Objective:
A systematic review on the reproducibility of ambulatory blood pressure measurements (ABPM) has not yet been conducted. This meta-analysis compared 24-h/daytime/night-time SBP and DBP mean values and SBP/DBP nocturnal dipping status from ABPMs in participants with or without hypertension.
Methods:
Ovid MEDLINE, EMBASE, and CINAHL Complete databases were searched for articles published before 3 May 2019. Eligible studies reporting a 24-h ABPM repeated at least once within 1 month were included. The mean daytime/night-time/24-h BP values, percentage of nocturnal dipping, and proportion of nondippers were compared between the first and second day of measurements, and the proportion of participants with inconsistent dipping status were estimated using a random effect model.
Results:
Population-based analysis found a 0–1.1 mmHg difference between the first and second ABPM for 24-h/daytime/night-time SBP and DBP and 0–0.5% for percentage of SBP/DBP nocturnal dipping. The proportion of non-dippers was not different between the first and second ABPM. Intra-individual analysis found that the 95% limit of agreements (LOA) for SBP/DBP were wide and the 95% LOA for daytime SBP, common reference to diagnose hypertension, ranged −16.7 to 18.4 mmHg. Similarly, 32% of participants had inconsistent nocturnal dipping status.
Conclusion:
ABPM had excellent reproducibility at the population level, favouring its application for research purposes; but reproducibility of intra-individual BP values and dipping status from a 24-h ABPM was limited. The available evidence was limited by the lack of high-quality studies and lack of studies in non-Western populations.
Keywords: ambulatory blood pressure measurement, blood pressure, dipping, meta-analysis, reproducibility
INTRODUCTION
Hypertension is the most common chronic condition, contributing to physical complications and substantial burden to healthcare systems [1]. The diagnosis and management of hypertension depends heavily on accurate measurement of blood pressure (BP) [2]. Ambulatory BP measurements (ABPM) are now considered by virtually all international guidelines as the ‘gold standard’ of clinical BP measurement and ABPM has been shown to predict morbidity and mortality, even after controlling for office BP values [2–5]. Furthermore, certain BP parameters, including nocturnal BP values and nocturnal BP dipping (if BP decrease by more than 10% at night), carry prognostic significance and can only be detected clinically by ABPM [6,7]. The use of ABPM is increasingly common in research and in routine clinical management.
However, to date, a systematic review about the reproducibility of ABPM has yet to be conducted. Individual studies were small in size, used different ABPM machines, different intervals to repeat ABPM, different statistical analysis, and yielded different conclusions about the reproducibility of various ABPM parameters [8–14]. Reproducibility of results from a 24-h ABPM is clinically important as doctors need to be certain that BP values and diagnosis provided by ABPM is reliable; similarly, researchers need to know that any change in BP is because of interventions, rather than because of random fluctuations of BP values on ABPMs.
This systematic review and meta-analysis aimed to investigate and summarize the short-term reproducibility of 24-h/daytime/night-time SBP and DBP mean values and dipping status from 24-h ABPMs in participants with or without hypertension.
METHODS
Study selection and search strategies
The electronic databases Ovid MEDLINE, EMBASE, and CINAHL Complete were searched for articles published up until 3 May 2019. A combination of search terms was used including ‘ambulatory blood pressure monitoring’, ‘ABPM’, ‘24 hour’, ‘diurnal’, and ‘reproducibility’. Details of search strategy are listed in Appendix 1, Supplemental Digital Content.
To ensure literature saturation, the search also included published abstracts from major international conferences about hypertension, such as the European Society of Hypertension and the International Society of hypertension, which publish their conference abstracts in major journals. All titles and abstracts were inputted into Covidence (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org). Two independent reviewers (E.L./Y.B.) screened title, abstract and full text separately. Although a third reviewer was originally invited to resolve discrepancies, all conflicts were resolved with discussion between the two reviewers.
Inclusion and exclusion criteria
Studies were included if they were observational studies, in which a 24-h ABPM was repeated at least once; the majority of ABPM had to be repeated within 1 month, that is, the reported mean/median were within 4 weeks or 31 days or 1 month; studies that used ABPM consecutively (i.e. 48 h or more) were included if reproducibility data (e.g. mean BP values on different days) were reported; and results concerning reproducibility including mean BP values of two ABPMs and/or number of participants with dipping and non-dipping on two ABPMs were reported. Studies were excluded if: any interventions were used; they aimed to assess changes in BP because of a significant change in environment (e.g. before and after earthquake); they involved any children (aged less than 18 years); or studies involved participants who suffered from atrial fibrillation (ABPM was not validated in these patients), who were pregnant, who were receiving dialysis, who were diagnosed to have secondary hypertension, who were at acute phase of illness where BP might change rapidly (e.g. acute stroke). If the ABPM was repeated more than two times, data from the first 2 days of ABPM were used for meta-analysis. Abstracts were included if they were published in an international journal and if they satisfied the inclusion and exclusion criteria.
Clinical data extraction
The following data were extracted by two independent reviewers (E.L./B.Y.): year of publication; country where the research was conducted; number of participants who had repeated ABPM; percentage of male participants; percentage of participants with hypertension; percentage of participants on antihypertension medications; the model of ABPM used; the interval between the duplicated ABPM; frequency of ABPM BP measurement during daytime and night-time by the ABPM, reproducibility parameters including mean daytime/night-time/24-h BP values, mean percentage of nocturnal dipping, and the proportion and number of nondippers and dippers. The data were compared, and discrepancies were resolved by the two reviewers.
