Abstract
Introduction
Physical inactivity, high screen time, and short sleep are targets of public health initiatives for children. However, few data exist on how many U.S. children meet guidelines for these behaviors—data vital to inform which need greater targeting. This study describes national prevalence estimates of U.S. children who meet physical activity, screen time, and sleep guidelines alone or in combination across each childhood year.
Methods
This analysis (completed in 2019) used cross-sectional data from the 2016–2017 National Survey of Children’s Health, a nationally representative sample of U.S. children. Child physical activity (days/week with ≥60 minutes), recreational screen time (hours/day of TV viewing and electronic device use), and sleep duration (hours/day) were assessed via parental report. Guidelines recommend ≥60 minutes/day of physical activity, ≤2 hours/day of screen time, and 9–12 hours/day of sleep for ages 6–12 years (8–10 hours for ages 13–17 years).
Results
Only 8.8% (95% CI=8.2%, 9.5%) of U.S. children meet all three guidelines combined. Most attain the sleep guideline (86.0%, 95% CI=85.2%, 86.7%), but a lower proportion meet physical activity (23.0%, 95% CI=22.1%, 23.9%) or screen time (32.9%, 95% CI=31.9%, 33.8%) guidelines. A substantial age effect was identified, with prevalence of meeting each distinct guideline, and all three, declining with age (p<0.001).
Conclusion
Few U.S. children meet all three movement guidelines; with prevalence rates of children meeting guidelines declining with age. Although many meet sleep guidelines, few meet physical activity or screen time guidelines. Initiatives targeting physical activity and screen time, particularly for adolescents, should be pursued.
INTRODUCTION
Health during childhood is a strong predictor of health in adulthood: Evidence shows healthy children are more likely to become healthy adults.1–3 Disconcertingly, approximately 27% of U.S. children have a chronic health condition.4 Notably, national rates of obesity, diabetes, and mental health impairment continue to increase among children and adolescents in the U.S.,4–7 imposing significant personal and societal burdens.8,9 In light of the immediate and long-term effects and accompanying comorbidities of these health conditions, there is a great need to optimize programs that address health behaviors in childhood. This is of particular importance given that health behaviors in childhood track into adulthood and considering evidence suggests the health benefits incurred from health behaviors carry forward into adulthood.10–12
Preventive public health initiatives for children and adolescents have focused primarily on lifestyle management, with a specific emphasis on time spent in moderate-to-vigorous physical activity (MVPA) each day. However, MVPA accounts for only a small proportion (~4%) of the 24-hour day. More recently, other behaviors along the movement continuum that comprise the 24-hour day, including time spent in sedentary behavior and time sleeping, have been acknowledged as additional modifiable considerations. Each of these three factors independently contribute to disease risk including obesity, type 2 diabetes, and mental health disorders.13–18 Thus, they have been targets of public health initiatives with parental/caregiver guidelines released on ideal levels of MVPA (≥60 minutes/day),19 sedentary time (in the form of recreational screen time; ≤2 hours/day),20 and sleep (9–12 hours/day for ages 6–12 years; 8–10 hours/day for ages 13–17 years).16
Although benefits are accrued from meeting each individual movement guideline, preventive health initiatives that only focus efforts on a single factor (e.g., MVPA) limit the potential effect on health outcomes.21 Emerging evidence suggests appropriate levels of physical activity (PA), screen time, and sleep need to be achieved simultaneously (e.g. a “healthy 24 hours”) for optimal child health.22 However, integrated 24-hour movement guidelines for children/adolescents do not yet exist in the U.S., and few data exist regarding the extent to which youth meet more than one of the individual recommendations (PA, screen time, or sleep). Failing to look at these factors in unison restricts the ability to understand how habitual movement behaviors interact to influence health outcomes. Such information is vital for informing public health programs and identifying which preventive measures are in most need of targeting. Initial evidence among a representative sample of U.S. high school–aged youth suggests that few (~5%) meet guidelines for PA, screen time, and sleep simultaneously.23 However, it is unclear if similar rates exist across all school-aged children in the U.S.
The purpose of this study is to calculate national prevalence estimates of U.S. children and adolescents who meet PA, recreational screen time, and sleep guidelines alone or in combination. Furthermore, little evidence exists on prevalence of meeting these guidelines as children age, thus limiting the possibility of designing age-tailored programs to promote adoption of these preventive health measures during childhood or discerning which health behaviors are in most need of targeting across age groups; therefore, comprehensive trend analyses across each year of childhood from age 6 to 17 years are also conducted.
METHODS
Study Population
This analysis used data from the 2016 and 2017 National Survey of Children’s Health (NSCH), a nationally representative survey of U.S. children aged 0–17 years since 2003.24 Sample design and data collection procedures have been described previously25 and are available online.24 Households from all 50 states were randomly selected and mailed a screener questionnaire querying information pertaining to children in the household. Those with children aged <18 years were then invited to complete a comprehensive topical questionnaire about this child online or via mail.
