Abstract
Background
In the United States, non-Hispanic Black (NHB), Hispanic, and non-Hispanic American Indian/Alaska Native (NHAIAN) populations experience excess COVID-19 mortality, compared to the non-Hispanic White (NHW) population, but racial/ethnic differences in age at death are not known. The release of national COVID-19 death data by racial/ethnic group now permits analysis of age-specific mortality rates for these groups and the non-Hispanic Asian or Pacific Islander (NHAPI) population. Our objectives were to examine variation in age-specific COVID-19 mortality rates by racial/ethnicity and to calculate the impact of this mortality using years of potential life lost (YPLL).
Methods and findings
This cross-sectional study used the recently publicly available data on US COVID-19 deaths with reported race/ethnicity, for the time period February 1, 2020, to July 22, 2020. Population data were drawn from the US Census. As of July 22, 2020, the number of COVID-19 deaths equaled 68,377 for NHW, 29,476 for NHB, 23,256 for Hispanic, 1,143 for NHAIAN, and 6,468 for NHAPI populations; the corresponding population sizes were 186.4 million, 40.6 million, 2.6 million, 19.5 million, and 57.7 million. Age-standardized rate ratios relative to NHW were 3.6 (95% CI 3.5, 3.8; p < 0.001) for NHB, 2.8 (95% CI 2.7, 3.0; p < 0.001) for Hispanic, 2.2 (95% CI 1.8, 2.6; p < 0.001) for NHAIAN, and 1.6 (95% CI 1.4, 1.7; p < 0.001) for NHAP populations. By contrast, NHB rate ratios relative to NHW were 7.1 (95% CI 5.8, 8.7; p < 0.001) for persons aged 25–34 years, 9.0 (95% CI 7.9, 10.2; p < 0.001) for persons aged 35–44 years, and 7.4 (95% CI 6.9, 7.9; p < 0.001) for persons aged 45–54 years. Even at older ages, NHB rate ratios were between 2.0 and 5.7. Similarly, rate ratios for the Hispanic versus NHW population were 7.0 (95% CI 5.8, 8.7; p < 0.001), 8.8 (95% CI 7.8, 9.9; p < 0.001), and 7.0 (95% CI 6.6, 7.5; p < 0.001) for the corresponding age strata above, with remaining rate ratios ranging from 1.4 to 5.0. Rate ratios for NHAIAN were similarly high through age 74 years. Among NHAPI persons, rate ratios ranged from 2.0 to 2.8 for persons aged 25–74 years and were 1.6 and 1.2 for persons aged 75–84 and 85+ years, respectively. As a consequence, more YPLL before age 65 were experienced by the NHB and Hispanic populations than the NHW population—despite the fact that the NHW population is larger—with a ratio of 4.6:1 and 3.2:1, respectively, for NHB and Hispanic persons. Study limitations include likely lag time in receipt of completed death certificates received by the Centers for Disease Control and Prevention for transmission to NCHS, with consequent lag in capturing the total number of deaths compared to data reported on state dashboards.
Conclusions
In this study, we observed racial variation in age-specific mortality rates not fully captured with examination of age-standardized rates alone. These findings suggest the importance of examining age-specific mortality rates and underscores how age standardization can obscure extreme variations within age strata. To avoid overlooking such variation, data that permit age-specific analyses should be routinely publicly available.
Mary Bassett and colleagues anzlyze US data on COVID-19 deaths to determine if, in addition to dying at higher rates, racial and ethnic minorities are also dying at younger ages.
Author summary
Why was this study done?
Data from media coverage and local health department reports suggest that, as compared to the non-Hispanic White population, COVID-19 mortality rates are substantially higher among non-Hispanic Black, Hispanic, and non-Hispanic American Indian or Alaska Native populations.
But no national data have been available to determine whether, in addition to dying at higher rates, these groups also die at younger ages.
What did the researchers do and find?
Using recently released national data on COVID-19 deaths by racial/ethnic group and age, along with US Census population data, we explored variation in mortality risk by calculating age-specific mortality measures in the above groups as well as in the non-Hispanic Asian or Pacific Islander population, the 5 census-defined groups for which data are available.
We found that for all groups, as compared to the non-Hispanic White population, there were excess COVID-19 deaths across all ages. Although for all racial/ethnic groups, most deaths occurred at older ages, there was also striking loss of life at younger ages, before age 65, among people of color.
More years of life were lost before 65 years among the non-Hispanic Black and Hispanic populations, despite the smaller size of these groups, than among the non-Hispanic White population. Scrutinizing age-specific mortality rates, we found that for young adults into midlife, comparatively, the non-Hispanic Black, Hispanic, and non-Hispanic American Indian or Alaska Native populations had a much higher risk of death from COVID-19 than the non-Hispanic White population.
What do these findings mean?
These data support the conclusion that US populations of color die of COVID-19 at younger ages as well as at higher rates than the non-Hispanic White population.
Enhancing protection from infection, including assurance of workplace protections, may be relevant to prevention of COVID-19 in working-age adults.
Introduction
The first death due to COVID-19 in the United States was reported on February 29, 2020. In late March, media reports brought to national attention the disproportionate number of COVID-19 cases and deaths occurring among the US Black and Latino populations [1]. Typically, these reports compared the proportion of cases and deaths by reported race/ethnicity to the racial/ethnic composition of the population. For example, a news report noted on March 27 that all (100%) of 8 deaths in Milwaukee were among Black Americans, who comprised 38% of the city’s population; in all of Wisconsin, only 15 deaths statewide had occurred [2]. Such reports came from state and local jurisdictions. At the time, the Centers for Disease Control and Prevention (CDC) made COVID-19 data publicly available only by age and sex, prompting many calls to release racial/ethnic data [3]. On April 6, New York City first released both crude and age-adjusted COVID-19 mortality rates, permitting some insight into the impact of population age structure and age at death on race/ethnicity-specific mortality rates [4]. Estimates of US national racial/ethnic mortality rate disparities, produced in mid-May, used indirect age standardization to compare rates, to address concerns about differences in population age structures [5]. Also suggesting that information on age-specific risks could be important, marked racial/ethnic inequities in premature morbidity and mortality are well documented for numerous health outcomes, reflecting inequities in working and living conditions [6–8]. Journalists additionally have become a critical source of data highlighting how COVID-19 racial/ethnic disparities have become ubiquitous [9].
Data released by the National Center for Health Statistics (NCHS) [10], initially in mid-May and recently updated to July 22, 2020, make it possible for the first time to explore with national data, using federally classified racial/ethnic groups, the likelihood that the Black, Hispanic, American Indian or Alaska Native, and Asian or Pacific Islander populations, in addition to experiencing higher COVID-19 mortality rates than the non-Hispanic White population, are also dying at younger ages.