Quality assessment
There is no standard tool for quality assessment for reproducibility research [15]. The current review had only included studies that reported to have most ABPM repeated within 4-week duration and have excluded studies in which BP changes because of other environment factors were likely. Quality was, therefore, assessed according to the current European Society of Hypertension guidelines [16] and studies were graded as high quality only if: the ABPM was recommended for use by the European guideline or British Hypertension Society (http://dableducational.org/sphygmomanometers/recommended_cat.html OR https://bihsoc.org/bp-monitors/); the ABPM was conducted on a working day; the number of valid readings per ABPM was higher than the current recommendation, (i.e. at least 70% of total readings from a ABPM was valid OR at least 20 valid daytime reading and at least 7 valid night-time reading); no editing was done to results of ABPM or editing was considered reasonable by the two reviewers (E.L./B.Y.).
Statistical analysis
R 3.3.2 software (R Core Team, Vienna, Austria) and Stata software (version 15.0; StataCorp. 2017. Stata Statistical Software: Release 15. College Station, Texas, USA: StataCorp LLC.) were used for the main analysis. Firstly, pooled mean daytime/night-time/overall 24-h BP values, proportion of nondippers, and the percentage of nocturnal dipping were compared between the first and second day of measurements using the random effect model with Mantel–Haenszel weighting. The results were expressed in a forest plot with combined mean value with 95% confidence intervals (CI). Secondly, intra-individual reproducibility of BP values was estimated using Bland–Altman statistics. The method used in this meta-analysis was published previously [17]. Lastly, the meta-analysis of proportion of inconsistent dipping was performed using the random effect model by the metaprop comments in Stata. Publication bias was assessed by Egger's test and Funnel plots.
Subgroup analyses including ABPM devices used, frequency of BP measurements and if the studies included patients with hypertension were conducted for all analysis. For intra-individual variability and reproducibility of dipping fistatus, further subgroup analysis was performed if the study involved participants with higher BP variability (e.g. in patients with diabetes and renal impairment) and if the study involved participants taking antihypertension medications.
RESULTS
Search results
The PRISMA flow chart is shown in Fig. 1. We initially identified 5379 articles. After removing 1447 duplicate articles, 3932 studies were screened for titles and abstracts. Of these, 119 articles were reviewed in full text, 82 articles were further excluded, and 37 studies remained eligible. Of the remaining 37 articles, two studies were not included in the meta-analysis despite reporting of reproducibility of BP readings of ABPM as there were no extractable data. Gardener et al. (n = 17) reported the mean of BP readings only at baseline and that the coefficient of variation ranged from 2.3 4% for these BP readings [18]. Similarly, Trazzi et al. (n = 20) reported the mean of BP readings only at baseline and that the correlation of BP readings on ABPM on two different days was high (r ≥ 0.9) [19]. As a result, there were 35 articles constituting 4058 participants were included for the meta-analysis.
FIGURE 1.
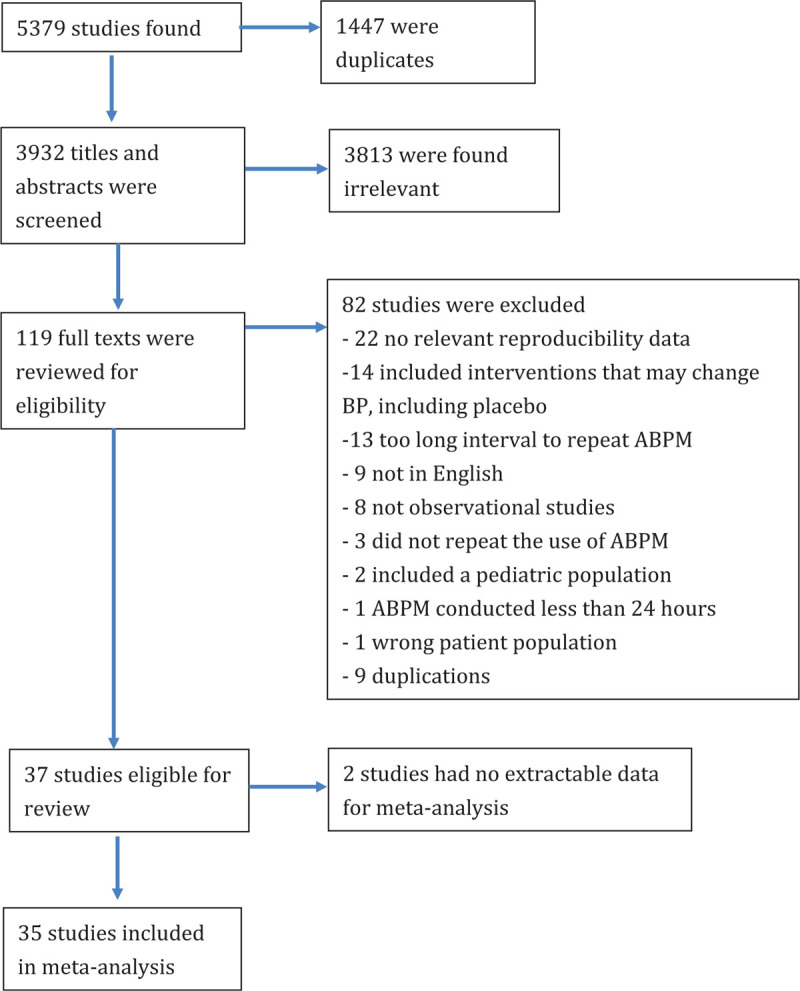
PRISMA diagram of included studies.
Characteristics of included studies
Details of included studies can be found in Appendix 2, Supplemental Digital Content. Most studies were small and only 37.14% (13 out of 35) had recruited over 100 patients (range 6–658). The age of participants ranged from around 22–104 years. Most studies (60%; 21 studies) involved patients with essential hypertension. However, only participants in only 10 studies (28.5%) received antihypertensive medications. Spacelab 90207 (Spacelabs Healthcare, Snoqualmie, Washington, USA) was the most commonly used ABPM machine (54.2%; 19 studies) and most studies defined night-time using fixed time method (45.7%; 16 studies) or using a diary (40%; 14 studies). Almost all studies were conducted in Western countries (including Italy, USA, Denmark, Netherlands, Spain, Finland, Australia, Russia, Greece, and Germany) and only 2 studies (5.7%) were conducted in Japan. Most studies measured BP every 15 min during the daytime and 20–30 min during the night-time.
