Abstract
Gestational choriocarcinoma with kidney and lung metastases with delayed presentation after term pregnancy is rare event and not described frequently in literature. We describe a rare case of 24-year-old female with hematuria after 3 years of term delivery. Management includes chemotherapy and even renal embolization in case of life threatening hematuria.
Keywords: Choriocarcinoma, Metastases, Renal artery embolization
Introduction
Choriocarcinoma is one of the highly malignant tumor in women of reproductive age. Some of the unique features of this tumor are: Its aggressive hematogenous spread and excellent response to chemotherapy. Choriocarcinoma occurs either in gestational or non-gestational form. Distinguishing between their origin is important for purpose of management. Gestational choriocarcinoma with kidney and lung metastases with delayed presentation after term pregnancy is rare event and not described frequently in literature.1 Cure rate of choriocarcinoma is >90% even in metastatic context because of its excellent sensitivity to chemotherapy.2
Case report
24-year-old married female presented with painless total hematuria in ER for 4 days. It was associated with passage of clots and dizziness and weakness. No history of trauma, no bleeding from other sites, no fever, no abdominal pain. She was married and had term delivery 3 years ago with regular menstrual cycle. Her vitals were stable except for tachycardia and pallor. Immediate resuscitation was done and blood investigation along with blood grouping was sent. Her hemoglobin was 6.2 gm/dl and 3 units of blood transfused. Per abdominal examination was normal. Per vaginal examination showed no abnormality. Ultrasonography done at ER showed Bilateral heterogeneous multi-cystic lesions in kidneys with clot in urinary bladder suggestive of bilateral renal cell carcinoma with bleeding. Urine routine examination showed packed RBC per high power field. Three-way catheter was placed and continuous bladder irrigation was started.
Urine pregnancy test was done as part of protocol in patient of reproductive age group which was positive. Renal function test was normal and patient underwent contrast enhanced Computed tomography of abdomen and pelvis (CECT) which showed multiple heterogeneously enhancing complex cystic lesion hyper-vascular, larger on left side 7 × 3 cm involving upper and middle pole and upper pole on right kidney. Bilateral adnexa were normal and no retroperitoneal lymph nodes were identified (Fig. 1, Fig. 2). Quantitative beta hcG was very high (403,700 mIU/mL) and gynecological consultation and evaluation was done. Tran-Vaginal Ultrasound was normal. Chest X-Ray showed multiple bilateral cannon ball metastases (Fig. 3). Hematuria stopped after 2 days and catheter was removed and medical oncology consultation done.
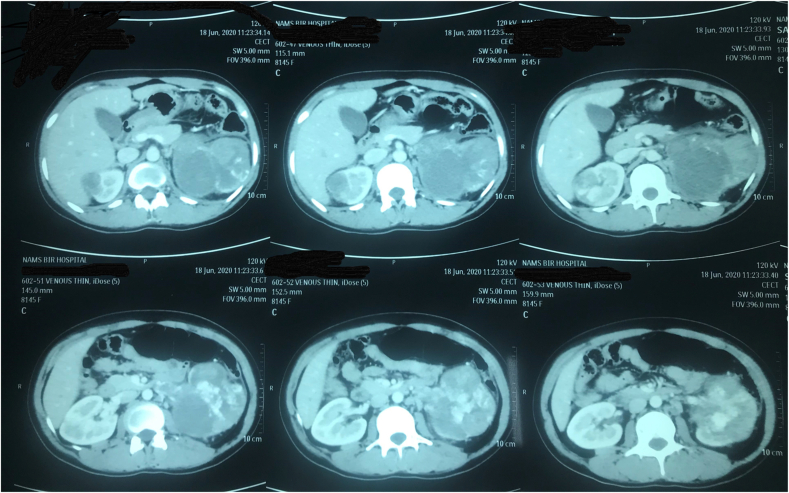
Fig. 1.
Shows CECT Abdomen and pelvis (axial films) active contrast extravasation on left kidney suggestive of active bleeding.
