ABSTRACT
Background:
The limb occlusion pressure (LOP) is determined to calculate the relative LOP. The different levels of relative LOP (percentage of LOP) influence the treatment effect and perceived discomfort during low-load blood flow restriction (BFR) strength training. Thus, determining the LOP is of the utmost importance when using BFR in clinical practice.
Purpose:
The objective of this study was to investigate the concurrent validity and intra-rater (test-retest), intra-day reliability of an inexpensive, portable, easy-to-use handheld (HH) oximeter compared to a high-resolution Doppler ultrasound scanner in detecting LOP in the lower extremity.
Study design:
Cross-sectional validity and reliability study
Methods:
Two raters who were blinded from each other simultaneously assessed 50 healthy participants (mean age of 25.8 years). A 20 cm-wide thigh cuff with an attached sphygmomanometer was inflated until the raters independently registered the LOP with the HH oximeter and the Doppler ultrasound scanner. The test session was repeated once after a five-minute time interval.
Results:
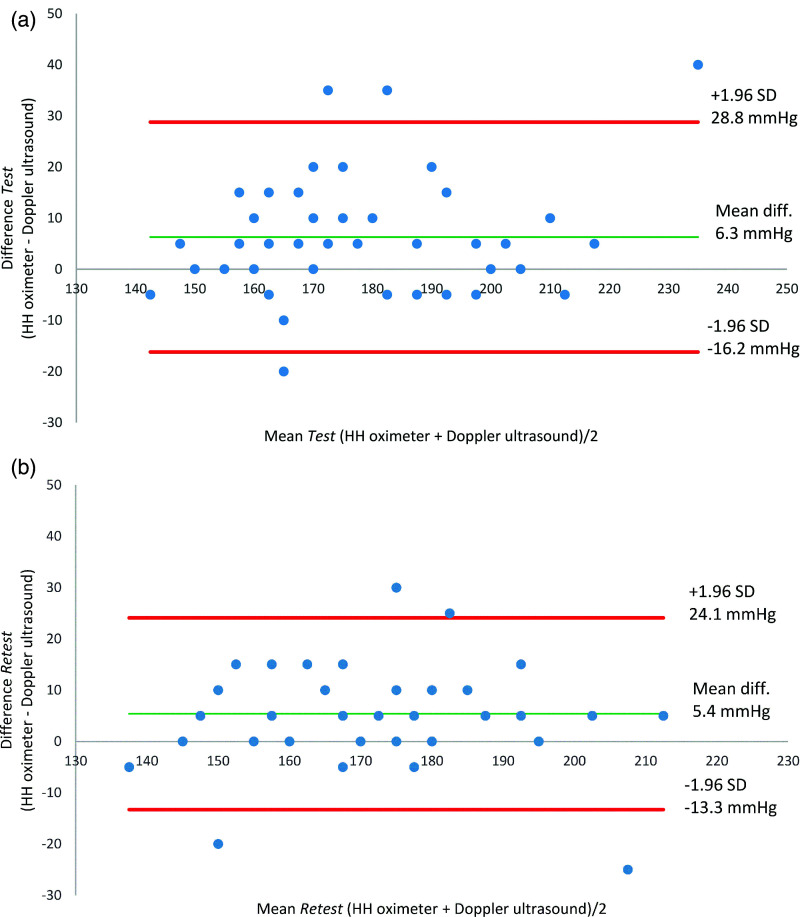
The HH oximeter recorded a non-significantly higher LOP than the Doppler ultrasound scanner, with a mean difference of 6.3 mmHg in the test session (95% limits of agreement (LoA): -16.2 to 28.8, p = 0.13) and 5.4 mmHg in the retest session (95% LoA: -13.3 to 24.0, p = 0.10). The intra-rater reliability for both devices was moderate (ICC = 0.72-0.79). The measured LOP was significantly lower (p < 0.005) in the retest session than in the test session for both the HH oximeter (mean difference: -5.7 mmHg) and the Doppler ultrasound scanner (mean difference: -4.8 mmHg).
Conclusions:
The HH oximeter is a valid and reliable measuring device for determining the LOP in the lower extremity in healthy adults. The authors recommend performing at least two LOP measurements with a one-minute rest interval.