Using our criteria to assess studies’ quality, only one study was classified as high quality [20] (Fig. 2). Although most studies used ABPM machines that were considered validated when this article was written, most did not report how the ABPM report was defined as valid or if editing was done to the ABPM report. As only one small study was classified as high quality (n = 32), subgroup analysis according to quality of studies was not conducted.
FIGURE 2.
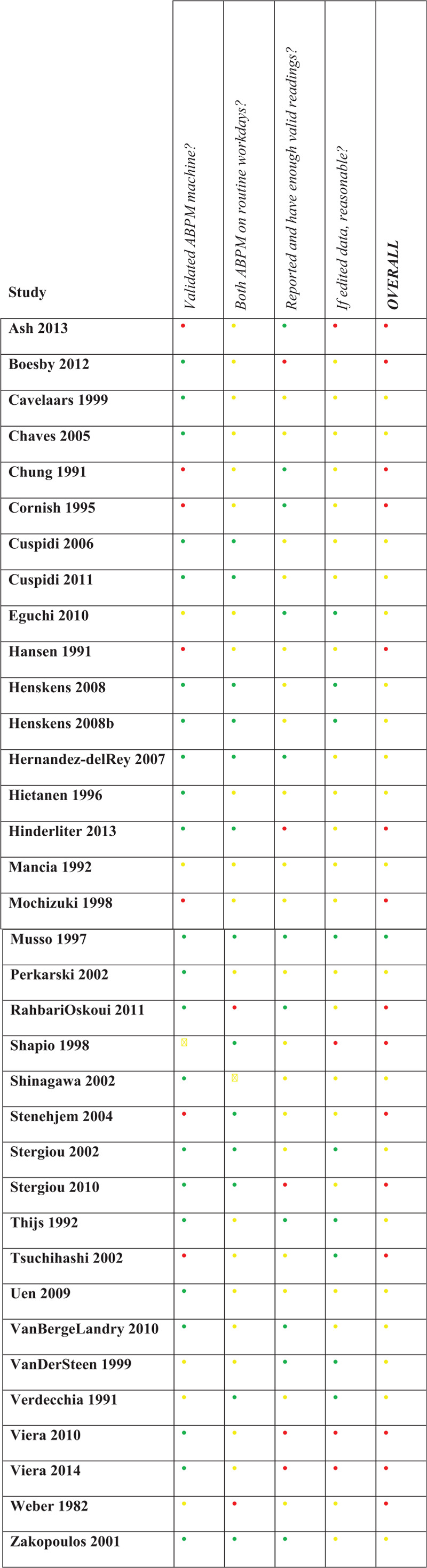
Quality assessment of included studies in the meta-analysis.
Results from meta-analyses
Population-based reproducibility of daytime, night-time, and 24-h overall blood pressure values
The mean difference of SBP values (first day value minus second day value) can be found in Fig. 3. SBP obtained on the first and second days was not different for 24-h SBP (0.71 mmHg; 95% CI: −0.08 to 1.51; I2 = 0%) (Fig. 3a). SBP was higher on the first day for daytime (1.01 mmHg; 95% CI: 0.37–1.64; I2 = 0%) (Fig. 3b) and night-time SBP (0.86 mmHg; 95% CI: 0.11–1.61; I2 = 0%) (Fig. 3c).
FIGURE 3.
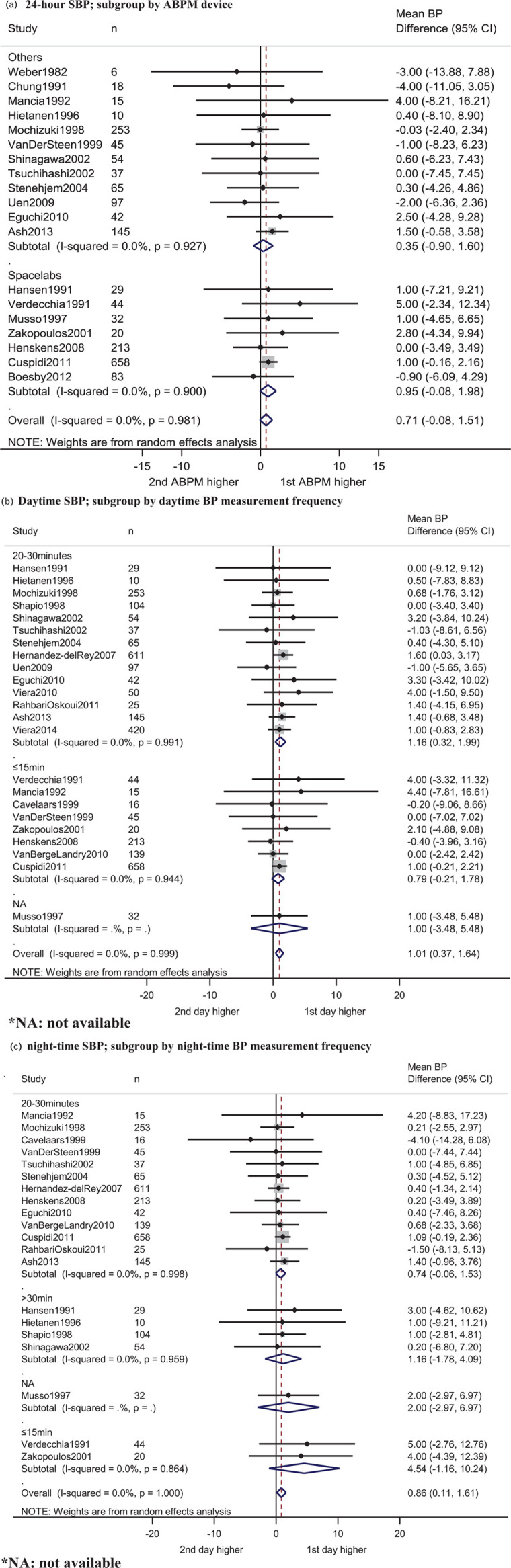
Meta-analysis of weighted mean SBP difference between the first ambulatory blood pressure measurement and second ambulatory blood pressure measurement by (a) 24-h, (b) daytime, (c) night-time measurements.
