Abstract
Background and Purpose:
Proximal hamstring tendinopathy is a chronic, overuse condition that commonly develops in athletes. Eccentric exercise has been widely accepted in the clinic as the treatment of choice for the management of tendinopathies. However, this form of treatment has seldom been compared to other forms of load-based management for hamstring tendinopathies. Heavy slow resistance training, which consists of both concentric and eccentric phases, increases the loading time experienced by the tendon compared to eccentric only exercises. Heavy slow resistance training has achieved positive clinical results in the management of Achilles and patellar tendinopathy.
Purpose:
The purpose of this case report is to describe the outcomes of a powerlifter with proximal hamstring tendinopathy who responded favorably to a heavy slow resistance biased rehabilitation program after traditional, conservative management failed to alleviate symptoms.
Case Description:
A 31-year-old male competitive powerlifter was seen in physical therapy for the management of proximal hamstring tendinopathy. The subject had experienced long duration pain localized at the ischial tuberosity combined with hip weakness that limited his ability to lift weigtht and sit for longer than 30 minutes. Treatment included a 12-week heavy slow resistance program with the focus of increasing load intensity.
Outcomes:
Numeric pain-rating scale was assessed at baseline, after a 12-week heavy slow resistance protocol, and 12 months post protocol. Within four weeks of starting the heavy slow resistance program, the subject noted a meaningful decrease in pain. The subject experienced clinically important improvements in numeric pain-rating scale immediately after the protocol and these improvements remained 12 months after completing the protocol. The subject was able to return to competitive powerlifting after the 12-week program.
Discussion:
A meaningful change in pain occurred within four weeks of starting the program and continued improvement throughout the remainder of the 12 weeks with outcomes maintained 12 months after completing the program suggests that increasing the loading strategy with a heavy slow resistance program was helpful for this subject.
Level of Evidence:
4
Keywords: Hamstring, heavy slow resistance, eccentrics, tendinopathy
BACKGROUND AND PURPOSE
Proximal hamstring tendinopathy (PHT) is a chronic, overuse condition that develops as a result of repetitive mechanical loading at the proximal hamstring tendon.1 Tendinopathic changes are attributed to a combination of tensile loading and compressive forces applied to the common hamstring tendon near the attachment at the ischial tuberosity during movements that require the hamstrings to contract or lengthen while in hip flexion and adduction.2,3 PHT is most commonly diagnosed in sagittal plane dominant athletes such as middle and long-distance runners or in individuals who routinely perform exercises and activities that contribute to tensile and compressive loading of the proximal hamstring tendon.1 Exercises and activities thought to increase the tensile and compressive load at the proximal tendon insertion include those involving hip-flexion dominant movements such as squatting, lunging, leaning forward, stairs, uphill running, and sitting for long periods.1
The primary subjective complaint of PHT is well-localized pain of insidious onset at the ischial tuberosity that is exacerbated with sitting, driving, and activities requiring end-range hip flexion.2 PHT is often diagnosed clinically based on a detailed history and physical examination.1 Traditional treatment strategies of PHT are almost always conservative and focuses on the progressive loading of the tendon, within a pain-monitoring framework, in order to reduce pain, restore function, and prevent reinjury.1,2 Eccentric exercise, which involves isolated, slow-lengthening muscle contractions, has been widely accepted as the treatment of choice for the management of tendinopathies.4 However, recent evidence suggests that not all patients with tendinopathy respond to this intervention.5 In one study, up to 45% of patients with Achilles tendinopathy did not improve with an eccentric exercise regimen.6 Mechanisms underlying the effectiveness of eccentric training alone are poorly understood and the treatment has seldom been compared to other forms of load-based management.7 A recent systematic review reported that when load is normalized in patients with patellar and Achilles tendinopathy, eccentric loading does not lead to greater muscle-tendon recruitment than concentric and isometric contractions when external load and speed are constant.5 This suggests that load intensity rather than contraction type may be the driving stimulus. Therefore, it is not entirely clear why avoiding the concentric component should produce more favorable outcomes.8
Heavy slow resistance (HSR) training, which contains both concentric and eccentric phases, increases the loading time, or time under tension, experienced by the tendon compared to eccentric only training.8 The focus, with HSR training, is to perform slow, fatiguing, progressive resistance exercise with both concentric and eccentric components.2 Increasing a tendons time under tension leads to greater tendon adaptation.5 A recent randomized clinical trial compared HSR with traditional eccentric only exercise in the management of Achilles and patellar tendinopathy.8 Both the HSR and eccentric only groups yielded positive clinical results at 12- and 52-weeks post-treatment, however, the HSR group reported greater treatment satisfaction after 12-weeks due to the decreased time required to complete the HSR training regimen.8 Research has yet to examine the effectiveness of HSR training on the PHT or on upper extremity tendinopathies such as rotator cuff tendinopathies, common flexor tendinopathy (i.e. golfer's elbow), and common extensor tendinopathy (i.e. tennis elbow).