Methods
Study population and data sources
The analytic plan, designed before data were reviewed or analyses began, was to quantify the age-specific COVID-19 mortality rates and to determine the magnitude of racial/ethnic disparities, in both relative and absolute terms. We did not create a formally documented analysis plan, but our a priori hypothesis was that these magnitudes would vary by age and that the relative magnitude would be greater at younger ages. In addition to computing rate ratios and rate differences, we also planned in advance to quantify the impact of COVID-19 mortality in relation to years of potential life lost (YPLL), using YPLL 65 and YPLL 75 (as a sensitivity analysis), and to quantify the racial/ethnic inequities in COVID-19 mortality rates using mortality risk ratios, risk differences, and premature mortality rates. The YPLL 75 analyses were included in the primary text at the request of reviewers.
These data were provided by the NCHS (https://data.cdc.gov). This analysis was based on data from https://data.cdc.gov/NCHS/Deaths-involvingcoronavirus-disease-2019-COVID-19/ks3g-spdg, accessed on July 22, 2020 [10], used rather than the data posted by the CDC COVID Data Tracker [11]. The NCHS data file includes death counts from New York City, a major initial hotspot for COVID-19, which is excluded in the CDC COVID Data Tracker, and also provides the data jointly (rather than separately) by race and ethnicity (Hispanic or not). Analysis of racial/ethnic groups was limited by the availability of denominator data in CDC WONDER [12] to non-Hispanic White (NHW), non-Hispanic Black (NHB), non-Hispanic American Indian or Alaska Native (NHAIAN), non-Hispanic Asian or Pacific Islander (NHAPI), and Hispanic. Only 0.9% of the NCHS COVID-19 deaths had missing data on race/ethnicity. Both the mortality data [10] and the denominator data [12] are publicly available de-identified datasets, and the data we used for our analyses are fully and freely available from the cited websites. Because this study used publicly available, nationally aggregated, de-identified mortality data, IRB review was not required.
Population data were the Vintage 2019 population estimates [12]. This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline (See S1 STROBE Checklist).
Mortality rates, rate ratios, and rate differences
We calculated rates for 100,000 person-years by dividing deaths by the person-time from February 1 (the “Start Week” listed in the CDC data file) to July 22 (the “Data as of” field in the data file). This permits comparison of the age-specific and age-standardized rates to published mortality rates for common causes of death in previous years. We age-standardized to the Year 2000 standard million (used by the NCHS since 1999) and computed age-standardized rates, rate ratios, rate differences, and their confidence intervals using standard methods [13,14]. The methodology for computing directly age-standardized rates uses the following formula [14,15]:
This approach weights the age-specific death rates (ri) by the US standard population age distribution (using 11 age categories: <1, 1–4, 5–14, …, 75–84, 85+ years), where wi is the standard population for age group.
As an additional simple summary metric to quantify differential premature mortality risk [16,17], we calculated the age-standardized premature mortality rates, using age 65 and age 75 as cut points.
YPLL and YPLL rates
To capture the population impact of premature death, we computed YPLL. This measure is calculated by multiplying the number of deaths in each age category by the number of years from the midpoint of the age category to a selected age cutoff, and summing over age (pp. 159–160 of [10]). The selection of any age cut point is arbitrary. Our goal was to capture years of life lost prematurely due to COVID-19, because we hypothesized that racial disparities for deaths at younger ages were especially marked. We used a cut point of 65 years because deaths before age 65 occur among people who are generally considered of working age and who are also more likely to leave dependent children than older adults. Additionally, 65 years corresponds to eligibility for Medicare and Social Security. To explore how robust our findings were using this cut point, we also examined a cut point of 75 years.
Because YPLL is sensitive to the size of the population and differences in the age distribution for racial/ethnic groups, we also computed the age-standardized YPLL rate per 100,000 persons by computing age-specific YPLL rates and then taking a weighted sum, with the weights coming from the Year 2000 standard million [16].
Results