The MD of the DBP values (first day value minus second day value) can be found in Fig. 4. The DBP obtained on the first and second days were not different for the 24-h DBP (0.36 mmHg, 95% CI: −0.20 to 0.91; I2 = 0%) (Fig. 4a) and for night-time DBP (0.34 mmHg, 95% CI: −0.17to 0.85; I2 = 0%) (Fig. 4c). DBP was higher on the first day for daytime DBP (0.54 mmHg, 95% CI: 0.09–0.99; I2 = 0%) (Fig. 4b).
FIGURE 4.
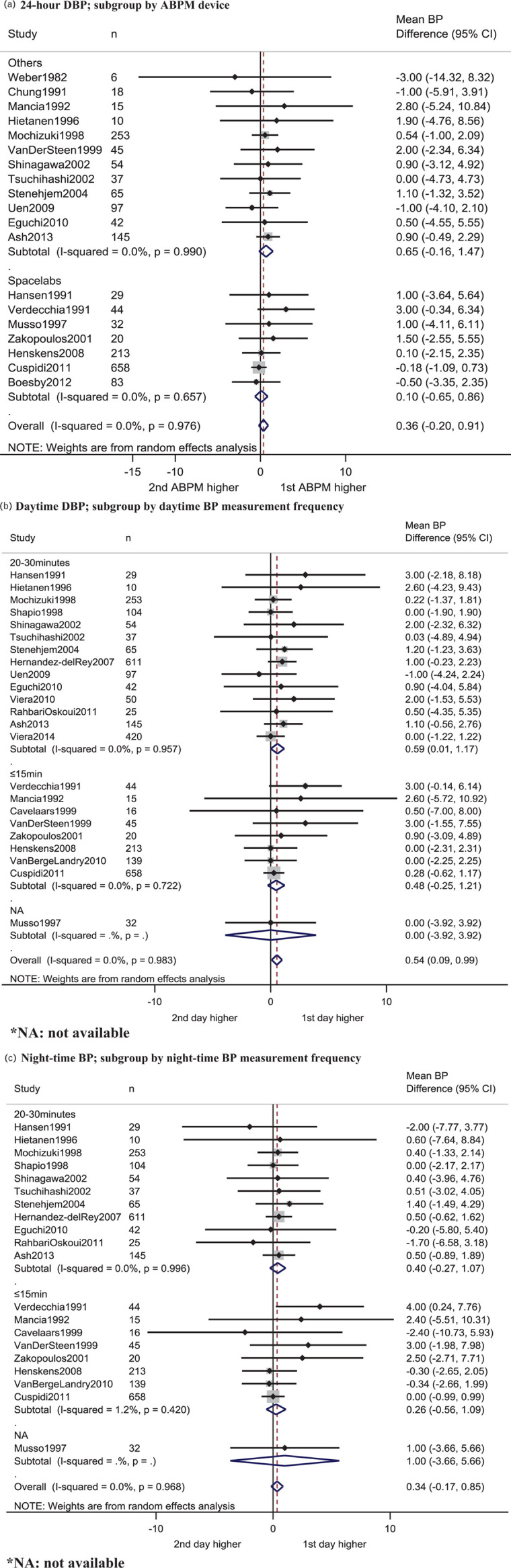
Meta-analysis of weighted mean DBP difference between first ambulatory blood pressure measurement and second ambulatory blood pressure measurement by (a) 24-h, (b) daytime, (c) night-time.
Subgroup analysis including the frequency of BP measurements, if hypertension and normotension participants were included, and the ABPM model used were conducted. Different subgroups did not show different results, despite the differences in daytime SBP/DBP values between the first and second day appeared to be higher if the BP was taken at 20–30 min intervals (see Figs. 3 and 4, Appendix 3, Supplemental Digital Content).
The “leave-one-out” sensitivity analysis suggested that no individual study significantly affected the pooled effect, which indicated that our results were statistically robust.
Intra-individual reproducibility using Bland–Altman statistics
Several studies used Bland–Altman statistics to describe intra-individual reproducibility and had provided enough data for meta-analysis [9,11,14,21–27,28]. The detailed meta-analysis results can be found in Appendix 4, Supplemental Digital Content. The overall 95% limit of agreements (LOA) were −14.2 to 14.7 mmHg for 24 h SBP, −9.3 to 10.2 mmHg for 24-h DBP, −16.7 to 18.4 mmHg for daytime SBP, −10.4 to 12.3 mmHg for daytime DBP, −19.6 to 21.3 mmHg for night-time SBP and −11.3 to 12.4 mmHg for night-time DBP.
Subgroup analysis was conducted. The width of 95% LOA was similar in different subgroups despite a wider LOA was generally observed for patients receiving antihypertensive drugs (except for 24-h DBP) and a narrower LOA was found for studies that only included normotensive participants (Appendix 4, Supplemental Digital Content). Two studies also included patients with possible higher BP variability, namely patients with diabetes [25] and patients with chronic kidney diseases [22]. However, subgroup analysis did not show a wider 95% LOA for these studies.