The purpose of this case report is to describe the outcomes of a powerlifter with PHT who responded favorably to a HSR biased rehabilitation program after traditional, conservative management failed to alleviate symptoms.
CASE DESCRIPTION
The patient was seen in physical therapy for the management of left proximal hamstring tendinopathy. The subject provided clinical information for this case presentation and signed a written form of consent.
SUBJECT HISTORY AND SYSTEMS REVIEW
The subject was a 31-year-old male competitive powerlifter that was referred to physical therapy with a differential medical diagnosis of left PHT. The subject had a history of symptomatic bilateral femoroacetabular impingement (FAI), with the presence of a cam deformity that was confirmed with imaging. The subject had undergone a bilateral hip femoroplasty and labral repair five years prior, which resolved his anterior groin pain associated with this condition. The subject was otherwise healthy and did not report any other outstanding past medical history. The subject stated that prior to seeking recent treatment for his current condition, his sports medicine physician referred him to physical therapy at a different facility with a prescription labeling his health condition as PHT. This treatment included static and dynamic hamstring stretching, hamstring soft tissue mobilization (STM), dry-needling, general hamstring strengthening exercises, and exercises that eccentrically loaded his hamstrings using body weight or manual resistance applied by the treating therapist. The subject self-discharged from physical therapy after nine visits due to lack of progress. Approximately 60 days after discharging from physical therapy, the subject discussed additional treatment options with his referring physician. The subject opted to receive a left proximal hamstring tendon tenotomy and platelet-rich plasma (PRP) injection. After the PRP procedure was performed without complication, the subject was referred to a different physical therapy clinic for treatment of his left PHT. Treatment at this facility included left hip joint self-mobilizations, active release techniques at the ischial tuberosity, proximal hamstring cupping, and free weight exercises that included kettlebell Romanian deadlifts and modified trap bar deadlifts. After four visits, the subject did not see any improvement of symptoms and self-discharged from physical therapy again due to a continued lack of progress.
When asked about his current condition, the subject stated that symptoms consistent with his left PHT were still present. The subject stated that he experienced an insidious onset of pain localized at the ischial tuberosity approximately two years prior but was able to continue powerlifting submaximally with intermittent symptoms. His one repetition maximum (1RM) lifts for the back squat and deadlift were 400 pounds and 475 pounds, respectively. The subject's primary complaint was pain that worsened with activities that required hip flexion while maintaining a neutral spine such as deadlifting, squatting, and lifting objects off of the floor. His previous physical therapists advised him to keep loaded hip extension movements during weight lifting pain free by limiting load and reducing range of motion, which resolved some of his symptoms; however, the subject continued to have pain with prolonged sitting and driving (>30 minutes). The subject rated his pain as 8/10 with prolonged sitting and driving. This affected the subject's ability to meet the expectations of his job. The subject's primary goal was to decrease pain with functional activities such as sitting and return to competitive powerlifting.
CLINICAL IMPRESSION #1
This subject appeared to be a good candidate for an alternative form of load-based management due to his history of unsuccessful physical therapy utilizing traditional, conservative treatment and ongoing subjective complaints consistent with PHT. Specifically, HSR training was considered due to its increased intensity and tendon time under tension, as compared to his previous rehabilitation loading strategy. Greater tendon time under tension has been shown to cause changes in fibril morphology and creation of new fibrils, altering the pathological tendon towards normal morphology.9 A physical examination to include standing posture, palpation, strength, ROM, special testing, functional testing consisting of visual appraisal of weight lifting movements, and self-report outcome measures was warranted. Standing posture was performed to determine if there were any flagrant bony malalignments or soft tissue asymmetries which may have developed over his two-year history of this condition. Palpation, strength, and ROM were performed to confirm PHT as the primary diagnosis. Special tests were performed to rule out other possible diagnoses. Functional testing was performed to determine if movement faults or asymmetries were present and to better understand his pain characteristics and determine prognostic factors that may suggest appropriateness for the intervention approach.