Across the 2016 and 2017 surveys, 71,811 of 199,058 (36.1%) households completed the topical questionnaire. The present analysis was restricted to children aged 6–17 years (n=51,156) as data on PA were not collected on children aged <6 years. After excluding those who had missing data for PA, screen time, or sleep (n=1,550), a total of 49,606 participants were included in the final analytic sample. The NSCH adhered to the U.S. Federal Policy for protection of human subjects and all participants provided informed consent.
Measures
Children’s PA was assessed by parental response to the question: During the past week, on how many days did this child exercise, play a sport, or participate in physical activity for at least 60 minutes? Response options were: 0 days, 1–3 days, 4–6 days, or every day. Children were classified as meeting PA guidelines if their parent chose the response option of every day.19
Recreational screen time was calculated from two questions that queried TV viewing and electronic device use. Time spent in these screen-based activities was assessed by the questions: On an average weekday, about how much time does this child usually spend in front of a TV watching TV programs, videos, or playing video games? and On an average weekday, about how much time does this child usually spend with computers, cell phones, handheld video games, and other electronic devices doing things other than schoolwork? Response options were: none, less than 1 hour, 1 hour, 2 hours, 3 hours, or 4 or more hours. TV viewing and electronic device use responses were summed to derive hours/day of screen time (with the less the 1 hour response option set to the midpoint of 0.5 hours). Children with ≤2 hours/day of recreational screen in total were classified as meeting screen time guidelines.15,20
Sleep was assessed by parental response to the question: During the past week, how many hours of sleep did this child get on most weeknights? Response options were: less than 6 hours, 7 hours, 8 hours, 9 hours, 10 hours, and 11 or more hours. Children were classified as meeting sleep guidelines if their parent chose a response option that agreed with the recommended 9–11 hours for ages 6–13 years, or 8–10 hours for ages 14–17 years.16
Sociodemographic and lifestyle characteristics derived from the NSCH topical questionnaire included age, sex, race, Hispanic ethnicity, household poverty level, and BMI. A detailed summary of sociodemographic/lifestyle measures is provided in the online supplement.
Statistical Analysis
To produce nationally representative estimates, survey analysis procedures were used to account for sample weights, stratification, and clustering of the complex survey design. The prevalences and 95% CIs of meeting zero, one, two, or all three of the movement guidelines were estimated overall among all U.S. children/adolescents and stratified by sociodemographic characteristics including age group (children [aged 6–11 years] and adolescents [aged 12–17 years]), sex, race, Hispanic ethnicity, household poverty level, and BMI category. The prevalences of meeting each guideline, individually, and in different combinations (e.g. meeting PA and screen time, but not sleep guidelines) were also estimated.
Logistic regression modeling was used to assess the association of sociodemographic and lifestyle characteristics with meeting each movement guideline and all three simultaneously. Models were adjusted for age, sex, race, Hispanic ethnicity, and household poverty level. The authors did not adjust for BMI in the primary models because BMI classification in the NSCH was limited to children aged 10–17 years. As a secondary analysis, the association of BMI category with meeting each movement guidelines and all three simultaneously was also examined with adjustment for the above listed covariates. To examine the degree to which each characteristic was predictive of meeting movement guidelines, the difference in variance (ΔR2) between the full model and the model when omitting each specific characteristic (i.e., each variable uniquely accounts for a proportion of the variance accounted for by all the variables combined) was calculated and expressed as the percentage of a model’s R2 value.
To evaluate trends in meeting movement guidelines with increasing age, the prevalence and 95% CI of meeting guidelines in each year of childhood from age 6 to 17 years were estimated. Linear trends (i.e., p-trend) in prevalence estimates across age groups were evaluated using generalized additive models with adjustments for sex, race, Hispanic ethnicity, and household poverty level. To inform which specific screen time habits differ by age, a secondary analysis was conducted examining age trends for prevalence of TV viewing ≤2 hours/day and electronic device use ≤2 hours/day, separately. Analyses were conducted in 2019 using SAS, version 9.4.