Reproducibility of dipping status
When analysed as a group, no difference was detected between the first and second ABPM for percentage of SBP nocturnal dipping −0.06%, 95% CI: −0.37 to 0.25; I2:0%) (Fig. 5a), and the prevalence of nondippers (Relative risk 0.97, 95% CI: 0.89–1.04, I2: 0%) (Fig. 5c). The percentage of DBP nocturnal dipping was slightly higher on the second ABPM than on the first ABPM (0.43%, 95% CI: −0.65 to −0.21; I2: 0%) (Fig. 5b). For the meta-analysis of the percentage of SBP/DBP dipping, an outliner was identified as the study by Chaves et al. [10] had very small standard deviation although the sample size was only comparable with other studies. When the analysis was conducted after this study was removed, the percentage of SBP/DBP nocturnal dipping was not different between the first and second ABPM (Appendix 5, Supplemental Digital Content).
FIGURE 5.
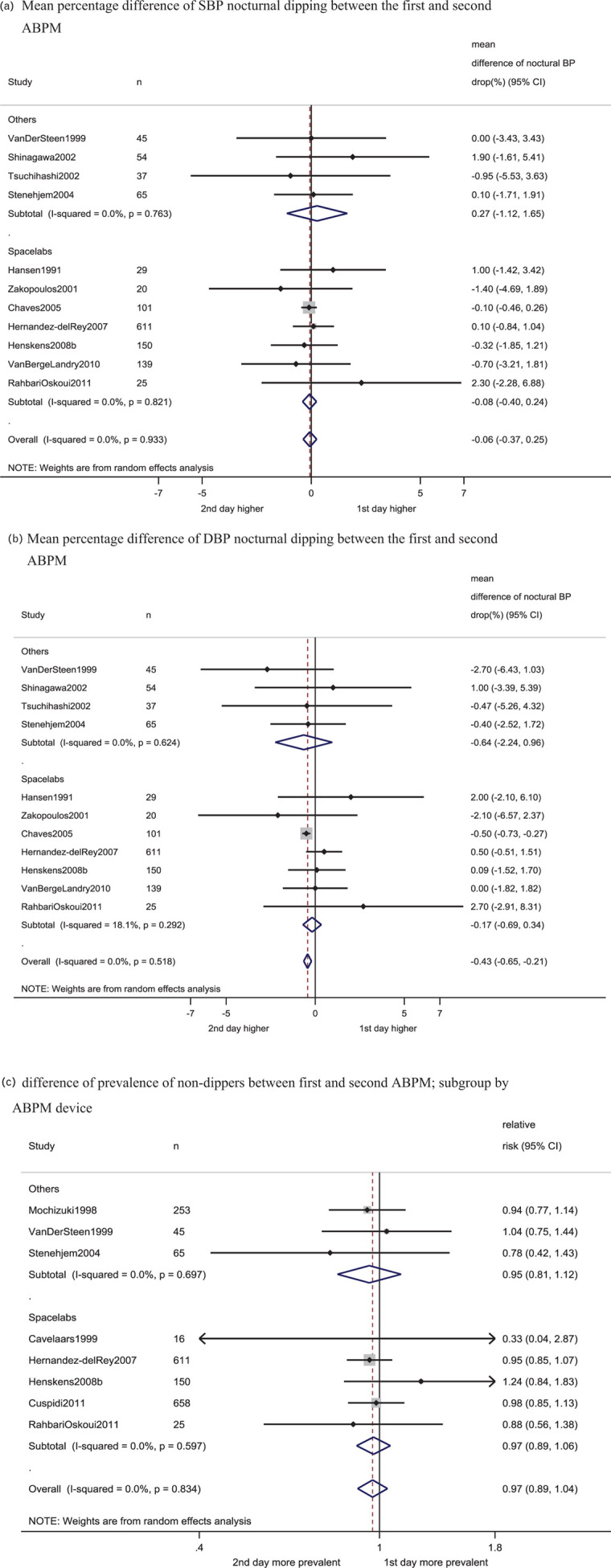
Meta-analysis comparing first and second ambulatory blood pressure measurement for (a) degree of SBP dipping (b) degree of DBP dipping and (c) prevalence of nondippers.
When analysed at an individual level, our meta-analysis found that 32% (95% CI: 26–38%; I2 = 89.04%) of participants had inconsistent dipping (i.e. changed from dipping to nondipping and vice versa on repeated ABPM) (Fig. 6). For studies using only SBP to define dipping, a higher proportion of participants had inconsistent dipping (42%; 95% CI: 15–68%, I2 = 96.15%) (Fig. 6a). Subgroup analysis was conducted for variables including: the ABPM machine model used, if the study included patients with higher BP variability (these studies included patients with kidney disease [22,29], diabetes mellitus [30], resistant hypertension [31], and stroke [32]), if participants were on hypertension drugs, different definition of night-time, different frequency of measurements (Appendix 6, Supplemental Digital Content). The “leave-one-out” sensitivity analysis found that, by removing the study by Tsuchihashi et al. [32], which had a high proportion of inconsistent dipper values, the proportion of patients in studies that defined dipping by SBP only had a similar proportion of inconsistent dippers with other groups (27%; 95% CI: 23–30%; I2: 57.32%) (Appendix 7, Supplemental Digital Content). As one study defined dipping using ‘SBP only’, ‘SBP or DBP’ and ‘SBP and DBP’, sensitivity analysis was conducted using these different data but showed similar results (after the outlier Tsuchihashi et al. 2002 was removed) [33].
FIGURE 6.