As of July 22, 2020, the number of COVID-19 deaths equaled 68,377 for NHW, 29,476 for NHB, 23,256 for Hispanic, 1,143 for NHAIAN, and 6,468 for NHAPI populations; the corresponding population sizes were 186.4 million, 40.6 million, 57.7 million, 2.6 million, and 19.5 million. (See S1 Table). For all racial/ethnic groups, the larger share of deaths occurred at older ages, although this proportion varies. For example, 10% of NHW deaths occurred before age 65 and 27% before age 75. In contrast, 28% and 54% of NHB deaths were before age 65 and age 75, respectively (See Table 1). Corresponding proportions for other groups are as follows: 37% and 61% for Hispanic, 45% and 69% for NHAIAN, and 23% and 49% for NHAPI.
Table 1. Crude, age-specific, and age-standardized COVID-19 mortality rates per 100,000 person-years for non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic American Indian or Alaska Native, and non-Hispanic Asian or Pacific Islander populations, and age-specific mortality rate ratios and rate differences per 100,000 person-years.
| Population | Deaths | Percent of deaths | Population | Percent of population | Age-specific mortality rate per 100,000 person-years (95% CI) | Rate ratio (95% CI) | p-Value | Rate difference per 100,000 person-years (95% CI) | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White | |||||||||
| Under 1 year | 3 | 0.0% | 1,994,440 | 1.1% | 0.3 (0.1, 0.8) | 1.0 (reference) | 0.0 (reference) | ||
| 1–4 years | 3 | 0.0% | 8,244,087 | 4.4% | 0.1 (0.0, 0.2) | 1.0 (reference) | 0.0 (reference) | ||
| 5–14 years | 2 | 0.0% | 21,483,759 | 11.5% | 0.0 (0.0, 0.1) | 1.0 (reference) | 0.0 (reference) | ||
| 15–24 years | 31 | 0.0% | 23,544,616 | 12.6% | 0.3 (0.2, 0.4) | 1.0 (reference) | 0.0 (reference) | ||
| 25–34 years | 151 | 0.2% | 25,657,465 | 13.8% | 1.2 (1.1, 1.4) | 1.0 (reference) | 0.0 (reference) | ||
| 35–44 years | 353 | 0.5% | 23,709,326 | 12.7% | 3.2 (2.8, 3.5) | 1.0 (reference) | 0.0 (reference) | ||
| 45–54 years | 1,366 | 2.0% | 26,232,985 | 14.1% | 11.1 (10.5, 11.6) | 1.0 (reference) | 0.0 (reference) | ||
| 55–64 years | 4,998 | 7.3% | 15,189,511 | 8.1% | 69.9 (67.9, 71.8) | 1.0 (reference) | 0.0 (reference) | ||
| 65–74 years | 11,746 | 17.2% | 23,091,706 | 12.4% | 108.0 (106.1, 110.0) | 1.0 (reference) | 0.0 (reference) | ||
| 75–84 years | 19,334 | 28.3% | 12,034,203 | 6.5% | 341.2 (336.4, 346.0) | 1.0 (reference) | 0.0 (reference) | ||
| 85 years and over | 30,390 | 44.4% | 5,223,448 | 2.8% | 1,235.5 (1,221.6, 1,249.4) | 1.0 (reference) | 0.0 (reference) | ||
| All ages—crude | 68,377 | 186,405,546 | 36.7 (36.4, 37.0) | 1.0 (reference) | 0.0 (reference) | ||||
| All ages—age-standardized | 68,377 | 186,405,546 | 49.9 (48.8, 51.0) | 1.0 (reference) | 0.0 (reference) | ||||
| Before 65 (age-standardized) | 6,907 | 10.1% | 146,056,189 | 78.4% | 9.5 (8.9, 10.1) | 1.0 (reference) | 0.0 (reference) | ||
| Before 75 (age standardized) | 18,653 | 27.3% | 169,147,895 | 90.7% | 16.4 (15.8, 17.1) | 1.0 (reference) | 0.0 (reference) | ||
| Non-Hispanic Black | |||||||||
| Under 1 year | 2 | 0.0% | 591,754 | 1.5% | 0.7 (0.1, 2.0) | 2.2 (0.4, 13.4) | 0.188 | 0.4 (−0.7, 1.5) | 0.230 |
| 1–4 years | 1 | 0.0% | 2,447,225 | 6.0% | 0.1 (0.0, 0.3) | 1.1 (0.1, 10.8) | 0.460 | 0.0 (−0.2, 0.2) | 0.461 |
| 5–14 years | 8 | 0.0% | 6,217,144 | 15.3% | 0.3 (0.1, 0.5) | 13.8 (2.9, 65.1) | <0.001 | 0.3 (0.1, 0.4) | 0.005 |
| 15–24 years | 58 | 0.2% | 6,500,474 | 16.0% | 1.9 (1.4, 2.4) | 6.8 (4.4, 10.5) | <0.001 | 1.6 (1.1, 2.1) | <0.001 |
| 25–34 years | 278 | 0.9% | 6,658,091 | 16.4% | 8.9 (7.8, 9.9) | 7.1 (5.8, 8.7) | <0.001 | 7.6 (6.6, 8.7) | <0.001 |
| 35–44 years | 723 | 2.5% | 5,414,553 | 13.3% | 28.4 (26.3, 30.4) | 9.0 (7.9, 10.2) | <0.001 | 25.2 (23.1, 27.3) | <0.001 |
| 45–54 years | 2,029 | 6.9% | 5,287,236 | 13.0% | 81.5 (77.9, 85.0) | 7.4 (6.9, 7.9) | <0.001 | 70.4 (66.8, 74.0) | <0.001 |
| 55–64 years | 4,997 | 17.0% | 2,653,390 | 6.5% | 399.9 (388.8, 411.0) | 5.7 (5.5, 6.0) | <0.001 | 330.0 (318.8, 341.3) | <0.001 |
| 65–74 years | 7,778 | 26.4% | 3,006,666 | 7.4% | 549.3 (537.1, 561.6) | 5.1 (4.9, 5.2) | <0.001 | 441.3 (429.0, 453.7) | <0.001 |
| 75–84 years | 7,705 | 26.1% | 1,329,955 | 3.3% | 1,230.3 (1,202.8, 1,257.7) | 3.6 (3.5, 3.7) | <0.001 | 889.1 (861.2, 917.0) | <0.001 |
| 85 years and over | 5,897 | 20.0% | 507,505 | 1.2% | 2,467.5 (2,404.5, 2,530.5) | 2.0 (1.9, 2.0) | <0.001 | 1,232.0 (1,167.5, 1,296.5) | <0.001 |
| All ages—crude | 29,476 | 40,613,993 | 72.6 (71.7, 73.4) | 2.0 (2.0, 2.0) | <0.001 | 35.9 (35.0, 36.8) | <0.001 | ||
| All ages—age-standardized | 29,476 | 40,613,993 | 181.7 (175.7, 187.8) | 3.6 (3.5, 3.8) | <0.001 | 131.8 (125.7, 138.0) | <0.001 | ||
