Purpose of review
Technological advancement has led to the development of novel treatment approaches for attention deficit hyperactivity disorder (ADHD). This review aims to review recent studies which employ the use of technology to treat ADHD, with particular focus on studies published during a 1-year period from February 2019 to February 2020.
Recent findings
Most recent studies involved children aged 12 years and below. Interventions included cognitive training through games, neurofeedback and a combination of several approaches. More novel approaches included trigeminal nerve stimulation and brain–computer interface, and studies had utilized technology such as X-box Kinect and eye tracker. There was a shift towards delivering intervention at home and in school, enabled by technology. The study outcomes were variable and mainly included executive functioning measures and clinical ratings. These interventions were generally safe with few reported adverse events.
Summary
Technology has enabled interventions to be delivered outside of the clinic setting and presented an opportunity for increased access to care and early intervention. Better quality studies are needed to inform on the efficacy of these interventions.
Keywords: attention deficit hyperactivity disorder, attention training, cognitive training
INTRODUCTION
Attention deficit hyperactivity disorder (ADHD) is among the most prevalent child psychiatric conditions [1–4]. This neurodevelopmental disorder can persist into adulthood and result in significant adverse health and psychosocial outcomes including higher incidence of comorbid mental health disorders, occupational difficulties and marital conflicts; hence ADHD is associated with significant burden [5–7]. Pharmacological and psychosocial interventions are the main evidence-based approaches [8–11]. However, due to the limitations associated with these treatments including undesirable side effects, an intense level of commitment and unclear long-term benefits, alternatives which are effective, safe and cost-efficient are needed [12–14].
Understanding the pathophysiology of ADHD is necessary to enable the search for other intervention approaches (Fig. 1). Although stimulant and nonstimulant medications correct the underlying neurochemical (catecholamine) deficit, neuroimaging studies have helped identify affected brain networks in ADHD. These include the ventral attention, frontoparietal, default mode and visual networks [15▪]. ADHD has long been associated with executive function deficits including organization, working memory and inhibition [16,17]. Cognitive training could reducing these deficits by strengthening key neural networks, leading to overall functional improvement [18,19]. Neurofeedback therapy targets electroencephalogram (EEG) abnormalities such as excessive cortical slowing and increased theta waves (with corresponding reduced beta-theta ratios), another reflection of the underlying network abnormalities [20–23]. Neurofeedback therapy has been shown to strengthen the brain's attentional circuits [24▪]. Others have examined the use of physical exercise which can lead to neuroplastic changes and neurophysiological changes such as increased levels of fronto-striatal catecholamines [25,26].
FIGURE 1.
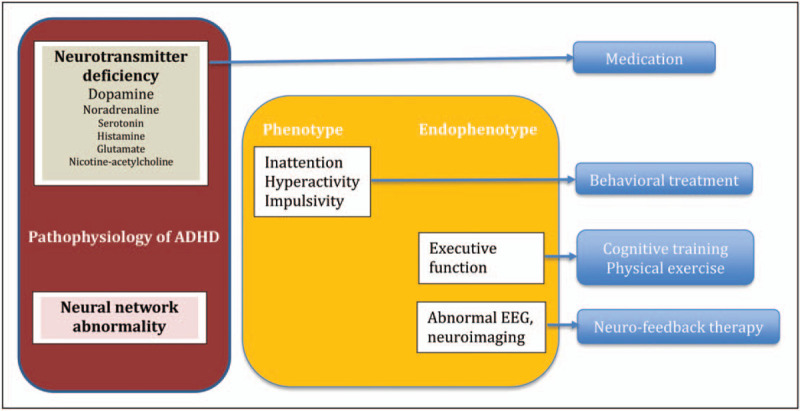
Pathophysiology of attention deficit hyperactivity disorder and targets of intervention.
Box 1.
no caption available
Technological advancement has led to more specific adaption of intervention options for ADHD. Indeed, progress in technology has reduced the reliance on mental health professionals to administer intervention and allowed for a more cost-effective and flexible delivery of treatment [27]. In their review of technology-based care for ADHD, Benyakorn et al.[28] categorized the use of technology into direct care provision (e.g. computerized cognitive training) and supporting care provision (e.g. health information technology). It is critical to fully understand the emerging evidence around the domains of ADHD difficulties in which technology has been applied to address, describe associated key findings, as well as identify any limitations. This rapid review will provide an update to the current empirical base by identifying research involving technology for treating ADHD, with particular focus on the preceding 1-year period.
METHOD
Studies were identified through a systematic search across the following electronic databases: PsycINFO and MEDLINE. The search terms used were (attention deficit hyperactivity disorder) in combination with (intervention, programme, treatment, training, therapy) and (computer, Internet, technology, video, online). The respective terms with truncation were first searched and subsequently combined using Boolean searching. Specific key words were also identified in empirical articles arising from the initial search, and further searches utilized combinations of the following search string: neurofeedback OR electroencephalogram OR transcranial-magnetic OR brain OR executive function OR cognition OR virtual reality OR augmented reality.
A study was deemed to be suitable for inclusion if it met the following criteria:
-
(1)
Examined the effectiveness of a technology-based intervention for ADHD,
-
(2)
The intervention was tested on both children and/or adults with ADHD,
-
(3)
The intervention was directed to improve primary ADHD symptoms (e.g. impulsivity, inattention),
-
(4)
Written in English,
-
(5)
Published in a peer-reviewed journal (dissertations, book chapters were excluded),
-
(6)
Published between February 2019 to February 2020.