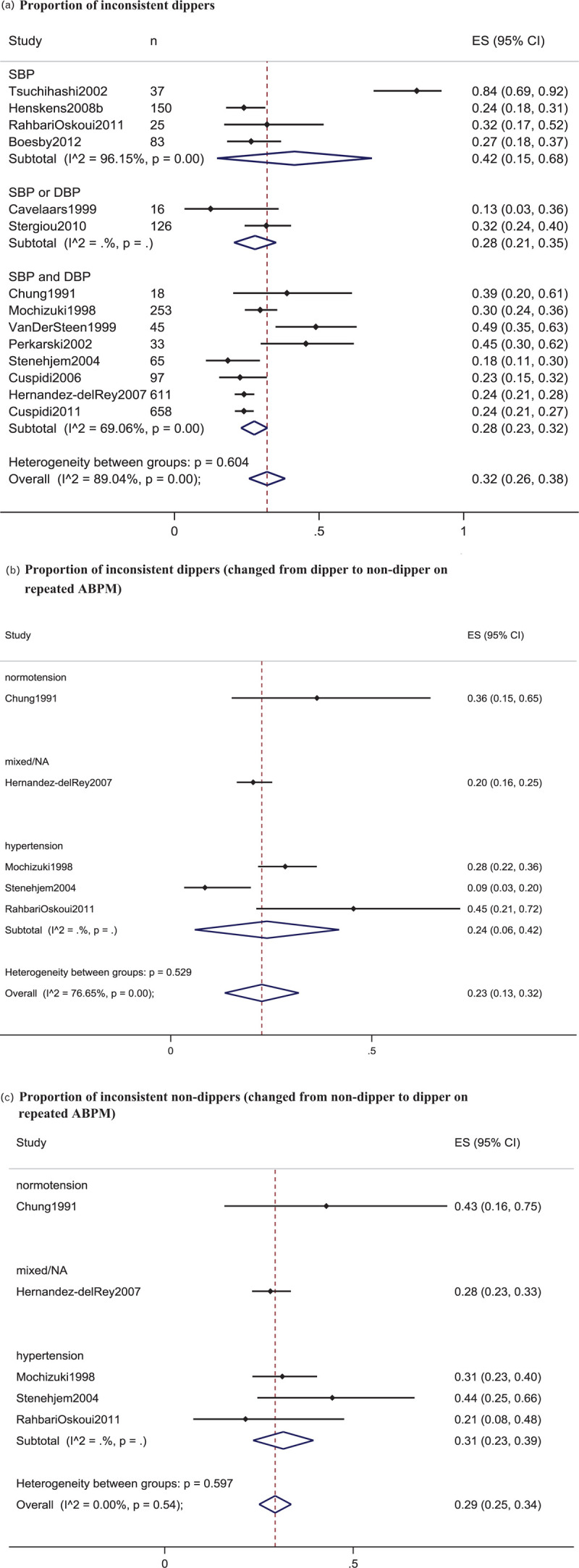
Meta-analysis of proportion of participants with (a) inconsistent dipping status, subgroup by the definition of dipping by the authors, (b) proportion of patients with inconsistent dipping (dipping on the first day but nondipping on second day), (c) proportion of patients with inconsistent nondipping (nondipping on the first day but dipping on second day).
Similarly, 23% of participants changed from dipper to nondipper on repeated ABPM (95% CI: 13–32%; I2: 76.65%), 29% of participants changed from nondipper to dipper on repeated ABPM (95% CI: 25–34%; I2 = 0%).
Publication bias
Egger test and funnel plots showed no evidence of significant small study bias (t = −0.87, P = 0.396 for 24 h SBP; t = 0.19, P = 0.848 for daytime SBP; t = 0.27, P = 0.792 for night-time SBP; t = 1.34, P = 0.198 for 24 h DBP; t = 1.72, P = 0.091 for daytime DBP; t = 0.80, P = 0.434 for night-time DBP) (Appendix 8, Supplemental Digital Content).
DISCUSSION
To the authors’ best knowledge, this is the first systematic review and meta-analysis that investigated the population-based and intra-individual reproducibility of ABPM and found that ABPM had excellent reproducibility at the population level, but that the intra-individual reproducibility of ABPM results, in terms of mean SBP/DBP values and dipping status, were limited. At the population level, the results were homogeneous with I2 at 0%, indicating that our results were robust. Our analysis also found that there was no significant small study bias.
The current study provided evidence that ABPM is an excellent outcome measure for BP research as ABPM had excellent reproducibility at the population level. Although our results indicated that the BP mean values dropped by 0.5–1 mmHg on repeated ABPM, this is likely to be clinically insignificant and can hardly impact on research findings; similarly, the percentage of nocturnal drop and proportion of nondipper were highly reproducible on ABPM. Conversely, another commonly used outcome measure, office BP measurements, had higher variability in interventional trials on repeated measurements than ABPM [34]; and it was reported that SBP could drop more than 10 mmHg without intervention on repeated office BP measurements [35]. Recently, two published meta-analyses reported that a newer office BP measurement method, called the automated office BP measurement (AOBP), could provide similar mean SBP readings to daytime ABPM [15,36]. However, more data is needed to confirm if AOBP can be as reproducible as ABPM.
In contrast, the intra-individual reproducibility of mean BP values was poor. The 95% LOA between two measurements for daytime SBP, which is often used for diagnosis of hypertension, ranged from −16.7 to 18.4 mmHg. This could impact on diagnosing in patients with hypertension or suboptimal BP control.
Clinicians can use our results as reference to decide if repeated ABPM is needed for their patients. Similarly, given the high number of studies comparing different BP measurement methods (e.g. home BP measurement to ABPM) [37]; when interpreting these results, the results of current study can provide an important reference for comparison. Our results showed that, in individual participant, night-time BP was less reproducible. The exact reasons were not known. However, BP is known to be a volatile parameter and is affected by a number of factors, such as season [38], temperature [38], emotional state [39], and exercise level [40]. At night, BP is also known to be affected by sleep quality [41], which can be affected by frequent measurements of BP during sleep [42]. Although ABPM may have better reproducibility in participants with normotension and the LOA was narrower (95% LOA: daytime SBP ranged −8.5 to 5.7 mmHg), these results were reported in only two studies.
