Abstract
Background
Mental health disorders are becoming more recognized in pregnancy. Whether mental health disorders are associated with health services utilization after child birth is not completely understood.
Objective
This study aimed to investigate postpartum emergency department use within 30 days of delivery among women with preexisting mental health disorders during pregnancy.
Study Design
This was a retrospective cohort study evaluating emergency department use among postpartum women with or without mental health disorders who delivered at an academic center between January 2014 and June 2018. Demographic and outcome data were medical record abstracted and analyzed. Multivariate regression was performed to adjust for covariates.
Results
During the study period, 13,605 women delivered at the institution, 2355 of whom (17.3%) had an underlying mental health disorder. The primary diagnoses of mental health disorder were anxiety (48.8%), depression (34.8%), substance use disorder (11.4%), bipolar disorder (3.4%), psychosis (0.7%), and other (0.8%). There were a total of 565 emergency department visits within 30 days of delivery. Women who presented to the emergency department after delivery were more likely to have public insurance, identify as black or Asian, and have an underlying mental health disorder. Among women with mental health disorders, 155 (6.6%) used the emergency department within 30 days of their delivery compared with 410 (3.6%) of patients without mental health disorder (adjusted odds ratio, 1.74; 95% confidence interval, 1.42–2.13; P<.001). When assessing the risk of emergency department usage per the type of mental health disorder, anxiety (adjusted odds ratio, 1.73; 95% confidence interval, 1.31–2.27) and depression (adjusted odds ratio, 2.13; 95% confidence interval, 1.59–2.86) carried the highest risk. Compared with women without mental health disorders, women with underlying mental health disorders had more presentations for hypertension (15.5% vs 11.2%) and psychiatric evaluations (4.5% vs 0.2%; both P<.001).
Conclusion
Women with mental health disorders use the emergency department during the postpartum period for psychiatric and obstetrical reasons more frequently than women without mental health disorders. Increased surveillance, treatment, and follow-up during pregnancy and the early postpartum period may be warranted for this high-risk population.
Key words: anxiety, depression, emergency department, fourth trimester, maternal, mood disorders, obstetrical, perinatal, pregnancy, psychiatric
AJOG MFM at a Glance.
Why was this study conducted?
This study aimed to evaluate postpartum emergency department (ED) usage among women with mental health disorders.
Key findings
Women with preexisting mental health disorders use the ED during the postpartum period almost twice as frequently as women without mental health disorders.
What does this add to what is known?
Women with underlying mental health disorders are associated with a higher likelihood of using the ED after child birth for psychiatric and obstetrical causes.
Introduction
Approximately 1 in 20 women will use the emergency department (ED) within the first 6 weeks after delivery for unscheduled medical care.1 This prevalence rises to 1 in 12 women within the first 90 days after delivery.2 The predictors of ED usage after delivery include public insurance, age younger than 20 years, severe maternal morbidity at delivery, and cesarean delivery.2 Previous studies have evaluated a published definition of antepartum complications,2 which incorporates mental health disorders (MHDs) as an additional risk factor. However, to date, there is limited evidence whether MHDs specifically are an additional risk factor for postpartum ED use for any indication.
Preexisting MHDs affect up to 15% of pregnant women in the United States3 , 4 and have been demonstrated to contribute substantially to preterm delivery and lower rates of breastfeeding initiation.5 Hospital administrative data have shown an overall increase of postpartum depression by 34% in the past years, especially among women with public insurance and a complicated antepartum course.6 The postpartum period has also been identified as the time of the highest risk for many women in terms of morbidity and mortality. Recent efforts by the American College of Obstetricians and Gynecologists (ACOG) have increased the awareness of the postpartum period or “fourth trimester” of pregnancy7 during which time more than 60% of maternal mortality occurs.8 Furthermore, up to 30% of maternal mortality is due to self-harm,9 most commonly among women with preexisting MHDs. In addition, an ED visit within 30 days of discharge is a frequently used quality metric10 and a focus of this study. Our objective was to investigate whether women with preexisting MHDs have higher all-cause usage of the ED within 30 days of delivery than women without preexisting MHDs.