Level of Evidence:
2, Validity and reliability study
Keywords: Blood flow restriction, limb occlusion pressure, oximeter, Doppler ultrasound, validity, reliability
INTRODUCTION
Blood flow restriction with low-load strength training (BFR-LLST) (20-40% of 1-repetition maximum [1RM]) is a novel exercise training modality intended to increase muscle hypertrophy and strength in the extremities which requires less load than traditional strength training (70-80% of 1RM). This exercise training modality seems to be highly relevant for patients who either are not allowed weight-bearing activities or experience pain during traditional strength training.1
BFR-LLST involves the application of a wrapping device, such as an inflated tourniquet/cuff or a specially designed strap,2 to restrict the arterial inflow and venous outflow to the muscle(s) during exercise. Safety is a common concern raised while performing BFR exercise, as this type of exercise can negatively affect the cardiovascular system, for example, among the elderly and immediately after surgery. Some of the specific concerns that have been raised include lower extremity muscle pain, nerve damage,3,4 and cardiovascular adverse events, such as deep venous thrombosis.5,6 A factor that can impose a safety risk is high limb (arterial) occlusion pressure (LOP) during BFR-LLST, which limits or stops the arterial inflow to the muscle(s).4 The LOP is defined as the minimum occlusion pressure necessary to stop the flow of arterial blood into the lower limb distal to the cuff.7
The relative LOP is a percentage of the estimated LOP. In rehabilitation protocols for BFR-LLST, relative LOP is reported between 40% and 90%.8-10 When BFR-LLST is implemented in clinical practice, the LOP is commonly not determined.11 Despite this, very few adverse events have been reported.12
The determination of the LOP relies primarily on cuff width,13 cuff type,8 and limb circumference.14 Recently, use of a handheld (HH) Doppler (auscultatory signal) has been proposed as a valid and practical method to determine the LOP, compared to a pulse wave Doppler ultrasound.15 An alternative, inexpensive, portable, and easy method of detecting LOP could be the use of a handheld oximeter, which, in addition to monitoring an individual's saturation, simultaneously measures the pulse rate. The sensor is placed on the index finger or the second toe, and LOP is detected when the restrictive pressure from the inflated cuff reaches a level where the pulse is undetectable on a graphical pulse frequency display (pulse stop). The validity of an oximeter also measuring the pulse rate (Zimmer Biomet, Warsaw, IN, United States), compared to that of an HH Doppler ultrasound, exhibited unacceptable accuracy in determining the LOP in the lower limb, but not in the upper limb, in a healthy population.16
To use a HH oximeter (CR-100 Handheld Pulse Oximeter, Henzhen Coreray Technology Co., Ltd., China) for the measurement of LOP, it is crucial to assess the clinimetric characteristics, both the validity and reliability, in healthy adults. Therefore, the objective of this study was to compare an HH oximeter with a pulse wave Doppler ultrasound scanner as the reference standard in terms of its validity in detecting LOP in the lower extremity. Additionally, the intra-rater (test-retest), intra-day reliability was determined for both the HH oximeter and the Doppler ultrasound. It was hypothesized that the HH oximeter would provide a valid and reliable method for detecting LOP in healthy adults.
METHODS
Design
This study was a concurrent validity and intra-rater (test-retest), intra-day reliability study between an HH oximeter with a graphical pulse frequency display and a pulse wave Doppler ultrasound scanner. The HH oximeter was compared with the Doppler ultrasound scanner in terms of its accuracy in determining the LOP in the lower extremity. The reporting of the study was in accordance with Guidelines for Reporting Reliability and Agreement Studies (GRRAS)17 and adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cross-sectional studies.18
Participants
A convenience sample of 50 healthy participants was recruited from University College Absalon, Denmark. Inclusion criteria were participants aged between 18 and 70 years, able to understand and speak Danish. Participants were excluded if they had a diagnosed cardiovascular or musculoskeletal disorder, used any medication, or were pregnant. All participants were informed of the procedures and any potential risks before they gave their written informed consent. Ethical approval was obtained from the Committee for Medical Research Ethics in the Capital Region of Denmark (identification number: 17031344).
Instruments
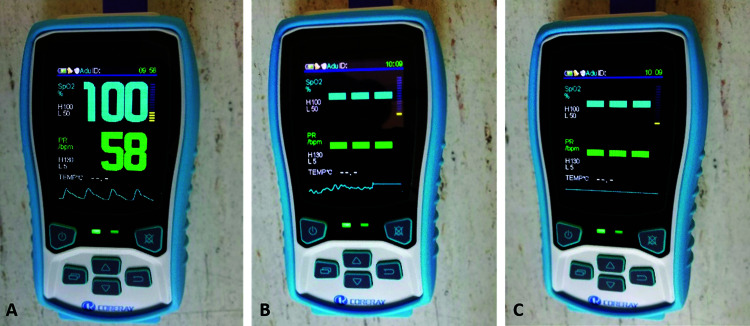
The HH oximeter (CR-100 Handheld Pulse Oximeter, Henzhen Coreray Technology Co., Ltd., China) displays the pulse (0-250 beats per minute (BPM)) rate with an interval of 1 BPM (Figure 1). The displayed hemoglobin saturation (SpO2) was not used.
Figure 1.
Illustration of A) the handheld (HH) oximeter displaying hemoglobin saturation of 100%, a pulse rate of 58 beats per minute, and regular sinus curves at the bottom of the screen, B) the HH oximeter showing the transition phase with limited arterial blood flow to limb occlusion (LOP) indicated by the flat line with no sinus curves, and C) the HH oximeter shows LOP.