Similarly, despite studies having consistently shown that nondipping was associated with increased mortality and end-organ damage [6,43], this study confirmed that intra-individual classification of dippers and nondippers were unstable and around one quarter to one-third of participants had their dipping status changed on repeated measurements. The current study also showed that dipping status was more likely to change in nondippers than dippers on the initial ABPM. More research is needed to delineate, which individuals may be more likely to have unstable dipping status or poor intra-individual mean BP reproducibility on ABPM; similarly, it is unclear how reproducibility of dipping status on ABPM can be enhanced.
A strength of the current study is the extensive literature search. However, several limitations should be discussed. Firstly, as the team of reviewers could only read Chinese and English, the literature search was limited to these two languages. Nonetheless, we extracted data from available abstracts, thus any non-Chinese or non-English literature was included if their abstracts were published in English and if the abstract provided enough data for extraction. Secondly, only one relatively small study was classified as high quality. As no widely used relevant quality assessment tools existed, our team developed a quality assessment tool that included criteria that could reflect that the ABPM was conducted properly. Rather than be conducted improperly, these studies may have been omitted as there was no commonly used reporting format or checklist. Furthermore, most studies were conducted in western countries, the extent that these results could be applied to other populations (e.g. Chinese) is not known and more research in various ethnicities is needed.
In conclusion, our study found that ABPM is an excellent outcome measure for BP research, because of its excellent population-based reproducibility; but ABPM's intra-individual reproducibility of BP values and dipping status in patients with or without hypertension was limited.
ACKNOWLEDGEMENTS
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: ABPM, ambulatory blood pressure measurement; AOBP, automated office blood pressure measurement; BP, blood pressure; CI, confidence interval; LOA, limit of agreement; MD, mean difference
REFERENCES
- 1.Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA 2017; 317:165–182. [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Clinical Excellence. Hypertension in adults: diagnosis and management. London:National Institute for Health and Care Excellence (UK); 2019. [Google Scholar]
- 3.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018; 36:1953–2041. [DOI] [PubMed] [Google Scholar]
- 4. Hypertension Canada Guidelines [Internet]. Available at: https://guidelines.hypertension.ca/ [Accessed 7 April 2020]. [Google Scholar]
- 5.Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, et al. DACO Investigators Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7030 individuals. J Hypertens 2007; 25:1554–1564. [DOI] [PubMed] [Google Scholar]
- 6.Cuspidi C, Sala C, Tadic M, Rescaldani M, Grassi G, Mancia G. Nondipping pattern and subclinical cardiac damage in untreated hypertension: a systematic review and meta-analysis of echocardiographic studies. Am J Hypertens 2015; 28:1392–1402. [DOI] [PubMed] [Google Scholar]
- 7.Fan HQ, Li Y, Thijs L, Hansen TW, Boggia J, Kikuya M, et al. International Database on Ambulatory Blood Pressure In Relation to Cardiovascular Outcomes Investigators Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens 2010; 28:2036–2045. [DOI] [PubMed] [Google Scholar]
- 8.Abdalla M, Goldsmith J, Muntner P, Diaz KM, Reynolds K, Schwartz JE, Shimbo D. Is isolated nocturnal hypertension a reproducible phenotype? Am J Hypertens 2016; 29:33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ash G, Walker T, Olson K, Stratton J, Gómez A, Kraemer W, et al. Reproducibility of ambulatory blood pressure changes from the initial values on two different days. Clinics (Sao Paulo) 2013; 68:1509–1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaves H, Campello De Souza FM, Krieger EM. The reproducibility of dipping status: beyond the cutoff points. Blood Press Monit 2005; 10:201–205. [DOI] [PubMed] [Google Scholar]
- 11.Eguchi K, Hoshide S, Hoshide Y, Ishikawa S, Shimada K, Kario K. Reproducibility of ambulatory blood pressure in treated and untreated hypertensive patients. J Hypertens 2010; 28:918–924. [DOI] [PubMed] [Google Scholar]
- 12.Roas S, Sudano I, Ruschitzka F, Lüscher TF, Noll G. Reproducibility of ambulatory blood pressure measurement in patients with coronary heart disease. Cardiovasc Med 2014; 17:221–227. [Google Scholar]
- 13.Keren S, Leibowitz A, Grossman E, Sharabi Y. Limited reproducibility of 24-h ambulatory blood pressure monitoring. Clin Exp Hypertens 2015; 37:599–603. [DOI] [PubMed] [Google Scholar]
- 14.van der Steen MS, Lenders JW, Graafsma SJ, Den AJ, Thien T. Reproducibility of ambulatory blood pressure monitoring in daily practice. J Hum Hypertens 1999; 13:303–308. [DOI] [PubMed] [Google Scholar]
- 15.Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis. JAMA Intern Med 2019; 179:351–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013; 31:1731–1768. [DOI] [PubMed] [Google Scholar]
- 17.Williamson PR, Lancaster GA, Craig JV, Smyth RL. Meta-analysis of method comparison studies. Stat Med 2002; 21:2013–2025. [DOI] [PubMed] [Google Scholar]
- 18.Gardner JP, Cho JH, Skurnick JH, Awad G, Gutkin M, Byrd LH, et al. Blood pressure inversely correlates with thrombin-evoked calcium rise in platelets. Hypertension 1994; 23 (6 Pt 1):703–709. [DOI] [PubMed] [Google Scholar]