| Before 65 (age-standardized) | 8,096 | 27.5% | 35,769,867 | 88.1% | 59.5 (56.2, 62.9) | 6.3 (5.8, 6.8) | <0.001 | 50.0 (46.6, 53.4) | <0.001 |
| Before 75 (age standardized) | 15,874 | 53.9% | 38,776,533 | 95.5% | 94.0 (89.9, 98.0) | 9.9 (9.2, 10.6) | <0.001 | 84.4 (80.3, 88.5) | <0.001 |
| Hispanic or Latino | |||||||||
| Under 1 year | 5 | 0.0% | 1,007,577 | 1.7% | 1.1 (0.1, 2.0) | 3.3 (0.8, 13.8) | 0.051 | 0.7 (−0.3, 1.7) | 0.073 |
| 1–4 years | 4 | 0.0% | 4,164,396 | 7.2% | 0.2 (0.0, 0.4) | 2.6 (0.6, 11.8) | 0.102 | 0.1 (−0.1, 0.3) | 0.128 |
| 5–14 years | 5 | 0.0% | 10,535,155 | 18.2% | 0.1 (0.0, 0.2) | 5.1 (1.0, 26.3) | 0.026 | 0.1 (−0.0, 0.2) | 0.043 |
| 15–24 years | 83 | 0.4% | 9,814,256 | 17.0% | 1.8 (1.4, 2.2) | 6.4 (4.2, 9.7) | <0.001 | 1.5 (1.1, 1.9) | <0.001 |
| 25–34 years | 387 | 1.7% | 9,429,166 | 16.3% | 8.7 (7.8, 9.6) | 7.0 (5.8, 8.4) | <0.001 | 7.5 (6.6, 8.4) | <0.001 |
| 35–44 years | 1,122 | 4.8% | 8,587,112 | 14.9% | 27.7 (26.1, 29.4) | 8.8 (7.8, 9.9) | <0.001 | 24.6 (22.9, 26.2) | <0.001 |
| 45–54 years | 2,569 | 11.0% | 7,025,565 | 12.2% | 77.7 (74.6, 80.7) | 7.0 (6.6, 7.5) | <0.001 | 66.6 (63.5, 69.7) | <0.001 |
| 55–64 years | 4,487 | 19.3% | 2,749,799 | 4.8% | 346.5 (336.4, 356.6) | 5.0 (4.8, 5.2) | <0.001 | 276.6 (266.3, 287.0) | <0.001 |
| 65–74 years | 5,435 | 23.4% | 2,682,684 | 4.6% | 430.2 (418.8, 441.7) | 4.0 (3.9, 4.1) | <0.001 | 322.2 (310.6, 333.8) | <0.001 |
| 75–84 years | 5,106 | 22.0% | 1,236,374 | 2.1% | 877.0 (852.9, 901.0) | 2.6 (2.5, 2.6) | <0.001 | 535.8 (511.3, 560.4) | <0.001 |
| 85 years and over | 4,053 | 17.4% | 499,028 | 0.9% | 1,724.7 (1,671.6, 1,777.8) | 1.4 (1.4, 1.4) | <0.001 | 489.2 (434.3, 544.1) | <0.001 |
| All ages—crude | 23,256 | 57,731,112 | 40.3 (39.8, 40.8) | 1.1 (1.1, 1.1) | <0.001 | 3.6 (3.0, 4.2) | <0.001 | ||
| All ages—age-standardized | 23,256 | 57,731,112 | 141.2 (135.8, 146.5) | 2.8 (2.7, 3.0) | <0.001 | 91.3 (85.8, 96.7) | <0.001 | ||
| Before 65 (age-standardized) | 8,662 | 37.2% | 53,313,026 | 92.3% | 53.4 (50.4, 56.4) | 5.6 (5.2, 6.1) | <0.001 | 43.9 (40.9, 47.0) | <0.001 |
| Before 75 (age standardized) | 14,097 | 60.6% | 55,995,710 | 97.0% | 79.9 (76.2, 83.6) | 8.4 (7.8, 9.1) | <0.001 | 70.4 (66.7, 74.1) | <0.001 |
| Non-Hispanic American Indian or Alaska Native* | |||||||||
| Under 1 year | 0 | 0.0% | 38,260 | 1.5% | 0.0 (0.0, 0.0) | — | — | −0.3 (−0.7, 0.0) | 0.042 |
| 1–4 years | 1 | 0.1% | 156,473 | 6.0% | 1.4 (0.0, 5.0) | 17.6 (1.8, 168.8) | 0.007 | 1.3 (−1.4, 3.9) | 0.173 |
| 5–14 years | 0 | 0.0% | 409,393 | 15.8% | 0.0 (0.0, 0.0) | — | — | −0.0 (−0.0, 0.0) | 0.079 |
| 15–24 years | 8 | 0.7% | 419,255 | 16.2% | 4.1 (1.2, 6.9) | 14.5 (6.7, 31.5) | <0.001 | 3.8 (1.0, 6.6) | 0.004 |
| 25–34 years | 47 | 4.1% | 418,797 | 16.2% | 23.8 (17.0, 30.6) | 19.1 (13.8, 26.5) | <0.001 | 22.6 (15.8, 29.4) | <0.001 |
| 35–44 years | 70 | 6.1% | 333,378 | 12.9% | 44.6 (34.1, 55.0) | 14.1 (10.9, 18.2) | <0.001 | 41.4 (31.0, 51.9) | <0.001 |
| 45–54 years | 145 | 12.7% | 326,384 | 12.6% | 94.3 (79.0, 109.7) | 8.5 (7.2, 10.1) | <0.001 | 83.3 (67.9, 98.7) | <0.001 |
| 55–64 years | 245 | 21.4% | 174,263 | 6.7% | 298.6 (261.2, 335.9) | 4.3 (3.8, 4.9) | <0.001 | 228.7 (191.2, 266.1) | <0.001 |
| 65–74 years | 267 | 23.4% | 202,493 | 7.8% | 280.0 (246.4, 313.6) | 2.6 (2.3, 2.9) | <0.001 | 172.0 (138.3, 205.6) | <0.001 |
| 75–84 years | 219 | 19.2% | 85,020 | 3.3% | 547.0 (474.6, 619.4) | 1.6 (1.4, 1.8) | <0.001 | 205.8 (133.2, 278.4) | <0.001 |
| 85 years and over | 141 | 12.3% | 28,950 | 1.1% | 1,034.3 (863.5, 1,205.0) | 0.8 (0.7, 1.0) | 0.982 | −201.2 (−372.5, −29.9) | 0.011 |
| All ages—crude | 1,143 | 2,592,666 | 44.1 (41.5, 46.6) | 1.2 (1.1, 1.3) | <0.001 | 7.4 (4.8, 10.0) | <0.001 | ||
| All ages—age-standardized | 1,143 | 2,592,666 | 108.9 (90.5, 127.4) | 2.2 (1.8, 2.6) | <0.001 | 59.0 (40.5, 77.6) | <0.001 | ||
| Before 65 (age-standardized) | 516 | 45.1% | 2,276,203 | 87.8% | 57.1 (44.3, 69.9) | 6.0 (4.7, 7.6) | <0.001 | 47.6 (34.7, 60.4) | <0.001 |
| Before 75 (age standardized) | 783 | 68.5% | 2,478,696 | 95.6% | 72.8 (58.6, 86.9) | 7.6 (6.2, 9.4) | <0.001 | 63.2 (49.1, 77.4) | <0.001 |
| Non-Hispanic Asian or Pacific Islander | |||||||||
| Under 1 year | 1 | 0.0% | 216,177 | 1.1% | 1.0 (0.0, 3.6) | 3.1 (0.3, 29.6) | 0.165 | 0.7 (−1.3, 2.6) | 0.254 |
| 1–4 years | 0 | 0.0% | 949,886 | 4.9% | 0.0 (0.0, 0.0) | — | — | −0.1 (−0.2, 0.0) | 0.958 |
| 5–14 years | 1 | 0.0% | 2,429,718 | 12.5% | 0.1 (0.0, 0.3) | 4.4 (0.4, 48.8) | 0.112 | 0.1 (−0.1, 0.2) | 0.222 |
| 15–24 years | 7 | 0.1% | 2,692,199 | 13.8% | 0.6 (0.1, 1.0) | 2.0 (0.9, 4.5) | 0.052 | 0.3 (−0.1, 0.7) | 0.102 |
| 25–34 years | 58 | 0.9% | 3,534,255 | 18.1% | 3.5 (2.6, 4.4) | 2.8 (2.1, 3.8) | <0.001 | 2.2 (1.3, 3.2) | <0.001 |