RESULTS
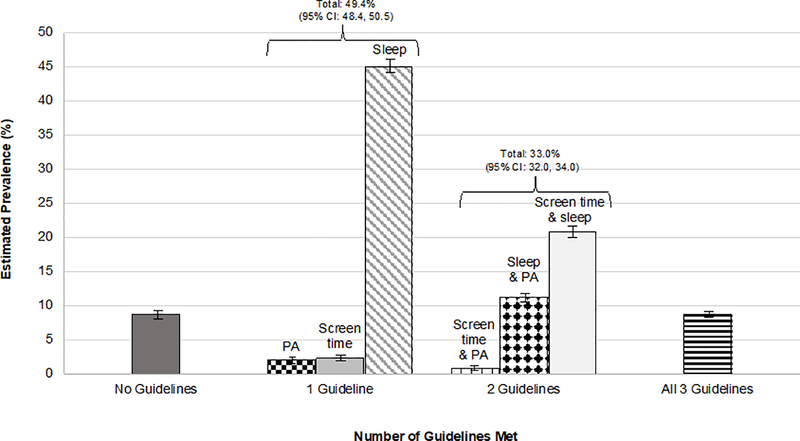
Table 1 shows the estimated prevalence of those meeting each specific guideline and meeting all three, stratified by demographic characteristics. Overall, only 8.8% (95% CI=8.2%, 9.5%) of children/adolescents met all three guidelines; however, a majority (91.2%) met at least one with 49.4% (95% CI=48.4%, 50.5%) and 33.0% (95% CI=32.0%, 34.0%) meeting one and two guidelines, respectively (Figure 1; Appendix Table 1). Most children/adolescents (86.0%, 95% CI=85.2%, 86.7%) met sleep guidelines, but only 32.9% (95% CI=31.9%, 33.8%) met screen time and 23.0% (95% CI=22.1%, 23.9%) met PA guidelines. Across age groups, children had the highest estimated prevalence of achieving all three guidelines (12.9%, 95% CI=11.8%, 14.0% vs 4.7%, 95% CI=4.1%, 5.4% for adolescents). A higher estimated percentage of children than adolescents also met each of the discrete guidelines for PA (27.8%, 95% CI=26.4, 29.3% vs 18.2%, 95% CI=17.0%, 19.4%), screen time (44.8%, 95% CI=43.2%, 46.3% vs 20.9%, 95% CI=19.8%, 22.1%), and sleep (88.7%, 95% CI=87.8%, 89.7% vs 83.2%, 95% CI=82.1%, 84.3%). Appendix Table 2 shows the estimated prevalence of children/adolescents meeting the various combinations of guidelines (e.g. screen time plus sleep).
Table 1.
Estimated Prevalence of U.S. Children/Adolescents Meeting Movement Guidelines (Physical Activity/Screen Time/Sleep)
| Characteristic | Unweighted sample size, n | Guidelines met |
||||
|---|---|---|---|---|---|---|
| None, weighted % (95% CI) | Physical activity (PA),a weighted % (95% CI) | Screen time,b weighted % (95% CI) | Sleep,c weighted % (95% CI) | PA + screen time + sleep, weighted % (95% CI) | ||
| Overall | 49,606 | 8.8 (8.2, 9.4) | 23.0 (22.1, 23.9) | 32.9 (31.9, 33.8) | 86.0 (85.2, 86.7) | 8.8 (8.2, 9.5) |
| Sex | ||||||
| Female | 24,242 | 9.7 (8.8, 10.6) | 19.4 (18.1, 20.6) | 33.6 (32.1, 35.0) | 85.4 (84.3, 86.5) | 7.8 (6.9, 8.9) |
| Male | 25,364 | 7.9 (7.2, 8.7) | 26.5 (25.2, 27.8) | 32.2 (30.9, 33.5) | 86.6 (85.6, 87.6) | 9.7 (9.0, 10.6) |
| Age groups | ||||||
| Children (aged 6–11 years) | 20,919 | 5.3 (4.6, 6.2) | 27.8 (26.4, 29.3) | 44.8 (43.2, 46.3) | 88.7 (87.8, 89.7) | 12.9 (11.8, 14.0) |
| Adolescents (aged 12–17 years) | 28,687 | 12.2 (11.3, 13.1) | 18.2 (17.0, 19.4) | 20.9 (19.8, 22.1) | 83.2 (82.1, 84.3) | 4.7 (4.1, 5.4) |
| Race/ethnicity | ||||||
| White | 38,444 | 7.2 (6.6, 7.8) | 23.2 (22.2, 24.3) | 36.0 (34.8, 37.2) | 88.1 (87.4, 88.9) | 10.1 (9.3, 10.9) |
| Black | 3,219 | 16.5 (14.1, 19.0) | 24.8 (22.1, 27.4) | 20.6 (18.3, 23.0) | 75.9 (73.1, 78.7) | 4.8 (3.7, 6.2) |
| Asian | 2,699 | 6.2 (4.8, 8.0) | 16.4 (13.0, 19.7) | 38.1 (34.2, 42.0) | 88.0 (85.3, 90.1) | 6.1 (4.5, 8.1) |
| Otherd | 5,244 | 9.1 (7.6, 10.8) | 22.3 (19.4, 25.3) | 28.7 (25.8, 31.5) | 85.4 (83.4, 90.8) | 7.5 (6.0, 9.4) |
| Ethnicity | ||||||
| Not Hispanic | 44,115 | 8.5 (8.0, 9.2) | 23.7 (22.8, 24.5) | 34.5 (33.6, 35.5) | 86.0 (85.3, 86.8) | 9.2 (8.7, 9.8) |
| Hispanic | 5,491 | 9.4 (7.9, 11.0) | 21.1 (18.5, 23.7) | 27.9 (25.1, 30.7) | 85.8 (83.8, 87.7) | 7.6 (6.0, 9.7) |
| Family poverty-to-income ratio level, % | ||||||
| <200 | 12,669 | 11.0 (9.8, 12.2) | 26.3 (24.6, 28.1) | 27.7 (25.9, 29.5) | 82.9 (81.5, 84.3) | 8.7 (7.5, 10.0) |