- 19.Trazzi S, Mutti E, Frattola A, Imholz B, Parati G, Mancia G. Reproducibility of non-invasive and intra-arterial blood pressure monitoring: implications for studies on antihypertensive treatment. J Hypertens 1991; 9:115–119. [DOI] [PubMed] [Google Scholar]
- 20.Musso N, Vergassola C, Barone C, Lotti G. Ambulatory blood pressure monitoring: how reproducible is it? Am J Hypertens 1997; 10:936–939. [DOI] [PubMed] [Google Scholar]
- 21.Uen S, Fimmers R, Brieger M, Nickenig G, Mengden T. Reproducibility of wrist home blood pressure measurement with position sensor and automatic data storage. BMC Cardiovasc Disord 9:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verdecchia P, Schillaci G, Boldrini F, Guerrieri M, Zampi I, Porcellati C. Quantitative assessment of day-to-day spontaneous variability in non-invasive ambulatory blood pressure measurements in essential hypertension. J Hypertens 1991; 9:S322–S323. [PubMed] [Google Scholar]
- 23.Boesby L, Thijs L, Elung-Jensen T, Strandgaard S, Kamper AL. Ambulatory arterial stiffness index in chronic kidney disease stage 2-5. Reproducibility and relationship with pulse wave parameters and kidney function. Scand J Clin Lab Invest 2012; 72:304–312. [DOI] [PubMed] [Google Scholar]
- 24.Cavelaars M, Tulen JHM, Man’t Veld AJ, Gelsema ES, Van den Meiracker AH. Assessment of body position to quantify its effect on nocturnal blood pressure under ambulatory conditions. J Hypertens 2000; 18:1737–1743. [DOI] [PubMed] [Google Scholar]
- 25.Wong Chung MY, Smits P, Lenders JWM, Thien T. Reproducibility of the blood pressure fall at night in healthy normotensive volunteers. J Hypertens 1991; 9:S234–S235. [PubMed] [Google Scholar]
- 26.Hansen KW, Schmitz A, Pedersen MM. Ambulatory blood pressure measurement in type 2 diabetic patients: methodological aspects. Diabet Med 1991; 8:567–572. [DOI] [PubMed] [Google Scholar]
- 27.Henskens LHG, Van Oostenbrugge RJ, Kroon AA, De Leeuw PW, Lodder J. Brain microbleeds are associated with ambulatory blood pressure levels in a hypertensive population. Hypertension 2008; 51:62–68. [DOI] [PubMed] [Google Scholar]
- 28.Stenehjem AE, Os I. Reproducibility of blood pressure variability, white-coat effect and dipping pattern in untreated, uncomplicated and newly diagnosed essential hypertension. Blood Press 2004; 13:214–224. [DOI] [PubMed] [Google Scholar]
- 29.Rahbari-Oskoui FF, Miskulin DC, Hogan MC, Fielder O, Torres VE, et al. Short-term reproducibility of ambulatory blood pressure monitoring in autosomal dominant polycystic kidney disease. Blood Press Monit 2011; 16:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cuspidi C, Meani S, Lonati L, Fusi V, Valerio C, Sala C, et al. Short-term reproducibility of a non-dipping pattern in type 2 diabetic hypertensive patients. J Hypertens 2006; 24:647–653. [DOI] [PubMed] [Google Scholar]
- 31.Hernández-del Rey R, Martin-Baranera M, Sobrino J, Gorostidi M, Vinyoles E, Sierra C, et al. Spanish Society of Hypertension Ambulatory Blood Pressure Monitoring Registry Investigators Reproducibility of the circadian blood pressure pattern in 24-h versus 48-h recordings: the Spanish Ambulatory Blood Pressure Monitoring Registry. J Hypertens 2007; 25:2406–2412. [DOI] [PubMed] [Google Scholar]
- 32.Tsuchihashi T, Kawakami Y, Imamura T, Abe I. Reproducibility of blood pressure variation in older ambulatory and bedridden subjects. J Am Geriatr Soc 2002; 50:1069–1074. [DOI] [PubMed] [Google Scholar]
- 33.Henskens LH, Kroon AA, Van Oostenbrugge RJ, Haest RJ, Lodder J, de Leeuw PW. Different classifications of nocturnal blood pressure dipping affect the prevalence of dippers and nondippers and the relation with target-organ damage. J Hypertens 2008; 26:691–698. [DOI] [PubMed] [Google Scholar]
- 34.Warren RE, Marshall T, Padfield PL, Chrubasik S. Variability of office, 24-hour ambulatory, and self-monitored blood pressure measurements. Br J Gen Pract 2010; 60:675–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hartley RM, Velez R, Morris RW, D'Souza MF, Heller RF. Confirming the diagnosis of mild hypertension. Br Med J (Clin Res Ed) 1983; 286:287–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pappaccogli M, Di Monaco S, Perlo E, Burrello J, D’Ascenzo F, Veglio F, et al. Comparison of automated office blood pressure with office and out-off-office measurement techniques. Hypertension 2019; 73:481–490. [DOI] [PubMed] [Google Scholar]
- 37.Filipovský J, Seidlerová J, Kratochvíl Z, Karnosová P, Hronová M, Mayer O., Jr Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press 2016; 25:228–234. [DOI] [PubMed] [Google Scholar]
- 38.Modesti PA. Season, temperature and blood pressure: a complex interaction. Eur J Intern Med 2013; 24:604–607. [DOI] [PubMed] [Google Scholar]
- 39.Bruehl S, Carlson CR, McCubbin JA. The relationship between pain sensitivity and blood pressure in normotensives. Pain 1992; 48:463–467. [DOI] [PubMed] [Google Scholar]
- 40.Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc 2013; 2:e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bowman MA, Buysse DJ, Foust JE, Oyefusi V, Hall MH. Disturbed sleep as a mechanism of race differences in nocturnal blood pressure non-dipping. Curr Hypertens Rep 2019; 21:51. [DOI] [PubMed] [Google Scholar]
- 42.Hamdani G, Flynn JT, Daniels S, Falkner B, Hanevold C, Ingelfinger J, et al. Ambulatory blood pressure monitoring tolerability and blood pressure status in adolescents: The SHIP AHOY study. Blood Press Monit 2019; 24:12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cicek Y, Durakoglugil ME, Kocaman SA, Cetin M, Erdogan T, Dogan S, et al. Non-dipping pattern in untreated hypertensive patients is related to increased pulse wave velocity independent of raised nocturnal blood pressure. Blood Press 2013; 22:34–38. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