Methods
This was an institutional review board–approved (number 18-000584) retrospective cohort of women who delivered at an academic quaternary care center from January 2014 to June 2018. We used a hospital database designed for quality improvement to identify all discharges after a delivery greater than 20 weeks’ gestation and to evaluate ED encounters within 30 days of delivery. All women presenting to our institution in the postpartum period were initially evaluated in the main ED and included in this study. If women had multiple deliveries during this period, only the first delivery was included. Available patient demographics, psychiatric comorbidities, delivery data, and ED visit diagnoses were collected. We then identified women who had a diagnostic code for a preexisting MHD during the pregnancy and categorized them into the following: depression, anxiety, bipolar disorder, substance use disorder, psychosis, and other (the sum of personality and eating disorders) (Supplemental Table). If women had multiple MHDs, they were categorized by their primary diagnosis. The primary outcome was an ED encounter within 30 days of delivery, in accordance with the ACOG’s initiative to prioritize this period. Only the first ED encounter was analyzed whether women had multiple visits during the 30 days after delivery. Secondary outcomes included obstetrical outcomes, such as method and gestational age at time of delivery. Data collected included age, race, parity, marital status, insurance payer, body mass index, length of delivery encounter, delivery data, and indications for the ED encounter. Data were analyzed using the Student' t test, Wilcoxon rank-sum test, Fisher exact test, and chi-square test as appropriate. We ran a logistic regression to adjust for covariates using a backward elimination method. All covariates with anticipated association based on literature review or those with observed differences in univariate analysis were initially included. Variables with a P value of >.2 in univariate analysis were eliminated. Crude and adjusted odds ratios (ORs) were reported with their 95% confidence intervals (CIs). Data were analyzed using the Stata software (version 15.1; StataCorp LLC, College Station, TX).
Results
There were 15,115 births between January 2014 and June 2018 to 13,605 women. Only the first delivery for each patient during this period was included in the analysis and second (n=1482) and third (n=28) deliveries were excluded (Figure 1 ). Among all women, 2355 (17.3%) had underlying MHDs. The following are the primary diagnoses listed for those women with MHDs: 48.8% for anxiety (n=1151), 34.8% for depression (n=819), 11.4% for substance use disorder (n=269), 3.4% for bipolar disorder (n=81), 0.7% for psychosis (n=17), and 0.8% for other (n=18). Women with MHDs were more likely to identify as non-Hispanic white (white), non-Hispanic black (black), single, with public insurance, and with a longer hospital length of stay (Table 1 ).
Figure 1.

Participant flowchart
ED, emergency department.
Pluym et al. Emergency department use among postpartum women with mental health disorders. AJOG MFM 2021.
Table 1.
Demographics and obstetrical outcomes of pregnant patients with and without mental health disorders (N=13,605)
| Variables | Patients with mental health disorders (N=2355) | Patients without mental health disorders (N=11,250) | P value |
|---|---|---|---|
| ED visit within 30 d of delivery | 155 (6.6) | 410 (3.6) | <.001a |
| Age, y | 33.3±5.3 | 33.2±5.3 | .013b |
| Race | <.001a | ||
| Asian | 271 (11.5) | 2154 (19.2) | |
| Black | 170 (7.2) | 577 (5.1) | |
| Latinx | 535 (22.7) | 2595 (23.1) | |
| Other | 227 (9.6) | 1302 (11.6) | |
| White | 1152 (48.9) | 4622 (41.1) |
| N=2214 | N=9890 | ||
|---|---|---|---|
| Public insurance | 319 (14.4) | 1212 (12.3) | .006a |
| Marital status | <.001a | ||
| Single | 659 (28.0) | 2418 (21.5) | |
| Married or other | 1696 (72.0) | 8832 (78.5) |
| N=2059 | N=9645 | ||
|---|---|---|---|
| BMI, kg/m2 | 30.0±5.7 | 29.1±5.0 | <.001b |
| NTSV | 1108 (47.1) | 5199 (46.2) | .460a |
| Cesarean delivery | 893 (37.9) | 3481 (30.9) | <.001a |
| Length of stay for delivery encounter (d) | 3.0 (2.4–4.1)c | 2.7 (2.2–3.6)c | <.001d |
| Preterm delivery | 365 (15.5) | 1171 (10.4) | <.001a |
Data are presented as number (percentage) or mean±standard deviation unless otherwise specified.
