Abstract
A competency-based approach to health human resources (HHR) planning is one that explicitly considers the spectrum of knowledge, skills and judgement (competencies) required for the health workforce based on the health needs of the relevant population in some specific circumstances. Such an approach is of particular benefit to planners challenged to make optimal use of limited HHR as it allows them to move beyond simply estimating numbers of certain professionals required and plan instead according to the unique mix of competencies available from the existing health workforce. This kind of flexibility is particularly valuable in contexts where healthcare providers are in short supply generally (e.g. in many developing countries) or temporarily due to a surge in need (e.g. a pandemic or other disease outbreak). A pilot application of this approach using the context of an influenza pandemic in one health district of Nova Scotia, Canada, is described, and key competency gaps identified. The approach is also being applied using other conditions in other Canadian jurisdictions and in Zambia.
Keywords: Health workforce planning, healthcare competencies, needs-based planning, competency-based planning, pandemic influenza
KEY MESSAGES.
When planning for health workforces in the context of short- or long-term shortages, consideration of the specific competencies required of the health workforce can help to ensure efficient use of scarce health human resources.
An analytical framework for competency-based planning has been developed to allow health workforce planning based on the competencies required to deliver the specific services planned to address key population health conditions.
Competency-based planning can be used to guide pre- and post-licensure training, recruitment and management of healthcare providers.
The framework has been pilot tested in the context of an influenza pandemic in one District Health Authority in Nova Scotia, Canada.
Introduction
Background
One of the most challenging tasks healthcare planners face is aligning the workforces they plan and manage with the health needs of the populations they serve, while ensuring efficient and effective use of human and non-human resources. This task becomes more daunting when resources (both human and non-human) are limited and emerging health conditions add to the unpredictability of resource use. Health human resources (HHR) planning typically involves understanding or planning for the production and supply of, demand for and use and deployment of health professionals to meet the needs of the population. Traditional HHR planning methods have limited their attention to demographic change by applying current provider-to-population ratios or levels of service use by age and gender to the estimated changes in the size and mix of the future population (Centre for Workforce Intelligence 2009; Cook 2009; Lavieri and Puterman 2009; Spetz 2009; Barber and López-Valcárcel 2010; Barnett et al. 2010; Yun et al. 2010). Such methods implicitly assume the healthcare needs of the population, the types and quantity of healthcare services delivered to meet those needs and the ways in which such services are delivered are constant over time. In contrast, needs-based HHR planning methods allow policy makers to explicitly consider the separate effects of each of these factors as they plan for their healthcare workforces (Birch et al. 2007). In this article, we describe the development and testing of a competency-based HHR assessment and planning tool in the context of an influenza pandemic in one District Health Authority (DHA) in Nova Scotia, Canada.
Having an understanding of how the healthcare competencies of the health workforce—defined for the purposes of this work as the combinations of knowledge, skills and judgement they possess—are aligned with the health needs of the population they serve can help to inform this type of planning. Within the broad category of needs-based planning methods, competency-based approaches are designed to allow policy makers to move beyond profession-centred plans and consider the specific combinations of knowledge, skills and judgement (competencies) required to meet healthcare needs. Such consideration is consistent with the growing call for more comprehensive approaches to HHR planning in general (Bloor and Maynard 2003; Campbell et al. 2008; Birch et al. 2009; Stordeur and Léonard 2010) and in pandemic or emergency planning specifically (Sandrock 2010). Competency-based approaches are intended to offer increased flexibility to planners compared with typical profession-specific models and are of particular value in cases where healthcare resources (human or non-human) are especially scarce, where the health needs of the population to be served are not well understood, or where the respective roles of the provider groups involved in service delivery are not well-defined.
An influenza pandemic creates a unique set of challenges to which the healthcare system must adapt. Illness is widespread and affects patients as well as healthcare providers (HCPs) and their families. Resources cannot be brought in from other jurisdictions as the outbreak is global in scope. A range of interventions, such as immunization programmes, public health measures and new approaches to treatment and prevention must be implemented. Furthermore, it is difficult to maintain the usual range of essential healthcare services, such as cardiac emergency care and essential (non-elective) surgeries. The Severe Acute Respiratory Syndrome crisis of 2003 and the global H1N1 influenza pandemic of 2009–10 emphasized the importance of containing an epidemic and providing the appropriate personnel to care for the ill. In the latter case, there were laboratory confirmed cases of H1N1 in more than 200 countries, including more than 18 000 deaths (WHO 2010). There continues to be concern in the public health community that other novel influenza strains, such as H5N1 with its case fatality rate of more than 50% (e.g. Blumenshine et al. 2008; Ten Eyck, 2008), will mutate such that they will transmit efficiently among humans.
It appears the Public Health Agency of Canada (2006) was correct in its prediction that, in an event of an influenza pandemic,
… there will be a marked increase in demand for people (health care providers and others) to care for the sick and for appropriate locations and equipment to facilitate the provision of health care. Communities and health care organizations will need to have plans in place that will address what will be done when the health care system is overwhelmed and care must be provided by persons, both health care workers and volunteers, doing work that is not normally part of their daily activities and possibly in settings not usually used for health care.