EXAMINATION
A thorough regional and global physical examination was performed on the subject by a licensed physical therapist with notable findings presented in Table 1. A postural assessment, performed in a standing position, revealed the iliac crest was elevated on the left side relative to the right side and the subject stood with a posterior pelvic tilt. While in a prone position, the subject reported mild tenderness to palpation over the left proximal hamstring tendon and its attachment at the ischial tuberosity. There was no apparent swelling, redness, or additional palpatory findings associated with this area.
Table 1.
Summary of Symptoms and Physical Exam Findings
| Symptoms | Physical Exam Findings |
|---|---|
| Localized L buttock pain, ranging from 0-8/10 | MMT results: L hip flexors (4/5), abductors (4+/5), adductors (4-/5), extensors (4+/5) |
| Pain worsens with sitting, deadlifting, driving, squatting, and bending over to pick up objects from floor | Pain with resisted hip extension and adduction during MMT |
| Decreased AROM L hip: extension 7 °, ER 10 ° | |
| 90-90 hamstring passive length test on L revealed normal extensibility, but provoked pain | |
| Tenderness to palpation at L proximal hamstring tendon and ischial tuberosity | |
| In standing, iliac crest was elevated on L relative to R side and posterior pelvic tilt was noted |
Abbreviations: left (L), right (R), manual muscle test (MMT), active range of motion (AROM), external rotation (ER)
Left hip joint active and passive ROM and strength measurements were collected in their respected standardized testing positions.10,11 Left hip extension and external rotation ROMs were limited. Hip flexion, extension, adduction, and abduction manual muscle tests were performed, with weakness noted in all planes of movement and pain upon resistance during testing of the extensors and adductors. Special tests performed on the left hip included the flexion-abduction-external rotation (FABER), flexion-adduction-internal rotation (FADIR), and hip scour tests, which were all negative.12 The left sacroiliac joint was assessed using Gaenslen's provocation test, which was negative.12
Muscle extensibility on the left extremity was assessed using the Thomas test, Ober's test, and the 90-90 hamstring length test, which were all negative.5 Although the 90-90 hamstring length test did show normal hamstring extensibility, it did reproduce the subject's concordant sign. The spine and possible sciatic nerve involvement was assessed using the quadrant test with overpressure at end-ranges and straight leg raise (SLR) test, which were both negative.12 When considering reliability, sensitivity, specificity, and likelihood ratios, evidence moderately supports the use of SLR and FABER tests; minimally supports or does not support the use of Gaenslen's provocation, FADIR, and Thomas tests; and the quadrant and hip scour tests have not been researched sufficiently to determine their value.13
Neurological testing was unremarkable for light touch sensation and deep tendon reflexes of the patellar and Achilles tendons.12 An observational gait-analysis was performed. No symptoms were reproduced with walking and no deviations were noted. The subject performed an unloaded single-leg Romanian deadlift (RDL) on the left extremity, with concordant pain increasing from a 1/10 to 5/10.
Self-report outcome measures included the Lower Extremity Functional Scale (LEFS), which is a valid and reliable measure for assessing functional impairments resulting from lower extremity musculoskeletal conditions.14 The subject scored 65/80 points, indicating a mild degree of functional limitations.
CLINICAL IMPRESSION #2
A number of pathologies can refer pain to the posterior thigh region, including piriformis syndrome, ischiogluteal bursitis, ischiofemoral impingement, lumbar disc or facet dysfunction, sacroiliac joint dysfunction, and spondylogenic lesions. These pathologies were unlikely due to findings in the examination such as pain with resisted motion into hip extension and adduction, concordant sign when the PHT is subjected to tensile and compressive loading during the single-leg RDL, tenderness to palpation over the ischial tuberosity, and negative special tests. Slight hip weakness was documented in all cardinal planes, with pain noted with resisted hip extension and adduction. This slight weakness was unlikely to have been “true” muscular weaknesses, considering the subject's experience with resistance training and 1RMs in the deadlift and back squat being 475 pounds and 400 pounds, respectively. Therefore, this slight weakness may have been a consequence of pain. His exam findings suggest that the dysfunction was contractile in nature and involved the proximal hamstring tendon.
