ABSTRACT
Background
and purpose: Second anterior cruciate ligament (ACL) injury rates continue to be high, with a majority of injuries occurring soon after return-to-play, potentially because athletes may not be ready for the external load demands of the sport. Load metrics, tracked through wearable technology, may provide complementary information to standard limb symmetry indices in the return-to-play decision making process. The purpose of this case report was to quantify and monitor load using innovative technology during physical therapy rehabilitation after ACL reconstruction (ACLr) and compare to normative sport participation data.
Case Description: The subject was a 12-year-old female soccer player that suffered an ACL injury followed by surgical reconstruction with a hamstring autograft and standard rehabilitation. Single-leg hop performance, isokinetic strength, and external loads (using wearable technology) were measured longitudinally during rehabilitation and analyzed at the time of return-to-play.
Outcomes: The subject successfully achieved >90% LSI for isometric quadriceps strength (week 14), single leg hop battery (week 23), and isokinetic hamstrings (week 26) and quadriceps (week 31) strength by the time of return-to-play (week 39). At the time of return to play, external load metrics indicated that the subject's most intense rehabilitation session consisted of 36% less frequent movements, 38% lower total distances, and activity durations that were 29% lower than the expected demands of a match.
Discussion
Standard rehabilitation may underload patients relative to required sport demands. Measuring external load during the rehabilitation period may help clinicians adequately progress workload to the necessary demands of the patient's sport. With the current emphasis on restoring limb symmetry, clinicians may need to shift focus towards load preparation when returning a patient to their sport.
Level of Evidence: 4
Keywords: anterior cruciate ligament, load, rehabilitation, return to play, step count, movement system
BACKGROUND
Anterior cruciate ligament (ACL) injuries can be devastating because of the significant short- and long-term physical, psychological, and financial consequences.1,2 Most ACL ruptures are treated surgically, followed by long-term intense rehabilitation. Despite successful efforts to prevent these injuries,3 incidence rates remain high and continue to grow. In the United States, the rate of ACL reconstruction (ACLr) reached 73.6 reconstructions per 100,000 person years in 2014, up 22% over a 10-year span.4 ACL injuries are particularly high in multi-directional women's sports like soccer, which has an incident rate of 2.0 injuries per 10,000 athletic exposures.5 These numbers indicate that the rehabilitation of individuals after ACLr will continue to be common practice in orthopaedic and sports physical therapy settings.
A majority of the population that suffer ACL injuries participate in sports and desire to return to their pre-injury sport. Rehabilitation can take 6-24 months before athletes are released back to participate in their sport. However, only 83% of athletes return to some level of sport after surgery,6 65% return to their pre-injury levels of activity, and 55% return to competitive sport.7 For those that do return to sport, the risk of a second ACL injury is high. Re-rupture of the surgical graft occurs 5.2% of the time,6 and up to 20% of individuals suffer a secondary tear of the contralateral ACL.8 Moreover, many of these secondary injuries occur shortly after return to sport, with 30% occurring within the first 20 athletic exposures and 52.2% occurring within the first 72 exposures.8 These data may indicate that current rehabilitation and return to play procedures are not optimally preparing athletes for return to play or identifying athletes incapable of a safe and successful return. Clinicians commonly use a testing battery that consists of self-report functional outcome measures (i.e. International Knee Documentation Committee Questionnaire [IKDC], the Knee Injury and Osteoarthritis Outcome Score [KOOS]), symmetry measures from single-leg hopping, and isokinetic strength tests. However, poor outcomes9-11 and second injury incidence in such close proximity to return to play8,12 indicates the need for continued efforts to optimize rehabilitation and return to sport practices.
Workload management in a hot topic in the field of sports medicine. External workload, or the mechanical work done by an athlete, is an often overlooked component of rehabilitation, despite evidence that links workload to injury risk.13 The 2016 consensus statement on return to sport from the First World Congress in Sports Physical Therapy emphasizes load management and progression as key components of return to sport practice.14 Current return to sport practices with individuals after ACLr encompass self-rated functional and neuromuscular performance symmetry tests, but do not account for the on-court or on-field demands associated with the sport to which an athlete is returning. Sports have varying demands of straight line running, jumping, directional changes, accelerations, and decelerations.15 Not having the requisite fitness to return to the full demands of the sport, or the inability to display biomechanical control throughout the duration of a practice or competition could conceivably factor into the high second ACL injury rate. Thus, the purpose of this case report was to quantify and monitor workload using innovative technology (e.g. wearable technology) during physical therapy rehabilitation after ACLr and compare to normative sport participation data. Data from this case report will attempt to shape future directions for incorporating load measures into rehabilitation and return to play clinical decision making.