The second author with the help of her intern independently reviewed the included abstracts according to the inclusion criteria outlined above. Any further duplication of studies and/or data was removed. Discrepancies were discussed, and the first author was consulted where appropriate. The full text of studies that met the selection criteria were then retrieved, and reviewed by the authors to ensure their relevance. Figure 2 illustrates the search and inclusion process.
FIGURE 2.
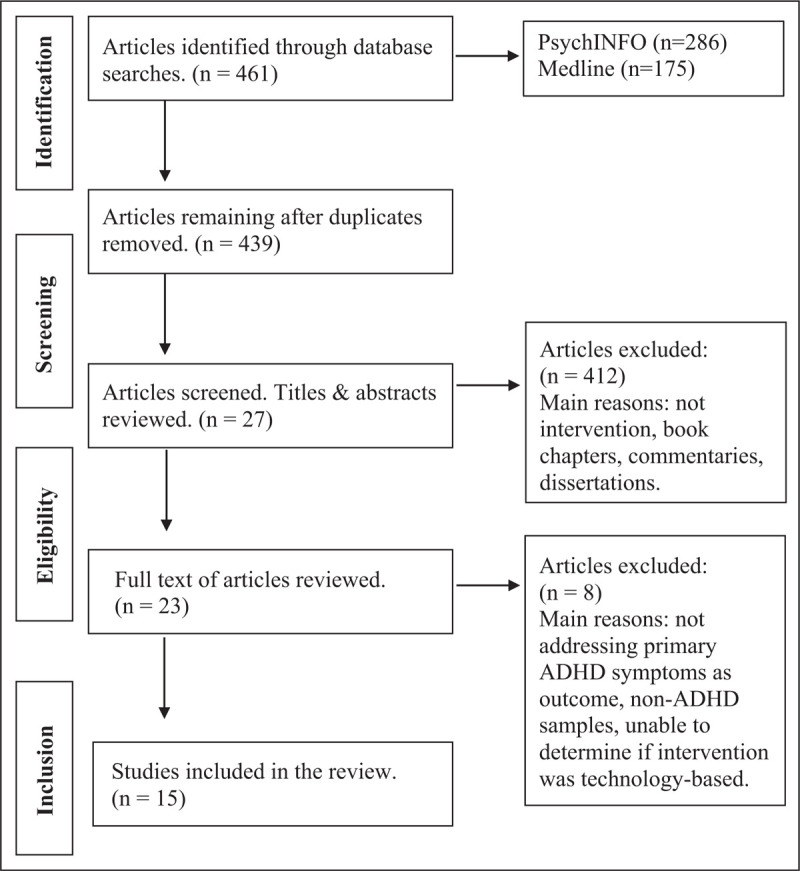
Information about study screening, selection and inclusion.
SUMMARY OF MAIN FINDINGS
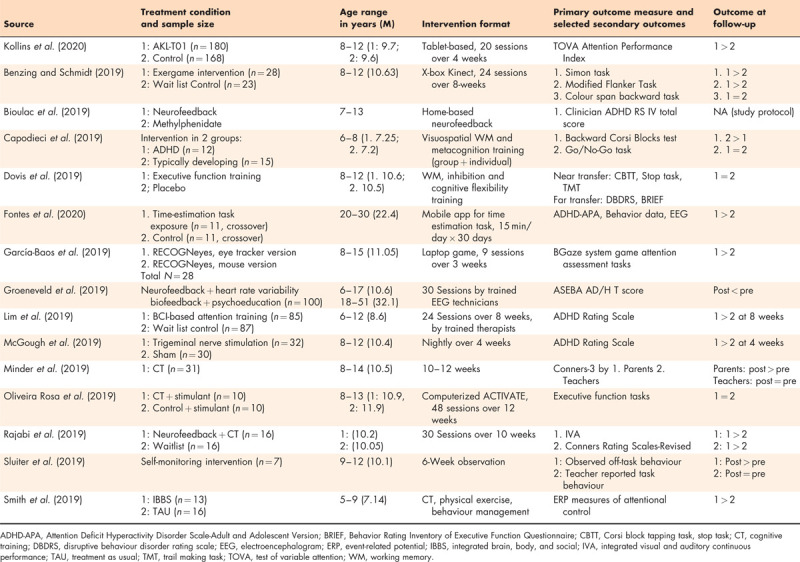
In all, 15 studies fulfilled all the selection benchmarks and were included. The majority of the identified studies offered treatment for young person's between the age of 5–17 years old (n = 14; 93.3%). These interventions were offered through a variety of technology-assisted modalities. Duration and intensity of the treatment differed across the studies. Table 1 presents a detailed summary of the characteristics of the identified studies.
Table 1.
All eligible studies identified during systematic review
RESULTS AND DISCUSSION
Digital interventions and serious games
With today's connected youths, cognitive training through games may be more engaging [29–33]. Termed ‘serious games’ due to their training purpose rather than for entertainment, these digital games for ADHD can train several cognitive domains [34]. They can also incorporate biofeedback, virtual reality and augmented reality to facilitate mastery and transfer effect to untrained domains and ultimately, to daily life situations [35–38]. Such digital training has been shown to lead to EEG changes in the prefrontal cortex [39]. Reviews of previous studies on serious games for ADHD had cited concern regarding the limited quality of most studies [40▪,41].