| 35–44 years | 115 | 1.8% | 3,233,519 | 16.6% | 7.6 (6.2, 8.9) | 2.4 (1.9, 3.0) | <0.001 | 4.4 (3.0, 5.8) | <0.001 |
| 45–54 years | 373 | 5.8% | 2,759,529 | 14.2% | 28.7 (25.8, 31.6) | 2.6 (2.3, 2.9) | <0.001 | 17.6 (14.7, 20.6) | <0.001 |
| 55–64 years | 905 | 14.0% | 1,174,022 | 6.0% | 163.7 (153.0, 174.4) | 2.3 (2.2, 2.5) | <0.001 | 93.8 (83.0, 104.7) | <0.001 |
| 65–74 years | 1,518 | 23.5% | 1,508,767 | 7.7% | 213.7 (202.9, 224.4) | 2.0 (1.9, 2.1) | <0.001 | 105.6 (94.7, 116.6) | <0.001 |
| 75–84 years | 1,629 | 25.2% | 708,822 | 3.6% | 488.0 (464.3, 511.7) | 1.4 (1.4, 1.5) | <0.001 | 146.9 (122.7, 171.0) | <0.001 |
| 85 years and over | 1,861 | 28.8% | 285,572 | 1.5% | 1,383.9 (1,321.0, 1,446.7) | 1.1 (1.1, 1.2) | <0.001 | 148.4 (84.0, 212.8) | <0.001 |
| All ages—crude | 6,468 | 19,492,466 | 33.2 (32.4, 34.0) | 0.9 (0.9, 0.9) | <0.001 | −3.5 (−4.4, −2.6) | <0.001 | ||
| All ages—age-standardized | 6,468 | 19,492,466 | 77.4 (71.9, 82.9) | 1.6 (1.4, 1.7) | <0.001 | 27.5 (21.9, 33.1) | <0.001 | ||
| Before 65 (age-standardized) | 1,460 | 22.6% | 16,989,305 | 87.2% | 22.8 (19.8, 25.9) | 2.4 (2.1, 2.8) | <0.001 | 13.3 (10.2, 16.5) | <0.001 |
| Before 75 (age standardized) | 2,978 | 46.0% | 18,498,072 | 94.9% | 36.3 (32.6, 39.9) | 3.8 (3.4, 4.3) | <0.001 | 26.7 (23.0, 30.4) | <0.001 |
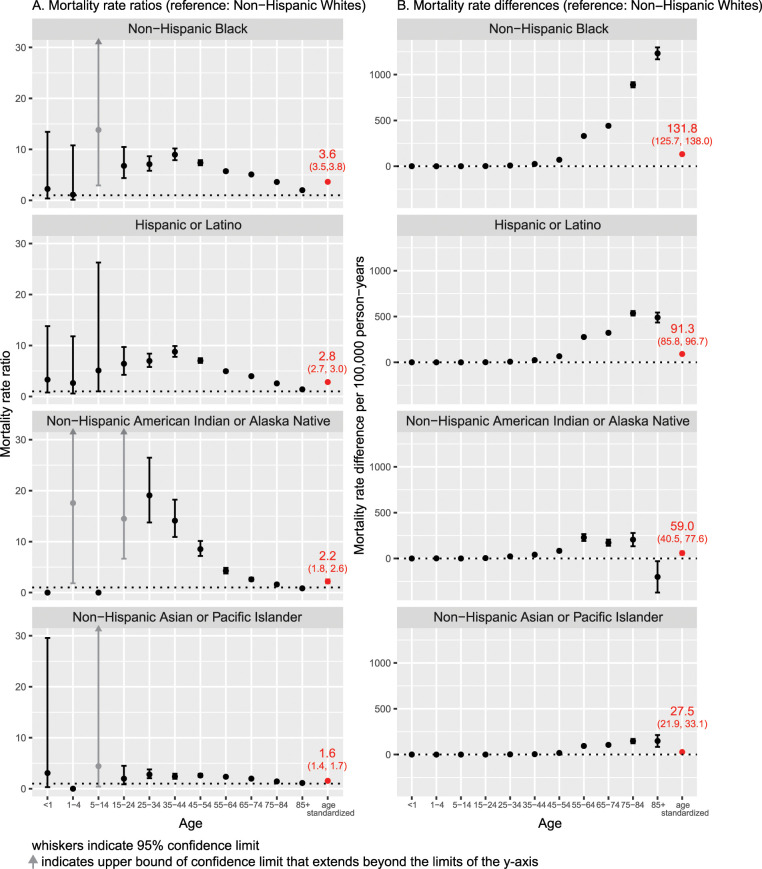
Fig 1 shows the racial/ethnic disparities in COVID-19 mortality by age categories as reflected in rate ratios and risk differences, with the NHW population as the reference, along with the age-standardized rate. For data on all-cause mortality, see S1 Table.
Fig 1. Age-specific and age-standardized COVID-19 mortality rate ratios and rate differences per 100,000 person-years with 95% confidence intervals (reference: non-Hispanic White population), as of July 22, 2020, United States.
(A) Mortality rate ratios. (B) Mortality rate differences.
Relative rate ratios
Discounting patterns for ages below 25 years, where the small numbers of deaths mean rate estimates are unstable, Fig 1A shows that there are racial/ethnic disparities, relative to the NHW population, in every age stratum. Among the NHB, Hispanic, and NHAIAN populations, these relative gaps widen and become especially stark among young adults into midlife (persons aged 25–54 years). NHB rate ratios relative to NHW were as high as 7.1 (95% CI 5.8, 8.7; p < 0.001) for persons aged 25–34 years, 9.0 (95% CI 7.9, 10.2; p < 0.001) for persons aged 35–44 years, and 7.4 (95% CI 6.9, 7.9; p < 0.001) for persons aged 45–54 years. Even at older ages, NHB rate ratios were between 2.0 and 5.7. Similarly, rate ratios for the Hispanic versus NHW population were 7.0 (95% CI 5.8, 8.4; p < 0.001), 8.8 (95% CI 7.8, 9.9; p < 0.001), and 7.0 (95% CI 6.6, 7.5; p < 0.001) for the corresponding age strata above, with remaining rate ratios ranging from 1.4 to 5.0. Rate ratios for the NHAIAN population were similarly high through age 84 years. Among NHAPI persons, rate ratios ranged from 2.0 to 2.8 for persons aged 25–74 years and were 1.4 and 1.1 for persons aged 75–84 and 85+ years, respectively. By contrast, the age-standardized rate ratios equaled 3.6 (95% CI 3.5, 3.8; p < 0.001) for NHB, 2.8 (95% CI 2.7, 3.0; p < 0.001) for Hispanic, 2.2 (1.8, 2.6; p < 0.001) for NHAIAN, and 1.6 (1.4, 1.7; p < 0.001) for NHAPI populations (see Table 1).
Rate differences
Fig 1B displays the racial/ethnic mortality rate differences, an absolute measure, for each age stratum, as compared to the NHW population. For all groups, these differences compared to the NHW population increased with advancing age and were especially pronounced for the NHB population. For example, among persons aged 75–84 years, the mortality rate difference equaled 889.1 (95% CI 861.2, 917.0; p < 0.001) per 100,000 person-years for NHB, 535.8 (95% CI 511.3, 560.4; p < 0.001) for Hispanic, 205.8 (95% CI 133.2, 278.4; p < 0.001) for NHAIAN, and 146.9 (95% CI 122.7, 171.0; p < 0.001) for NHAPI populations.
Finally, we examined whether the age-standardized premature COVID-19 mortality rates per 100,000 person-years reflect the racial/ethnic disparity in risk of early death, either before age 65 or before age 75. The age-standardized premature mortality (before age 65) per 100,000 person-years was 9.5 (95% CI 8.9, 10.1) for NHW, 59.5 (95% CI 56.2, 62.9) for NHB, 53.4 (95% CI 50.4, 56.4) for Hispanic, 57.1 (95% CI 44.3, 69.9) for NHAIAN, and 22.8 (95% CI 19.8, 25.9) for NHAPI populations. Similarly, for premature death before age 75, the age-standardized rates per 100,000 person-years were as follows: NHW, 16.4 (95% CI 15.8, 17.1); NHB, 94.0 (95% CI 89.9, 98.0); Hispanic, 79.9 (95% CI 76.2, 83.6); NHAIAN, 72.8 (95% CI 58.6, 86.9); and NHAPI, 36.3 (95% CI 32.6, 39.9) (see Table 1).