In this example of a surge in requirements for HHR it can be seen that optimal use of these resources is critical to the viability of the system. There are feelings of unpreparedness for such an event in a number of jurisdictions (e.g. O’Sullivan et al. 2008; Ten Eyck 2008) during which healthcare planners and practitioners, among others, may face difficult ethical decisions regarding the allocation of limited healthcare resources (Torda 2006; Kass et al. 2008). To plan for the challenging circumstances of a pandemic, simulation models and other kinds of planning tools can be of value (Moghadas et al. 2009), and there are several such tools available to planners, such as Influsim (e.g. Eichner et al. 2007). However, few if any of these tools explicitly consider the range of competencies that may be required of the workforce during an influenza pandemic. The value of competency-based planning in the context of a pandemic lies in its explicit consideration of the service needs of populations at risk in such circumstances and how the competencies of the available health workforce align—or do not—with those needs. Such knowledge can guide the development of policies for staff deployment, education and training, and hiring with a view towards pandemic preparedness; this is in keeping with recent recommendations by the European Society of Intensive Care Medicine’s Task Force for Intensive Care Unit Triage during an Influenza Epidemic or Mass Disaster (Sandrock 2010).
Objective
The purpose of this research was to test and validate a competency-based HHR planning framework and tool, focusing on influenza care competencies (ICCs) as an illustration. This approach considers relevant legal and regulatory frameworks of each care setting and is intended to enhance the management of HHR according to population health needs.
Methods
This work has been guided by a needs-based conceptual framework (Tomblin Murphy and O’Brien-Pallas 2005) and analytical framework (Birch et al. 2007) and builds on earlier work in the province of Ontario (Tomblin Murphy et al. 2006), where the competency-based approach was initiated. In this study, the application of the approach is demonstrated in Pictou County DHA in Nova Scotia, Canada, in progressing from the theoretical stage to the pilot testing phase of a framework and a tool. The competency-based framework used in this study is represented visually in Figure 1.
Figure 1.
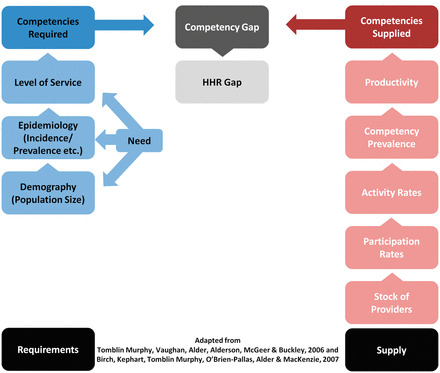
Competency-based HHR planning framework.
The components of the competency-based framework are:
- (1) Competencies required: the components on this side of the framework examine the population’s needs for healthcare services, according to the following determinants:
- Demography (population size) refers to the number of people potentially needing care broken down according to relevant characteristics, such as age and sex.
- Epidemiology (health status, attack rate, mortality and morbidity) refers to the distribution of severity of illness across the population; the proportion of individuals who become ill, and within that group, the variance of healthcare needs, from those who can care for themselves to those who require intensive care in a hospital.
- Level of service will vary by care setting. Although the appropriate level of service for a patient is ideally based on individual needs, it is realistically influenced by other factors, such as geography (e.g. how far from care do vulnerable elderly live?), existing infrastructure (e.g. the location of hospitals and clinics and how they are staffed), the patient’s social support and budget constraints. Needs must be considered in terms of the setting and its associated level of care. For instance, the delivery of services and settings can include primary health care, acute hospital care and critical care. For the purposes of this study, level of service is represented as the proportion of patients within each care setting who require each specific care competency.
Multiplying these three components—demography, epidemiology and level of service—in the same manner described by Birch et al. (2007) yields the number of patients requiring each competency. In a simple application, population would be the number of people living in the jurisdiction, epidemiology would be the proportion of them who are ill and level of service would be the proportion of patients who would require a respiratory assessment, given that they are ill. Multiplying each of these gives the number of respiratory assessments required by a population of a given size and illness profile. This figure can then be compared with the number of patients who can be ‘covered’ with each competency by the existing health system. The latter quantity is calculated by the other side of the framework as follows.
- (2) Competencies supplied refer to the identification of the variety and quantity of competencies (knowledge, skills and judgement) that are available to deliver the necessary level of service in different care settings. The number of patients that can be supplied with these competencies will depend on the five components on this side of the framework:
- Stock of providers: the number of HCPs available to provide care. This includes the registered/licensed workforce currently providing patient care and those not providing patient care (e.g. administrators, researchers or educators).
- Participation rate: the proportion of the stock that is involved in the delivery of patient care. This rate acknowledges that there are those who are working in clinical environments but may not be participating in care.
- Activity rate: the number of hours spent in the delivery of service (i.e. worked hours per provider). This rate can be increased by reducing absenteeism (e.g. with prophylactic antiviral medication), shifting part-time staff to full-time or even implementing overtime for short periods of high need.
- Competency prevalence: the prevalence of competence among the existing stock of providers; in other words, the proportion of available providers who currently possess the knowledge, skills and judgement to perform each required service. For instance, how many have the ability to triage, administer prophylaxis, screen for vaccine eligibility, or prescribe medication?
- Productivity of HCPs refers to the average rate of services per unit time delivered to people requiring care. It depends upon a variety of factors, including the proportion of worked hours given to care for patients, how work is organized, technology inputs, and other inputs, such as availability of other HCPs, volunteers and health profession students.
Combining these five components provides an estimate of the number of patients who can be provided each competency by the existing health workforce. Multiplying the first three components translates the existing health workforce from a headcount to a number of full-time equivalents (FTEs). Multiplying this value by the competency prevalence yields the number of FTEs available with each competency. Finally, multiplying this figure by productivity produces the number of patients who can be ‘covered’ with each competency by the existing health workforce given its make-up.