BMI, body mass index; ED, emergency department; NTSV, nulliparous, term, singleton, vertex.
Pluym et al. Emergency department use among postpartum women with mental health disorders. AJOG MFM 2021.
Chi-square test
Student t test
Median (interquartile range, 25%–75%)
Wilcoxon rank-sum test.
There were a total of 565 (4.2%) ED visits within 30 days of delivery among women that delivered during this period. Women who used the ED after delivery were more likely to have an MHD, identify as black or Asian, have public insurance, carry a nulliparous, term, singleton, vertex pregnancy and have had a cesarean delivery (Table 2 ). Among women with MHDs, 155 of 2355 (6.6%) used the ED within 30 days of delivery compared with 410 of 11,250 patients (3.6%) without MHDs (P<.001). Multivariable logistic regression demonstrated that women with MHDs had greater usage of the ED after adjusting for covariates (adjusted OR [aOR], 1.74; 95% CI, 1.42–2.13) (Table 2). When assessing the risk of ED usage per the type of MHD, anxiety (aOR, 1.73; 95% CI, 1.31–2.27] and depression (aOR, 2.13; 95% CI, 1.59–2.86) carried the highest risk (Table 3 ).
Table 2.
Adjusted ORs of ED visit within 30 days of delivery (N=13,605)
| Variables | Use of ED (n=565) N=508 |
No use of ED (n=13,040) N=11,596 |
Crude OR(95% CI) | Adjusted OR (95% CI)a |
|---|---|---|---|---|
| Public insurance | 111 (21.9) | 1420 (12.3) | 2.00 (1.61–2.49) | 1.99 (1.56–2.54)b |
| Race and ethnicity | ||||
| Asian | 106 (18.8) | 2319 (17.8) | 1.34 (1.04–1.70) | 1.43 (1.11–1.83)b |
| Black | 55 (9.7) | 692 (5.3) | 2.32 (1.70–3.17) | 1.90 (1.35–2.68)b |
| Latinx | 153 (27.1) | 2977 (22.8) | 1.50 (1.21–1.87) | 1.24 (0.97–1.60) |
| Other | 60 (10.6) | 1469 (11.3) | 1.19 (0.88–1.60) | 1.10 (0.81–1.52) |
| White | 191 (33.8) | 5583 (42.8) | Reference | Reference |
| Mental health disorder | 155 (27.4) | 2200 (16.9) | 1.86 (1.54–2.25) | 1.74 (1.42–2.13)b |
| Cesarean delivery | 244 (41.2) | 4130 (31.7) | 1.64 (1.38–1.94) | 1.70 (1.41–2.03)b |
| NTSV | 291 (51.5) | 6016 (46.1) | 1.24 (1.05–1.47) | 1.47 (1.21–1.76)b |
Data are presented as number (percentage) or mean±standard deviation unless otherwise specified.
CI, confidence interval; ED, emergency department; NTSV, nulliparous, term, singleton, vertex; OR, odds ratio.
Pluym et al. Emergency department use among postpartum women with mental health disorders. AJOG MFM 2021.
Adjusted for covariates
Statistically significant.
Table 3.
Adjusted ORs of ED visit by type of mental health disorder
| Variables | ED visit (N=565) | No ED visit (N=13,040) | Crude OR | Adjusted OR (95% CI)a |
|---|---|---|---|---|
| No mental health disorder | 410 (72.5) | 10,840 (83.1) | Reference | Reference |
| Anxiety | 67 (11.9) | 1084 (8.3) | 1.63 (1.25–2.13) | 1.73 (1.31–2.27)b |
| Depression | 60 (10.6) | 759 (5.8) | 2.09 (1.58–2.77) | 2.13 (1.59–2.86)b |
| Other | 28 (5.0) | 357 (2.7) | 2.07 (1.39–3.08) | 1.46 (0.93–2.28) |
Data are presented as number (percentage) or mean±standard deviation unless otherwise specified.