| 200–299 | 8,131 | 7.4 (6.4, 8.5) | 22.7 (20.6, 24.8) | 32.4 (30.1, 34.6) | 88.0 (86.7, 89.4) | 8.7 (7.4, 10.1) |
| 300–399 | 7,675 | 7.7 (6.6, 9.0) | 19.0 (16.9, 21.0) | 34.8 (32.3, 37.2) | 87.4 (85.5, 89.3) | 7.4 (6.4, 8.6) |
| ≥400 | 21,131 | 6.6 (6.0, 7.3) | 20.1 (19.0, 21.2) | 39.9 (38.5, 41.2) | 88.7 (87.8, 89.6) | 9.7 (8.8, 10.6) |
| p-trend | <0.001 | <0.001 | <0.001 | <0.001 | 0.476 | |
| BMIe | ||||||
| Under weight (BMI <5th percentile) | 2,124 | 9.0 (6.5, 12.3) | 17.5 (14.3, 20.8) | 30.3 (26.1, 34.5) | 86.2 (82.6, 89.8) | 4.0 (3.0, 5.4) |
| Normal weight (5th–85th percentile) | 22,903 | 8.8 (8.1, 9.6) | 21.4 (20.0, 22.7) | 27.4 (26.0, 28.7) | 86.6 (85.6, 87.6) | 6.7 (6.0, 7.6) |
| Overweight (BMI 85th–94th percentile) | 4,888 | 12.6 (10.5, 14.7) | 16.5 (13.8, 19.2) | 21.0 (18.4, 23.6) | 82.8 (80.1, 85.6) | 4.6 (3.2, 6.5) |
| Obese (BMI ≥95th percentile) | 4,386 | 16.1 (13.3, 19.0) | 14.5 (11.7, 17.2) | 17.7 (14.9, 20.5) | 79.1 (76.0, 82.2) | 4.3 (3.0, 6.2) |
Notes: Boldface indicates statistical significance (p<0.001). All estimates were weighted to be nationally representative.
Physical activity ≥60 minutes every day.
Screen time ≤2 hours each day.
Sleep duration per night between 9 and 11 hours (aged 6–13 years), or between 8 and 10 hours (aged 14–17 years).
Other race category includes American Indian or Alaska Native (unweighted n=369), Native Hawaiian and other Pacific Islander (unweighted n=162), some other race (unweighted n=1,261), and two or more races (unweighted n=3,452).
BMI data only available for those aged 10–17 years.
Figure 1.
Estimated prevalence of meeting zero, one, two, or three of the movement guidelines (physical activity, screen time, or sleep) in the 2016–2017 National Survey of Children’s Health. Data are weighted to be nationally representative. Error bars indicate 95% CI.
PA, physical activity.
Being female (versus male); an adolescent (versus child); black, Asian, or other race (versus white race); and underweight, overweight, or obese (versus normal weight) were all significantly associated with a lower likelihood of meeting all three guidelines (Table 2). When examining each specific guideline, adolescents and those with BMI classifications of overweight and obese were notably less likely to meet PA, screen time, and sleep guidelines. No consistent pattern of differences emerged for all other demographic subgroups. Appendix Table 3 shows the ORs for meeting each of the possible combinations of guidelines.
Table 2.
Adjusted Relative Odds of U.S. Children/Adolescents Meeting Movement Guidelines (Physical Activity/Screen Time/Sleep)
| Guidelines met |
||||
|---|---|---|---|---|
| Characteristic | Physical activity (PA),a OR (95% CI) | Screen time,b OR (95% CI) | Sleep,c OR (95% CI) | PA + screen time + sleep, OR (95% CI) |
| Sex | ||||
| Female | 0.66 (0.59, 0.74) | 1.01 (0.98, 1.18) | 0.90 (0.80, 1.02) | 0.63 (0.50, 0.80) |
| Male | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (Ref) |
| ΔR2 | 25.2% | 0.3% | 1.3% | 3.8% |
| Age groups | ||||
| Children (aged 6–11 years) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Adolescents (aged 12–17 years) | 0.58 (0.52, 0.64) | 0.31 (0.29, 0.35) | 0.63 (0.56, 0.71) | 0.44 (0.35, 0.56) |
| ΔR2 | 44.1% | 71.9% | 26.9% | 71.0% |
