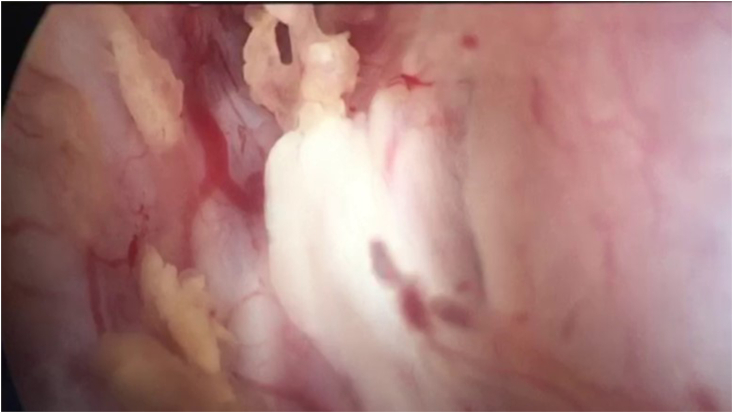
Fig. 1.
Endoscopic view of the prostatic urethra, with multiple papillary lesions.
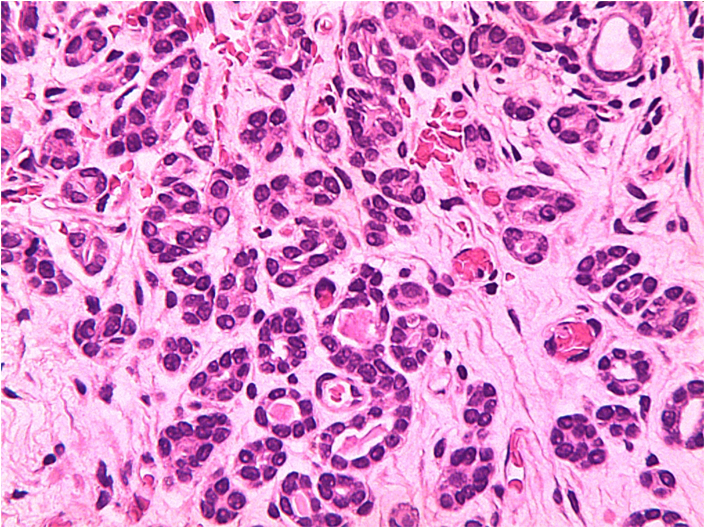
Fig. 2.
Histological aspect of nephrogenic adenoma, with multiple tubular structures, mimicking renal tissue (X400).
Discussion
Nephrogenic adenoma (NA) was first described in 1949 by Davis under the name of hamartoma.3 This disease, sometimes called nephrogenic metaplasia, is an unusual benign lesion of the urinary tract mostly found in association with urothelial injury or inflammation.2 It is most frequently found as small isolated lesions (<1cm), but it can occur in larger areas (up to 7cm) or in a multifocal presentation. Histologically, the classic form of NA is composed of tubules, resembling renal structures, confined to the lamina propria.1,4 The tubules are often surrounded by a hyalinized membrane, lacking the desmoplastic stromal response and the mitotic activity which could support a diagnosis of invasive carcinoma.1 When NA affects the prostatic urethra, its morphology may mimic prostatic adenocarcinoma, presenting with a pseudo infiltrative pattern, containing small tubules with no basal cell layer. The diagnosis of prostatic NA can be difficult; it can be mistaken for adenocarcinoma due to confounding features such as a moderate cytologic atypia. However, the lack of mitoses and of significant cytologic atypia, papillary architecture in the adjacent urothelium, amongst other alterations in the inflammatory stroma, guide the diagnosis towards NA. Immunohistochemical analysis may provide additional evidence for the diagnosis of NA, such as a negative expression of P63 and a positive expression of alpha-methylacyl-CoA racemase (AMACR), PAX2, cytokeratin 7 (CK7) and epithelial membrane antigen1,4,5
NA occurs over a very wide age range and affects mainly males in a 2:1 ratio. It mostly affects adults; nevertheless, it may occur in children (approximately 10% of cases).1,2 The most common location for the development of NA is the urinary bladder, although it may be found less frequently in the urethra, in the ureters or in the renal pelvis.1,2,4 Risk factors for NA are mostly events that bring injury or inflammation to the urinary tract mucosa, such as prior surgery, endourological procedures, infection, calculi, radiation therapy and trauma. Also, immunosuppressive therapy, renal transplantation and bacillus Calmette-Guérin (BCG) therapy for urothelial carcinoma of the bladder may lead to NA.1,2,4 The progressive increase in the diagnoses of NA in the prostatic urethra over the last years may be due to the higher frequency of prostate needle biopsies performed in the process of prostate cancer early detection. Likewise, TUR of the prostate and laser therapy performed either to alleviate symptoms of BPH or to treat suspicious lesions appear to be associated with NA.5