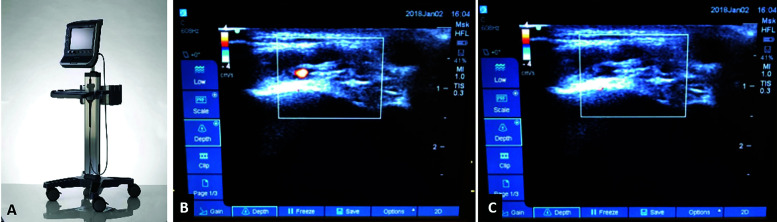
A portable high-resolution color pulse wave Doppler ultrasound scanner (SonoSite S-MSK™, FUJIFILM SonoSite, Inc., United States) was used, with the depth set at 2.5 cm (Figure 2). Selection of an auscultatory Doppler signal was not possible on this device.
Figure 2.
Illustration of A) the portable high-resolution color pulse wave Doppler ultrasound scanner, B) blood flow through the dorsalis pedis artery visualized as a red pulsation with the 2D visual Doppler function, and C) the same participant displays limb occlusion pressure indicating no arterial blood flow denoted by the red arrow.
Data Acquisition Set-up
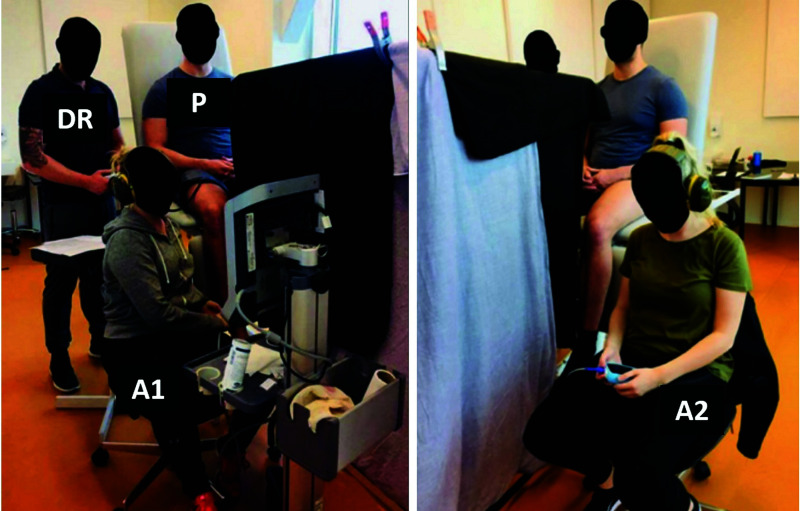
The measurements were taken in a quiet and temperature-controlled room (21–24° C). The test leg was randomly chosen by flipping a coin. The participants were positioned in an upright sitting position with back support, with their legs hanging freely over the edge of an examination couch. A 20 cm-wide (Heine Gamma® XXL LF, Thigh, HEINE, Optotechnik GmbH & Co., Herrsching, Germany) nylon cuff was placed around the most proximal part of the thigh. The two raters were blinded visually and auditorily from each other by a curtain and the use of earmuffs (Figure 3). The foot and instruments were cleaned with alcohol and allowed to dry before each test. One of the raters attached the adult-size finger clip SpO2 connected to the HH oximeter to the tip of each participant's second toe. The other rater located the dorsalis pedis artery by palpation, lateral to the extensor hallucis muscle-tendon over the navicular bone, and placed the transducer of the Doppler ultrasound perpendicular to the skin, in a water-soluble gel. The data recorder inflated the thigh cuff with a sphygmomanometer attached (Heine Gamma® G5, HEINE, Optotechnik GmbH & Co., Herrsching, Germany) to a starting pressure level of 80 mmHg and added 5 mmHg every 10 seconds until both raters signaled that they had registered the LOP, as indicated by lifting their hands. This implied that the raters measured the LOP simultaneously. The data recorder noted the level of LOP recorded by each rater. The cuff was deflated and removed; each participant then walked around in the room for two minutes. After a rest period of two minutes, the test procedure was repeated on the same leg. Between testing sessions, the participants were given a break of approximately five minutes in total. Thus, the intra-rater LOP was measured for both the HH oximeter and the Doppler ultrasound.
Figure 3.
Data collection setup. The two raters monitor the limb occlusion pressure on the Doppler ultrasound (A1) and the handheld oximeter (A2), respectively, on a participant (P), while the data recorder (DR) manages and registers the pressure of the cuff.
The participants rated their thigh pain on a numeric rating scale (NRS)19 ranging from 0 (”no pain”) to 10 (”worst possible pain”) points, and they rated their level of perceived exertion on a Borg RPE (ratings of perceived exertion) scale20 ranging from 6 (“no exertion at all”) to 20 (“maximal exertion”) points. Thigh pain at rest was rated without the cuff before and after each test session. Thigh pain and perceived exertion during the occlusion were rated immediately after the occlusion, as the recall of pain and perceived exertion during the occlusion. This test procedure was repeated on the same leg.
