Recently, a modelling study published in the Lancet Global Health highlighted that the risk of TB associated deaths in LMICs over 5 years could increase by up to 20% most probably due to reductions in timely diagnosis and treatment of new cases.1 Given the concerns highlighted in the abovementioned study and compromised TB control efforts in many high burden countries2 , 3, there is a need to embrace a major transition in National Tuberculosis Programme (NTP), especially in LMICs. Based on the envisaged role of community pharmacist in every facet of the TB care cascade, we would like to suggest the integration of community pharmacies into NTP to facilitate TB control efforts in the midst of COVID-19 as well as prepare healthcare system for any future public health crisis.
The COVID-19 is expected to have significant implications for patients living with TB, undiagnosed TB patients and TB survivors because of clinical reasons and disruption in healthcare services.4 In addition, preventive TB care for family members is expected to be undermined. A South Korean,5 Chinese studies2 reported that detection of new tuberculosis cases declined dramatically within the first 18 weeks of 2020 from the same duration for each year between 2015 and 2019, thereby demanding improved diagnose, control, and prevention of TB by plugging loopholes in the TB care cascade. In this respect, community pharmacists are capable to aid early diagnosis in the event of COVID-19, as existing evidence from many high burden countries also indicated that patients with a prolonged cough (a non-specific TB symptom) often seek initial care at a community pharmacy.6 During pandemic, when people are more inclined towards self-medication with antibiotics, use of broad spectrum antibiotics, such as fluoroquinolones or poor referral practices can contribute to drug resistance and detection delays. Therefore, to avoid such consequences, community pharmacist could perform a Mantoux tuberculin skin test in patients with a cough of duration two weeks or longer, as evidenced by a study.7 In case of positive results, patient can be referred for sputum testing to a nearby designated microscopy centre. Based on the results of the laboratory report, an authorized community pharmacist can either arrange an online session with a pulmonologist for a confirmed active TB patient or refer him to the hospital if needed. According to a study, the rate of TB diagnosis (25 times higher) and patient enrollment (62 times higher) into the TB care cascade significantly increased with community pharmacist referral or intervention.8 Besides, patient with confirmed LTBI report can be successfully treated by authorized community pharmacist. In this regard, a study assessing the viability of administering LTBI treatment in a community pharmacy setting reported that 3HP with directly observed therapy (DOT) (combination weekly therapy with isoniazid and rifapentine (3HP) plus DOT for 12 week) can be successfully delivered and contribute to higher rates of completion of LTBI treatment (75% in community pharmacy setting; 77.5% overall).9
Moreover, treatment disruption for TB patients, and especially multidrug-resistant TB (MDR-TB), is another major challenge in the wake of COVID-19. The second-line drugs for MDR-TB are not widely accessible, and MDR-TB patients are required to return to hospital for evaluation and seek medication every month. Nevertheless, the COVID-19 has not only reduced the capacity of hospitals to deal with patients and deliver effective TB services, but has also lowered patient enthusiasm for these visits due to fear of infection. Under such conditions, authorization of community pharmacists to offer medication for MDR-TB is imperative, as pharmacists have undoubtedly well-established expertise in the dispensing of anti-TB medicines with appropriate counseling. Besides, community pharmacist can also consult or arrange online session with pulmonologist or psychologist if MDR-TB patient is reporting any clinical or psychological problem beyond their understanding and there is need to make amendments in treatment regimen.