Kollins et al.[42▪] reported their large randomized, double blind, parallel-group, controlled trial involving 346 children aged 8–12 years. The intervention programme was a home-based digital game with cognitive training components involving attention control and set shifting, within built real-time adaptive mechanism to personalize the training level. Although there was evidence of effective attention control (i.e. near transfer effect) postintervention, these skill set was not generalized to new contextual settings (far transfer effect).
Studies have examined metacognitive therapy in adults with ADHD [43▪]. To enhance far transfer skills, Capodieci et al.[44] incorporated metacognitive elements such as active reflection and promotion of self-awareness to the working memory training tasks. Their open-label study suggested that both children with ADHD and typically developing children showed some transfer effect to other executive functions after intervention, with the ADHD group showing improved behavioural rating.
Cognitive therapy may be more beneficial for a subgroup of children with ADHD, especially those with more severe executive function deficit [45–48]. Dovis et al. tested this hypothesis in their placebo-controlled study to elucidate the effect of pretraining executive function as a moderator of outcome of a gamified home-based 5-week training programme. However, those with poorer pretraining working memory and inhibition did not benefit more [49].
In an interesting study conducted in a classroom setting, teachers delivered the gamified attention training to students aged 5–9 years. Compared with the control groups, students in the intervention group showed improved attention and hyperactivity ratings, even at 6 months’ follow-up, although there were no cognitive or academic gains [50▪]. Although the study did not specifically enrol children with ADHD, it represents an opportunity for upstream school-based intervention.
Earlier studies have shown that cognitive training results in increased activation in related brain regions [51,52]. In their functional MRI study of children with ADHD, de Oliveira Rosa et al.[53▪] found that those who received cognitive training and stimulant medication showed greater activation of the right fronto-parietal brain areas that mediate sustained attention after intervention, compared with those who received nonactive computerized intervention with stimulant medication. This added further evidence that cognitive training could normalize neural circuits in children with ADHD.
Future cognitive training programmes should involve several cognitive domains, be personalized to the individual needs and ability, include components to increase engagement as well as promote transfer of skills to daily tasks. Delivering interventions at home and in school can increase access to intervention and promote upstream intervention.
Neurofeedback and related therapy
Standard neurofeedback treatment protocols include sensori-motor rhythm neurofeedback, theta/beta neurofeedback and slow cortical potential neurofeedback [54]. Though many studies have reported positive results, reviews have highlighted the need for better quality studies, need to examine longer term efficacy and the lack of standardized training for therapists [55–59].
An alternative approach is Z-score neurofeedback which is less studied [60]. Groeneveld et al.[61] combined Z-score neurofeedback and heart rate variability training (biofeedback) in their study involving both adults and children with clinical and subclinical ADHD symptoms. They reported improvement in behavioural symptoms and normalization of EEG postintervention.
A novel brain computer interface-based intervention used machine learning technique to develop a unique algorithm utilizing the entire EEG spectrum, with feedback and training activities incorporated into a game [62–64]. Academic tasks were included to promote skills transfer. Their large randomized wait-list control trial involving 172 children aged 6–12 years diagnosed with ADHD found the effect size of the intervention was small, based on blinded clinician ratings [65▪]. A subgroup of the children underwent neuroimaging, which revealed that those with improved behavioural rating tended to exhibit increased functional network reorganization, especially within the salience/ventral attention network [66].
As we move towards personalized medicine, further research can uncover predictors of positive response to neurofeedback [67]. Technology advancement has boosted the ease of programmed home-based neurofeedback treatment, removing the need for therapist training [68]. For instance, the multichannel EEG cap has now been replaced by the more user-friendly headband utilizing much fewer channels. One study to look out for is Bioulac's head-to-head clinical trial comparing a novel home-based neurofeedback intervention with long-acting methylphenidate [69].
Technology-assisted delivery of standard treatment
Telehealth has been on the rise to improve access to mental healthcare, as communication technology like videoconferencing improves. Synonymous terms include telepsychiatry and telemental health. Telepsychiatry can be an effective way to deliver care for ADHD [70–74]. A review has concluded that telemedicine was cost-effective for children and suggested that research should also be conducted in adults with ADHD [75]. In the pipeline, there is a randomized controlled trial underway to investigate the efficacy of a web-assisted self-help programme for parents of children with ADHD [76].
Mobile apps have been developed to support young persons and their caregivers including parents, teachers and professionals, as well as adults with ADHD [77,78]. Despite the large number of apps available, they may not necessarily match the users’ needs and there has been little research done to properly evaluate them [79,80▪].
Biederman's study found that text messages could significantly improve timely refill of prescriptions in adult patients with ADHD [81]. The use of readily available technology can facilitate more effective delivery of evidence-based intervention and are potential quality improvement projects.
Multidomain approaches
Technology can combine the training of multiple domains into a seamless programme. In their randomized waitlist control trial, Johnstone et al.[82] tested a home-based gamified intervention combining working memory, inhibitory control and neurofeedback in 85 children aged 7–12 with clinical and subclinical ADHD. Behavioural improvement did not reach significance and the children became less engaged with further sessions. Similarly, Rajabi et al.[83] studied combined cognitive training and neurofeedback, and their sample improved in behavioural ratings and visual attention, compared with untreated controls. We are likely to see more similar multimodal intervention emerging.