| Race | ||||
| White | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Black | 0.95 (0.82, 1.11) | 0.49 (0.42, 0.57) | 0.46 (0.39, 0.55) | 0.47 (0.30, 0.71) |
| Asian | 0.62 (0.48, 0.80) | 1.06 (0.90, 1.26) | 1.00 (0.76, 1.32) | 0.59 (0.35, 0.99) |
| Otherd | 0.97 (0.80, 1.17) | 0.80 (0.68, 0.95) | 0.84 (0.69, 1.02) | 0.61 (0.38, 0.98) |
| ΔR2 | 4.9% | 11.2% | 42.7% | 18.8% |
| Ethnicity | ||||
| Not Hispanic | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Hispanic | 0.75 (0.63, 0.88) | 0.73 (0.63, 0.86) | 0.95 (0.79, 1.14) | 0.88 (0.61, 1.29) |
| ΔR2 | 7.7% | 3.0% | 0.0% | 4.1% |
| Family poverty-to-income ratio level, % | ||||
| <200 | 1.50 (1.34, 1.69) | 0.64 (0.57, 0.71) | 0.70 (0.61, 0.80) | 1.24 (0.94, 1.64) |
| 200–299 | 1.19 (1.03, 1.37) | 0.75 (0.66, 0.84) | 0.99 (0.85, 1.16) | 0.88 (0.65, 1.19) |
| 300–399 | 0.93 (0.79, 1.08) | 0.82 (0.73, 0.92) | 0.90 (0.74, 1.16) | 0.70 (0.54, 0.92) |
| ≥400 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| p-trend | <0.001 | <0.001 | <0.001 | 0.107 |
| ΔR2 | 21.0% | 6.9% | 13.2% | 2.4% |
| BMIe | ||||
| Underweight (BMI <5th percentile) | 0.69 (0.54, 0.88) | 1.00 (0.81, 1.25) | 0.89 (0.65, 1.21) | 0.49 (0.35, 0.68) |
| Normal weight (5th–85th percentile) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Overweight (BMI 85th–94th percentile) | 0.69 (0.55, 0.85) | 0.71 (0.60, 0.85) | 0.79 (0.63, 0.98) | 0.65 (0.44, 0.94) |
| Obese (BMI ≥95th percentile) | 0.52 (0.41, 0.66) | 0.60 (0.48, 0.73) | 0.64 (0.52, 0.78) | 0.57 (0.38, 0.86) |
| ΔR2 | 25.8% | 16.5% | 12.5% | 19.4% |
Notes: All estimates were weighted to be nationally representative. Boldface indicates statistical significance (p<0.001). All models adjusted for sex, age, race, ethnicity, and family poverty to income level. ΔR2 denotes the unique variance accounted for by each variable (i.e., the difference in variance between the full model and the model when omitting each specific characteristic). It reflects the percent of the percent of variance explained (e.g., percent of a model’s R2) by each variable.
Defined as physical activity ≥60 minutes every day.
Defined as screen time ≤2 hours each day.
Defined as sleep duration per night between 9 and 11 hours (ages 6–13 years), or between 8 and 10 hours (ages 14–17 years).
Other race category includes American Indian or Alaska Native (unweighted n=369), Native Hawaiian and other Pacific Islander (unweighted n=162), some other race (unweighted n=1,261), and two or more races (unweighted n=3,452).
BMI data only available for those aged 10–17 years.
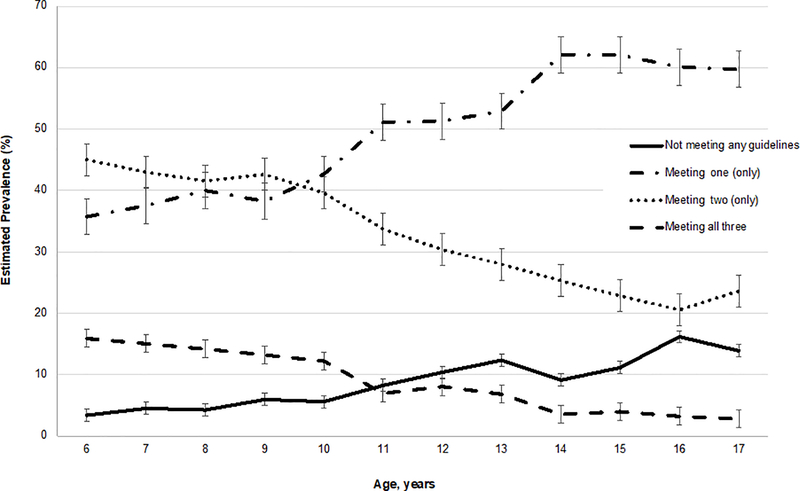
The estimated prevalence of meeting two or three guidelines significantly decreased with increasing age, whereas the estimated prevalence of meeting zero or only one guideline significantly increased with increasing age (p<0.001) (Figure 2 and Appendix Table 4). From age 6 to 17 years, the estimated prevalence of meeting all three guidelines decreased from 15.9% (95% CI=12.5%, 19.2%) to 2.8% (95% CI=2.1%, 3.7%).
Figure 2.
Estimated prevalence of children and adolescents meeting zero, one, two, or three of the movement guidelines by age in the 2016–2017 National Survey of Children’s Health. Data are weighted to be nationally representative. Error bars indicate 95% CI.