Identifying main health concerns
The first step in applying a competency-based planning framework is to determine the most pressing health concerns facing the population in question. In the context of an influenza pandemic, that disease becomes the focus; however, in other situations health conditions can be prioritized through examinations of administrative data, considerations of the burdens of various diseases and consultations with key community stakeholders.
Development of competencies list
To implement a competency-based approach to HHR planning, it is necessary to understand the variety of services that are required, or planned to be delivered, to address the specific conditions and circumstances for which the approach is to be used. From this, a list of the specific competencies required of the health workforce to deliver those services can be developed. In this case, it was necessary to develop a list of the competencies that would be required by the population of Nova Scotia during an influenza pandemic. This was done by updating a list developed for another Canadian province (Tomblin Murphy et al. 2006) in keeping with the Nova Scotia Department of Health’s unique Pandemic Plan (Province of Nova Scotia 2007).
To validate this set of ICCs in Nova Scotia, a 1-day workshop was held with more than 20 key clinical HCPs representing different disciplines from across the province. In this forum the project team, in collaboration with the provincial Department of Health, obtained the opinions and expertise on the ICCs that would be required to provide both direct care for ill patients, as well as additional support in the form of administrative, educational, prevention and surveillance activities. Revisions proposed during the workshop included requests for additional detail and/or clarification to listed ICCs and suggestions to add new ICCs. Overall, the workshop confirmed that the list of ICCs was appropriate and representative of the Nova Scotia context.
The ICCs are organized under six main ‘domains’: Infection Control and Prevention, Occupational Health, Public Health, Care for Influenza Patients, Education and Administrative/Support. The full list of ICCs by domain is provided in Table 1.
Table 1.
Nova Scotia ICCs
| Domain #1: Infection control and prevention | |
| 1. | Develop and implement a surveillance programme for influenza and influenza-like illness at a specific care site (co-ordinate data collection, summarize outbreak progression, submit report to care site officials and/or Public Health officials) |
| 2. | Co-ordinate with Public Health to meet surveillance requirements |
| 3. | Advise HCPs regarding appropriate patient placement to minimize/prevent infectious disease transmission |
| 4. | Advise HCPs, patients and visitors regarding barrier precautions, hand hygiene and other measures to minimize infectious disease transmission |
| 5. | Advise on appropriate cleaning, disinfection and sterilization of medical equipment |
| Domain #2: Occupational health | |
| 6. | Screen staff for illness |
| 7. | Identify staff who, due to illness or burnout, need assistance/rest |
| 8. | Identify workplace hazards related to risks from influenza |
| 9. | Provide on-going education and training related to such hazards |
| 10. | Rectify such hazards |
| 11. | Systematically monitor absenteeism (by various causes) |
| 12. | Administer influenza immunization to staff (where appropriate) |
| 13. | Monitor and manage adverse events associated with immunization (surveillance) among staff |
| 14. | Administer antiviral prophylaxis to staff (where appropriate) |
| 15. | Monitor and manage adverse events associated with prophylaxis (surveillance) among staff |
| 16. | Provide psychosocial support for staff |
| 17. | Recognize the logistical support needs of staff (e.g. food, family support and pet care) |
| Domain #3: Public health | |
| a. Competence in surveillance and infectious disease control | |
| 18. | Develop and implement active, passive and enhanced surveillance in the population at large |
| 19. | Plan and conduct epidemiological analysis (design databases, co-ordinate data collection, conduct descriptive analyses, summarize outbreak progression and prepare reports) |
| 20. | Manage cases identified in the community (including initial assessment, triage, specimen collection, referral, follow-up, etc.) |
| b. Competence in immunization | |
| 21. | Organize and conduct mass immunization clinics in a community setting |
| 22. | Screen for eligibility for immunization |
| 23. | Perform an assessment of medical history, contraindications, allergies, etc. |
| 24. | Obtain informed consent for immunization |
| 25. | Dispense vaccine for administration |
| 26. | Implement appropriate vaccine safety (maintenance of cold chain during storage and transport) |
| 27. | Administer vaccine |
| 28. | Recognize and manage initial adverse events (e.g. anaphylaxis) occurring in community immunization clinics |
| 29. | Monitor for adverse events associated with immunization among members of the public (surveillance) |
| c. Competence responding to people affected by stress (caused by threat of illness) | |
| 30. | Provide psychosocial support to the public |
| 31. | Provide pastoral/spiritual support/guidance to the public |
| Domain #4: Care for influenza patients | |
| 32. | Receive and direct patients seeking patient care (manage patient flow within a care site) |
| 33. | Take a screening history of the chief complaint and relevant aspects of the past medical history, current medications, etc. |
| 34. | Triage patients according to acuity of illness and need for care, and referring to appropriate care setting (primary and secondary assessment, hospital, emergency department, non-traditional care site and community) |
| 35. | Perform appropriate hand hygiene |
| 36. | Don and remove appropriate personal protective equipment (PPE) |
| 37. | Conduct a respiratory assessment (heart rate, respiratory rate, inspection, percussion, palpation and auscultation, etc.) |
| 38. | Assess level of consciousness |
| 39. | Take a complete health history and perform a physical examination |
| 40. | Order clinical diagnostic tests |
| 41. | Perform clinical laboratory testing service (haematology, chemistry, etc.) |
| 42. | Provide diagnostic imaging services |
| 43. | Interpret the results of history, physical examination, chest X-ray and (point of care) laboratory tests, leading to a diagnosis |
| 44. | Prescribe medication |
| 45. | Provide pharmacy services |