Furthermore, adherence and compliance are the most challenging aspect of TB therapy due to the lengthy and complex course of treatment accompanied by possible adverse drug reactions. To this end, counseling with community pharmacist on follow-ups can be of particular importance. A previous research reinforced this by documenting that more than half of the respondents were willing to seek a community pharmacist to help them complete a treatment regimen for MDR-TB.10
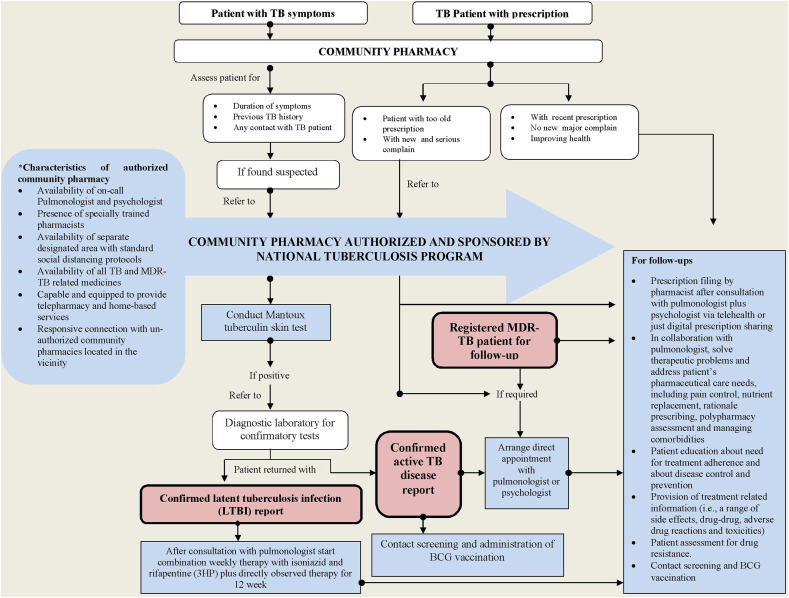
In sum, community pharmacies have tremendous potential to make a positive contribution to every facet of TB care cascade (Fig. 1 ) and ensure the continuity of TB control efforts during COVID-19, its forthcoming waves or any other public health crises. Though, in public-private mix approach – which is an essential component of WHO's End TB Strategy – contribution of community pharmacies has been greatly encouraged owing to their easy access and widespread usage by communities in many high burden nations, but these recommendations have not been extensively put into effect. As a result, interaction of TB patients with community pharmacies remained insignificant, especially in terms of TB screening, testing, and treatment.8 In view of the compromised attempts to monitor TB patients during COVID-19 pandemic, specific community pharmacies need to be associated with national TB programme along with proper reimbursement. The characteristics of the authorized community pharmacy should include availability of on-call pulmonologist and psychologist, presence of specially trained pharmacists, availability of separate designated area with standard social distancing protocols, availability of all TB and MDR-TB related medicines, availability of telepharmacy and home-based services, and responsive connection with un-authorized community pharmacies located in the vicinity. To accomplish this, collaborative efforts by all the stakeholders involved in healthcare policy recommendations as well as its development and enforcement are warranted. The international and national healthcare organizations and pharmacy associations, such as WHO and FIP, should play a key role in helping regulatory bodies recognize that contributions of community pharmacies have potential to permeate in every aspect of TB control efforts. Whereas, regulatory bodies in collaboration with the WHO, STOP TB programme, NTP and national pharmacy associations need to develop well-thought enforcement mechanisms and allocate specific budget on priority basis.
Fig. 1.
A referral model depicting contributions of authorized community pharmacies in TB care cascade.
Ethical approval
Not applicable.
Authors’ contributions
All authors made equal contributions in writing this article.
Funding
None.
Declaration of competing interest
We declare no competing interests.
References
- 1.Hogan A.B., Jewell B.L., Sherrard-Smith E. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. The Lancet Global Health. 2020/09/01/2020;8(9):e1132–e1141. doi: 10.1016/S2214-109X(20)30288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Q., Lu P., Shen Y. Collateral impact of the covid-19 pandemic on tuberculosis control in Jiangsu Province, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dookie N., Padayatchi N., Naidoo K. Tuberculosis elimination in the era of COVID-19: a moving target. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saunders M.J., Evans C.A. COVID-19, tuberculosis, and poverty: preventing a perfect storm. Eur Respir J. 2020 doi: 10.1183/13993003.01348-2020. 2001348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwak N., Hwang S.-S., Yim J.-J. Effect of COVID-19 on tuberculosis notification, South Korea. Emerg Infect Dis. 2020;26(10) doi: 10.3201/eid2610.202782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Surya A., Setyaningsih B., Suryani Nasution H. Quality tuberculosis Care in Indonesia: using patient pathway analysis to optimize public–private collaboration. J Infect Dis. 2017;216(suppl_7):S724–S732. doi: 10.1093/infdis/jix379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitchell E.M., Pérez-Then E., Orejel-Juarez I. Effectiveness of interventions to increase referral of clients exhibiting TB symptoms by pharmacies and corner stores in santo domingo, Dominican Republic. Open Infect Dis J. 2013;7(1) [Google Scholar]
- 8.Daftary A., Satyanarayana S., Jha N. Can community pharmacists improve tuberculosis case finding? A mixed methods intervention study in India. BMJ global health. 2019;4(3) doi: 10.1136/bmjgh-2019-001417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jakeman B., Logothetis S., Roberts M. Addressing latent tuberculosis infection treatment through a collaborative care model with community pharmacies and a health department. Prev Chronic Dis. 2020;17:E14. doi: 10.5888/pcd17.190263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Brien S., Downey J. Patients' Perception of a community pharmacist-managed multidrug-resistant tuberculosis Program in Peru: a public health Perspective. INNOVATIONS in pharmacy. 2017;8(3) 11-11. [Google Scholar]