Other indicates substance use, bipolar, psychosis and other disorders.
ED, emergency department; OR, odds ratio.
Pluym et al. Emergency department use among postpartum women with mental health disorders. AJOG MFM 2021.
Adjusted for race and public insurance
Statistically significant.
The most common indications for ED use were hypertension, pain control, and evaluation of an obstetrical wound (Figure 2 ). Compared with women without MHDs, women with underlying MHDs had more presentations for hypertension (15.5% vs 11.2%) and psychiatric evaluations (4.5% vs 0.2%). Women with MHDs were less likely to present to the ED for complaints of an obstetrical wound (14.8% vs 21.0%), breast issue (3.2% vs 9.3%), or gastrointestinal issue (0.6% vs 3.9%). The median postpartum day of presentation to the ED did not differ among women with MHDs (mean, 7.4; interquartile range [IQR], 5.1–12.8) compared with those without MHDs (mean, 8.2; IQR, 5.1–13.6; P=.584) (Figure 3 ).
Figure 2.

Indications for postpartum emergency department visits
Error bars indicate standard error.
Chest, cardiorespiratory; GI, gastrointestinal; GU, genitourinary; HTN, hypertension; Neuro, neurologic; Psych, psychiatric; VB, vaginal bleeding; VTE, venous thromboembolism.
Pluym et al. Emergency department use among postpartum women with mental health disorders. AJOG MFM 2021.
Figure 3.
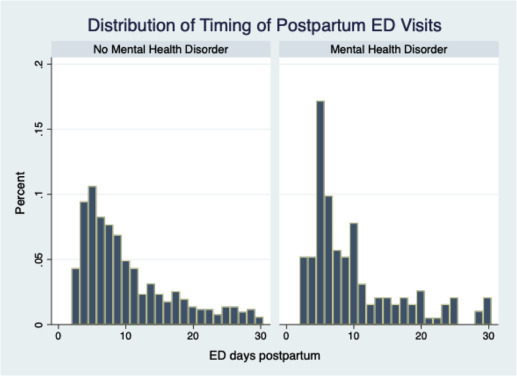
Distribution of timing of postpartum ED visits
ED, emergency department.
Pluym et al. Emergency department use among postpartum women with mental health disorders. AJOG MFM 2021.
Comment
Principal findings
In this study, we set out to determine whether the presence of underlying MHDs affected postpartum use of the ED. Our data indicate that mental health is a considerable risk factor for postpartum ED use by almost 2-fold in women with MHDs compared with those without MHDs.
Results
Women with MHDs use the ED for psychiatric complaints and other obstetrical complications, including hypertension, mostly within the first 2 weeks after delivery. This finding was in the context that all patients with hypertensive disorders at our institution were scheduled for outpatient blood pressure checks around 1 week after delivery. Our data support existing literature that identifies preexisting MHDs as a risk factor for postpartum psychiatric illness.11 , 12 However, there are limited studies evaluating MHDs and the risk of all-cause postpartum use of the ED. A case-control study by Sheen et al13 did not demonstrate previous psychiatric history as a risk factor for postpartum ED usage, although their cohort is notable for a lower rate of psychiatric illness (12%) self-reported or coded in the medical record, possibly limiting the generalizability of their results. Among an exclusive publicly insured population, bipolar disorder has been found to increase the odds of postpartum ED use and hospital admission, but the findings did not hold true to depression or other mental health conditions.14 In our cohort, patients with public health insurance and depression or anxiety were more likely to seek out care in the ED, and the associations held true after adjusting for each other.