| 46. | Transport patients including assessment and provision of care to patients during transport |
| 47. | Perform basic life support techniques (CPR) |
| 48. | Provide assistance with activities of daily living to patients |
| 49. | Provide psychosocial support to patients and families |
| 50. | Provide pastoral/spiritual support/guidance to patients and families |
| 51. | Provide support to patients in their homes (e.g. delivery of meals, groceries, medication, care for dependents, etc.) |
| 52. | Measure temperature |
| 53. | Take pulse |
| 54. | Take blood pressure |
| 55. | Take venous blood samples |
| 56. | Obtain nasal samples |
| 57. | Obtain nasopharyngeal samples |
| 58. | Obtain throat swabs (with tip touching posterior pharynx) |
| 59. | Obtain specimens for other cultures (e.g. urine, stool and wound) |
| 60. | Measure oxygen saturation |
| 61. | Screen for eligibility for antiviral treatment/prophylaxis |
| 62. | Obtain consent for antiviral treatment/prophylaxis |
| 63. | Prescribe antivirals for treatment/prevention of influenza |
| 64. | Dispense antivirals for treatment/prevention of influenza (from Public Health or hospital supply) |
| 65. | Monitor and manage adverse events associated with treatment/prophylaxis |
| 66. | Admit a patient or discharge a patient to home or to another care setting |
| 67. | Obtain electrocardiogram |
| 68. | Order chest X-rays and CT scans |
| 69. | Perform intramuscular injections |
| 70. | Start intravenous lines |
| 71. | Maintain intravenous lines (site and tubing) |
| 72. | Set up oxygen |
| 73. | Check oxygen administration setups |
| 74. | Administer medication by inhalation |
| 75. | Administer medication by injection (subcutaneous and intramuscular) |
| 76. | Administer medication orally |
| 77. | Administer medication by intravenous route |
| 78. | Administer medication by intravenous push |
| 79. | Suction patients who are not intubated or trached |
| 80. | Insert and maintain Foley catheters |
| 81. | Perform intubation |
| 82. | Set up ventilation (establishing ventilation parameters) |
| 83. | Monitor ventilation |
| 84. | Insert a central line |
| 85. | Maintain a central line |
| 86. | Insert an arterial line |
| 87. | Maintain an arterial line |
| 88. | Administer medication by continuous infusion |
| 89. | Suction intubated/ventilated patients |
| 90. | Undertake Advanced Cardiac Life Support interventions |
| 91. | Manage inotropes and vasopressors |
| 92. | Manage insulin infusions |
| 93. | Manage dialysis |
| 94. | Decide on palliative care/withdrawal of care |
| 95. | Pronounce cessation of life |
| 96. | Sign death certificate |
| Domain #5: Education | |
| a. Competence in educating HCPs (including alternate care providers when appropriate) | |
| 97. | Educate HCPs about influenza in general and pandemic influenza in particular |
| 98. | Educate HCPs about Nova Scotia’s emergency measures preparedness and its pandemic health services delivery model |
| 99. | Educate HCPs about how to use assessment, triage and management protocols (for patients with and without co-morbidities) |
| 100. | Educate HCPs about the ethical considerations and decision-making framework of Nova Scotia’s Health System Pandemic Influenza Plan |
| 101. | Educate HCPs about the chain of command and responsibilities within the Nova Scotia emergency response plan |
| 102. | Educate HCPs about advance directives (i.e. medical consents and durable powers of attorney) |
| 103. | Educate HCPs about individual preparedness (e.g. family support while working, care for ill family members, wills, etc.) |
| 104. | Educate HCPs about PPE (i.e. what to wear, when and how) |
| 105. | Educate HCPs about immunization (delivery, safety, etc.) |
| 106. | Educate HCPs about self-screening for influenza illness or other illness (physical and psychological) |
| 107. | Educate HCPs about deciding to discontinue/continue working |
| b. Competence in educating the general public | |
| 108. | Educate the public about influenza in general and pandemic influenza in particular |
| 109. | Educate the public about Nova Scotia’s pandemic health services delivery model |
| 110. | Educate the public about the ethical considerations and decision-making framework of Nova Scotia’s Health System Pandemic Influenza Plan |
| 111. | Educate the public about disease prevention strategies (e.g. mode of transmission, hand hygiene, isolation and immunization) |
| 112. | Educate the public about self-care (includes responding to questions by phone, in-person and web) |
| 113. | Educate the public about individual preparedness (e.g. caring for ill family members, palliative care, wills, etc.) |
| 114. | Develop health education strategies and associated materials |
| 115. | Train members of the public who have volunteered to assist in various care settings |
| Domain #6: Administration and support | |
| a. Competence in managing a care setting (public health, primary care, long-term care, acute care or intensive care) | |
| 116. | Organize and staff a traditional care setting for markedly changing patient volumes |
| 117. | Establish and manage a non-traditional care site (e.g. gymnasium set up as an influenza care facility) |
| 118. | Assess staff competencies and match them to needs (including support staff, technical staff, volunteers and other staff not usually assigned to that care site) |
| 119. | Schedule, deploy and redeploy staff |
| 120. | Carry out succession and contingency planning |
| 121. | Make decisions about the allocation of resources (human and non-human) based on an ethical framework |
| 122. | Manage command and control structures |
| 123. | Supply chain management |
| 124. | Manage the availability of beds |
| 125. | Manage pharmacy services (including pharmaceutical storage and maintenance of cold chain for vaccines) |
| 126. | Manage clinical laboratory services |
| 127. | Manage diagnostic imaging services |
| 128. | Manage health records services (including knowledge of freedom of information policies and practices) |
| 129. | Design and implement a security plan for the protection of staff, patients, supplies and information |
| 130. | Manage food services (for patients, families and staff) |
| 131. | Manage laundry services (commercial and/or in-house) |
| 132. | Manage housekeeping services |
| 133. | Establish and manage alternate morgue sites/temporary morgues |
| 134. | Manage waste disposal (including biohazardous waste) |
| 135. | Manage a care facility in terms of ventilation, creation of isolation space, etc. |
| 136. | Manage information infrastructure (telephones, email, hospital information system and surveillance infrastructure) |