CASE DESCRIPTION
History
The subject was a 12-year-old female club soccer player with no significant past medical history. On the day of injury, the subject was playing as an attacker in a competitive match. In the second half of the match, she was running (self-reported 60-70% speed) after a loose ball with two defenders in close pursuit. As the subject tried to split the defenders, she lunged for the ball and attempted to cut to the left and received a slight lateral perturbation to her trunk from an oncoming defender. The subject landed with a relatively straight knee that immediately buckled into a valgus position and caused the subject to fall. She experienced immediate pain, joint effusion, and muscle inhibition and was assisted off the field and subsequently sought medical care. An MRI completed two days after injury revealed a complete acute ACL tear, lateral femoral and posterior tibial condyle contusions, moderate joint effusion, and a low-grade sprain of the proximal posterior cruciate ligament.
The subject attended four sessions of pre-operative physical therapy over four weeks prior to surgery. These sessions focused on reducing joint effusion, regaining range of motion, promoting neuromuscular control of the quadriceps, hamstrings, gastrocnemius, and hip musculature, and patient education in a home exercise program.
Surgical Intervention
The subject's surgery consisted of arthroscopically assisted ACL reconstruction using a hamstrings autograft with suspensory fixation at the femur and tibia. The graft measured 9mm at the femoral attachment and 9.5mm at the tibial attachment.
Examination
The subject's initial post-operative physical therapy evaluation was performed four days after surgical intervention. The subject had been prescribed oxycodone as needed but ceased taking at five days post-op and subsequently managed pain with Tylenol and ice. All incisions were appropriately healing with no signs of infection. Physical examination findings were unremarkable and consistent with post-operative norms. Specifically, she presented with the following impairments: moderate pain (3/10), moderate joint effusion (2 + stroke test), and reduced knee range of motion (flexion = 80 degrees, extension = -3 degrees). Functionally, per the surgeon's protocol, the subject was limited to 50-75% weight bearing for two-weeks post-operatively with the use of bilateral axillary crutches. She wore a hinged knee brace (Telescoping TROM Advance Post-op Knee Brace, DJO Global, Inc, Dallas, TX, USA) that immobilized the knee at 0 degrees for the first two weeks after surgery. Instructions from the physician allowed the brace to be unlocked as tolerated at two-weeks post-op and progress from 50% to full weight bearing as tolerated. These impairments and limitations restricted her participation in age-appropriate social and sports activities. Her primary goal was to return to soccer at her full pre-injury level.
The subject and her family agreed to participate in a research study aimed at incorporating wearable technology into rehabilitation after ACLr. The lead physical therapist (JBT) informed her and her family that rehabilitation would follow standard physician-given and evidence based protocols16 as performed in conventional post-operative rehabilitation. The wearable technology would allow the clinical team to monitor her progress, but because of the lack of evidence regarding their use, would not drive clinical decision making in her case. The family provided written informed consent and the child provided written assent to participate in the study and allow the collected data to be submitted for publication. The study was approved by the High Point University Institutional Review Board prior to patient treatment.
Rehabilitation
Rehabilitation procedures (Table 1) and decision making were performed in the context of the physician-given post-operative protocol, guidelines reported by the MOON group,16 and other current evidence.17 During the immediate post-operative phase (weeks 0-2), interventions were prescribed and performed to normalize gait, regain knee extension range of motion to neutral and knee flexion range of motion to 120 degrees, reduce effusion, care for surgical wounds, and introduce neuromuscular re-education of the lower extremity musculature (quadriceps focus). The early rehabilitation phase (post-operative weeks 2-6) focused on regaining full knee joint range of motion and progressing neuromuscular retraining to achieve functional strength and control in daily activities and a global rating of function ≥ 70%. The strengthening and control phase (post-operative weeks 7-15) emphasized maintaining full knee joint range of motion and introducing more moderate impact functional activities such as running, jumping and landing. During the advanced training phase (post-operative weeks 16-20), the focus of rehabilitation was running, jumping, and agility progressions. The final stage of rehab, the return-to-sport phase (post-operative weeks 21 to return to sport), continued to progress reactive, power, and sport-specific activities in the context of symmetrical lower extremity strength. The plan of care consisted of formal physical therapy 2x/week for 30 weeks, 1x/week thereafter until return to sport. The subject's treatment duration was not limited by any factor, with each session lasting for an average of 68 minutes. Overall, the subject completed 57 physical therapy rehabilitation sessions, equating to 1.7 visits per week. Because of the research focus of her patient care, the rehabilitation was not subject to reimbursement or treatment time constraints typical of traditional clinical settings.