Cognitively engaging physical exercise can increase cognitive performance in ADHD possibly through training the brain regions involved in higher order cognition [84,85]. Benzing and Schmidt [86] developed a home-based ‘exergaming’ intervention and tested the 8-week programme in 51 children aged 8–12 in their randomized waitlist-control study. Utilizing X-box Kinect to control movement, these adaptive games train strength, coordination and endurance, as well as cognitive functions of inhibition, attention and set shifting. The intervention group improved in their executive functions (inhibition, switching, updating), general psychopathology and motor abilities compared with the control group. In their multisite study, Smith et al.[87] combined computerized cognitive training and physical exercises in their intervention, which was delivered in a classroom setting by teachers and therapists. Their behaviour ratings at the end of the study did not differ from the control group which received psychosocial and or pharmacological interventions.
Other approaches
Neurostimulation induces longer term changes in brain excitability or neurotransmission through the application of electrical or magnetic stimulation [88▪]. Trigeminal nerve stimulation (TNS) can activate higher brain centres through the nerve's projections, including those involved in ADHD such as the locus coeruleus, thalamus and anterior cingulate cortex [89,90]. The Monarch external TNS System became the first medical device for treating ADHD to receive marketing authorization from the US Food and Drug Administration, based on the study by McGough et al.[91]. They conducted a blinded sham-controlled trial and randomized 62 children 8–12 years old with ADHD to 4 weeks of nightly treatment with active TNS or sham treatment [92▪]. The intervention group improved significantly in their behavioural and clinical ratings. Though well tolerated, it remains to be seen if the results can be replicated in other clinical trials, and whether any improvement can be sustained over time.
García-Baos et al.[93▪] hypothesized that eye gaze can therefore be a proxy measure for attention and inhibitory control. They designed a computerized game which utilized an eye tracker, to train the child's visual attention control, to influence the attention network. The intervention group, when compared with the control group playing the same game without the eye tracker, showed improvement in their impulsivity, reaction time and gaze control. More studies will be needed to support this approach.
Time estimation has recently gained interest, with studies suggesting interval-timing dysfunction being associated with ADHD [94–96]. In their study involving young adults with ADHD, Fontes et al.[97] showed, in their crossover study, that a training programme involving time estimation exposure tasks was promising in improving ADHD symptoms and cognitive function.
Monitoring sensors such as accelerometer and technology such as smartglassees were previously studied [98]. Sluiter et al.[99] used a timer to regularly remind seven students with ADHD in a special needs classroom to monitor their on-task behaviour. Although their observed off-task behaviour was significantly reduced, most of their executive functions did not improve except for inhibition. This approach is not likely to be a primary treatment but may be a tool to aid behavioural management in ADHD.
CONCLUSION
The use of technology has moved intervention for ADHD towards becoming home-based and even school-based, with the potential for individualization of treatment, improved access to care and early intervention. This exciting development is in the right direction towards personalized medicine and population health. The lack of high-quality trials to provide more reliable evidence for the efficacy of most intervention remains a significant challenge. More rigorous studies will be needed to inform us whether technology-based advancement contributes positively towards the accessibility of early intervention as well as the efficacy and challenges of home-based intervention. In addition, a combination of interventional components, and individualization of treatment appears feasible and may be promising.
Acknowledgements
The authors gratefully acknowledge the support received from Ms Ng Weng Lin, who was working as an intern with our department then, and contributed to the systematic search process and identification of suitable articles.
Financial support and sponsorship
None.
Conflicts of interest
The authors’ work was described and referenced within the article.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007; 164:942–948. [DOI] [PubMed] [Google Scholar]
- 2.Erskine HE, Ferrari AJ, Nelson P, et al. Epidemiological modelling of attention-deficit/hyperactivity disorder and conduct disorder for the Global Burden of Disease Study 2010. J Child Psychol Psychiatry 2013; 54:1263–1274. [DOI] [PubMed] [Google Scholar]
- 3.Polanczyk GV, Willcutt EG, Salum GA, et al. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol 2014; 43:434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas R, Sanders S, Doust J, et al. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics 2015; 135:e994–e1001. [DOI] [PubMed] [Google Scholar]
- 5.Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev 2013; 33:215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Erskine HE, Ferrari AJ, Polanczyk GV, et al. The global burden of conduct disorder and attention-deficit/hyperactivity disorder in 2010. J Child Psychol Psychiatry 2014; 55:328–336. [DOI] [PubMed] [Google Scholar]
- 7.Epidemiology & Disease Control Division, Ministry of Health, Singapore; Institute for Health Metrics and Evaluation The burden of disease in Singapore, 1990–2017: an overview of the global burden of disease study 2017 results. Seattle, WA: IHME; 2019. [Google Scholar]
- 8.Cortese S, Coghill D. Twenty years of research on attention-deficit/hyperactivity disorder (ADHD): looking back, looking forward. Evid Based Mental Health 2018; 21:173–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kemper AR, Maslow GR, Hill S, et al. Attention deficit hyperactivity disorder: diagnosis and treatment in children and adolescents. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018. [PubMed] [Google Scholar]
- 10.NICE Attention deficit hyperactivity disorder: diagnosis and management. 2019; Available from: www.nice.org.uk/guidance/NG87. [Accessed on 8 May 2020]. [PubMed] [Google Scholar]
- 11.Boland H, DiSalvo M, Fried R, et al. A literature review and meta-analysis on the effects of ADHD medications on functional outcomes. J Psychiatr Res 2020; 123:21–30. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006; 163:716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Molina BS, Hinshaw SP, Swanson JM, et al. MTA Cooperative Group The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 2009; 48:484–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hechtman L, Swanson JM, Sibley MH, et al. MTA Cooperative Group Functional adult outcomes 16 years after childhood diagnosis of attention deficit/hyperactivity disorder: MTA results. J Am Acad Child Adolesc Psychiatry 2016; 55:945–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15▪.Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet 2020; 395:450–462. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a succinct and current review which provides an up-to-date summary of current knowledge regarding the cause, assessment and treatment of attention deficit hyperactivity disorder (ADHD).