Statistical Analysis
QQ-plots and histograms of the test-retest and HH oximeter-Doppler ultrasound residuals were visually examined for normal distribution. Normalized and categorical data were analyzed using parametric and non-parametric statistics, respectively. Concurrent validity between the HH oximeter and the Doppler ultrasound was assessed by a) inspecting scatter plots, with a fitted regression line of the sum of least squares; b) performing a simple linear regression to determine the Pearson correlation coefficient; and c) conducting an unpaired t-test to investigate potential differences between the means of the HH oximeter and the Doppler ultrasound. Bland-Altman plots with associated 95% of limits of agreement (LoA) were used to assess the agreement between the two methods of measuring LOP. A 95% LoA (mean difference between HH oximeter and Doppler ultrasound ± 1.96 SD of the difference) was considered acceptable if the 95% LoA was ± 20 mmHg LOP. Finally, the differences between the test session and the retest session in terms of thigh pain and perceived exertion were non-normally distributed and were analyzed using the Wilcoxon matched pairs signed rank test. Linear relationships (correlation coefficient, R) between 0.40 and 0.69, 0.70 and 0.89, and 0.90 and 1.00 were interpreted as moderate, strong, and very strong, respectively.21 Relative intra-rater (test-retest) reliability was assessed using the intraclass correlation coefficient (ICC2.1, 2-way random effects, absolute agreement, single rater/measurement) with the corresponding 95% confidence interval (CI). Absolute intra-rater (test-retest) reliability was assessed using the standard error of measurement (SEM), calculated as , from a two-factor repeated measures analysis of variance (ANOVA), and the smallest detectable change (SDC) (95% CI) was calculated as . ICC values of less than 0.5, between 0.5 and 0.75, between 0.75 and 0.9, and greater than 0.90 were considered indicative of poor, moderate, good, and excellent reliability, respectively.22 For both the HH oximeter and the Doppler ultrasound, paired t-tests investigated the systematic differences between test sessions (test-retest), and Bland-Altman plots evaluated the heteroscedasticity of the test sessions by examining whether the magnitude of test session differences was related to the means of the two test sessions. The level of significance was set at an alpha level of p < 0.05. On the basis of previous work,23 a sample size of 50 participants was known to be required to achieve 80% power, 5% type 1 error, an expected ICC of 0.9, and a minimum acceptable ICC of 0.75.22 A total of 50 participants were therefore included. Stata 15.1 (StataCorp LLC, TX, United States) was used for all the statistical analyses.
RESULTS
Fifty-two eligible participants volunteered to participate in this study. Two participants were excluded: One participant's data could not be used due to a technical registration error of the limb occlusion pressure, and one participant experienced dizziness during testing. Thus, 50 participants, 28 males (56%), were included in the study (Table 1). Seven of the participants (14%) had previously tried limb occlusion as part of a blood flow restriction exercise.
Table 1.
Summary of participant characteristics (n=50)
| Variable | Mean (SD) |
|---|---|
| Age, years | 25.8 (7.4) |
| Height, cm | 174.4 (9.3) |
| Weight, kg | 75.8 (15.1) |
| BMI, kg/m2 | 24.8 (3.9) |
BMI: Body Mass Index
Validity
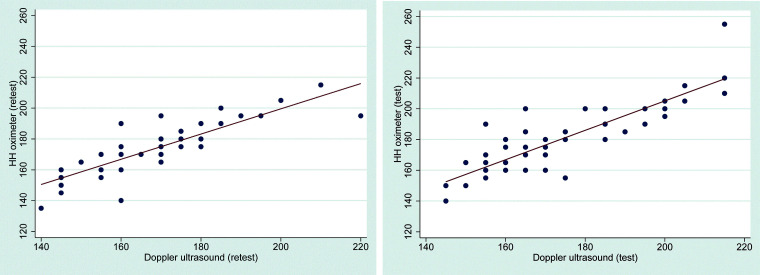
The scatter plots (Figure 4) and simple linear regression revealed a strong linear relationship between the two measurement methods in both the test session (r = 0.86, 95% CI 0.76-0.92, p < 0.001) and the retest session (r = 0.84, 95% CI 0.73-0.91, p < 0.001), indicating strong concurrent validity.
Figure 4.
Scatterplots with fitted simple linear regression lines of handheld (HH) oximeter and Doppler ultrasound relationship in measuring limb occlusion pressure at the left) test and right) retest session.
The mean LOP measured with the HH oximeter was not significantly higher than the mean LOP measured with the Doppler ultrasound in either the test (p = 0.13) or the retest (p = 0.10) session (Table 2).
Table 2.