Table 1.
General overview of rehabilitation program emphasis by phase.
| Early Rehabilitation | Strengthening and Control | Advanced Training | Return-to-Sport | |
|---|---|---|---|---|
| Effusion Management | XXX | X | X | X |
| Gait Normalization | XXX | XXX | XX | X |
| ROM | XXX | XX | X | X |
| Neuromuscular Control / Re-education | XXX | XXX | XX | X |
| Strength | XX | XXX | XXX | XX |
| Proprioception | XX | XXX | XX | XX |
| Endurance | XX | XXX | XXX | |
| Plyometric / Agility | X | XXX | XXX | |
| Sport-Specific | X | XX | XXX |
XXX – emphasized
XX – performed, not emphasized
X – not emphasized, used when indicated
OUTCOMES
The subject's rehabilitation timeline milestones are reported in Table 2.
Table 2.
Timeframes associated with rehabilitation milestones.
| Measure | Goal | Week achieved (post-operative) |
|---|---|---|
| Gait | Unassisted | Week 2.5 |
| Controlled single-leg squat | >70 degrees | Week 8 |
| Double-leg jumping | Initiation | Week 12 |
| Single-leg hopping | Initiation | Week 13.5 |
| Isometric quadriceps strength | >90% LSI | Week 14 |
| Running | Initiation | Week 14.5 |
| Hop battery | >90% LSI | Week 23 |
| Isokinetic hamstrings strength | >90% LSI | Week 25 |
| Isokinetic quadriceps strength | >90% LSI | Week 31 |
| Sport | Medical Clearance | Week 39 |
| Sport | Unrestricted | Week 49 |
Traditional outcome measures
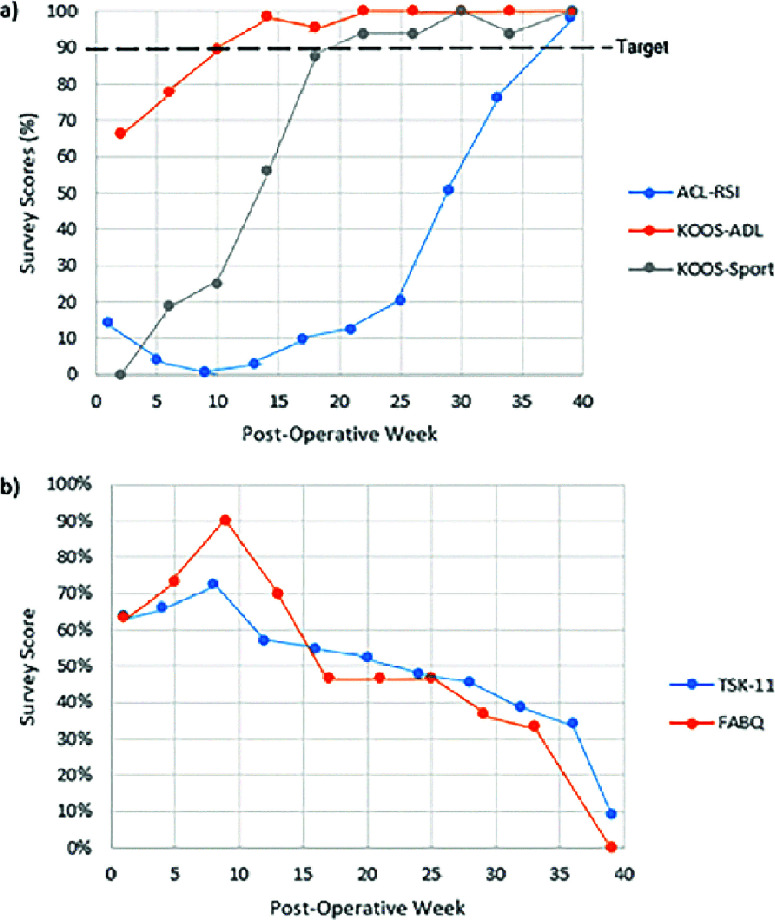
Self-perceived functional outcome measures
The subject completed a number of standard self-report functional psychological questionnaires every four weeks throughout her rehabilitation (Figure 2). Functionally, scores on the Knee Injury and Osteoarthritis (KOOS) Activities of Daily Living (KOOS-ADL) and KOOS-Sport scale reached greater than 90% at week 10 and 22, respectively. The Anterior Cruciate Ligament-Return to Sport after Injury (ACL-RSI) score, a measure of a patient's perception of readiness to return to sport, showed dramatic increases after week 25 and was greater than 90% at week 39. Fear avoidance and kinesiophobia perceptions increased from surgery to week 10. As the subject grew more confident, both scores showed consistent reductions throughout the rest of rehabilitation, bottoming out at 9% for the Tampa Scale for Kinesiophobia-11 (TSK-11) and 0% for the Fear-Avoidance Belief Questionnaire (FABQ) at the time of return to sport.