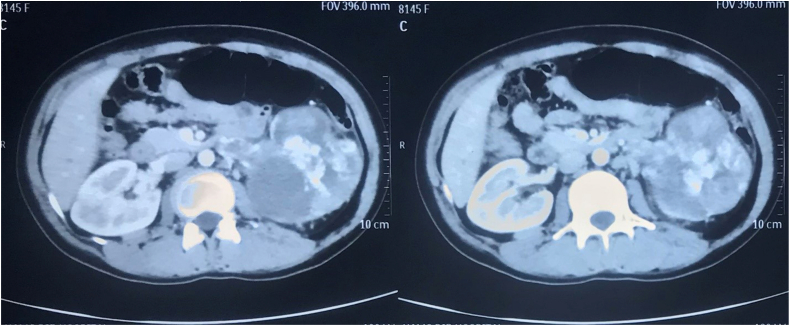
Fig. 2.
Shows CECT Abdomen and pelvis (axial films) with bilateral hypervascular heterogenous renal lesion with larger mass on left kidney mainly in upper and mid pole.
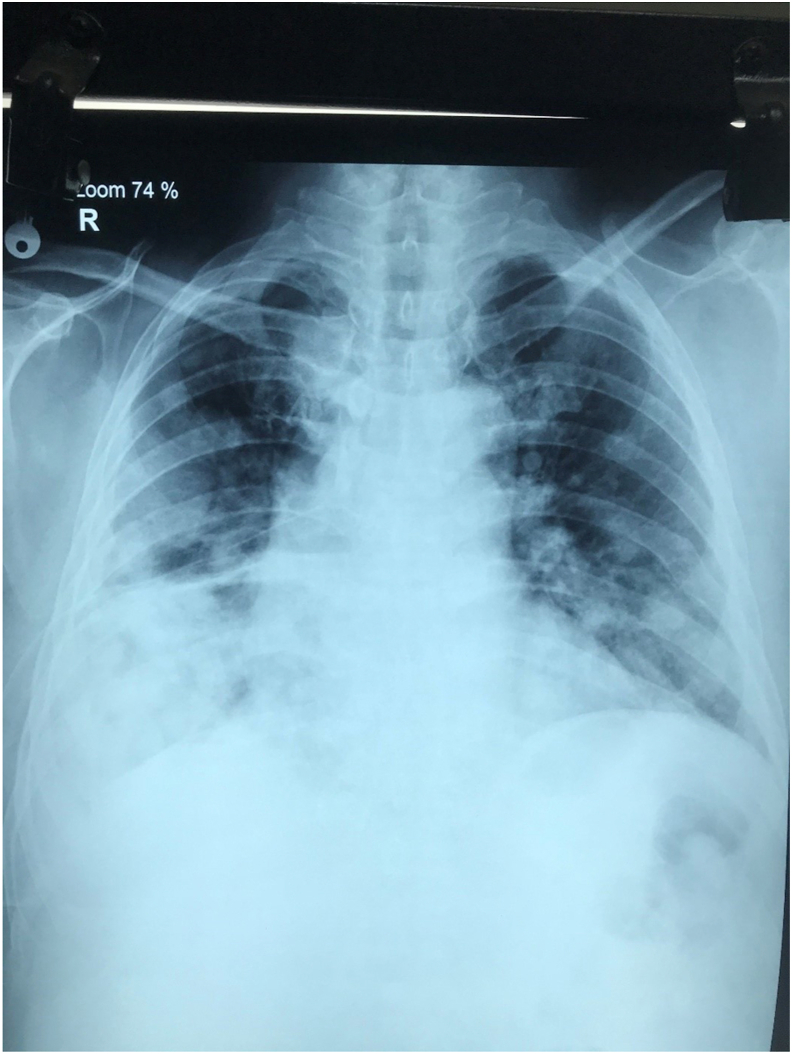
Fig. 3.
Shows chest X Ray with multiple bilateral cannon ball metastases.