Summary measures and differences in limb occlusion pressures for handheld (HH) oximeter and Doppler ultrasound between test-retest sessions (n=50).
| HH oximeter, (mmHg) mean (SD) | Doppler ultrasound, (mmHg) mean (SD) | Difference | |
|---|---|---|---|
| Test | 179.0 (3.1) | 172.7 (2.8) | 6.3 (11.2)NS |
| Retest | 173.3 (2.3) | 167.9 (2.4) | 5.4 (9.4)NS |
| Difference | 5.7 (13.8)* | 4.8 (11.0)* |
mmHg: Thigh cuff pressure measured in millimeters of mercury
SD: ± 1 standard deviation
NS: Not significant at p>0.05 (unpaired t-test)
Statistically significant at p<0.01 (paired t-test)
Bland-Altman plots illustrating the agreement between the HH oximeter and the Doppler ultrasound as methods for measuring LOP are presented in Figure 5. The 95% LoA is expressed as the mean difference ( ± 1.96 SD). The two methods of measuring LOP had a mean difference of 6.3 mmHg in the test session (LoA: -16.2 to 28.8) and a mean difference of 5.4 mmHg in the retest session (LoA: -13.3 to 24.1).
Figure 5.
Bland Altman plots of the handheld oximeter and Doppler ultrasound method comparison in measuring limb occlusion pressure a) test and b) retest session. The red lines indicate the 95% limits of agreement.
Reliability
The average LOP recorded by the HH oximeter was 5.7 mmHg higher in the test session (179 mmHg) than in the retest session (173.3 mmHg), indicating a systematic difference between the test sessions (p = 0.005) (Table 2). A similar systematic difference (p = 0.003) was also found for the Doppler ultrasound, which recorded an average LOP that was 4.8 mmHg higher in the test session (172.7 mmHg) than in the retest session (167.9 mmHg). The relative intra-rater (test-retest), intra-day reliability achieved by the HH oximeter and the Doppler ultrasound was moderate (ICC = 0.72) and good (ICC = 0.79), respectively. Both the HH oximeter and the Doppler ultrasound achieved acceptable absolute reliability (SEM = 10 and 8 mmHg, and SDC = 27 and 22 mmHg), respectively. (Table 3).
Table 3.
Intra-rater (test-retest), intra-day reliability for the handheld (HH) oximeter and the Doppler ultrasound
| ICC2.1 [95% CI] | SEM mmHg | SDC95 mmHg | |
|---|---|---|---|
| HH oximeter | 0.72 [0.52 to 0.83] | 10 | 27 |
| Ultrasound | 0.79 [0.63 to 0.88] | 8 | 22 |
ICC: Intraclass Correlation Coefficient
SEM: Standard Error of Measurement
mmHg: Thigh cuff pressure measured in millimeters of mercury
CI: Confidence Interval
SDC95: Smallest Detectable Change with a 95% CI
Pain and Perceived Exertion
No difference between the test and retest session was observed in terms of the level of thigh pain or perceived exertion (Table 4).
Table 4.
Thigh pain and perceived exertion during the test and retest session
| Test | Retest | p-value | |
|---|---|---|---|
| Thigh pain (NRS scale) | |||
| Before testing | 0 [0-0] | 0 [0-0] | 0.16 |
| During testing | 3 [2-4] | 3 [1-5] | 0.29 |
| After testing | 0 [0-1] | 0 [0-0] | 0.06 |
| Perceived exertion (Borg RPE scale) | |||
| During testing | 12 [9-15] | 11 [9-15] | 0.81 |
Data presented as median, [interquartile range (IQR)]
NRS: Numeric Rating Scale ranging from 0 = no pain to 10 = worst imaginable pain
RPE: Ratings of Perceived Exertion scale ranging from 6 = no exertion at all to 20 = maximal exertion
DISCUSSION
This study compared an HH oximeter with a high-resolution color pulse wave Doppler ultrasound scanner in terms of its validity in determining the LOP in the lower extremity in healthy participants. Furthermore, the intra-rater (test-retest), intra-day reliability of the HH oximeter and Doppler ultrasound in determining LOP was evaluated.
The main findings were as follows: 1) the HH oximeter provides a valid measurement in determining LOP in healthy participants; 2) the HH oximeter and the Doppler ultrasound exhibited moderate intra-rater (test-retest) reliability and measurement error in measuring LOP; and 3) a systematic difference was found between the test and retest sessions for both the HH oximeter and the Doppler ultrasound.
Explanation of results and comparison with other studies
Validity
Strong linear relationship and no significant difference were found between the HH oximeter and the Doppler ultrasound. Although the 95% LoAs (the range within which 95% of the differences between measurements by the HH oximeter and the Doppler ultrasound fell) were wide, they were considered acceptable (≈ ± 20 mmHg).24 The reason for the variation between the HH oximeter and the Doppler ultrasound seems to be multifactorial. First, the recorder incrementally increased the pressure in the cuff by 5 mmHg manually while simultaneously assessing a potential pulse stop indicated by the raters’ hands. As an alternative, a person focusing only on increasing the pressure in the cuff could have increased the agreement between the HH oximeter and the Doppler ultrasound. Second, an easy-to-use, relatively inexpensive, and portable inflatable cuff system with a standard sphygmomanometer widely used in clinical practice was pragmatically chosen. To enhance the clinical applicability to rehabilitation programs using BFR open-chain knee-extensions (i.e. quadriceps strength exercises), the participants were seated with the cuff placed around the most proximal part of the thigh. A small movement of the thigh could have changed the pressure measured by the sphygmomanometer. Third, it took approximately eight seconds for the HH oximeter to detect a change in pulse rate and, thus, a pulse stop. As the Doppler ultrasound measured a pulse stop instantly, a discrepancy in LOP recordings may have occurred.