Clinical implications
Guidance varies as to the optimal timing of postpartum visits, particularly in women with MHDs. The ACOG suggests that the initial assessment occurs within the first 3 weeks of birth, followed by a comprehensive well-woman visit no later than 12 weeks after delivery,7 a recommendation that most patients find desirable.15 Furthermore, they suggest that additional or earlier postpartum visits are recommended for women who experience complications during pregnancy, including MHDs. In our institution, we subscribe to the common practice of scheduling a follow-up mood check at 1 to 2 weeks after delivery for patients with unstable MHDs. The findings suggest that early follow-up may be indicated in all patients with MHDs, regardless of the degree of the MHD.
The ED is often the first point of contact for mental health concerns in up to 60% of women with MHDs.16 Although their chief complaint may not specifically be a psychiatric issue, it is not uncommon for women to seek the ED for somatic complaints, which may be masking their underlying mental health concerns.17 This remains true for antepartum ED use as well, as population data have demonstrated that ED presentations during pregnancy are associated with hospitalizations for postpartum depression.18 For this reason, we believe that all pregnant and postpartum women who present to the ED warrant a thorough investigation into her signs and symptoms and a screen for depression. Routine screening for depression has been implemented in mothers presenting their infants to a pediatric ED with up to 25% screen-positive rates, highlighting the enormity of the disease.19 , 20 Feasibility of routine depression screening in all adults at a regular ED has been done and similarly demonstrates a 20% screen-positive rate.21
Strengths and limitations
These results highlight an understudied and high-risk population, but the authors acknowledge that further prospective studies are required to determine what interventions are necessary to reduce morbidity and healthcare cost. First, we were limited in our ability to identify the use of non-ED medical resources. There is likely a selection bias of women presenting to the ED toward those that are unable to obtain an outpatient visit secondary to limited access, insurance, or a therapeutic alliance with a provider, all of which can coexist with MHDs. It is difficult to predict whether shortening the time interval to or increasing the frequency of outpatient appointments would decrease ED usage. Secondary to coding limitations, we were unable to identify the risks of concurrent psychiatric illness and substance use disorder on pregnancy, a known risk factor to all-cause mortality in the general population.22 , 23 Importantly, we were also unable to identify antenatal medical comorbidities, including hypertension or diabetes or postpartum complications in the mother or neonate that could exacerbate underlying MHDs. Finally, like any analysis relying on administrative data, we are limited to the accuracy of the coding. Some strengths include the generalizability of these data to other institutions, most importantly determined by the comparable rates of perinatal depression in California (13.0%) vs the national average (12.5%).24 However, in light of the racial associations we encountered with ED usage, it is important to note the higher and lower proportion of Asian and black patients, respectively, in California compared with that of other regions of the United States.25
Conclusions
This study included an evaluation of the risks of MHDs on postpartum use of the ED. We identified that a preexisting MHD is associated with postpartum ED use within 30 days of delivery for several issues, including hypertension and psychiatric complaints. Among postpartum women presenting to the ED, we encourage a thorough evaluation of signs and symptoms and consideration of screening for depression. Capturing this high-risk cohort in the ED can facilitate the connection with mental health resources and optimize long-term mental health. Finally, although the ED is an appropriate venue for certain complaints, we believe that it may represent an inefficient use of resource allocation that could be better handled in the clinical setting. Identifying this high-risk population provides insight into those who require earlier routine outpatient follow-up in an attempt to improve care and decrease visits that may fuel increasing healthcare cost. Future studies include identifying the optimal timing and venue for such follow-up, as the role of telehealth has dramatically increased, especially in patients with preexisting MHDs.26
Footnotes
The authors report no conflict of interest.
Cite this article as: Pluym ID, Holliman K, Afshar Y, et al. Emergency department use among postpartum women with mental health disorders. Am J Obstet Gynecol MFM 2021;3:100269.
Appendix
Supplemental Table.