Thus, the working clinical diagnosis was PHT. Based on these findings, it was determined that the subject would be a good candidate for HSR training due to its tendon loading properties. It was determined that a functional outcome measure would include the NPRS, which would be assessed for prolonged sitting and during weight lifting at baseline, after a 12-week HSR protocol, and 12-month post HSR protocol. Prolonged sitting and weight lifting tolerance were monitor throughout the intervention as these were his goals for physical therapy and these tasks easily reproduced his concordant sign. It was hypothesized that the subject would have clinically important improvements in sitting and weight lifting if HSR training were to be successful.
INTERVENTION
Due to the history of unsuccessful PT, the subject chose to perform this program independently as a home exercise program under the supervision of the overseeing therapist to avoid having to go into the clinic for scheduled treatment sessions. The subject performed three weekly sessions, each of which consisted of the choice of two bilateral exercises, which included: low bar back squats, sumo deadlifts, Romanian deadlifts, conventional deadlifts, trap bar deadlifts, good mornings, loaded barbell hip thrusts, and lying leg curl and the choice of one unilateral exercise, which included: single-leg Romanian deadlifts with dumbbells, single-leg hamstring curls, and reverse dumbbell lunges. These exercises were selected, in collaboration with the subject, due to their reproducibility of the concordant sign and the subject was familiar with these movements. The subject was instructed to spend three seconds completing each of the concentric and eccentric phases, respectively (i.e. 6 s/repetition).
The repetitions in reserve (RIR)-based rating of perceived exertion (RPE) scale for resistance training was used as a method to assign daily training load and intensity and aid in session-to-session and weekly load progression. The RIR-based RPE scale provides a valid measure of resistance training intensity based on how many repetitions are remaining at the completion of a set.15 This approach accounts for individual differences and ensures that the appropriate load is applied for each repetition, while reducing the risk for failure.16 Minimizing the risk for failure with this RIR scale increased the safety of the program and helped ensure the subject would be able to complete the 12-week HSR program. Some of the exercises (eg. back squat) required a spotter if the RIR was less than one and may have led to injury if this program routinely had this subject lifting to failure. The RIR used also ensured the intensity could be maintained while load was increased throughout the 12-week program. The subject initially performed all resistance exercises at a RPE of 7 (3 RIR) and progressed to a RPE of 9 (1 RIR) as the subject became more accustomed to the protocol in order to accommodate for muscular adaptation. The subject was told that moderate pain during exercises was acceptable and encouraged, but pain and discomfort was not to increase following cessation of training. A RPE of 7-9 was used to ensure adequate load intensity during the progressive loading of the tendon during these resistance exercises. These recommendations on pain were based on prior research on HSR,8 Achilles tendinopathies,17,18 and patellar tendinopathies.19,20 The subject's HSR protocol is presented in Table 2. The subject's detailed exercise program is presented in Appendix 1. Load intensities based on 1 RM are presented in Table 3. No other co-interventions were received or performed by the subject.
Table 2.
Outline of the Heavy Slow Resistance (HSR) Training Protocol and Instructions
| Sets | 3 |
| Repetitions | 6-15 |
| Pacing/tempo | 3 seconds for eccentric phase, 3 seconds for concentric phase |
| Pain allowance | Exercises should elicit moderate but not disabling pain |
| Load | Keep RPE in a range of 7 (3 RIR)- 9 (1 RIR); increase load or repetitions to maintain this range as tolerated |
| Frequency | 3x/week |
| Movement type | Each workout included: 2 bilateral exercises and 1 unilateral exercise. Subject was given a choice between these exercises: Bilateral – back squats, sumo deadlifts, conventional deadlifts, Romanian deadlifts, good mornings, barbell hip thrust, prone hamstring curl Unilateral – single leg Romanian deadlifts, single leg hamstring curls, reverse lunges |
Abbreviations: repetitions in reserve (RIR), rating of perceived exertion (RPE)
Table 3.