The validity of LOP in the lower extremity has been executed on similar and more costly devices, such as a pulse oximeter (Zimmer Biomet, Warsaw, IN, USA),16 a handheld auscultatory Doppler ultrasound,15 a distal-sensor-based automatic measurement technique,25 and a personalized tourniquet instrument with the dual purpose of controlling limb pressure and measuring pulse.26 All the studies using auscultatory Doppler ultrasound as a gold standard, except for the study using a pulse oximeter, reported no systematic differences between their device and the Doppler ultrasound.16 The distal-sensor-based technique25 and the personalized tourniquet system26 achieved similar 95% LoAs of ≈ ± 18 mmHg and ≈ ± 26 mmHg (outliers removed), respectively; meanwhile, a HH Doppler ultrasound achieved slightly more favorable results with a better agreement (95% LoA of ≈ ± 13 mmHg) than in the present study.15 In the study by Zeng et al, LOP was assessed after the participants were allowed 15 minutes of rest in a supine position.15 The better agreement may be attributable to both a longer resting period prior to the assessment of LOP and the supine position of the participants. Finally, the pulse oximeter demonstrated a substantial disagreement, 95% LoA of ≈ ± 41 mmHg (outliers removed), which was primarily explained by epidermal thickness at the sole of the first toe, temperature changes, and nail polish.16
This indicates that the HH oximeter is comparable to other, more expensive and sophisticated devices, and more acceptable than a similar pulse oximeter, in terms of validity in detecting LOP.
Reliability
There was a significant difference between the test session and the retest session in terms of the LOP recorded by both the HH oximeter and Doppler ultrasound. The variability between multiple readings of blood pressure assessment has been described previously,27 and blood pressure readings are higher in the clinical setting than at home.28 This has been ascribed to the alerting response, anxiety, and/or a conditional response to an unusual situation, such as the first-time determination of LOP.29 At least two blood pressure recordings are recommended when the measurements are being taken in a clinical setting. If the first two readings differ by > 10 mmHg, a third blood pressure measurement should be taken. The blood pressure should be recorded as an average of the last two readings.28 Additionally, a study found that the LOP in the upper arm changed by up to 20 mmHg within a day and between days, and the authors of the study emphasized the necessity of taking multiple LOP measurements to account for the influence of time30. The relative intra-rater (test-retest), intra-day reliability of the HH oximeter (ICC = 0.72) was moderate and slightly lower than that of the Doppler ultrasound (ICC=0.79). Similar findings were observed for the absolute reliability, where the measurement error for the HH oximeter at the individual level (SDC = 27 mmHg) was slightly larger than for the Doppler ultrasound (22 mmHg).
Both the relative and absolute intra-rater (test-retest) reliability of similar devices in determining LOP23,31 have been evaluated in studies with small sample sizes (n < 20).
For a handheld Doppler ultrasound with an automatically pressure-adjusted system and a personalized tourniquet instrument with the dual purpose of controlling limb pressure and measuring pulse, the relative reliability was found to be good (ICC = 0.8) and excellent (ICC = 0.95-0.98), respectively, and the absolute reliability (coefficient of variance (CV)) was found to be 5.5% and ≈ 2% to 3%, respectively.23,31 The CV in the present study was 3.3% (not reported in the results section). Unfortunately, the SDC was not reported in these two other studies, which represents the measurement error at an individual level in the actual units (mmHg) of the measurement. The SDC is easier to interpret in clinical practice.32
Study Limitations and Strengths
The present study population consisted of healthy and primarily young subjects. Because validity and reliability are population-specific, the findings may not be extrapolated to populations with musculoskeletal disorders (e.g., older patients with leg injuries). This seems relevant, as it has been proposed that the measurements provided by an HH oximeter could be dependent on variables such as cold digits or poor peripheral circulation in the leg.33 The experimental set-up with a tester who simultaneously inflated the cuff and recorded the pulse stops could have caused the variation in measurements. To avoid the systematic bias between test and retest trials (reliability) for both the HH oximeter and the Doppler ultrasound, several tests or “practice” trials of the LOP should have been performed to reach stable measurements. Future research is needed to determine the reliability and validity of the oximeter with a LOP measurement protocol consisting of at least two to three subsequent measurements with intervals of one to two minutes between tests. Finally, one participant was excluded due to a faulty reading of the LOP by the rater, and one participant withdrew due to psychological factors (dizziness). In a retrospective survey examining the side effects of BFR, dizziness was reported in a limited number of cases (two out of 12642 persons).12 On average, the participants in the present study perceived LOP determination as fairly light (Borg-exertion ≈ 12 points)20 and thigh pain as mild (NRS-pain ≈ 3 points),19,34 indicating that the determination of LOP using an HH oximeter can be considered safe.