Figure 2.
Self-report a) functional and b) psychological questionnaires.
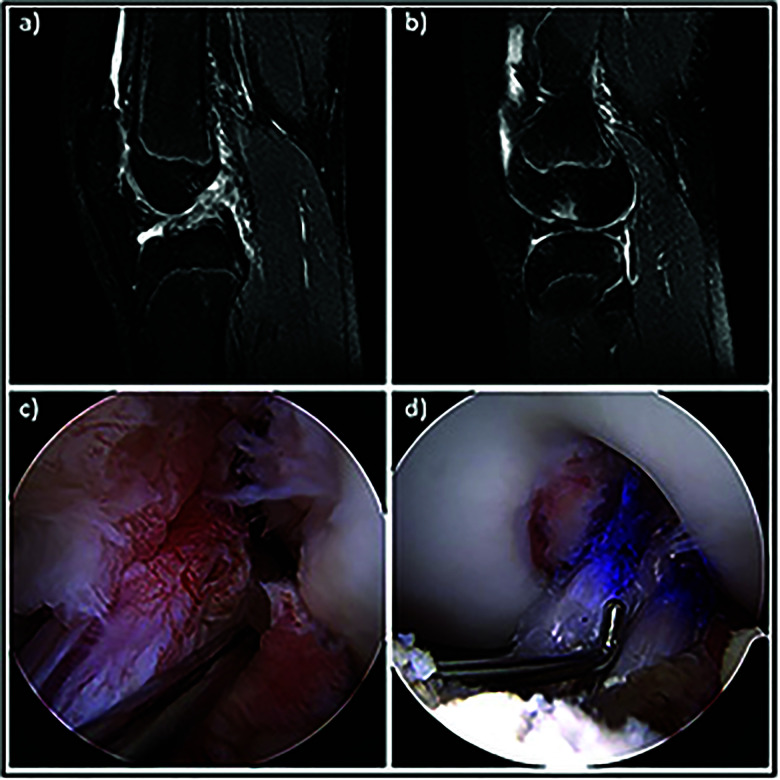
Figure 1.
Top row shows MRI sagittal slices of the subject's: a) ACL rupture and b) bone bruise pattern. Bottom row shows operative images of: a) ACL rupture and b) reconstructed ACL.
Hop battery
Standard single-leg hop battery testing was initiated at week 22 when the physical therapist decided the subject could safely perform the procedures. Repeat testing was then performed every two to four weeks thereafter to monitor the subject's progress. The battery consisted of the single-leg hop for distance, timed single-leg 6m hop, single-leg triple hop for distance, and single-leg crossover hop for distance tests. Limb symmetry indices (LSI) were calculated by dividing the involved limbs data by the uninvolved limb. 90% LSI were achieved for all single-leg hopping tests by week 23.