Load Intensities Based on 1RM
| Start of HSR Program | Week 6 of HSR Program | Peak of HSR Program |
|---|---|---|
| Back Squat: 95# (24% of 1RM) Deadlift: 115# (24% of 1RM) | Back Squat: 265# (66% of 1RM) Deadlift: 235# (49% of 1RM) | Back Squat: 365# (91% of 1RM) Deadlift: 405# (85% of 1RM) |
Abbreviations: 1RM = one repetition maximum, HSR = heavy slow resistance, # = pounds
The subject chose to perform this plan of care independently at home. The physical therapist followed up with the subject via email, phone, or text every two weeks during the 12-week HSR program. These follow up conversations focused on monitoring program compliance; collecting data related to pain, sitting tolerance, and weight lifting tolerance; and offering encouragement.
OUTCOME
Following a 12-week independent rehabilitation program utilizing HSR training, the subject showed functional improvement and was able to return to competitive powerlifting with minimal pain. Additionally, prolonged sitting and driving was no longer an aggravating activity for the subject. Numeric pain-rating scale (NPRS) was verbally assessed at baseline, after a 12-week HSR protocol, and 12 months post HSR protocol. An 11-point NPRS (0, no pain; 10, worst imaginable pain) was used to assess the intensity of pain during weight lifting and prolonged sitting. The NPRS has been shown to possess strong reliability and validity.21 During the fourth week of this 12-week HSR protocol, the subject noted that his pain decreased a meaningful amount both while weight lifting and with prolonged sitting. The subject reported that this improvement provided encouragement to remain compliant with the remainder of the protocol. The subject experienced clinically important improvements in NPRS immediately after the HSR protocol and these improvements remained one year after completing the HSR protocol. NPRS decreased 6 points during lower body weight lifting exercises and 7 points during prolonged sitting.
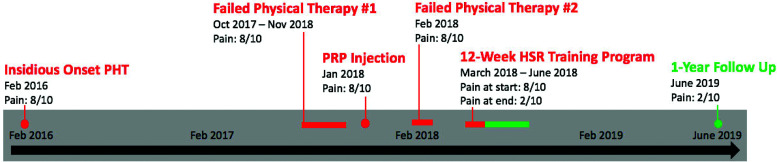
A subject management timeline with numeric pain-rating scale outcomes are depicted in Figure 1. The subject was instructed to continue this program without reservation and follow-up with the treating therapist if symptoms returned. Outcomes for the subject are summarized in Table 4.
Figure 1.
Patient management timeline from February 2016 to June 2019 with related numeric pain-rating scale outcomes before, during, and after novel treatment. Abbreviations: proximal hamstring tendinopathy (PHT), plasma-rich platelet (PRP), heavy-slow resistance (HSR)
Table 4.
Visual Analogue Scale and Patient's Functional Goals
| Outcome Measure | Initial Assessment | 12 Weeks | 12 Month Follow Up |
|---|---|---|---|
| Visual Analogue Scale | 8/10 | 2/10 | 2/10 |
| Self-Reported Function | Unable to sit > 30 minutes due to pain | 2/10 with sitting > 30 minutes | 2/10 with sitting > 60 minutes |
| Pain caused patient to discontinue performing loaded hip extension movements during weightlifting | 1/10 with weight lifting | 1/10 with weight lifting |
DISCUSSION
This case report describes the clinical reasoning and the physical therapy management of a subject with chronic PHT who was not able to return to his prior level of functioning (prolonged sitting and weight lifting) with previous interventions consisting of hamstring stretching, soft tissue and joint mobilization, dry-needling, low load and intensity hamstring strengthening, eccentric exercises using the subject's body weight, cupping, and PRP injection. The subject reported minimal short-term effects and no long-lasting effects to the aforementioned interventions. The primary goal in tendinopathy rehabilitation is improving the capacity of the tendon to manage load. There is evidence that tendons are highly responsive to diverse active loading strategies22,23,24 while there is minimal evidence to support the efficacy of the use of manual therapy for the management of tendinopathy.25
Because previous physical therapy and medical interventions were not effective for this subject, a HSR program was proposed in an attempt to increase the load intensity of the rehab program, as well as the PHT's time under tension, in order to reduce pain and restore function. Within four weeks of starting this HSR program, the subject noted a meaningful decrease in pain, which help to provide motivation to remain compliant with the entire 12-week program. This short time to improvement is similar to the time frame reported in previous research on tendinopathies after initiating a load-based exercise strategy.26,27 The ability to experience a meaningful decrease in pain within four weeks likely contributed to the subject's compliance with the independent 12-week HSR protocol, due to the fact that the subject self-discharged from physical therapy