The estimated prevalence of meeting each of the PA, screen time, and sleep guidelines, separately, significantly decreased with increasing age (p<0.001) (Appendix Figure 1 and Appendix Table 5). From age 6 to 17 years, the estimated prevalence of meeting PA, screen time, and sleep guidelines declined 15.5%, 33.8%, and 8.8%, respectively. The largest year-to-year declines occurred from age 10 to 11 years for PA (decline of 5.4%) and screen time (decline of 11.0%) guidelines. For sleep, the largest year-to-year decline occurred from age 15 to 16 years (decline of 8.0%). When TV viewing and electronic device use were evaluated separately, the prevalence of children/adolescents watching TV ≤2 hours/day declined 10.2% from age 6 to 17 years, while the prevalence of electronic device use ≤2 hours/day declined 50.5% (p<0.001) (Appendix Table 6).
DISCUSSION
In this nationally representative survey, it was estimated that fewer than one in ten (~9%) U.S. children/adolescents meet all three movement guidelines (PA, screen time, and sleep), although most meet at least one (~91%). A high proportion achieve the recommended amount of sleep (86%), but a much lower percentage meet guidelines for PA (23%) and screen time (33%). A substantial age effect was also identified as the estimated prevalence of meeting each and all three movement guidelines decreased with age. Notably, from age 6 to 17 years, the estimated prevalence of children meeting all three guidelines decreased approximately 13%, with almost none (~2%) meeting all three by age 17 years.
Historically, preventive health interventions targeting movement behaviors in children have focused on each aspect of the movement continuum in isolation.26–29 Emerging evidence, however, shows these movement behaviors interact such that their combined effects (i.e., meeting all three guidelines) on health indicators are greater than their individual effects. For example, in a sample of >6,000 children from 12 countries, meeting all three movement behavior recommendations was associated with a 72% lower likelihood of obesity versus a 55%, 14%, and 33% lower likelihood of obesity when individually meeting PA, sedentary time, and sleep time guidelines, respectively.30 Similar findings have been reported for other health indicators of cardiometabolic risk and cognition.30–32 This growing body of research has informed a paradigm shift toward an integrated model that incorporates all 24-hour movement behaviors to optimize health benefits rather than focusing on a single specific behavior.32 Notably 24-hour movement guidelines for children/adolescents have been released in Canada and Australia that recommend optimization of PA, sedentary behavior, and sleep simultaneously.33,34 As such guidelines continue to develop, there is a need to identify how specific countries meet such recommendations and identify where deficits lie with respect to meeting each of the movement guidelines. The present study reports that only around 9% of U.S. children/adolescents meet all three movement guidelines. Similar findings (~2%–5% meeting all three guidelines) have been reported in non-representative U.S. samples.30,32 This is lower than the 17.5% of Canadian and 14.9% of Australian youth meeting all three guidelines in previous studies.22,30 With rising rates of chronic diseases in children and young adults in the U.S., these findings highlight a sizeable public health problem that, if targeted, may help to mitigate rising chronic disease rates. Notably, these findings suggest efforts targeting reductions in recreational screen time and increases in PA are most needed to optimize movement behaviors among U.S. youth.
A key finding of this study is the observed decreases from childhood to adolescence in those achieving each movement guideline and all three in combination. Prior results from the Youth Risk Behavior Surveillance Survey showed only 5% of U.S. adolescents met all movement recommendations.23 This study extends upon this work by reporting prevalence estimates among children (13% meeting all three guidelines) versus adolescents (5% meeting all three) and evaluating age trends across childhood. From age 6 to 17 years, prevalence of meeting all three and each specific guideline declined, with <3% of 17-year-olds meeting all three, and <20% meeting PA and screen time guidelines, respectively. Such findings are alarming given the substantive literature showing that movement behaviors in adolescence are predictive of movement behaviors in adulthood.35–37 Notably, the largest decline among movements behaviors was observed for screen time, with more than half (52%) of 6-year-olds meeting recommendations versus 18% of 17-year-olds. When assessing screen time by its component parts (TV viewing and electronic device use), the proportion of children with ≤2 hours/day of electronic device declined 50% from age 6 to 17 years whereas TV viewing ≤2 hours/day declined only approximately 10%. Thus, the decline in children meeting screen time guidelines was largely driven by increased electronic device use. Although contributing factors to the declines in children/adolescents who used electronic devices ≤2 hours/day are unclear, market research shows the average age for getting a first phone is 10.3 years, with 95% of U.S. teens reporting phone access in 2018.38 Thus, increased access to smartphones and other electronic devices, which are typically restricted in younger children, may be a contributing factor. Consistent with market research, the authors observed the largest declines in meeting PA and screen time guidelines from age 10 to 11 years, suggestive that efforts targeting increases in PA/reductions in sedentary behavior may be warranted during early adolescence when electronic device access may be increasing.