| 137. | Manage parking |
| 138. | Manage transportation of laboratory specimens |
| 139. | Manage transportation of biohazardous waste |
| 140. | Manage transportation of dangerous goods |
| 141. | Manage transportation of staff |
| 142. | Manage transportation of patients |
| 143. | Manage transportation and preparation of bodies for burial/cremation |
| b. Competence in co-ordinating patient flow | |
| 144. | Answer questions about navigating the care delivery system |
| 145. | Direct patients to appropriate care sites |
| c. Competence in managing communications | |
| 146. | Develop and implement internal communications plans (e.g. status of pandemic) |
| 147. | Develop and implement external communications plans (e.g. with other levels of care, Public Health, community including non-healthcare organizations) |
| 148. | Managing confidentiality (emails, telephone calls, face-to-face and documents) |
| 149. | Carry out risk management/risk communication |
| 150. | Provide general leadership to a care setting population (e.g. assuming the role of leader, directing and delegating, responding to group needs, problem solving and role modelling) |
Alignment of competencies to regulated health professions in Nova Scotia
An additional workshop was held with more than 20 representatives from regulatory colleges and professional associations in the province, as well as a legal expert in provincial health professional legislation, to ensure that the competency-based approach being tested was appropriate within the legal and regulatory frameworks of Nova Scotia. In Nova Scotia, most health professions are self-regulated, rather than covered by comprehensive legislation. Each ICC was reviewed and discussed by the group as a whole to determine which competencies were regulated acts, and, therefore, which professions could perform them within their scopes of practice. In addition, there was substantial discussion about how these ICCs could be managed during a crisis; that is, some ICCs, while not within a particular profession’s scope of practice, could be performed by other professions. For example, the ICC, ‘Administer influenza immunization to staff (where appropriate)’, is a regulated act that is clearly within the regulated scopes of practice for Physicians, Nurse Practitioners, Registered Nurses and Licensed Practical Nurses. However, depending on the urgency of the situation and the needs of the population, a broader interpretation of the legislation could ensure that there are more professions available to perform this service, including dentists, pharmacists or physiotherapists. As a result of this workshop, many of the linkages were adapted and/or refined to better represent the regulatory context in Nova Scotia.
Influenza care competency survey
To determine the prevalence of each ICC among the health workforce, a competency self-assessment questionnaire was developed. The questionnaire asks individuals to consider the competencies they currently use and/or have previously used and indicate their self-assessed level of competence using a five-point Likert scale: 1 = ‘I am not competent to perform it’, 2 = ‘I have performed it in the past, but I am not currently competent’, 3 = ‘I am competent to perform it with supervision’, 4 = ‘I am competent to perform it without supervision’ and 5 = ‘I am competent to perform it and could supervise others performing it’.
Questions within this section of the survey cover the six domains earlier noted. The survey also includes questions asking respondents to indicate their profession, work setting, primary care of practice, their level of work activity (hours typically worked per week) and their productivity (patients/clients seen per week).
The ICC survey was pilot-tested in late 2008 with over 20 providers from across Nova Scotia assess its clarity, flow, construct validity and internal consistency. It was re-administered to the same group within 3 weeks to assess test/re-test reliability. The survey was further refined based on the results of the pilot testing, and research ethics and privacy impact assessment (PIA1) approvals were obtained to permit its administration.
Data collection and analysis
The pilot district of Pictou was selected for participation in the project based on criteria established by the Department of Health; these included a large portion of the population living in rural areas, availability of administrative data on the health workforce and willingness to participate among DHA leadership. HCPs working in Pictou DHA were notified of the survey via hard copy invitation, with the exception of paramedics. As paramedics in Nova Scotia are managed provincially, they are not assigned specifically to one DHA; therefore, they were invited through Emergency Health Services, the division of the Nova Scotia Department of Health responsible for pre-hospital emergency health services in the province. The survey was administered online in early 2009. Providers had 2 weeks to complete the survey; after 10 days, providers were sent a reminder by postcard. Data from the competency survey were analysed using SAS software, and analysis was weighted according to respondent profession to adjust for non-response.
Estimates of the proportion of patients requiring each competency were provided by a physician with expertise in infectious disease and validated by the project steering committee. These were estimated separately for each of four care settings—home, primary care, hospital and intensive care. Data on the distribution of patients across these settings during previous influenza pandemics in 1918 and in 1958/68 (GlobalSecurity.org 2009) were used to estimate these proportions for a future pandemic. The size of the district’s population was then multiplied by the distributions of patients across settings to estimate the number of people who would require each of the four levels of care. Within each level of care, the number of patients was multiplied by the proportion requiring each service to estimate the number requiring each service within that setting. The numbers requiring each service within each setting were then summed to estimate the total number of people within the district who would require each service during a future pandemic. For each service, this value was compared against the estimated number of patients who could be provided with that service—estimated by multiplying the number of HCPs by measures of participation, activity, competency and productivity obtained from the questionnaire.