ICD-9 and ICD-10 diagnosis and procedure codes included in the psychiatric and substance use disorder composites
| Mental health condition | ICD-9 | ICD-10 |
|---|---|---|
| Anxiety | 293.84, 300.0–300.89, 306.4, 306.8, 307.2, 307.59, 307.81, 308.0, 308.3, 308.9, 309.24, 309.28, 309.4 309.81-309.90, V61.9, V62.89 | F06.4, F40.01, F40.10, F40.231, F40.240, F40.243, F40.248, F40.298, F40.8, F40.9, F41.0, F41.1, F41.9, F42.0, F42.2, F42.9, F43.0, F43.1, F43.22, F43.29, F43.8, F43.9, F44.5, F44.9, F45.21, F45.22, F45.41, F45.8, F68.1, F95.0, R46.89 |
| Depression | 296.2–296.99, 300.4, 309, 309.1, 301.12, 309.24, 309.28, 309.29, 309.4, 311 | F32.0–F32.9, F33, F33.1, F33.2, F33.4, F33.41, F33.42, F33.9, F34.1, F41.8, F43.2, F43.21, F43.23, F43.25, F43.29, F45.89 |
| Substance use | 291.9, 292, 292.85, 292.9, 303.03, 303.9, 303.93, 304.0–304.9, 305, 305.01–305.03, 305.1–305.93 | F10.10–F10.99, F11.1–F11.9, F12.1–F12.9, F13.1, F13.282, F14.1–F14.9, F15.2–F15.9, F17.2–F17.29, F18.1, F19.1–F19.9, F55.8 |
| Bipolar | 293.83, 296.01–296.99 | F31.3–F31.9, F34.81, F39 |
| Psychosis | 295.7, 295.9, 297, 297.1, 297.9, 298.9 | F20.9, F22, F23, F25.0, F25.8, F29 |
| Other | 307.1, 307.5–307.59 | F50.0–F50.9, F60.3 |
ICD-9, International Classification of Diseases, Ninth Revision; ICD-10, International Classification of Diseases, Tenth Revision.
Pluym et al. Emergency department use among postpartum women with mental health disorders. AJOG MFM 2021.
References
- 1.Clark S.L., Belfort M.A., Dildy G.A., et al. Emergency department use during the postpartum period: implications for current management of the puerperium. Am J Obstet Gynecol. 2010;203:38.e1–38.e6. doi: 10.1016/j.ajog.2010.02.033. [DOI] [PubMed] [Google Scholar]
- 2.Batra P., Fridman M., Leng M., Gregory K.D. Emergency department care in the postpartum period: California births, 2009-2011. Obstet Gynecol. 2017;130:1073–1081. doi: 10.1097/AOG.0000000000002269. [DOI] [PubMed] [Google Scholar]
- 3.ACOG Committee on Practice Bulletins--Obstetrics ACOG Practice Bulletin: clinical management guidelines for obstetrician-gynecologists number 92, April 2008 (replaces Practice Bulletin number 87, November 2007). Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2008;111:1001–1020. doi: 10.1097/AOG.0b013e31816fd910. [DOI] [PubMed] [Google Scholar]
- 4.Vesga-López O., Blanco C., Keyes K., Olfson M., Grant B.F., Hasin D.S. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65:805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grigoriadis S., VonderPorten E.H., Mamisashvili L., et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74:e321–e341. doi: 10.4088/JCP.12r07968. [DOI] [PubMed] [Google Scholar]
- 6.França U.L., McManus M.L. Frequency, trends, and antecedents of severe maternal depression after three million U.S. births. PLoS One. 2018;13 doi: 10.1371/journal.pone.0192854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKinney J., Keyser L., Clinton S., Pagliano C., ACOG Committee Opinion no 736: optimizing postpartum care. Obstet Gynecol. 2018;132:784–785. doi: 10.1097/AOG.0000000000002849. [DOI] [PubMed] [Google Scholar]
- 8.Creanga A.A., Syverson C., Seed K., Callaghan W.M. Pregnancy-related mortality in the United States, 2011-2013. Obstet Gynecol. 2017;130:366–373. doi: 10.1097/AOG.0000000000002114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Metz T.D., Rovner P., Hoffman M.C., Allshouse A.A., Beckwith K.M., Binswanger I.A. Maternal deaths from suicide and overdose in Colorado, 2004-2012. Obstet Gynecol. 2016;128:1233–1240. doi: 10.1097/AOG.0000000000001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vashi A.A., Fox J.P., Carr B.G., et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309:364–371. doi: 10.1001/jama.2012.216219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harlow B.L., Vitonis A.F., Sparen P., Cnattingius S., Joffe H., Hultman C.M. Incidence of hospitalization for postpartum psychotic and bipolar episodes in women with and without prior prepregnancy or prenatal psychiatric hospitalizations. Arch Gen Psychiatry. 2007;64:42–48. doi: 10.1001/archpsyc.64.1.42. [DOI] [PubMed] [Google Scholar]