on two separate occasions due to lack of progress. This early improvement indicated that the techniques and dosages used were probably appropriate. After completing a 12-week HSR program, this subject was able to sit and participate in his usual weight lifting regimen with minimal pain, after being restricted in these activities during the prior 18 months. The subject started the HSR protocol lifting 24% of his 1RM for back squat (95 pounds) and deadlift (115 pounds), and progressed to using a load that corresponded to 91% of 1RM for back squat (365 pounds) and 85% of 1RM for deadlift (405 pounds) during the HSR protocol. This supports the goal of increasing his load intensity of his rehab program. Although a case report of a single subject does not infer cause-and-effect relationship, a meaningful change within four weeks of starting the program and continued improvement throughout the remainder of the 12-week program, and the fact that the outcomes remained 12 months after completing the program, suggests that increasing the loading strategy with a HSR program was helpful.
As demonstrated in Appendix 1, the subject was not fully compliant with performing his HSR program three times each week or performing three exercises per training session. This suggests that there may have been benefit from the HSR protocol even with a lower training frequency than was intended. Previous research comparing HSR and eccentric only protocols noticed improved satisfaction with the HSR group due to the decreased time required to complete the HSR training program as compare to an eccentric only protocol.8 The subject of this case report responded with a lower frequency than previously discussed. Due to previously reported benefits seen with the lower frequency HSR protocol, future studies designed to look at the effect of frequency on outcomes are warranted.
Previous research on HSR has shown positive clinical results in the management of Achilles and patellar tendinopathies.8 This case report is the first study to demonstrate a favorable response to a HSR program in a subject with PHT. Relevant in this case is the unique anatomical features of the PHT that differ from the Achilles and patellar tendons. The PHT has thick soft tissue coverage as well a close location to the sciatic nerve. Anatomically, the semitendinosis, semimembranosis, and long head of biceps femoris tendons insert on the ischial tuberosity,28 with the inferior border of the gluteus maximus and the sciatic nerve having close proximity to the ischial tuberosity and proximal hamstring tendons. Due to these anatomical features, the general recommendations for treatment of tendinopathies have been questioned in terms of effectiveness and safety for PHT. This case report supports the notion that load intensity rather than contraction type is the optimal stimulus for the management of tendinopathies, including PHT.
This case report has multiple limitations. First, the subject received many therapeutic exercise interventions prior to initiating the HSR program and some of the HSR program movements were very similar to the previous exercises, which may have impacted his overall success. Nevertheless, as the exercise program was unsuccessful as previously implemented, it seems that increasing the intensity of the load and PHT's time under tension via a HSR program may have led to better outcomes. Second, the subject also received a PRP injection eight weeks prior to initiating the HSR program. While there is evidence suggesting that PRP for the treatment of PHT is ineffective, there is also evidence supporting the use of PRP injections to manage PHT especially after failed conservative care.29,30,31 It should also be acknowledged that some investigators claim that the best clinical benefit of PRP injections occurs in the long-term period (>12 months) which was included in the time span of this case report.32 Third, the natural recovery of PHT may have impacted the results for this subject.33 Although the time to full recovery for PHT is normally one to three months, the time to full recovery from tendon injuries can take more than a year, especially in patients that fail conservative treatment.34 Finally, in this case report, the clinician and the subject were not able to be blinded to the treatment or outcomes, which could have biased the results.
As the results of a single case report cannot be generalized to other patients, additional research is needed to determine the effectiveness of this protocol in a greater number of subjects. Performing a case series or eventually designing a randomized controlled trial that uses a greater number of participants, utilizes a control group, and blinds researchers would be helpful in determining the effectiveness of HSR training in the management of PHT.