Results
Five hundred and thirty-one health workers in Pictou DHA were invited to complete the competency questionnaire; 185 individuals (35% of those invited) responded to the survey. The percentage of responses to individual questions decreased as the survey went on. The first question, asking the respondents to indicate the DHA in which he or she worked had 174 responses (97% of all respondents). However, while 127 people responded to the first set of competency questions, only 119 responded to the second, 113 to the third and eventually, only 93 to the final set.
Participation and activity rates of HCPs and estimates of the number of patients these providers can care for during some period of time were determined. Respondents to the Pictou ICC survey were asked whether he or she participated in direct patient care (as opposed to, e.g., administration, research or education), how many hours he or she worked in a typical week and how many patients he or she treated or cases he or she managed in a typical week. About 94% of healthcare professionals respondents in this jurisdiction indicated that they were employed in direct patient care, and saw an average of 37 patients/clients a week. The average healthcare professional employed in Pictou County DHA (PCHA) represents about 76% of an FTE.
Data from the PCHA and Department of Health on the number of healthcare professionals working in PCHA, along with data from the competency survey, allowed for the estimation of the number of patients who could be ‘covered’ by each of the ICCs. Data on the population of PCHA, estimates of the attack rate and distribution of patients across care settings, and estimates of the proportion of patients in each setting who would require each competency allowed for the estimation of the number of patients who would require each of the ICCs.2 These two quantities were then compared for each competency to estimate the ‘gap’ in competencies.
The ‘gaps’ in each competency were estimated twice: once based on an estimated attack rate and distribution of patients across care settings (providing the epidemiology component of the framework) similar to the 1958/68 flu pandemics, and then again based on the characteristics of the 1918 flu pandemic (GlobalSecurity.org 2009). In both cases, there were ‘gaps’ in 20–30% of the pandemic influenza competencies; that is, there would be more patients requiring these competencies than the system can presently cover. The 10 competencies with the largest gaps in each case are shown in Table 2, from largest to smallest.
Table 2.
Ten largest influenza competency care gaps in a health authority in NS, using two different patterns of illness severity (1958/68 and 1918 influenza pandemics)
| 1958/68 Pattern | 1918 Pattern |
|---|---|
| Interpret the results of history, physical examination, chest X-ray and (point of care) laboratory tests, leading to a diagnosis | Interpret the results of history, physical examination, chest X-ray and (point of care) laboratory tests, leading to a diagnosis |
| Provide pharmacy services | Provide pharmacy services |
| Prescribe medication | Prescribe medication |
| Triage patients according to acuity of illness and need for care, and referring to appropriate care setting (primary and secondary assessment, hospital, emergency department, non-traditional care site and community) | Provide diagnostic imaging services |
| Measure temperature | Perform clinical laboratory testing service (haematology, chemistry, etc.) |
| Receive and direct patients seeking patient care (manage patient flow within a care site) | Triage patients according to acuity of illness and need for care, and referring to appropriate care setting (primary and secondary assessment, hospital, emergency department, non-traditional care site and community) |
| Assess level of consciousness | Measure temperature |
| Conduct a respiratory assessment (heart rate, respiratory rate, inspection, percussion, palpation and auscultation, etc.) | Receive and direct patients seeking patient care (manage patient flow within a care site) |
| Take blood pressure | Assess level of consciousness |
| Take a screening history of the chief complaint and relevant aspects of the past medical history, current medications, etc. | Conduct a respiratory assessment (heart rate, respiratory rate, inspection, percussion, palpation and auscultation, etc.) |
Discussion
The competencies with the largest gaps are for the most part identical under either pandemic scenario. The differences in the competency gaps between the two pandemic scenarios are largely due to the shift of the distribution of illness towards the acute care setting in the 1918 scenario, as compared with the 1958/68 scenarios, which had a relatively higher proportion of cases in the public/primary care settings.
These ‘gap’ competencies can be broken down into two main categories. The first are competencies that are not uncommon among the survey respondents, but would not be sufficiently available, simply due to the sheer volume of patients who would require them, such as triaging patients, taking temperature, assessing level of consciousness and conducting respiratory assessment. The vast majority of the healthcare professionals surveyed were competent to perform these, but during a major influenza pandemic there would simply be too many patients to manage based on current practice and distribution patterns. The second group of these competencies with large gaps are those that are relatively uncommon among providers but would also be required by a large number of patients. These include competencies such as prescribing medication, providing pharmacy services and interpreting test results and so on leading to a diagnosis. Relatively few of the healthcare professionals surveyed were competent to perform these services. Planners can seek to increase the availability of these competencies by, for example:
Training existing staff in competencies likely to be ‘short’ during a pandemic (i.e. increase the prevalence of these competencies in the health workforce) as appropriate within provincial legal and regulatory frameworks.
Recruiting additional staff who are already trained in these competencies (an alternative means of increasing the prevalence of these competencies and increasing the overall size of the provider stock).
Requesting that existing staff who are already trained in these competencies work in direct care if they are not already doing so, or do so more often (i.e. increase participation and/or activity rates).
Providing supports (human and non-human) to staff trained in these competencies so that they can treat patients more quickly (i.e. increase productivity).
Where regulatory and legal frameworks allow (as determined by the linkage performed through this project), train community volunteers in competencies that are relatively simple—such as taking temperature and blood pressure—but may not be sufficiently available from the existing professional workforce.