Diagnosis of Gestational choriocarcinoma with bilateral renal and lung metastases (FIGO Stage IV high risk) with unknown primary was made and multidisciplinary discussion was done. Multidrug chemotherapy was planned. Patient received 2 cycles of EMA/EP (platinum-based) regimen (etoposide 100 mg/m2 on Day 1, methotrexate 300 mg/m2 on Day 1, dactinomycin 0.5 mg on Day 1, etoposide 150 mg/m2 on Day 8, and cisplatin 75 mg/m2 on Day 8). Following first cycle of chemotherapy, beta-hCG decreased to 8763 mIU/mL. Her beta-hCG level dropped to 2912 MIU/ML and patient was responding well to treatment but she didn't show up for follow up for 3 months and presented with gross hematuria again in ER. Laboratory investigation showed hemoglobin of 3.4 gm/dl. Patient was resuscitated and 10 units of blood transfusion done. CECT Abdomen and pelvis was repeated which showed left kidney replaced with tumor and active arterial bleeding and selective embolization of renal arterial branches as a lifesaving procedure. Patient was stable after the procedure and planned for further chemotherapy.
Discussion
Gestational choriocarcinoma is commonly uterine in origin and can occur in any type of pregnancy and at variable duration during/after pregnancy. Sometimes primary uterine tumor undergoes spontaneous necrosis or complete regression and extra-uterine metastases manifest late. Case similar to ours with unknown primary with kidney and lung metastases has been mentioned in literature.3
Our patient had term delivery 3 years ago and regular menstrual cycle afterwards. We haven't done genetic analysis for our patient and based on clinical and imaging findings we have concluded; this is case of gestational choriocarcinoma with metastases.
Modified WHO prognostic scoring system4 as adopted by FIGO for our patient is FIGO stage IV; 15 This score falls under high risk group. Patients with non-metastatic (Stage I) and low-risk metastatic (Stages II and III, score < 7) GTN are recommended to receive single-agent chemotherapy, with resulting survival rates approaching 100%. Patients classified as having high-risk metastatic disease (Stage IV and Stages II or III with a score > 7) should be treated more aggressively with multi-agent chemotherapy and adjuvant radiation or surgery, which may achieve cure rates of 80–90%.5 In our patient, we planned to start chemotherapy and response to chemotherapy was excellent. But she was lost to follow up for 3 months again presented with life threatening hematuria and recurrence of growth as shown by resurge of beta-hCG level. She was subsequently managed with angio-embolization of bleeding renal arteries and further chemotherapy.
Conclusion
In summary, though uncommon, choriocarcinoma can present with variety of extrauterine clinical manifestations. The possibility of choriocarcinoma should be considered for women of reproductive age exhibiting unexplained hematuria.
Declaration of competing interest
Authors have no conflict of interest to disclose.
Consent from patient taken for publication without the disclosure of identity.
Acknowledgement
My sincere Acknowledgement to Dr. Manish Man Pradhan, Dr. Diwas Gyanwali, Dr. Prem Raj Sigdel, Dr. Sampanna Chudal Mrs Kunja Shrestha Parajuli, Miss Avishree Parajuli.
References
- 1.Park S.Y., Lee D.E., Park H.J., Kim K.C., Kim Y.H. Retroperitoneal nongestational choriocarcinoma in a 25-year-old woman. Obstet Gynecol Sci. 2014;57:544e8. doi: 10.5468/ogs.2014.57.6.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Biscaro A., Braga A., Berkowitz R.S. Diagnosis, classification, and treatment of gestational trophoblastic neoplasia. Rev Bras Ginecol Obstet. 2015;37:42e51. doi: 10.1590/SO100-720320140005198. [DOI] [PubMed] [Google Scholar]
- 3.Li H.M., Hou W.C., Lai Y.J. Gestational choriocarcinoma with renal and pulmonary metastases lacking a primary uterine origin. Taiwan J Obstet Gynecol. 2016;55(6):881–885. doi: 10.1016/j.tjog.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 4.FIGO Committee on Gynecologic Oncology Current FIGO staging for cancer of the vagina, fallopian tube, ovary, and gestational trophoblastic neoplasia. Int J Gynaecol Obstet. 2009 Apr;105(1):3–4. doi: 10.1016/j.ijgo.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 5.Lurain J.R. Gestational trophoblastic disease II: classification and management of gestational trophoblastic neoplasia. Am J Obstet Gynecol. 2011;204:11e8. doi: 10.1016/j.ajog.2010.06.072. [DOI] [PubMed] [Google Scholar]