Clinical Applicability
An HH oximeter with a portable inflatable cuff system and a sphygmomanometer is an acceptable, valid device for estimating limb occlusion pressure in the lower limb in healthy participants. In accordance with previous research, the participants’ average LOP was 5.7 mmHg higher (≈ 3%) in the first test (179.0 mmHg) than in the retest session (173.3 mmHg), indicating a systematic difference. Therefore, it is recommended to perform at least two measurements to determine LOP with a one-minute time interval between measurements. A 10 mmHg difference between readings would necessitate a third measurement. It is proposed taking an average of the last two readings.28 An advantage in clinical use would be that after the determination of the LOP, the participants/patients would not have to remove the portable inflatable cuff system, as the same system is used when engaging in BFR exercise for the lower extremity, such as knee extensions. In this study, it must be addressed that the HH oximeter was used to determine the LOP in relation to blood flow restriction exercise, not for the diagnosis of hypertension28 or levels of tourniquet inflation pressure in orthopedic surgery.26 A primary concern is that high LOP can completely occlude the arterial blood flow, thus imposing discomfort and a risk to the safety of the patient/participant during BFR. There is a likelihood that adverse events associated with BFR have been under-reported in the literature. Second, in order to determine the effectiveness of BFR in different populations, the dose response to different relative LOPs during BFR needs to be explored further. Therefore, the determination of LOP is vital and must occur before clinicians prescribe a BFR exercise protocol.
CONCLUSION
The HH oximeter is a valid and reliable measuring device for determining the LOP in the lower extremity in healthy adults. A systematic decrease was found from the test to the retest session; therefore, it is recommend taking at least two LOP measurements with a one-minute rest interval. An additional measurement should be taken if the first two readings differ by more than 10 mmHg. It is proposed that the average of the last two readings should be used as the LOP.
Acknowledgments
AFB acknowledge University College Absalon for providing testing facilities and equipment. TLJ acknowledge the support from the management at the Centre of Rehabilitation, City of Copenhagen, Denmark. We thank Jakob Fisker, PT, for initial valuable discussion about the study.
REFERENCES
- 1.Patterson SD Hughes L Head P Warmington S Brandner C. Blood flow restriction training: a novel approach to augment clinical rehabilitation: how to do it. Br J Sports Med. 2017;51(23):1648-9. [DOI] [PubMed] [Google Scholar]
- 2.Loenneke JP Wilson JM Wilson GJ Pujol TJ Bemben MG. Potential safety issues with blood flow restriction training. Scand J Med Sci Sports. 2011;21(4):510-8. [DOI] [PubMed] [Google Scholar]
- 3.Graham B Breault MJ Mcewen JA Mcgraw RW. Occlusion of arterial flow in the extremities at subsystolic pressures through the use of wide tourniquet cuffs. Clin Orthop Relat Res. 1993;286:257-61. [PubMed] [Google Scholar]
- 4.Loenneke JP Thiebaud RS Abe T Bemben MG. Blood flow restriction pressure recommendations: the hormesis hypothesis. Med Hypotheses. 2014;82(5):623-6. [DOI] [PubMed] [Google Scholar]
- 5.Nakajima T Morita T Sato Y. Key considerations when conducting KAATSU training. Int J Kaatsu Training Res. 2011;7(1):1-6. [Google Scholar]
- 6.Spranger MD Krishnan AC Levy PD O’Leary DS Smith SA. Blood flow restriction training and the exercise pressor reflex: a call for concern. Am J Physiol Heart Circ Physiol. 2015;309(9):H1440-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noordin S McEwen JA Kragh JF Jr. Eisen A Masri BA. Surgical tourniquets in orthopaedics. J Bone Joint Surg Am. 2009;91(12):2958-67. [DOI] [PubMed] [Google Scholar]
- 8.Mattocks KT Jessee MB Mouser JG Dankel SJ Buckner SL Bell ZW et al. The Application of Blood Flow Restriction: Lessons From the Laboratory. Curr Sports Med Rep. 2018;17(4):129-34. [DOI] [PubMed] [Google Scholar]
- 9.Lixandrao ME Ugrinowitsch C Laurentino G Libardi CA Aihara AY Cardoso FN et al. Effects of exercise intensity and occlusion pressure after 12 weeks of resistance training with blood-flow restriction. Eur J Appl Physiol. 2015;115(12):2471-80. [DOI] [PubMed] [Google Scholar]
- 10.Counts BR Dankel SJ Barnett BE Kim D Mouser JG Allen KM et al. Influence of relative blood flow restriction pressure on muscle activation and muscle adaptation. Muscle & nerve. 2016;53(3):438-45. [DOI] [PubMed] [Google Scholar]