CONCLUSION
This case report describes the management of a subject with chronic PHT. Physical therapy intervention consisted of an independent 12-week HSR protocol. The results of this case report indicate that load intensity rather than contraction type is the optimal stimulus for the management of PHT. The subject experienced clinically meaningful changes in pain and functional status at 12 weeks, and these changes remained at the 12 month follow up.
APPENDIX 1.
HEAVY SLOW RESISTANCE TRAINING EXERCISE PROGRESSION OVER 12 WEEKS
| Week | Exercises, Loads, Sets, Reps | ||
|---|---|---|---|
| 1 | Session 1 | Session 2 | Session 3 |
| BS: 95# 3×15 Barbell Hip Thrust: 55# ×l2,65# 2×12 Standing SL Curl: 10# 3×12 | BS: 135# ×l5,155# 2×15 DL:115#×l0,135# 2×10 Standing SL Curl: 10# 3×10 | BS: 165# 2×15,165# ×l2 Barbell Hip Thnist: 60# 2×15, 50#×l2 Lying Leg Curl: 30# ×l5,40# 2×15 | |
| 2 | Session 4 | Session 5 | Session 6 |
| Trap Bar DL: 290# 3×12 Barbell Hip Thrust: 65# 3×12 Lying Leg Curl: 50# ×l2, 55# 2×12 | BS: 185# 3×12 DB Lunge: 20# 3×12 Standing SL Curl: 10# ×10, 10# 2×12 | BS:185# 3×12 DB Lunge: 20# 4×12 Standing SL Curl: 10# 3×12 | |
| 3 | Session 7 | Session 8 | |
| BS: 185# ×l2,205# 2×12 Lying Leg Curl: 45# ×l2, 50# 2×12 SL Romanian DL: 0# 3×15 | BS: 205# 3×12 Romanian DL: 95# 3×12 Lying SL Curl: 15# ×l2,20# 2×12 | ||
| 4 | Session 9 | Session 10 | Session 11 |
| BS: 225# 4×10 Romaman DL: 135# ×10, 155# 2×10 Lying SL Curl: 20# ×10, 25# 2×10 | BS: 225# 2×10,230# 2×12 GM: 105# ×10, 115# 2×10 Reverse DB lunge: 20# ×10, 25# 2×10 | BS: 235# ×10, 245# 3×10 GM: 135# 2×10,145# ×10, 155# ×10 Lying SL Curl: 20# 4×10 | |
| 5 | Session 12 | Session 13 | Session 14 |
| BS: 255# 4×10 Romaiiian DL: 175# ×10, 185# 2×10 Reveise DB Lunge: 25# 3×10 | BS: 255# ×10, 265# 3×10 GM: 135# ×10, 155# 2×10, 160# ×10 Reverse DB Lunge: 25# 3×10 | BS: 275# 2×10,275# ×9,275# ×8 Romanian DL: 205# 3×10 Lying SL Curl: 20# ×10, 25# 2×10 | |
| 6 | Session 15 | Session 16 | Session 17 |
| BS:265#×8,275#×8,285# ×8 DL: 205# ×8,225# ×8,235# ×8 Reverse DB Lunge: 35# 3×8 | Sumo DL: 285# ×8,315# 2×8 GM: 135# ×8,165# 3×8 Lying SL Curl: 25# 3×8 | BS: 295#×8,315#×8,315#×7 DL: 255# ×8,265# ×8,275# ×8 SL Romanian DL: 35# 3×8 | |
| 7 | Session 18 | Session 19 | Session 20 |
| Sumo DL: 335# ×8,345# 2×8 GM: 165# ×8,170# ×8. 175# 2×8 Reverse DB Lunge: 40# 3×8 | BS:295#×8,315#3×8 Romanian DL: 235# ×8,245# ×8,255#×8 SL Seated Leg Curl: 45# ×8, 50# 2×8 | BS: 320# ×8,325# 2×7 DL: 285# ×8,295# 2×8 SL Romanian DL: 55# 3×8 | |
| 8 | Session 21 | Session 22 | |
| BS:315#×8,325# 2×8, 330# ×8 Romanian DL: 255# 2×8, 260# 2×8 SL Seated Leg Curl: 40# ×8,45#2×8 | Sumo DL: 335# ×8,355# ×8, 375# ×8 GM: 175# ×8,185# 3×8 Reverse DB Lunge: 40# 3×8 | ||
| 9 | Session 23 | Session 24 | Session 25 |
| BS: 325#×8,335#×7,335# ×8 Romanian DL: 260# ×8, 265# 2×8 SL Seated Leg Curl: 40# ×8,45#2×8 | SumoDL: 375# ×8,385# ×8, 395# ×8 GM: 175#×8,185#×8,190# ×8 SL Seated Leg Curl: 45# ×8, 50# 2×8 | BS:315#×6,320# ×6,325# 2×5 Reverse DB Lunge: 35# 3×8 | |