- 16.Castellanos FX, Tannock R. Neuroscience of attention-deficit/hyperactivity disorder: the search for endophenotypes. Nat Rev Neurosci 2002; 3:617–628. [DOI] [PubMed] [Google Scholar]
- 17.Hervey AS, Epstein JN, Curry JF. Neuropsychology of adults with attention deficit/hyperactivity disorder: a meta-analytic review. Neuropsychol 2004; 18:485–503. [DOI] [PubMed] [Google Scholar]
- 18.Klingberg T. Training and plasticity of working memory. Trends Cogn Sci 2010; 14:317–324. [DOI] [PubMed] [Google Scholar]
- 19.Vinogradov S, Fisher M, de Villers-Sidani E. Cognitive training for impaired neural systems in neuropsychiatric illness. Neuropsychopharmacology 2012; 37:43–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chabot RA, Serfontein G. Quantitative electroencephalographic profiles of children with attention deficit disorder. Biol Psychiatry 1996; 40:951–963. [DOI] [PubMed] [Google Scholar]
- 21.Monastra VJ. Electroencephalographic biofeedback (neurotherapy) as a treatment for attention deficit hyperactivity disorder: rationale and empirical foundation. Child Adolesc Psychiatr Clin N Am 2005; 14:55–82. [DOI] [PubMed] [Google Scholar]
- 22.Boutros N, Fraenkel L, Feingold A. A fourstep approach for developing diagnostic tests in psychiatry: EEG in ADHD as a test case. J Neuropsychiatry Clin Neurosci 2005; 17:455–464. [DOI] [PubMed] [Google Scholar]
- 23.Arns M, Conners CK, Kraemer HC. A decade of EEG theta/beta ratio research in ADHD: a meta-analysis. J Atten Disord 2013; 17:374–383. [DOI] [PubMed] [Google Scholar]
- 24▪.Rubia K, Criaud M, Wulff M, et al. Functional connectivity changes associated with functional magnetic resonance imaging (fMRI) neurofeedback of right inferior frontal cortex in adolescents with ADHD. Neuroimage 2019; 188:43–58. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study shows for the first time than fMRI-neurofeedback leads to changes in neural networks which may explain the clinical improvement.
- 25.Wigal SB, Nemet D, Swanson JM, et al. Catecholamine response to exercise in children with attention deficit hyperactivity disorder. Pediatr Res 2003; 53:756–761. [DOI] [PubMed] [Google Scholar]
- 26.Anish EJ. Exercise and its effects on the central nervous system. Curr Sports Med Rep 2005; 4:18–23. [DOI] [PubMed] [Google Scholar]
- 27.Boydell KM, Hodgins M, Pignatiello A, et al. Using technology to deliver mental health services to children and youth: a scoping review. J Can Acad Child Adolesc Psychiatry 2014; 23:87–99. [PMC free article] [PubMed] [Google Scholar]
- 28.Benyakorn S, Riley SJ, Calub CA, Schweitzer JB. Current state and model for development of technology-based care for attention deficit hyperactivity disorder. Telemed J E Health 2016; 22:761–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dovis S, Van der Oord S, Wiers RW, et al. Improving executive functioning in children with ADHD: training multiple executive functions within the context of a computer game. A randomized double-blind placebo controlled trial. PLoS One 2015; 10:e0121651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bul KCM, Franken IHA, Van der Oord S, et al. Development and user satisfaction of ‘Plan-It Commander,’ a serious game for children with ADHD. Games Health J 2015; 4:502–512. [DOI] [PubMed] [Google Scholar]
- 31.Bul KC, Kato PM, Van der Oord S, et al. Behavioral outcome effects of serious gaming as an adjunct to treatment for children with attention-deficit/hyperactivity disorder: a randomized controlled trial. J Med Internet Res 2016; 18:e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baranowksi T, Buday R, Thompson I, et al. Playing for real. Video games and stories for health-related behavior change. Am J Prev Med 2008; 34:74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prins PJM, Dovis S, Ponsioen A, et al. Does computerized working memory training with game elements enhance motivation and training efficacy in children with ADHD? Cyberpsychol Behav Soc Netw 2011; 14:115–122. [DOI] [PubMed] [Google Scholar]
- 34.Michael D, Chen S. Serious games: games that educate, train, and inform. Boston, MA: Thomson Course Technology; 2006. [Google Scholar]
- 35. Sonne T, Jensen MM. ChillFish: a respiration game for children with ADHD. Proceedings of the 10th Anniversary Conference on Tangible Embedded and Embodied Interaction (TEI). 14–17 February 2016; Eindhoven, Netherlands. New York: Association for Computing Machinery 2016; pp. 271–278. [Google Scholar]
- 36. Avila-Pesantez D, Rivera LA, Vaca-Cardenas L, et al. Towards the improvement of ADHD children through augmented reality serious games: preliminary results. Proceedings of the 2018 IEEE Global Engineering Education Conference (EDUCON). 18–20 April 2018; Santa Cruz de Tenerife, Canary Islands, Spain. Piscataway: Institute of Electrical and Electronics Engineers 2018; pp. 843–848. [Google Scholar]
- 37.Lau HM, Smit JH, Fleming TM, et al. Serious games for mental health: are they accessible, feasible, and effective? A systematic review and meta-analysis. Front Psychiatry 2017; 7:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shema-Shiratzky CS, Brozgol M, Cornejo-Thumm P, et al. Virtual reality training to enhance behavior and cognitive function among children with attention-deficit/hyperactivity disorder: brief report. Dev Neurorehabil 2019; 22:431–436. [DOI] [PubMed] [Google Scholar]
- 39.Anguera JA, Boccanfuso J, Rintoul JL, et al. Video game training enhances cognitive control in older adults. Nature 2013; 501:97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪.Kokol P, Vošner HB, Završnik J, et al. Serious game-based intervention for children with developmental disabilities. Curr Pediatr Rev 2020; 16:26–32. [DOI] [PubMed] [Google Scholar]; The article reviews serious games for developmental disorders including ADHD and provides a good summary of related work.