- 12.Munk-Olsen T., Laursen T.M., Mendelson T., Pedersen C.B., Mors O., Mortensen P.B. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66:189–195. doi: 10.1001/archgenpsychiatry.2008.528. [DOI] [PubMed] [Google Scholar]
- 13.Sheen J.J., Smith H.A., Tu B., Liu Y., Sutton D., Bernstein P.S. Risk factors for postpartum emergency department visits in an urban population. Matern Child Health J. 2019;23:557–566. doi: 10.1007/s10995-018-2673-0. [DOI] [PubMed] [Google Scholar]
- 14.Ehrenthal D.B., Gelinas K., Paul D.A., et al. Postpartum emergency department visits and inpatient readmissions in a Medicaid population of mothers. J Womens Health (Larchmt) 2017;26:984–991. doi: 10.1089/jwh.2016.6180. [DOI] [PubMed] [Google Scholar]
- 15.Peahl A.F., Novara A., Heisler M., Dalton V.K., Moniz M.H., Smith R.D. Patient preferences for prenatal and postpartum care delivery: a survey of postpartum women. Obstet Gynecol. 2020;135:1038–1046. doi: 10.1097/AOG.0000000000003731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barker L.C., Kurdyak P., Fung K., Matheson F.I., Vigod S. Postpartum psychiatric emergency visits: a nested case-control study. Arch Womens Ment Health. 2016;19:1019–1027. doi: 10.1007/s00737-016-0651-3. [DOI] [PubMed] [Google Scholar]
- 17.Wheaton N., Al-Abdullah A., Haertlein T. Late pregnancy and postpartum emergencies. Emerg Med Clin North Am. 2019;37:277–286. doi: 10.1016/j.emc.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 18.Xu F., Sullivan E.A., Forero R., Homer C.S. The association of emergency department presentations in pregnancy with hospital admissions for postnatal depression (PND): a cohort study based on linked population data. BMC Emerg Med. 2017;17:12. doi: 10.1186/s12873-017-0123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jarvis L.R., Breslin K.A., Badolato G.M., Chamberlain J.M., Goyal M.K. Postpartum depression screening and referral in a pediatric emergency department. Pediatr Emerg Care. 2018 doi: 10.1097/PEC.0000000000001499. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Emerson B.L., Bradley E.R., Riera A., Mayes L., Bechtel K. Postpartum depression screening in the pediatric emergency department. Pediatr Emerg Care. 2014;30:788–792. doi: 10.1097/PEC.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 21.Hoyer D., David E. Screening for depression in emergency department patients. J Emerg Med. 2012;43:786–789. doi: 10.1016/j.jemermed.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 22.Bogdanowicz K.M., Stewart R., Broadbent M., et al. Double trouble: psychiatric comorbidity and opioid addiction-all-cause and cause-specific mortality. Drug Alcohol Depend. 2015;148:85–92. doi: 10.1016/j.drugalcdep.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 23.Arnaudo C.L., Andraka-Christou B., Allgood K. Psychiatric co-morbidities in pregnant women with opioid use disorders: prevalence, impact, and implications for treatment. Curr Addict Rep. 2017;4:1–13. doi: 10.1007/s40429-017-0132-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United Health Foundation America's health rankings analysis of CDC and states PRAMSoe. America’s Health Rankings. 2020. https://www.americashealthrankings.org/explore/health-of-women-and-children/measure/postpartum_depression/state/CA Available at: Accessed May 14, 2020.
- 25.United States Census Bureau QuickFacts: California. 2020. https://www.census.gov/quickfacts/CA Available at:
- 26.Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]