Limitations
Several professions were under-represented among the respondents to the competency survey, including physicians, who would play an essential role in meeting the demands of an influenza pandemic. While the analysis was weighted to compensate for non-response, under-representation of certain professions could still lead to underestimation of the availability of certain competencies—perhaps in this case some of those which showed large gaps, such as providing pharmacy services and prescribing medication. In future applications of this approach, efforts to encourage response to the competency assessment questionnaire would be valuable.
Although a substantial number of healthcare professionals (185) responded to the survey, fewer than half of the respondents actually completed the survey, which makes it difficult to be certain about the degree to which the survey responses are representative of all healthcare professionals in Pictou DHA. In current applications of this work, a shortened version of the competency survey is being used to help reduce this limitation.
Analyses did not account for absenteeism among providers, which could be as high as 40% during a pandemic (Nap et al. 2008). Accounting for absenteeism is possible in this analytical framework by reducing the activity rate. However, in this study we have assumed that absenteeism could be offset by surge capacity endeavours that might be initiated by the Health Authority:
Requesting staff to work more hours.
Providing staff with prophylactic antiviral medication, which may reduce absenteeism to only 20% of what would be expected without such protection (Nap et al. 2008).
Redeploying staff from administrative and elective services to do non-technical tasks in more intensive care environments.
Finally, the study relied on individual respondents’ evaluations of their competencies, which is subject to some personal biases. Ideally, objective assessments of the competencies of the health workforce would be used as a measurement tool, but such an undertaking was not feasible in this context.
Conclusion
The objective of this study was to develop and test a competency-based framework for HHR planning. The context of an influenza pandemic in a DHA of Nova Scotia, Canada, was used to demonstrate its application. The test was successful in providing information on the services to be delivered to the District’s population during an influenza pandemic, the availability of the competencies, to perform these services within its existing health workforce and in identifying gaps between these two quantities. This kind of information is highly relevant to healthcare planners tasked with developing, deploying and managing a health workforce that is able to meet the needs of the population it serves, and the outputs of the application of this approach inform the development of specific strategies to address health workforce gaps. Furthermore, the linkage of each competency to relevant legal or regulatory frameworks facilitates the explicit consideration of these in developing policy solutions to address competency gaps—for example, it prevents the assignment of services to professions that are not legally permitted to perform them. The generalizability of the study’s findings is limited given the relatively low response rate, and the under-representation of some key professions; the applicability of the approach, however, nonetheless demonstrates the potential of the competency-based approach to provide valuable insights for planners in highlighting specific gaps in capacity to respond to population health needs so that policies to address these can be considered.
Several of the authors are currently engaged in applying this same methodology using influenza and other conditions in other parts of Canada and internationally. These applications focus on planning for providing health services to seniors receiving home care or long-term care in Nova Scotia and Nunavut, as well as managing the HHR crisis in rural Zambia. In both these applications, the same approach described in this framework is followed. First, the leading health conditions in each jurisdiction are identified; second, the specific services planned to address each condition—and the competencies required to deliver them—are identified; third, the prevalence of each competency is estimated by surveying the respective health workforces in each jursidiction; fourth, this prevalence is used to estimate the number of seniors who can be provided with each service; finally, this last figure is compared with the estimated number of seniors who will require each service (based on data on the size of the population, the distribution of the leading health conditions within that population and the proportion of patients requiring each service). Major service gaps can then serve as a guide to planners in developing policies related to recruitment, curriculum development for pre- and/or post-licensure training, task shifting and/or staff mixes. It is anticipated that, when completed, the lessons learned from these additional applications of the competency-based approach will further increase its value to healthcare planners.
Funding
This study was funded by the Nova Scotia Department of Health.
Endnotes
Footnotes
1 PIA is a comprehensive process, required by Nova Scotia law, for determining the privacy, confidentiality and security risks associated with the collection, use and disclosure of personal information by the province. It also defines the measures used to mitigate and, wherever possible, eliminate the identified risks. The PIA process ensures that measures intended to protect privacy and ensure the confidentiality and security of personal information are considered at the outset of any new programme or service delivery initiative. A PIA also communicates to the public how their privacy is protected and their information kept confidential and secure from unauthorized access.
2 For the purposes of this article, requirements were only estimated for competencies in Domains 3 and 4—Public Health and Care for Influenza Patients—because it was felt that the ‘level of service’ for other Domains was driven more by policy decisions rather than population health needs, and therefore less suitable for planning with a needs-based approach.