- 41.Strahler Rivero T, Herrera Nuñez LM, Uehara Pires E, Amodeo Bueno OF. ADHD rehabilitation through video gaming: a systematic review using PRISMA guidelines of the current findings and the associated risk of bias. Front Psychiatry 2015; 6:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42▪.Kollins SH, DeLoss DJ, Cañadas E, et al. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): a randomised controlled trial. Lancet Digital Health 2020; 2:e168–e178. [DOI] [PubMed] [Google Scholar]; The trial is important because of its strong design and large sample size, and probably gives a good estimate of the effect of game-based cognitive training. The games were also adaptive in nature ad trained multiple cognitive domains.
- 43▪.Nimmo-Smith V, Merwood A, Hank D. Nonpharmacological interventions for adult ADHD: a systematic review. Psychol Med 2020; 50:529–541. [DOI] [PubMed] [Google Scholar]; The review provides an overview of studies investigating various psychological therapies, neurofeedback, cognitive training and self-monitoring in adults with ADHD.
- 44.Capodieci A, Re AM, Fracca A, et al. The efficacy of a training that combines activities on working memory and metacognition: transfer and maintenance effects in children with ADHD and typical development. J Clin Exp Neuropsychol 2019; 41:1074–1087. [DOI] [PubMed] [Google Scholar]
- 45.Sjowall D, Thorell LB. A critical appraisal of the role of neuropsychological deficits in preschool ADHD. Child Neuropsychol 2019; 25:60–80. [DOI] [PubMed] [Google Scholar]
- 46.Bunger A, Urfer-Maurer N, Grob A. Multimethod assessment of attention, executive functions, and motor skills in children with and without ADHD: children's performance and parents’ perceptions. J Atten Disord 2019; 30:1087054718824985. [DOI] [PubMed] [Google Scholar]
- 47.Holst Y, Thorell LB. Functional impairments among adults with ADHD: a comparison with adults with other psychiatric disorders and links to executive deficits. Appl Neuropsychol Adult 2020; 27:243–255. [DOI] [PubMed] [Google Scholar]
- 48.Diamond A. Activities and programs that improve children's executive functions. Curr Dir Psychol Sci 2012; 21:335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dovis S, Maric M, Prins PJM, van der Oord S. Does executive function capacity moderate the outcome of executive function training in children with ADHD? Atten Defic Hyperact Disord 2019; 11:445–460. [DOI] [PubMed] [Google Scholar]
- 50▪.Kirk HE, Spencer-Smith M, Wiley JF, Cornish KM. Gamified attention training in the primary school classroom: a cluster-randomized controlled trial. J Atten Disord 2019. 1087054719887435. [DOI] [PubMed] [Google Scholar]; The trial demonstrated that the classroom-based intervention reduced overall hyperactivity and inattention in the students. This may be an opportunity for upstream intervention.
- 51.Stevens MC, Gaynor A, Bassette KL, Pearlson GD. A preliminary study of the effects of working memory training on brain function. Brain Imaging Behav 2016; 10:387–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hoekzema E, Carmona S, Tremols V, et al. Enhanced neural activity in frontal and cerebellar circuits after cognitive training in children with attention-deficit/hyperactivity disorder. Hum Brain Mapp 2010; 31:1942–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53▪.de Oliveira Rosa V, Rosa Franco A, Abrahão Salum Júnior G, et al. Effects of computerized cognitive training as add-on treatment to stimulants in ADHD: a pilot fMRI study. Brain Imaging Behav 2019; doi:10.1007/s11682-019-00137-0. [DOI] [PubMed] [Google Scholar]; The article is the first functional imaging study to compare the effect of cognitive training and medication, versus nonactive training and medication.