- 11.Patterson SD Brandner CR. The role of blood flow restriction training for applied practitioners: A questionnaire-based survey. J Sports Sci. 2018;36(2):123-30. [DOI] [PubMed] [Google Scholar]
- 12.Nakajima T Kurano M Iida H Takano H Oonuma H Morita T et al. Use and safety of KAATSU training: Results of a national survey. Int J Kaatsu Training Res. 2006;2(1):5-13. [Google Scholar]
- 13.Loenneke JP Fahs CA Rossow LM Sherk VD Thiebaud RS Abe T et al. Effects of cuff width on arterial occlusion: implications for blood flow restricted exercise. Eur J Appl Physiol. 2012;112(8):2903-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loenneke JP Allen KM Mouser JG Thiebaud RS Kim D Abe T et al. Blood flow restriction in the upper and lower limbs is predicted by limb circumference and systolic blood pressure. Eur J Appl Physiol. 2015;115(2):397-405. [DOI] [PubMed] [Google Scholar]
- 15.Laurentino GC Loenneke JP Mouser JG Buckner SL Counts BR Dankel SJ et al. Validity of the handheld doppler to determine lower-limb blood flow restriction pressure for exercise protocols. J Strength Cond Res. 2018; 34(9):2693-2696. [DOI] [PubMed] [Google Scholar]
- 16.Zeng Z Centner C Gollhofer A Konig D. Blood flow restriction training - validity of pulse oximetry to assess arterial occlusion pressure. Int J Sports Physiol Perform. 2019; 14(10):1408-1414. [DOI] [PubMed] [Google Scholar]
- 17.Kottner J Audige L Brorson S Donner A Gajewski BJ Hrobjartsson A et al. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64(1):96-106. [DOI] [PubMed] [Google Scholar]
- 18.Vandenbroucke JP von Elm E Altman DG Gotzsche PC Mulrow CD Pocock SJ et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500-24. [DOI] [PubMed] [Google Scholar]
- 19.Hartrick CT Kovan JP Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003;3(4):310-6. [DOI] [PubMed] [Google Scholar]
- 20.Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2:92-8. [PubMed] [Google Scholar]
- 21.Schober P Boer C Schwarte LA. Correlation coefficients: Appropriate use and interpretation. Anesth Analg. 2018;126(5):1763-8. [DOI] [PubMed] [Google Scholar]
- 22.Koo TK Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Husmann F Mittlmeier T Bruhn S Zschorlich V Behrens M. Impact of blood flow restriction exercise on muscle fatigue development and recovery. Med Sci Sports Exerc. 2018;50(3):436-46. [DOI] [PubMed] [Google Scholar]
- 24.Bland JM Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135-60. [DOI] [PubMed] [Google Scholar]
- 25.McEwen JA Inkpen KB Younger A. Thigh tourniquet safety: Limb occlusion pressure measurement and a wide contoured cuff allow lower cuff pressure. The Surgical Technologist. 2002;34(7):8-18. [Google Scholar]
- 26.Masri BA Day B Younger AS Jeyasurya J. Technique for measuring limb occlusion pressure that facilitates personalized tourniquet systems: A randomized trial. J Med Biol Eng. 2016;36(5):644-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mancia G Parati G Pomidossi G Grassi G Casadei R Zanchetti A. Alerting reaction and rise in blood pressure during measurement by physician and nurse. J Hypertens. 1987;9(2):209-15. [DOI] [PubMed] [Google Scholar]
- 28.Williams B Mancia G Spiering W Agabiti Rosei E Azizi M Burnier M et al. 2018 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC task force for the management of arterial hypertension. J Hypertens. 2018;36(12):2284-309. [DOI] [PubMed] [Google Scholar]
- 29.Mancia G Fagard R Narkiewicz K Redon J Zanchetti A Bohm M et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281-357. [DOI] [PubMed] [Google Scholar]
- 30.Ingram JW Dankel SJ Buckner SL Counts BR Mouser JG Abe T et al. The influence of time on determining blood flow restriction pressure. J Sci Med Sport. 2017;20(8):777-80. [DOI] [PubMed] [Google Scholar]
- 31.Hughes L Jeffries O Waldron M Rosenblatt B Gissane C Paton B et al. Influence and reliability of lower-limb arterial occlusion pressure at different body positions. PeerJ. 2018;6:e4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bruton A Conway JH Holgate ST. Reliability: what is it, and how is it measured? Physiotherapy. 2000;86(2):94-9. [Google Scholar]
- 33.Younger AS McEwen JA Inkpen K. Wide contoured thigh cuffs and automated limb occlusion measurement allow lower tourniquet pressures. Clin Orthop Relat Res. 2004(428):286-93. [DOI] [PubMed] [Google Scholar]
- 34.Breivik H Borchgrevink PC Allen SM Rosseland LA Romundstad L Hals EK et al. Assessment of pain. Br J Anaesth. 2008;101(1):17-24. [DOI] [PubMed] [Google Scholar]