Limitations
This study has several limitations. First, the NSCH comprises a survey sample and is therefore subject to non-response bias. Response rates in the NSCH tend to be lower in urban areas and among low-income and ethnic minority populations.39 However, non-response adjustment to the survey weights in the NSCH reduces the potential magnitude of these biases. Second, the NSCH is cross-sectional in nature. Third, all NSCH data, including movement behaviors, were parent-reported and may be subject to recall and response bias, as well as measurement error.40 For example, parents may misjudge PA intensity and be unable to accurately quantify PA during times away from home (e.g. school), thus leading to a possible underestimation or overestimation of the true prevalence of meeting MVPA guidelines.41 Fourth, relative to PA, which was assessed over a typical week (including weekends), screen time and sleep were assessed only on weekdays. Thus, the difference in measurement precision for assessing PA and sleep/screen time may have affected the findings. For example, it is unclear if average daily sleep is represented accurately, considering weekday versus weekend sleep variability and the possibility of sleep compensation on weekends. Finally, the NSCH survey questions assessing screen time did not ascertain active video gaming or device use while moving (e.g. texting while walking). Thus, some PA may be misclassified as screen time.42 Future studies should include objective measures of movement across the 24-hour period, including weekend days to present a more accurate reflection of children’s behaviors.
CONCLUSIONS
In a large national survey of children in the U.S., prevalence estimates suggest that fewer than one in ten meet all three movement guidelines. Low compliance to PA and screen time guidelines were the primary contributing factors, as most U.S. children met sleep guidelines. Thus, public health initiatives targeting replacing screen time with PA during leisure time may be warranted. Importantly, it was observed that the proportion of U.S. children meeting all three guidelines substantially decreased with age, with <3% of 17-year-olds meeting all three. As such, these data indicate that most U.S. adolescents are transitioning into adulthood with poor movement behaviors across the 24-hour period that will likely predispose them to heightened cardiometabolic risk at an early age. These findings highlight a pressing need to develop health promotion programs for children and adolescents that address a healthy 24 hours, targeting PA, recreational screen time, and sleep concurrently, to curtail the rising chronic disease burden in the U.S.
Supplementary Material
ACKNOWLEDGMENTS
No financial disclosures have been reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Merikangas KR. Time trends in the global prevalence of mental disorders in children and adolescents: gap in data on U.S. youth. J Am Acad Child Adolesc Psychiatry. 2018;57(5):306–307. 10.1016/j.jaac.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91(5):1499S–1505S. 10.3945/ajcn.2010.28701b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gordon-Larsen P, Nelson MC, Popkin BM. Longitudinal physical activity and sedentary behavior trends: adolescence to adulthood. Am J Prev Med. 2004;27(4):277–283. 10.1016/j.amepre.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623–630. 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015(219):1–8. [PubMed] [Google Scholar]
- 6.Mayer-Davis EJ, Lawrence JM, Dabelea D, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med. 2017;376(15):1419–1429. 10.1056/nejmoa1610187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34–46.e2. 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finkelstein EA, Graham WC, Malhotra R. Lifetime direct medical costs of childhood obesity. Pediatrics. 2014;133(5):854–862. 10.1542/peds.2014-0063. [DOI] [PubMed] [Google Scholar]
- 9.Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14(4):435 10.3390/ijerph14040435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandes RA, Zanesco A. Early physical activity promotes lower prevalence of chronic diseases in adulthood. Hypertens Res. 2010;33(9):926–931. 10.1038/hr.2010.106. [DOI] [PubMed] [Google Scholar]
- 11.Mantovani AM, De Lima MCS, Gobbo LA, et al. Adults engaged in sports in early life have higher bone mass than their inactive peers. J Phys Act Health. 2018;15(7):516–522. 10.1123/jpah.2017-0366. [DOI] [PubMed] [Google Scholar]
- 12.Pälve KS, Pahkala K, Magnussen CG, et al. Association of physical activity in childhood and early adulthood with carotid artery elasticity 21 years later: the cardiovascular risk in Young Finns Study. J Am Heart Assoc. 2014;3(2):e000594 10.1161/jaha.113.000594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. 2019;9(1):e023191 10.1136/bmjopen-2018-023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garber CE, Blissmer B, Deschenes MR, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. 10.1249/mss.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 15.Tremblay MS, Carson V, Chaput JP, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S311–S327. 10.1139/apnm-2016-0203. [DOI] [PubMed] [Google Scholar]
- 16.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. 10.5664/jcsm.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reinehr T Type 2 diabetes mellitus in children and adolescents. World J Diabetes. 2013;4(6):270–281. 10.4239/wjd.v4.i6.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu X, Haegele JA, Healy S. Movement and mental health: behavioral correlates of anxiety and depression among children of 6–17 years old in the U.S. Ment Health Phys Act. 2019;16:60–65. 10.1016/j.mhpa.2019.04.002. [DOI] [Google Scholar]
- 19.Piercy KL, Troiano RP, Ballard RM, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020–2028. 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Council on Communications and Media. Children, adolescents, and the media. Pediatrics. 2013;132(5):958–961. 10.1542/peds.2013-2656. [DOI] [PubMed] [Google Scholar]
- 21.Chaput JP, Carson V, Gray CE, Tremblay MS. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health. 2014;11(12):12575–12581. 10.3390/ijerph111212575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberts KC, Yao X, Carson V, Chaput JP, Janssen I, Tremblay MS. Meeting the Canadian 24-hour movement guidelines for children and youth. Health Rep. 2017;28(10):3–7. 10.1016/j.ypmed.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 23.Knell G, Durand CP, Kohl HW III, Wu IHC, Pettee Gabriel K. Prevalence and likelihood of meeting sleep, physical activity, and screen-time guidelines among U.S. youth. JAMA Pediatr. 2019;173(4):387–389. 10.1001/jamapediatrics.2018.4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Child and Adolescent Health Measurement Initiative (CAHMI). 2016–2017 National Survey of Children’s Health: Child and Family Health Measures, National Performance and Outcome Measures, and Subgroups, SAS Codebook, Version 1.0. www.census.gov/programs-surveys/nsch/data.html Published January 2019. Accessed February 1, 2019.