- 54.Arns M, Heinrich H, Strehl U. Evaluation of neurofeedback in ADHD: the long and winding road. Biol Psychol 2014; 95:108–115. [DOI] [PubMed] [Google Scholar]
- 55.Cortese S, Ferrin M, Brandeis D, et al. Neurofeedback for attention-deficit/hyperactivity disorder: meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. J Am Acad Child Adolesc Psychiatry 2016; 55:444–455. [DOI] [PubMed] [Google Scholar]
- 56.Razoki B. Neurofeedback versus psychostimulants in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a systematic review. Neuropsychiatr Dis Treat 2018; 14:2905–2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Enriquez-Geppert S, Smit D, Pimenta MG. Neurofeedback as a treatment intervention in ADHD: current evidence and practice. Curr Psychiatry Rep 2019; 21:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arns M, Clark CR, Trullinger M, et al. Neurofeedback and attention deficit/hyperactivity disorder (ADHD) in children: rating the evidence and proposed guidelines. Appl Psychophysiol Biofeedback 2020; 45:39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee GJ, Suhr JA. Expectancy effects on self-reported attention-deficit/hyperactivity disorder symptoms in simulated neurofeedback: a pilot study. Arch Clin Neuropsychol 2019; 34:200–205. [DOI] [PubMed] [Google Scholar]
- 60.Coben R, Hammond DC, Arns M. 19 Channel z-score and LORETA neurofeedback: does the evidence support the hype? Appl Psychophysiol Biofeedback 2019; 44:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Groeneveld KM, Mennenga AM, Heidelberg RC, et al. Z-Score neurofeedback and heart rate variability training for adults and children with symptoms of attention-deficit/hyperactivity disorder: a retrospective study. Appl Psychophysiol Biofeedback 2019; 44:291–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lim CG, Lee TS, Guan C, et al. Effectiveness of a brain–computer interface based programme for the treatment of ADHD: a pilot study. Psychopharmacol Bull 2010; 43:73–82. [PubMed] [Google Scholar]
- 63.Lim CG, Lee TS, Guan C, et al. A brain–computer interface based attention training program for treating attention deficit hyperactivity disorder. PLoS One 2012; 7:e46692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McDermott AF, Rose M, Norris T, Gordon E. A novel feed-forward modeling system leads to sustained improvements in attention and academic performance. J Atten Disord 2016; 24:1443–1456. [DOI] [PubMed] [Google Scholar]
- 65▪.Lim CG, Poh XWW, Fung SSD, et al. A randomized controlled trial of a brain–computer interface based attention training program for ADHD. PLoS One 2019; 14:e0216225. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the first randomized controlled trial to demonstrate the clinical efficacy of a brain–computer-interface-based attention training programme for treating ADHD. A related earlier publication by Qian et al. reported normalization of the salience network postintervention.
- 66.Qian X, Loo BRY, Castellanos FX, et al. Brain–computer-interface-based intervention re-normalizes brain functional network topology in children with attention deficit/hyperactivity disorder. Transl Psychiatry 2018; 8:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bashar R. Neurofeedback versus psychostimulants in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a systematic review. Neuropsychol Dis Treat 2018; 14:2905–2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Enriquez-Geppert S, Smit D, Pimenta MG, Arns M. Neurofeedback as a treatment intervention in ADHD: current evidence and practice. Curr Psychiatry Rep 2019; 21:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bioulac S, Purper-Ouakil D, Ros T, et al. Personalized at-home neurofeedback compared with long-acting methylphenidate in an European noninferiority randomized trial in children with ADHD. BMC Psychiatry 2019; 19:237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Myers K, Vander Stoep A, Zhou C, et al. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2015; 54:263–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Reese RJ, Slone NC, Soares N, Sprang R. Telehealth for underserved families: an evidence-based parenting program. Psychol Serv 2012; 9:320–322. [DOI] [PubMed] [Google Scholar]
- 72.Xie Y, Dixon JF, Yee OM, et al. A study on the effectiveness of videoconferencing in teaching parent training skills to parents of children with ADHD. Telemed J E Health 2013; 19:192–199. [DOI] [PubMed] [Google Scholar]
- 73.Tse YJ, McCarty CA, Stoep AV, Myers KM. Teletherapy delivery of caregiver behavior training for children with attention-deficit hyperactivity disorder. Telemed J E Health 2015; 21:451–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stoep AV, McCarty CA, Zhou C, et al. The children's attention-deficit hyperactivity disorder telemental health treatment study: caregiver outcomes. J Abnorm Child Psychol 2017; 45:27–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Spencer T, Noyes E, Biederman J. Telemedicine in the management of ADHD: literature review of telemedicine in ADHD. J Atten Disord 2020; 24:3–9. [DOI] [PubMed] [Google Scholar]
- 76.Döpfner M, Wähnke L, Klemp M, et al. Efficacy of web-assisted self-help for parents of children with ADHD (WASH) – a three-arm randomized trial under field/routine care conditions in Germany. BMC Psychiatry 2020; 20:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schuck S, Emmerson N, Ziv H, et al. Designing an iPad app to monitor and improve classroom behavior for children with ADHD: iSelfControl feasibility and pilot studies. PLoS One 2016; 11:e0164229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Luiu AL, Prada P, Perroud N, et al. ADHD mobile app feasibility test for adults. Stud Health Technol Inform 2018; 255:247–251. [PubMed] [Google Scholar]
- 79.Powell L, Parker J, Harpin V. ADHD: is there an app for that? A suitability assessment of apps for the parents of children and young people with ADHD. JMIR Mhealth Uhealth 2017; 5:e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80▪.Păsărelu CR, Andersson G, Dobrean A. Attention-deficit/hyperactivity disorder mobile apps: a systematic review. Int J Med Inform 2020; 138:104133. [DOI] [PubMed] [Google Scholar]; This is the first systematic review of mobile apps targeting the management of ADHD and highlights the lack of well designed studies to evaluate their efficacy despite their ready availability.