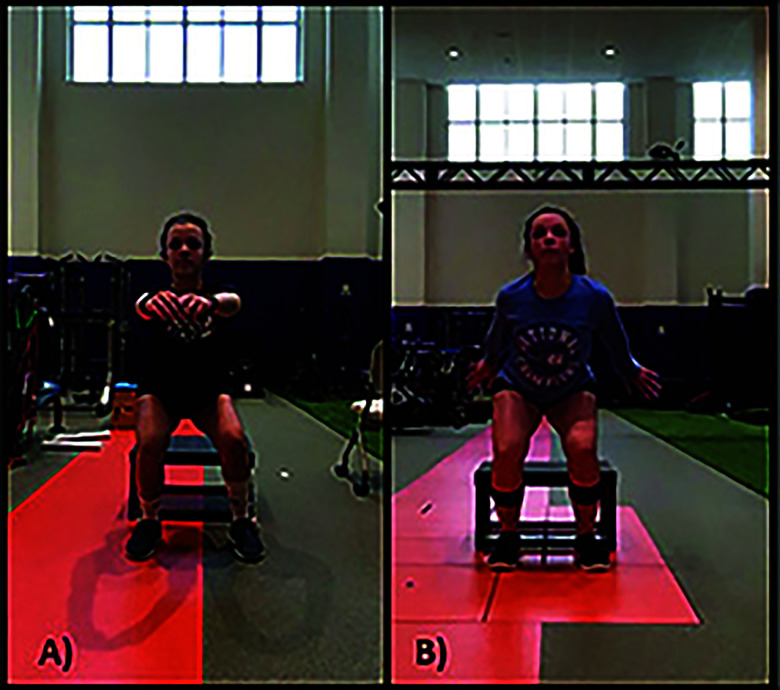
Movement quality
Movement quality was assessed weekly using the drop vertical jump test (Figure 3). The subject stood atop a 31-cm with her feet shoulder width apart. She was instructed to drop off the box with both feet at the same time, land bilaterally and subsequently perform a vertical jump for maximal height. Quality was assessed qualitatively by observation in real-time with two-dimensional video. Specifically, components of the Landing Error Scoring System (LESS), such as landing symmetry, knee flexion, and frontal plane knee control were observed. The subject needed verbal cueing for knee flexion and minor cueing with a mirror for landing symmetry before consistently exhibiting proper biomechanics for the remainder of rehabilitation.
Figure 3.
Landing biomechanics from a) drop land at 12 weeks (notice asymmetry in attempt to unload the left limb), and b) drop vertical jump at 37 weeks.
Strength Testing
Isometric strength testing of the quadriceps was initiated at week 8 in 90, 60 and 30 degrees of knee flexion using an isokinetic dynamometer (Humac NORM, CSMi, Stoughton, MA, USA). The subject's quadriceps strength progressed from ∼55% LSI to > 90% LSI at all angles by week 14. Because of the graft type, the subject performed conservative hamstring strengthening during this time and did not complete maximal isometric loading. Isokinetic strength testing at 60 and 180 degrees/sec was initiated for the quadriceps at week 16 and the hamstrings at week 24. The subject achieved > 90% LSI for the quadriceps at week 31 and for the hamstrings at week 25.
Traditional Workload Measures
Session Rating of Perceived Exertion (sRPE)
At the end of each rehabilitation session, the subject was asked to rate the intensity of the session as a sRPE. sRPE's were fairly consistent over the first six weeks of rehabilitation at 3-4/10, increased to 6-7/10 between weeks 7-17, and finished at 7-8/10 for the final 22 weeks.
Novel Workload Measures
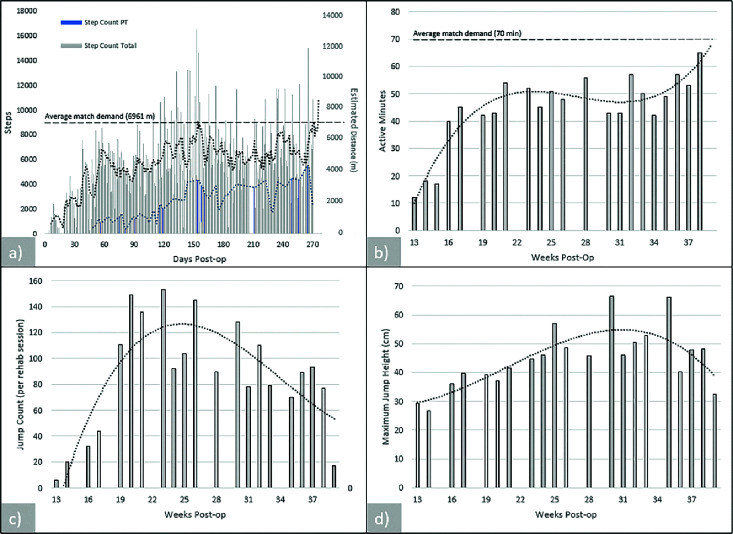
Steps and distance. To track the number of steps taken during rehabilitation sessions, a wearable activity tracker (Actigraph, Pensacola, FL, USA) was worn at waist level (weeks 7-39) throughout the duration of the rehabilitation session. Session step counts (Figure 4a) were highly variable and were dependent on the goal for the session and the time since surgery, with a maximum of 5,553 steps during the most intense rehab session in week 38. For the purpose of comparison to existing literature that has reported distance travelled in soccer matches, step count was converted to distance using her average step length (78.3 cm) during five self-paced walking trials, collected using standard 3D motion analysis techniques. Additionally, the subject wore the activity monitor during all waking hours outside of rehabilitation to quantify total daily loads (Figure 4a). On days of post-operative physical therapy, rehabilitation step count accounted for 26.5 ± 8.9% of total daily steps (maximum = 45.2%).