Table 2 shows the corresponding YPLL for COVID-19 (see S2 Table showing YPLL for all-cause mortality, for comparison). The disparities in COVID-19 mortality translate to 86,466 (95% CI 84,043 to 88,889) YPLL before age 65 (YPLL 65) for NHB, 107,146 (95% CI 104,315 to 109,976) for Hispanic, 7,217 (95% CI 6,433 to 8,001) for NHAIAN, and 15,460 (95% CI 14,439 to 16,480) for NHAPI populations, compared with 61,474 (95% CI 59,584 to 63,365) for the NHW population. Accounting for age distribution and population size differences between racial/ethnic groups, the age-standardized YPLL rate ratio, compared to the NHW population, equaled 6.9 (95% CI 6.9, 6.9; p < 0.001) for NHB, 6.9 (95% CI 6.8, 6.9; p < 0.001) for Hispanic, 8.7 (95% CI 8.6, 8.7; p < 0.001) for NHAIAN, and 2.5 (95% CI 2.4, 2.47; p < 0.001) for NHAPI.
Table 2. Years of potential life lost (YPLL) and age-standardized YPLL rates per 100,000 persons due to COVID-19 using age 65 and age 75 as cutoffs, with age-standardized YPLL ratios compared to the non-Hispanic White population as of July 22, 2020, United States.
| Measure | Non-Hispanic White | Non-Hispanic Black | Hispanic or Latino | Non-Hispanic American Indian or Alaska Native* | Non-Hispanic Asian or Pacific Islander |
|---|---|---|---|---|---|
| YPLL65 | 61,474 (59,584, 63,365) | 86,466 (84,043, 88,889) | 107,146 (104,315, 109,976) | 7,217 (6,433, 8,001) | 15,460 (14,439, 16,480) |
| YPLL65 difference (compared to Non-Hispanic White) | 0 (reference) | 24,992 (21,918, 28,065) | −54,258 (−56,305, −52,210) | −46,015 (−48,163, −43,867) | 45,671 (42,267, 49,075) |
| Age-standardized YPLL65 rate per 100,000 persons | 34.9 (31.7, 38.0) | 240.9 (222.6, 259.2) | 224.2 (209.1, 239.3) | 303.9 (213.4, 394.4) | 85.6 (70.9, 100.2) |
| Age-standardized YPLL65 rate ratio (compared to non-Hispanic White) | 1.00 (reference) | 6.9 (6.9, 6.9) | 6.4 (6.4, 6.4) | 8.7 (8.6, 8.9) | 2.5 (2.4, 2.5) |
| YPLL75 | 189,274 (185,799, 192,750) | 206,316 (202,270, 210,362) | 220,940 (216,458, 225,423) | 13,712 (12,532, 14,892) | 37,650 (35,936, 39,363) |
| YPLL75 difference (compared to non-Hispanic-White) | 0 (reference) | 17,042 (11,708, 22,375) | −175,562 (−179,233, −171,892) | −151,625 (−155,500, −147,750) | 31,666 (25,994, 37,338) |
| Age-standardized YPLL75 rate per 100,000 persons | 90.9 (85.3, 96.4) | 571.2 (539.0, 603.5) | 510.9 (483.2, 538.6) | 582.4 (440.1, 724.6) | 212.8 (185.3, 240.3) |
| Age-standardized YPLL75 rate ratio (compared to non-Hispanic White) | 1.00 (reference) | 6.3 (6.3, 6.3) | 5.6 (5.6, 5.6) | 6.4 (6.3, 6.5) | 2.3 (2.3, 2.4) |
Because there were relatively few deaths below age 65, ranging from 10% of all deaths for the NHW population to 45% of deaths among NHAIAN persons, a numerically small group with a population of about 2.6 million, we also examined YPLL75, because the number of deaths before age 75 is much larger. YPLL75 for all racial/ethnic groups was 2- to 3-fold larger than YPLL65, as expected because risk of COVID-19 death—and all death—increases with age. The YPLL75 rate ratios by race/ethnicity were similar to those for YPLL65, albeit slightly attenuated, and equaled, for NHB (6.3; 95% CI 6.3 to 6.33; p < 0.001), Hispanic (5.62; 95% CI 5.6 to 5.7; p < 0.001), NHAIAN (6.4; 95% CI 6.30 to 6.5; p < 0.001), and NHAPI (2.3; 95% CI 2.3 to 2.3; p < 0.001).
Discussion
We used newly available public data on COVID-19 deaths to analyze patterns of age-specific mortality by race/ethnicity. The main study finding is an excess risk of COVID-19 death at all ages in the NHB, NHAIAN, and NHAPI populations as compared to the NHW population. Disparities were particularly extreme at younger ages (25–54 years old). We additionally went beyond the computation and comparison of age-specific mortality rates to assess the differential burden of COVID-19 mortality in relation to both premature mortality and YPLL. The impact of lives prematurely cut short (before attaining 65 years) can be measured in the absolute number of YPLL. For both the NHB and Hispanic populations, this loss is much larger than for the NHW population—despite the fact that the NHW population is larger—with a ratio of is 4.6:1 and 3.2:1, respectively, for the NHB and Hispanic populations. Poor quality of NHAIAN mortality and population data likely means the estimated excesses are underestimates [18–21]. Although for all groups by far the majority of deaths occur above the age of 65 years, premature deaths deprive people of their anticipated life expectancy. As a consequence, the NHB and Hispanic populations lost nearly 7 times and the NHAIAN population nearly 9 times as many years of life before the age of 65 as did the NHW population.
Examination of age-specific mortality rates, and not simply counts of deaths or crude comparisons of the racial/ethnic composition of COVID-19 deaths to the total population, is crucial to revealing racial/ethnic disparities. Age-standardized rates are not sufficient because age standardization, while accounting for the different age distributions across racial/ethnic groups, notably obscure the magnitude of mortality inequities at younger ages [6–8]. These COVID-19 mortality rate ratios, 7- to 9-fold higher for the NHB, NHAIAN, and Hispanic populations, are extreme and reflect the devastating toll COVID-19 has taken among communities of color. To put these extreme rates in context, in 2017, the rate ratios for all-cause mortality comparing the US NHB to NHW populations, by 5-year groups for persons aged 25–29 years up through aged 60–64 years, ranged between 1.3 and 1.5 [22]. Additionally, in 2015, the age-standardized rate ratio for premature death (before age 65) among adults aged 20–64 years, comparing the US NHB to NHW population, equaled 1.5 for all-cause mortality, and ranged between 1.1 to at most 2.2 for specific causes of mortality, including leading causes of death (circulatory, neoplasms, endocrine [including diabetes], and respiratory) [7].