- 81.Biederman J, Fried R, DiSalvo M, et al. A novel text message intervention to improve adherence to stimulants in adults with attention deficit/hyperactivity disorder. J Clin Psychopharmacol 2019; 39:351–356. [DOI] [PubMed] [Google Scholar]
- 82.Johnstone SJ, Roodenrys SJ, Johnson K. Game-based combined cognitive and neurofeedback training using Focus Pocus reduces symptom severity in children with diagnosed AD/HD and subclinical AD/HD. Int J Psychophysiol 2017; 116:32–44. [DOI] [PubMed] [Google Scholar]
- 83.Rajabi S, Pakize A, Moradi N. Effect of combined neurofeedback and game-based cognitive training on the treatment of ADHD: a randomized controlled study. Appl Neuropsychol Child 2019; 9:193–205. [DOI] [PubMed] [Google Scholar]
- 84.Halperin JM, Healey DM. The influences of environmental enrichment, cognitive enhancement, and physical exercise on brain development: can we alter the developmental trajectory of ADHD? Neurosci Biobehav Rev 2011; 35:621–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Vazou S, Pesce C, Lakes K, Smiley-Oyen A. More than one road leads to Rome: a narrative review and meta-analysis of physical activity intervention effects on cognition in youth. Int J Sport Exerc Psychol 2016; 17:1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Benzing V, Schmidt M. The effect of exergaming on executive functions in children with ADHD: a randomized clinical trial. Scand J Med Sci Sports 2019; 29:1243–1253. [DOI] [PubMed] [Google Scholar]
- 87.Smith SD, Vitulano LA, Katsovich L, et al. A randomized controlled trial of an integrated brain, body and social intervention for children with ADHD. J Atten Disord 2020; 24:780–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88▪.Wong HC, Zaman R. Neurostimulation in treating ADHD. Psychiatr Danub 2019; 31: Suppl 3: 265–275. [PubMed] [Google Scholar]; The systematic review summarizes the literature on neurostimulation for treating ADHD, including transcranial magnetic stimulation, transcranial direct current stimulation and vagus nerve stimulation, and there is preliminary evidence to support further good-quality studies on these approaches.
- 89.De Sousa BH, Caous CA, Lindsey CJ. Projections of the paratrigeminal nucleus to the ambiguus, rostroventrolateral and lateral reticular nuclei, and the solitary tract. Auton Neurosci 2001; 87:187e200. [DOI] [PubMed] [Google Scholar]
- 90.Cook IA, Espinoza R, Leuchter AF. Neuromodulation for depression: invasive and noninvasive (deep brain stimulation, transcranial magnetic stimulation, trigeminal nerve stimulation). Neurosurg Clin North Am 2014; 25:103–116. [DOI] [PubMed] [Google Scholar]
- 91.Voelker R. Trigeminal nerve stimulator for ADHD. JAMA 2019; 321:2066. [DOI] [PubMed] [Google Scholar]
- 92▪.McGough JJ, Sturm A, Cowen J, et al. Double-blind, sham-controlled, pilot study of trigeminal nerve stimulation for attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2019; 58:403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the first randomized controlled trial to demonstrate the efficacy of trigeminal nerve stimulation over a sham treatment.
- 93▪.García-Baos A, D’Amelio T, Oliveira I, et al. Novel interactive eye-tracking game for training attention in children with attention deficit/hyperactivity disorder. Prim Care Companion CNS Disord 2019; 21:19m02428. [DOI] [PubMed] [Google Scholar]; The small study showed that a novel game-based intervention utilizing eye tracker technology resulted in some benefit over a control condition.
- 94.Bluschke A, Schuster J, Roessner V, et al. Neurophysiological mechanisms of interval timing dissociate inattentive and combined ADHD subtypes. Sci Rep 2018; 8:2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wilson TW, Heinrichs-Graham E, White ML, et al. Estimating the passage of minutes: deviant oscillatory frontal activity in medicated and unmedicated ADHD. Neuropsychology 2013; 27:654–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hwang-Gu SL, Gau S. Interval timing deficits assessed by time reproduction dual tasks as cognitive endophenotypes for attention-deficit/hyperactivity disorder. PLoS One 2015; 10:e0127157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fontes RM, Marinho V, Carvalho V, et al. Time estimation exposure modifies cognitive aspects and cortical activity of attention deficit hyperactivity disorder adults. Int J Neurosci 2020. 1–16. doi: 10.1080/00207454.2020.1715394. [DOI] [PubMed] [Google Scholar]
- 98.Vahabzadeh A, Keshav NU, Salisbury JP, Sahin NT. Improvement of attention-deficit/hyperactivity disorder symptoms in school-aged children, adolescents, and young adults with autism via a digital smartglasses-based socioemotional coaching aid: short-term, uncontrolled pilot study. JMIR Ment Health 2018; 5:e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sluiter MN, Groen Y, de Jonge P, Tucha O. Exploring neuropsychological effects of a self-monitoring intervention for ADHD-symptoms in school. Appl Neuropsychol Child 2019; 9:246–258. [DOI] [PubMed] [Google Scholar]