Figure 4.
External workload demands of: a) step count and estimated distance during rehabilitation (blue) and throughout the day (gray), b) active minutes during rehabilitation, c) jump count during rehabilitation, and d) jump height during rehabilitation.
Activity duration and distance rate
During rehabilitation, the subject also wore a tri-axial accelerometer around her waist (VERT, Mayfonk Athletic, Fort Lauderdale, FL, USA).18 Figure 4b shows the number of active minutes (number of minutes in which the accelerometer recorded an acceleration > 1G) during the most intense rehabilitation session of each post-operative week. Active minutes consistently increased from week 13 (12 mins) to week 21 (54 mins). Duration was relatively stable from week 20 to 37 (mean=50.0 ± 6.4 minutes), before reaching the maximum of 65 minutes in week 38. Distance rates were calculated for weeks 20-38 by dividing the total estimated distance in a rehabilitation session by the active minutes (mean=59.1 ± 11.2 m/min, max=77.9 m/min).
Jump workload
The accelerometer also measured the frequency (count) and intensity (height) of each jump that exceeded the minimum threshold of 15.2 cm (6 inches) during the rehabilitation sessions. Figure 4c illustrates jump frequency for the most intense rehabilitation session of each post-operative week (weeks 13-39). As plyometric progressions were introduced, the jump frequency increased rapidly and peaked at week 23. At week 23, the physical therapist determined that the subject exhibited good movement quality and fitness with the plyometric progressions, thus reducing the volume of jumping and transitioning loads to more sport-specific explosive maneuvers like direction changes and cutting. Jump performance (Figure 4d) gradually increased from week 13 (maximum jump height = 29.2 cm) to a maximum in week 35 (66.3 cm). It is worth noting that maximum jump height was not the primary focus at each rehabilitation session.
Relationship of workload measures to sport demands
Normative values from a youth (U15) women's soccer match were extracted from a previous study and compared to the data collected during rehabilitation.19 Rehabilitation workload was considerably lower than the expected workload in a normal match. When compared to normative values of total distance travelled during a competitive soccer match (6961 m),19 the rehabilitation session with the largest estimated distance (4348 m) equated to only 62% of the workload that would be expected when fully immersed in return to play. In respect to activity duration, the average rehabilitation session was only 71.4% of the expected activity duration of a game (70 mins). Similar under-loading was seen in distance rate, as the average and maximum distance rate achieved during rehabilitation was 49% and 64% of average distance rates recorded in a match.19 Conversely, because of the progressive plyometric program incorporated into the advanced phases of rehabilitation, the subject significantly over-performed jump loads relative to game demand averages (1-4 jumps).19
Discharge/Return To Sport
The subject was medically cleared (joint decision by physician and physical therapist) for restricted return to sport at post-operative week 37 after all standard tests were passed (Table 2) and the surgical graft had at least nine months to heal. The physical therapist was in constant contact with the subject's coach and family to ensure a progressive return to activity in training sessions and matches. The subject began with non-contact activities throughout practice and was slowly incorporated into contact drills within two weeks of return. After two weeks of full practice, the subject was cleared to return to game action for 10 minutes a half for the first month, increasing playing time by five minutes per half every 1-3 weeks until full safe participation was attained.
