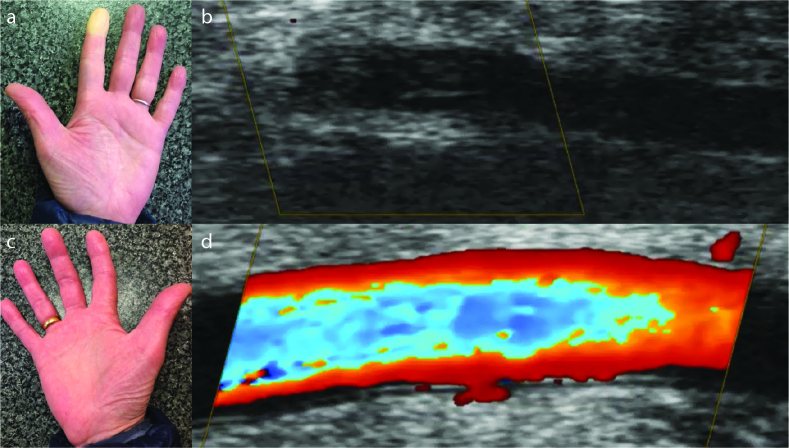
A 60-year-old female with known primary Raynaud’s phenomenon (RP) presented with an episodic unilateral attack of digital pallor change in the left index finger (Figure 1a) associated with paresthesia. Ultra-high-frequency (48 MHz) ultrasound of the affected digit revealed vasospasm of the proper digital arteries (Figure 1b), where color flow imaging shown in the longitudinal view was absent (Figure 1b). Contralaterally, the unaffected respective digit (Figure 1c) had normal color flow (Figure 1d). The attack lasted approximately 15 minutes and self-aborted.
Figure 1. a–d.
Unilateral attack (a) of primary Raynaud’s phenomenon and digital artery vasospasm as assessed by ultra-high-frequency ultrasound (b). The contralateral digit was unaffected (c) and had normal color flow (d).
Primary RP is a common vasospastic condition primarily affecting the digital artery. Typical attacks of the RP affect the extremities, presenting as episodic digital color changes in response to cold and/or emotional stress (1). Secondary RP can occur because of a broad range of medical and drug causes and is often the earliest manifestation seen in patients with systemic sclerosis (SSc) (1). Significant abnormalities (e.g., intimal hyperplasia and occlusion) of the digital arteries have been reported in SSc (2). Irrespective of the underlying cause, RP can have a significant impact on quality of life and function (3).
First-line treatment is patient education and behavioral adaptations (e.g., cold avoidance) (1, 4, 5). Pharmacological therapy (e.g., oral vasodilators) is indicated after the failure of general measures/behavioral adaptions. Calcium channel blockers are often used as the first-line drug treatment; however, clinicians are increasingly using phosphodiesterase type 5 inhibitors earlier for the pharmacological treatment of SSc-associated digital vasculopathy (1, 4, 5).
Patients with RP should seek emergency medical attention if they develop a permanently discolored digit and/or develop signs of tissue ulceration or gangrene.
Footnotes
Informed Consent: Written informed consent was obtained from the patient.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.R., M.H.; Design - S.R., M.H.; Supervision - S.R., M.H.; Materials - S.R.; Data Collection and/or Processing - S.R.; Analysis and/or Interpretation - S.R., M.H.; Literature Search - S.R., M.H.; Writing Manuscript - S.R., M.H.; Critical Review - S.R., M.H.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Pauling JD, Hughes M, Pope JE. Raynaud’s phenomenon - an update on diagnosis, classification and management. Clin Rheumatol. 2019;38:3317–30. doi: 10.1007/s10067-019-04745-5. [DOI] [PubMed] [Google Scholar]
- 2.Allanore Y, Seror R, Chevrot A, Kahan A, Drapé JL. Hand vascular involvement assessed by magnetic resonance angiography in systemic sclerosis. Arthritis Rheum. 2007;56:2747–54. doi: 10.1002/art.22734. [DOI] [PubMed] [Google Scholar]
- 3.Hughes M, Snapir A, Wilkinson J, Snapir D, Wigley FM, Herrick AL. Prediction and impact of attacks of Raynaud’s phenomenon, as judged by patient perception. Rheumatology (Oxford) 2015;54:1443–47. doi: 10.1093/rheumatology/kev002. [DOI] [PubMed] [Google Scholar]
- 4.Hughes M, Ong VH, Anderson ME, Hall F, Moinzadeh P, Griffiths B, et al. Consensus best practice pathway of the UK Scleroderma Study Group: Digital vasculopathy in systemic sclerosis. Rheumatology (Oxford) 2015;54:2015–24. doi: 10.1093/rheumatology/kev201. [DOI] [PubMed] [Google Scholar]
- 5.Denton CP, Hughes M, Nataliya G, Vila J, Buch MH, Chakravarty K, et al. BSR and BHPR guideline for the treatment of systemic sclerosis. Rheumatology (Oxford) 2016;55:1906–10. doi: 10.1093/rheumatology/kew224. [DOI] [PubMed] [Google Scholar]