The endoscopic appearance of the lesion is usually of a papillary pattern; nonetheless, polypoid, fungating or sessile lesions have been reported and the clinical manifestations may vary from an absence of urinary tract symptoms – with the lesion being an incidental finding in the investigation of microscopic hematuria or in follow up examinations of patients with a previous history of cancer of the urinary tract – to a history of frank hematuria (as in our case), dysuria and urinary frequency.1,2,4 In any case, regardless of the presentation of NA, TUR seems to be an efficient treatment, promoting adequate and long-lasting symptoms relief. Very few cases recur; however, even recurrences seem to respond well to TUR of the lesion.2
Conclusion
Nephrogenic adenoma of the prostate is a benign lesion of the urothelium, which may course with hematuria, dysuria, and frequent urination. It has a very strong correlation with previous urological procedures, needle biopsies, and, more recently, as in the case described, laser therapy of the prostate, and is treatable with TUR. The increased utilization of laser therapy for BPH must heighten the awareness for this condition, which may commonly be mistaken for prostatic adenocarcinoma.
Section heading
Endourology.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors have no conflict of interest.
Footnotes
- Pontifical Catholic University of Rio Grande do Sul: Av. Ipiranga, 6681, Partenon – Porto Alegre / RS – Brazil.
- Hospital Moinhos de Vento: Rua Ramiro Barcelos, 910, Moinhos de Vento – Porto Alegre / RS – Brazil.
References
- 1.Kunju L.P. Nephrogenic adenoma report of a case and review of morphologic mimics. Arch Pathol Lab Med. 2010;134(10):1455–1459. doi: 10.1043/2010-0226-CR.1. [DOI] [PubMed] [Google Scholar]
- 2.Peeker R., Aldenborg F., Fall M. Nephrogenic adenoma - a study with special reference to clinical presentation. Br J Urol. 1997;80(4):539–542. doi: 10.1046/j.1464-410x.1997.00418.x. [DOI] [PubMed] [Google Scholar]
- 3.Davis T.A. Hamartoma of the urinary bladder. Northwest Med. 1949;48(3):182–185. https://pubmed.ncbi.nlm.nih.gov/18114097/ [PubMed] [Google Scholar]
- 4.Ortiz-Rey J.A., Antón-Badiola I., Pérez-Pedrosa A., Peteiro-Cancelo Á., González-Carreró J. Nephrogenic adenoma: an immunohistochemical analysis using biotin-free methods. Appl Immunohistochem Mol Morphol. 2012;20(4):386–391. doi: 10.1097/PAI.0b013e3182444a4e. [DOI] [PubMed] [Google Scholar]
- 5.Allan C.H., Epstein J.I. Nephrogenic adenoma of the prostatic urethra: a mimicker of prostate adenocarcinoma. Am J Surg Pathol. 2001;25(6):802–808. doi: 10.1097/00000478-200106000-00013. [DOI] [PubMed] [Google Scholar]