To capture the magnitude of racial/ethnic inequities of COVID-19, age-specific mortality rates for COVID-19 should be routinely available by race/ethnicity as well as by sex. Grasping the disparate impact of this pandemic requires transparent reporting of not only age-specific rate ratios and rate differences, but also YPLL. Robust evidence documents the transgenerational adverse impacts of parental death at younger ages on their children’s economic and health trajectories [23–25]. Our data underscore that COVID-19 will likely exacerbate these harms.
This study has several limitations. NCHS data are based on the completed death certificates received by the CDC, and thus may lag in capturing the total number of deaths compared to what is reported on state dashboards [9]. However, this lag likely would lead to underestimates of YPLL (due to deaths not yet included). Further, reporting of deaths due to COVID-19 depends in part on the accessibility of COVID-19 tests, a problem that would likely introduce a conservative bias for our racial/ethnic comparisons, given evidence of reduced access to testing among US populations of color [26,27]. Another limitation is that analysis solely of deaths classified as due to COVID-19 do not capture the full excess burden of mortality due to the pandemic. At issue is not only potential misclassification of deaths but also deaths not directly due to SARS-COV-2 infection but nevertheless due to the pandemic, e.g., deaths due to people not seeking care for chest pains because of fear of viral exposure at hospitals [28–30]. Well-known problems affecting counts of NHAIAN deaths and the NHAIAN population likely lead to conservative estimates of risk [18–21], but misclassification of race/ethnicity on death certificates is very low for the remaining racial/ethnic groups [18].
The mortality data we report do not reveal why excess deaths occur among US populations of color compared to the US NHW population, but any explanation must account for these observed age-specific patterns, also replicated in recently released data from Massachusetts [31]. Mortality rates reflect both the incidence of COVID-19 and its case fatality rate. Higher rates of co-morbid conditions among young adults in the NHB and Hispanic populations would contribute to enhanced mortality risk, as would more limited adoption of social distancing in communities of color and lack of access to healthcare. However, the extremely high age-specific mortality rate ratios we report for working-age adults, ranging between 5 and 9, cannot plausibly be explained as due mainly to co-morbid conditions. While many common conditions show racial/ethnic disparities, the relative excess in the NHB and Hispanic populations is far lower than reported here for COVID-19 mortality, with risk ratios typically under or close to 2. For example, in the case of NHB versus NHW comparisons among adults under age 65, the rate ratios for mortality due to cardiovascular disease, cancer, and diabetes are all under 2 [7], as are the rate ratios for prevalence of obesity [32,33].
In addition, continued young adult participation in the workforce outside the home increases risk of exposure to SARS-CoV-2. Data suggest that communities with a high proportion of service workers [34] and communities with cell phone mobility patterns consistent with work-related commutes and overall mobility [35,36] also have higher prevalence of COVID-19. A community prevalence study in the Mission District of San Francisco showed that 90% of those with positive viral tests were working outside the home [37]. Together, these observations, while not conclusive, support concern that low-wage essential workers are not adequately protected in the workplace. While higher rates of chronic disease and barriers to healthcare access can be addressed by policy interventions, approaches that lower viral exposure would have an immediate short-term impact. Possible actions include permitting workers to stay home when personal or household members’ health creates a higher risk for poor outcome, offering hazard pay, paid sick leave, health insurance, personal protective equipment, access to handwashing, and social distancing at work, along with, for those who so choose, alternative accommodation.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Abbreviations
- CDC
Centers for Disease Control and Prevention
- NCHS
National Center for Health Statistics
- NHAIAN
non-Hispanic American Indian/Alaska Native
- NHAPI
non-Hispanic Asian or Pacific Islander
- NHB
non-Hispanic Black
- NHW
non-Hispanic White
- YPLL
years of potential life lost
Data Availability
These data were provided by the National Center for Health Statistics (data.cdc.gov). This analysis was based on data from https://data.cdc.gov/NCHS/Deaths-involvingcoronavirus-disease-2019-COVID-19/ks3g-spdg, accessed on July 22, 2020.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Eligon J, Burch ADS, Searcey D, Oppel RA Jr. Black Americans face alarming rates of virus infection in some states. New York Times. 2020. April 14 [cited 2020 Jun 24]. Available from: https://www.nytimes.com/2020/04/07/us/coronavirus-race.html. [Google Scholar]
- 2.Bauer S. Milwaukee’s black community hit hard by coronavirus. AP News. 2020. March 27 [cited 2020 Jun 24]. Available from: https://apnews.com/b52e4e9a63d64e3a25109f09010508b6. [Google Scholar]
- 3.Krieger N, Gonsalves G, Bassett MT, Hanage W. Krumholz HM. The fierce urgency of now: closing glaring gaps in us surveillance data on COVID-19. Health Affairs Blog, 2020. April 14 [cited 2020 Jun 24]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20200414.238084/full/. [Google Scholar]
- 4.New York City Department of Health and Mental Hygiene. COVID-19: data. New York: New York City Department of Health and Mental Hygiene; 2020. [cited 2020 Jun 24]. Available from: https://www1.nyc.gov/site/doh/covid/covid-19-data.page. [Google Scholar]
- 5.Gross CP, Essien UR, Pasha S, Gross JR, Wang S-Y, Nunez-Smith M. Racial and ethnic disparities in population-level Covid-19 mortality. medRxiv. 2020. May 11 10.1101/2020.05.07.20094250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cunningham TJ, Croft B, Liu Y, Lu H, Eke PI, Giles WH. Vital signs: racial disparities in age-specific mortality among Blacks or African-Americans—United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2017;66:444–56. 10.15585/mmwr.mm6617e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Y, Freedman ND, Rodriquez EJ. Shiels MS, Napoles AM, Withrow DR, et al. Trends in premature deaths among adults in the United States and Latin America. JAMA Netw Open. 2020;3(2):e1921085 10.1001/jamanetworkopen.2019.21085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams DR. The health of US racial and ethnic populations. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No 2):53–62. [DOI] [PubMed] [Google Scholar]
- 9.Oppel RA Jr, Gebeloff R, Lai KKR, Wright W, Smith M. The fullest look yet at the racial inequity of coronavirus. New York Times. 2020. July 5 [cited 2020 Jul 31]. Available from: https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html. [Google Scholar]
- 10.National Center for Health Statistics. Deaths involving coronavirus disease (COVID-19) by race and Hispanic origin group and age, by state. Atlanta: Centers for Disease Control and Prevention; 2020. July 20 [cited 2020 Jul 22]. Available from: https://data.cdc.gov/NCHS/Deaths-involving-coronavirus-disease-2019-COVID-19/ks3g-spdg. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Atlanta: Centers for Disease Control and Prevention; 2020. [cited 2020 Jul 31]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. [Google Scholar]
- 12.CDC WONDER. Bridged-race resident population estimates: United States, state and county for the years 1990–2019. Atlanta: Centers for Disease Control and Prevention; 2020. [cited 2020 Oct 5]. Available from: https://wonder.cdc.gov/wonder/help/bridged-race.html/. [Google Scholar]
- 13.National Cancer Institute Surveillance, Epidemiology, and End Results Program. Standard populations (millions) for age-adjustment. Bethesda (MD): National Cancer Institute; 2020. [cited 2020 Jun 24]. Available from: https://seer.cancer.gov/stdpopulations/. [Google Scholar]
- 14.Rothman KJ, Greenland S. Modern epidemiology. 2nd edition. Philadelphia: Lippincott-Raven; 1998. [Google Scholar]
- 15.CDC WONDER. Underlying cause of death 1999–2018. Atlanta: Centers for Disease Control and Prevention; 2020 [cited 2020 Oct 2]. Available from: https://wonder.cdc.gov/wonder/help/ucd.html.