References
- Barber P, López-Valcárcel BG. Forecasting the need for medical specialists in Spain: application of a system dynamics model. Human Resources for Health. 2010;8:24. doi: 10.1186/1478-4491-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett T, Namasivayam P, Narudin DAA. A critical review of the nursing shortage in Malaysia. International Nursing Review. 2010;57:32–9. doi: 10.1111/j.1466-7657.2009.00784.x. [DOI] [PubMed] [Google Scholar]
- Birch S, Kephart G, Tomblin Murphy G, et al. Human resources planning and the production of health: a needs-based analytical framework. Canadian Public Policy. 2007;XXXIII(Suppl.):S1–36. [Google Scholar]
- Birch S, Kephart G, Tomblin Murphy G, et al. Health human resources planning and the production of health: development of an extended analytical framework for needs-based health human resources planning. Journal of Public Health Management Practice. 2009;15(Suppl. 6):S56–61. doi: 10.1097/PHH.0b013e3181b1ec0e. [DOI] [PubMed] [Google Scholar]
- Bloor K, Maynard A. Planning Human Resources in Health Care: Towards an Economic Approach. An International Comparative Review. Ottawa: Canadian Health Services Research Foundation; 2003. [Google Scholar]
- Blumenshine P, Reingold A, Egerter S, et al. Pandemic influenza planning in the United States from a health disparities perspective. Emerging Infectious Diseases. 2008;14:709–15. doi: 10.3201/eid1405.071301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell BJ, Kissoon N, Syed N, Fraser HS. Health human resource planning in Barbados and the Eastern Caribbean states a matter of sustainability. West Indian Medicine Journal. 2008;57:542–8. [PubMed] [Google Scholar]
- Centre for Workforce Intelligence. CFWI Medical Factsheets 2011. London: CFWI; 2009. http://www.cfwi.org.uk/intelligence/cfwi-medical-factsheets/cfwi-medical-summary-sheets-2011, accessed 21 December 2011. [Google Scholar]
- Cook L. A Nurse Education and Training Board for New Zealand: Report to the Minister of Health. Wellington: Ministry of Health; 2009. http://www.moh.govt.nz/moh.nsf/pagesmh/9397/$File/nurse-education-training-board-nz-aug09-v2.pdf, accessed 22 December 2010. [Google Scholar]
- Eichner M, Schwehm M, Duerr HP, Brockmann S. The influenza pandemic preparedness planning tool Influsim. Infectious Diseases. 2007;7:17. doi: 10.1186/1471-2334-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GlobalSecurity.org. Flu Pandemic Morbidity/Mortality. 2009. http://www.globalsecurity.org/security/ops/hsc-scen-3_flu-pandemic-deaths.htm, accessed 30 May 2009. [Google Scholar]
- Kass N, Otto J, O’Brien D, Minson M. Ethics and severe pandemic influenza: maintaining essential functions through a fair and considered response. Biosecurity and Bioterrorism: Biodefense Strategy, Practice and Science. 2008;6:227–36. doi: 10.1089/bsp.2008.0020. [DOI] [PubMed] [Google Scholar]
- Lavieri MS, Puterman ML. Optimizing nursing human resource planning in British Columbia. Health Care Management Science. 2009;12:119–28. doi: 10.1007/s10729-008-9097-0. [DOI] [PubMed] [Google Scholar]
- Moghadas SM, Pizzi NJ, Wu J, Yan P. Managing public health crises: the role of models in pandemic preparedness. Influenza and Other Respiratory Viruses. 2009;3:75–79. doi: 10.1111/j.1750-2659.2009.00081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nap R, Andriessen M, Meessen N, et al. Pandemic influenza and excess intensive-care workload. Emerging Infectious Diseases. 2008;14:1518–25. doi: 10.3201/eid1410.080440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien-Pallas L, Tomblin Murphy G, Birch S, Baumann A. A Framework for Collaborative Pan-Canadian Health Human Resources Planning. Ottawa: Health Canada; 2005. A conceptual model for population needs-based, system design-driven HHR planning. In Advisory Committee on Health Delivery and Human Resources (2007) [Google Scholar]
- O’Sullivan T, Dow D, Turner M, et al. Disaster and emergency management: Canadian Nurses’ perceptions of preparedness on hospital front lines. Prehospital and Disaster Medicine. 2008;23(Suppl. 1):S11–8. [PubMed] [Google Scholar]
- Public Health Agency of Canada. The Canadian Pandemic Influenza Plan for the Health Sector. 2006. http://www.phac-aspc.gc.ca/cpip-pclcpi/s02-eng.php, accessed 30 May 2009. [Google Scholar]
- Province of Nova Scotia. Nova Scotia Health System Pandemic Influenza Plan Version 2. Halifax: Province of Nova Scotia; 2007. [Google Scholar]
- Sandrock C. Chapter 4: Manpower. In Sprung et al. (2010). Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Medicine. 2010;36(Suppl. 1):S32–7. doi: 10.1007/s00134-010-1767-y. [DOI] [PubMed] [Google Scholar]
- Spetz J. Forecasts of the Registered Nurse Workforce in California. Sacramento: California Board of Registered Nurses. 2009 Retrieved at http://www.rn.ca.gov/pdfs/forms/forecasts2009.pdf, accessed 29 July 2011. [Google Scholar]
- Stordeur S, Léonard C. Challenges in physician supply planning: the case of Belgium. Human Resources for Health. 2010;8:28. doi: 10.1186/1478-4491-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ten Eyck R. Ability of regional hospitals to meet projected Avian Flu pandemic surge capacity requirements. Prehospital and Disaster Medicine. 2008;23:103–112. doi: 10.1017/s1049023x00005707. [DOI] [PubMed] [Google Scholar]
- Tomblin Murphy G, Vaughan P, Alder R, et al. Health Human Resources Planning for an Influenza Pandemic: A Resource Handbook for Planners. Mississauga: Med-Emerg; 2006. [Google Scholar]
- Torda A. Ethical issues in pandemic planning. Medical Journal of Australia. 2006;185(Suppl.):S73–6. doi: 10.5694/j.1326-5377.2006.tb00713.x. [DOI] [PubMed] [Google Scholar]
- World Health Organizaiton. Pandemic (H1N1) 2009—Update 112. 2010. http://www.who.int/csr/don/2010_08_06/en/index.html, accessed 10 August 2010. [Google Scholar]
- Yun H, Jie S, Jieng A. Nursing shortage in China: state, causes, and strategy. Nursing Outlook. 2010;58:122–8. doi: 10.1016/j.outlook.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