DISCUSSION
These data represent the progression of rehabilitation in an adolescent female subject after ACL reconstruction with an extremely successful short-term outcome. Results illustrate how to incorporate and quantify conventional physical performance, functional, and psychological measures with novel internal and external load measures during rehabilitation. Wearable technology is becoming more affordable, and in turn, accessible to clinical settings. While this type of technology does not currently allow for the collection of data as robust as what may be collected in a laboratory setting, it can provide clinicians unique internal and external load information that is not currently captured in conventional physical therapy settings. This case report may have immediate inexpensive translation to the clinical setting as some patients are fortunate enough to own their own wearable technology (i.e. Fitbit, iPhone) that can provide clinicians with reliable information (i.e. steps, distances) to help understand workload volume and tolerance to assist in clinical decision making,20 while other wearable technology can be purchased for nominal costs that are consistent with other physical therapy related equipment.
External workload data from this case report indicated significant under-loading of the subject during rehabilitation, despite successful outcomes. With ever-increasing demands on therapists’ time and consistently decreasing reimbursement rates, a rehabilitation paradigm shift may be necessary. Late-stage rehabilitation in the return-to-sport phase may need to shift out of the clinic and towards the field, court, or athlete's training facility. The rehabilitation team, including the patient, physician, physical therapist, family, and coach, may need to collectively develop clear plans to re-integrate the patient from a relatively low load clinical setting to a high load training session. This subject received clinical care that did not have the typical constraints that most clinics have. Fortunately, this case was part of a research study and did not require health insurance reimbursement to cover the cost of care. The physical therapist did not have a standard patient case load and was able to spend as much individualized time as needed with the subject and was able to give care in an 18,000 ft2 facility that did not lack for clinical space. Therefore, the differences observed between rehabilitation load and expected game load during “gold standard” care are likely conservative estimates compared to traditional care settings. Results may suggest that other clinicians might also be severely under-loading athletes after ACL reconstruction during rehabilitation, despite thinking that their protocols and progressions significantly intensify over time.
In this case, clinicians did not use the workload data for clinical decision-making during rehabilitation progressions, but these data clearly indicate the need to incorporate workload measures in rehabilitation to ensure sufficient progressions and comparisons to benchmarks of patients’ sports. For example, jump count and performance can be tracked in real-time. While most clinicians track plyometric progressions in terms of repetitions or sets, a total jump or impact count may provide richer data more analogous to pitch counts in upper extremity rehabilitation. While the system used to track steps taken did not provide real-time data, clinicians could easily obtain these results post-session. Progressions for impact counts, steps, or distances can also allow the clinician to track the acute:chronic workload ratio21 to ensure no sudden spikes in workload for which the patient has not yet developed the requisite fitness capacity to safely incur.
Workload measures may also prove beneficial in return-to-play decisions. Current standard physical tests look at limb symmetry indices during strength and performance tests, but do not account for the demands that an athlete will need to incur when they return to sport. In this case, rehabilitation helped the subject successfully pass the conventional testing battery in an appropriate amount of time and its hopeful that the subject will have excellent long-term outcomes. However, despite relatively consistent implementation of these tests in clinical settings, the incidence of second ACL injury is around 25%, with 30% of second injuries occurring in the first 20 exposures after return to play.8 These athletes may have exhibited symmetrical strength and power, adequate movement quality, and good perceived function, but may not have adapted to the levels needed in their sport. Previous studies have linked large spikes in workload (particularly total distance) to lower extremity injury,13 which could be representative of an athlete that returned to sport after relatively low loading in physical therapy. Clinicians could consider incorporating simulated games22 as part of the in clinic or home exercise program and monitor load both in and out of rehabilitation.
A major limitation to incorporating workload monitoring into rehabilitation is the amount of time and space needed. In this case example, 70 minutes of activity and approximately 7000 m of distance would be recommended to simulate the demands of the subject's sport.19 While having the subject obtain these loads unsupervised on a treadmill might meet the target, this single type of loading does not incorporate the multi-directional demands of the sport and does not allow the clinician to provide adequate feedback or movement quality that has been shown to predict second ACL injury.23 Future work is needed to monitor workload during rehabilitation in a cohort of patients with various clinicians and settings to verify the findings from this case report and validate these measures as a potential risk factor for second injury.
CONCLUSIONS
The results of this case report suggest that standard rehabilitation, though effective at achieving limb symmetry goals, may underload patients relative to their required sport demands. Measuring external load during the rehabilitation period may help clinicians adequately progress workload to the necessary demands of the patient's sport. With current clinical emphasis on restoring limb symmetry, clinicians may need to shift focus towards load preparation when returning a patient to their sport.