- 25.Ghandour RM, Jones JR, Lebrun-Harris LA, et al. The design and implementation of the 2016 National Survey of Children’s Health. Matern Child Health J. 2018;22(8):1093–1102. 10.1007/s10995-018-2526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ekelund U, Brage S, Froberg K, et al. TV viewing and physical activity are independently associated with metabolic risk in children: the European Youth Heart Study. PLoS Med. 2006;3(12):e488 10.1371/journal.pmed.0030488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Poitras VJ, Gray CE, Borghese MM, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S197–S239. 10.1139/apnm-2015-0663. [DOI] [PubMed] [Google Scholar]
- 28.Carson V, Hunter S, Kuzik N, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metab. 2016;41(6):S240–S265. 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- 29.Chaput JP, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S266–S282. 10.1139/apnm-2015-0627. [DOI] [PubMed] [Google Scholar]
- 30.Roman-Vinas B, Chaput JP, Katzmarzyk PT, et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13(1):123 10.1186/s12966-016-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hjorth MF, Chaput JP, Damsgaard CT, et al. Low physical activity level and short sleep duration are associated with an increased cardio-metabolic risk profile: a longitudinal study in 8–11 year old Danish children. PloS One. 2014;9(8):e104677 10.1371/journal.pone.0104677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walsh JJ, Barnes JD, Cameron JD, et al. Associations between 24 hour movement behaviours and global cognition in U.S. children: a cross-sectional observational study. Lancet Child Adolesc Health. 2018;2(11):783–791. 10.1016/s2352-4642(18)30278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saunders TJ, Gray CE, Poitras VJ, et al. Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S283–S293. 10.1139/apnm-2015-0626. [DOI] [PubMed] [Google Scholar]
- 34.Australian Government Department of Health. Australian 24-Hour Movement Guidelines for Children and Young People (5–17 years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep. https://www1.health.gov.au/internet/main/publishing.nsf/Content/health-24-hours-phys-act-guidelines Published 2019. Accessed May 12, 2020.
- 35.Owens J, Adolescent Sleep Working Group, Committee on Adolescence. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–e932. 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Telama R, Yang X, Viikari J, Välimäki I, Wanne O, Raitakari O. Physical activity from childhood to adulthood: a 21-year tracking study. Am J Prev Med. 2005;28(3):267–273. 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 37.Lounassalo I, Salin K, Kankaanpaa A, et al. Distinct trajectories of physical activity and related factors during the life course in the general population: a systematic review. BMC Public Health. 2019;19(1):271 10.1186/s12889-019-6513-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Influence Central. Kids & Tech: The Evolution of Today’s Digital Natives. http://blog.influence-central.com/kids-tech-the-evolution-of-todays-digital-natives/ Published 2016. Accessed May 12, 2020.
- 39.U.S. Census Bureau, Associate Director of Demographic Programs, National Survey of Children’s Health. 2017. National Survey of Children’s Health Nonresponse Bias Analysis. www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/nonresponse-bias-analysis/NSCH_2017_Nonresponse_Bias_Analysis.pdf Updated January 10, 2019 Accessed May 12, 2020.
- 40.Himes JH. Challenges of accurately measuring and using BMI and other indicators of obesity in children. Pediatrics. 2009;124(Suppl 1):S3–S22. 10.1542/peds.2008-3586d. [DOI] [PubMed] [Google Scholar]
- 41.Adamo KB, Prince SA, Tricco AC, Connor-Gorber S, Tremblay M. A comparison of indirect versus direct measures for assessing physical activity in the pediatric population: a systematic review. Int J Pediatr Obes. 2009;4(1):2–27. 10.1080/17477160802315010. [DOI] [PubMed] [Google Scholar]
- 42.Straker L, Zabatiero J, Danby S, Thorpe K, Edwards S. Conflicting guidelines on young children’s screen time and use of digital technology create policy and practice dilemmas. J Pediatr. 2018;202:300–303. 10.1016/j.jpeds.2018.07.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.