- 16.Centers for Disease Control (CDC). Premature mortality in the United States: public health issues in the use of years of potential life lost. MMWR Suppl. 1986;35(2):1S‐11S. [PubMed] [Google Scholar]
- 17.Krieger N, Rehkopf DH, Chen JT, Waterman PD, Marcelli E, Kennedy M. The fall and rise of US inequities in premature mortality: 1960–2002. PLoS Med. 2008;5(2):e46 10.1371/journal.pmed.0050046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arias E, Heron M, National Center for Health Statistics, Hakes J, US Census Bureau. The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. Vital Health Stat 2. 2016;(172):1–21. [PubMed] [Google Scholar]
- 19.Anderson RN, Copeland G, Hayes JM. Linkages to improve mortality data for American Indians and Alaska Natives: a new model for death reporting? Am J Public Health. 2014;104(Suppl 3):S258–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krieger N. The US Census and the people’s health: public health engagement from enslavement and “Indians not taxed” to census tracts and health equity (1790–2018). Am J Public Health. 2019;109(8):1092–100. 10.2105/AJPH.2019.305017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bigback KM, Hoopes M, Dankovchik J, Knaster E, Warren-Mears V, Joshi S, et al. Using record linkage to improve data quality for American Indian and Alaska Natives in two Pacific Northwest state hospital discharge databases. Health Serv Res. 2015;50(Suppl 1):1390–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kochanek KD, Murphy SL, Xu JQ, Arias E. Deaths: final data for 2017. Natl Vital Stat Rep. 2019;68(9):1–76. [PubMed] [Google Scholar]
- 23.Umberson D. Black deaths matter: race, relationship loss, and effects on survivors. J Health Soc Behav. 2017;58(4):405–20. 10.1177/0022146517739317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Umberson D, Olson JS, Crosnoe R, Liu H, Pudrovska T, Donnelly R. Death of family members as an overlooked source of racial disadvantage in the United States. Proc Natl Acad Sci U S A. 2017;114(5):915–20. 10.1073/pnas.1605599114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thyden NH, Schmidt NM, Osypuk TL. The unequal distribution of sibling and parent deaths by race and its effect on attaining a college degree. Ann Epidemiol. 2020;45:76–82.e1. 10.1016/j.annepidem.2020.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lieberman-Cribbin W, Tuminello S, Flores RM, Taioli E. Disparities in COVID-19 testing and positivity in New York City. Am J Prev Med. 2020;59(3):326–32. 10.1016/j.amepre.2020.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Servick K. ‘Huge hole’ in COVID-19 testing data makes it harder to study racial disparities. Science Magazine. 2020. July 10 [cited 2020 Jul 31]. Available from: https://www.sciencemag.org/news/2020/07/huge-hole-covid-19-testing-data-makes-it-harder-study-racial-disparities. [Google Scholar]
- 28.Leon DA, Shkolnikov VM Smeeth L, Magnus P, Pecholdová M, Jarvis CI. COVID-19: a need for real-time monitoring of weekly excess deaths. Lancet. 2020;395(10234):e81 10.1016/S0140-6736(20)30933-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.New York Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team. Preliminary estimate of excess mortality during the COVID-19 outbreak—New York City, March 11–May 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:603–5. 10.15585/mmwr.mm6919e5 [DOI] [PubMed]
- 30.Chen JT, Waterman PD, Krieger N. COVID-19 and the unequal surge in mortality rates in Massachusetts, by city/town and ZIP Code measures of poverty, household crowding, race/ethnicity, and racialized economic segregation. HCPDS Working Paper Volume 19, Number 2. Cambridge: Harvard Center for Population and Development Studies; 2020 May 9 [cited 2020 Jun 24]. Available from: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/1266/2020/05/20_jtc_pdw_nk_COVID19_MA-excess-mortality_text_tables_figures_final_0509_with-cover-1.pdf.
- 31.COVID-19 Health Equity Advisory Group. Health Equity Advisory Group recommendations—July 2020. Boston: Massachusetts Department of Public Health; 2020. July 9 [cited 2020 Oct 5]. Available from: https://www.mass.gov/orgs/covid-19-health-equity-advisory-group. [Google Scholar]
- 32.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief. 2020;(360):1–8. [PubMed] [Google Scholar]
- 33.Office of Minority Health. Obesity and African Americans. Washington (DC): US Department of Health and Human Services; 2020. [cited 2020 Jun 24]. Available from: https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=25. [Google Scholar]
- 34.Afridi A, Block L. Frontline communities hit hardest by COVID-19. New York: Association for Neighborhood and Housing Development; 2020. April 2 [cited 2020 Jun 24]. Available from: https://anhd.org/blog/frontline-communities-hit-hardest-covid-19. [Google Scholar]
- 35.Kissler SM, Kishore N, Prabhu M, Goffman D, Beilin Y, Landau R, et al. Reductions in commuting mobility predict geographic differences in SARS-CoV-2 prevalence in New York City. Cambridge: Harvard University; 2020. [cited 2020 Jun 24]. Available from: http://nrs.harvard.edu/urn-3:HUL.InstRepos:42665370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glaeser EL, Gorback CS, Redding SJ. How much does COVID-19 increase with mobility? Evidence from New York and four other U.S. cities. NBER Working Paper No. 27519. Cambridge: National Bureau of Economic Research; 2020 Jul [cited 2020 Jul 31]. Available from: https://www.nber.org/papers/w27519.
- 37.Fernandez E, Weiler N. Initial results of Mission District COVID-19 testing announced. Latinx Community, men and economically vulnerable are at highest risk. San Francisco: University of California, San Francisco; 2020. May 4 [cited 2020 Jun 24]. Available from: https://www.ucsf.edu/news/2020/05/417356/initial-results-mission-district-covid-19-testing-announced. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
These data were provided by the National Center for Health Statistics (data.cdc.gov). This analysis was based on data from https://data.cdc.gov/NCHS/Deaths-involvingcoronavirus-disease-2019-COVID-19/ks3g-spdg, accessed on July 22, 2020.