REFERENCES
- 1.Stewart BA, Momaya AM, Silverstein MD, et al. The cost-effectiveness of anterior cruciate ligament reconstruction in competitive athletes. Am J Sports Med. 2017;45:23-33. [DOI] [PubMed] [Google Scholar]
- 2.Lie MM, Risberg MA, Storheim K, et al. What's the rate of knee osteoarthritis 10 years after anterior cruciate ligament injuryϿ. An updated systematic review. Br J Sports Med. 2019;53:1162-1167. [DOI] [PubMed] [Google Scholar]
- 3.Taylor JB, Waxman JP, Richter SJ, et al. Evaluation of the effectiveness of anterior cruciate ligament injury prevention programme training components: A systematic review and meta-analysis. Br J Sports Med. 2015;49:79-87. [DOI] [PubMed] [Google Scholar]
- 4.Herzog MM, Marshall SW, Lund JL, et al. Trends in incidence of acl reconstruction and concomitant procedures among commercially insured individuals in the united states, 2002-2014. Sports Health. 2018;10:523-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montalvo AM, Schneider DK, Silva PL, et al. ‘What's my risk of sustaining an acl injury while playing football (soccer)?’ A systematic review with meta-analysis. Br J Sports Med. 2019;53:1333-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai CCH, Ardern CL, Feller JA, et al. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52:128-138. [DOI] [PubMed] [Google Scholar]
- 7.Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-1552. [DOI] [PubMed] [Google Scholar]
- 8.Paterno MV, Rauh MJ, Schmitt LC, et al. Incidence of second acl injuries 2 years after primary acl reconstruction and return to sport. Am J Sports Med. 2014;42:1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zwolski C, Schmitt LC, Quatman-Yates C, et al. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:2242-2249. [DOI] [PubMed] [Google Scholar]
- 10.Zwolski C, Schmitt LC, Thomas S, et al. The utility of limb symmetry indices in return-to-sport assessment in patients with bilateral anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2030-2038. [DOI] [PubMed] [Google Scholar]
- 11.Wellsandt E, Failla MJ Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2017;47:334-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paterno MV, Rauh MJ, Schmitt LC, et al. Incidence of contralateral and ipsilateral anterior cruciate ligament (acl) injury after primary acl reconstruction and return to sport. Clin J Sport Med. 2012;22:116-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drew MK Finch CF. The relationship between training load and injury, illness and soreness: A systematic and literature review. Sports Med. 2016;46:861-883. [DOI] [PubMed] [Google Scholar]
- 14.Ardern CL, Glasgow P, Schneiders A, et al. 2016 consensus statement on return to sport from the first world congress in sports physical therapy, bern. Br J Sports Med. 2016;50:853-864. [DOI] [PubMed] [Google Scholar]
- 15.Taylor JB, Wright AA, Dischiavi SL, et al. Activity demands during multi-directional team sports: A systematic review. Sports Med. 2017;47:2533-2551. [DOI] [PubMed] [Google Scholar]
- 16.Wright RW, Haas AK, Anderson J, et al. Anterior cruciate ligament reconstruction rehabilitation: Moon guidelines. Sports Health. 2015;7:239-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Melick N, Van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506-1515. [DOI] [PubMed] [Google Scholar]
- 18.Skazalski C, Whiteley R, Hansen C, et al. A valid and reliable method to measure jump-specific training and competition load in elite volleyball players. Scand J Med Sci Sports. 2018;28:1578-1585. [DOI] [PubMed] [Google Scholar]
- 19.Vescovi JD. Motion characteristics of youth women soccer matches: Female athletes in motion (faim) study. Int J Sports Med. 2014;35:110-117. [DOI] [PubMed] [Google Scholar]
- 20.Evenson KR, Goto MM Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int J Behav Nutr Phys Act. 2015;12:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bowen L, Gross AS, Gimpel M, et al. Spikes in acute:Chronic workload ratio (acwr) associated with a 5-7 times greater injury rate in english premier league football players: A comprehensive 3-year study. Br J Sports Med. 2019; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cone JR, Berry NT, Goldfarb AH, et al. Effects of an individualized soccer match simulation on vertical stiffness and impedance. J Strength Cond Res. 2012;26:2027-2036. [DOI] [PubMed] [Google Scholar]
- 23.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]