| 10 | Session 26 | Session 27 | Session 28 |
| BS:285#×6,295#×6,315# ×6 DL:245#×8,255#×8,265# ×8 | SumoDL: 405# ×8,405# 3×6 GM: 185# ×5,195# 2×6 SL Seated Leg Curl: 50# 3×8 | BS:315#×6,335# ×6,345# 2×6 Romanian DL: 275# 3×6 Barbell Hip Thrust: 95# 4×8 | |
| 11 | Session 29 | Session 30 | Session 31 |
| BS: 335#×6,345#×6,355# ×6 Romanian DL: 285# 3×6 SL Hip Thrust: 45# ×8,45# 2×10 | BS:315#×6,325# 2×6,330# ×6 Barbell Hip Thrust: 105# 3×8 SL Romanian DL: 35# ×10, 45# 2×10 | Barbell Hip Thrust: 135# 4×10 SL Romanian DL: 55# 3×10 | |
| 12 | Session 32 | Session 33 | Session 34 |
| BS:315#×6,320#×6,325# ×6 Barbell Hip Thrust: 145# 3×8 SL Romanian DL: 40# ×8, 50# 2×8 | BS: 355# ×6,365#×6,315#×6 Barbell Hip Thrust: 155# 3×8 SL Romanian DL: 50# 3×10 | Romanian DL: 255# ×6,265# ×6,275# ×6 Barbell Hip Thrust: 155# ×8, 165# 2×8 Reverse DB Lunge: 35# 3×10 | |
REFERENCES
- 1.Beatty NR, Félix I, Hettler J, et al. Rehabilitation and prevention of proximal hamstring tendinopathy. Curr Sports Med Rep. 2017;16(3):162-171. [DOI] [PubMed] [Google Scholar]
- 2.Goom TS, Malliaras P, Reiman MP, et al. Proximal hamstring tendinopathy: Clinical aspects of assessment and management. J Orthop Sports Phys Ther. 2016;46(6):483-93. [DOI] [PubMed] [Google Scholar]
- 3.Docking S, Samiric T, Scase E, et al. Relationship between compressive loading and ECM changes in tendons. Muscles, Ligaments Tendons J. 2013;3(1)7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling: 2 case reports. J Orthop Sports Phys Ther. 2014;44(3):198-205. [DOI] [PubMed] [Google Scholar]
- 5.Malliaras P, Barton CJ, Reeves ND, et al. Achilles and patellar tendinopathy loading programmes: A systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med. 2013;43(4):267-86. [DOI] [PubMed] [Google Scholar]
- 6.Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport. 2007;10(1):52-8. [DOI] [PubMed] [Google Scholar]
- 7.Kongsgaard M, Kovanen V, Aagaard P, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sports. 2009;19(6):790-802. [DOI] [PubMed] [Google Scholar]
- 8.Beyer R, Kongsgaard M, Hougs Kjær B, et al. Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy: A randomized controlled trial. Am J Sports Med. 2015;43(7):1704-11. [DOI] [PubMed] [Google Scholar]
- 9.Kongsgaard M, Qvortrup K, Larsen J, et al. Fibril morphology and tendon mechanical properties in patellar tendinopathy: Effects of heavy slow resistance training. Am J Sports Med. 2010;38(4):749-756. [DOI] [PubMed] [Google Scholar]
- 10.Kendall FP, McCreary EK, Provance PG, et al. Muscles: Testing and Function, with Posture and Pain (5th Edition). Philadelphia: Lippincott, Williams, and Wilkins: 2005 [Google Scholar]
- 11.Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry (5th ed.) Philadelphia: F.A. Davis: 2016 [Google Scholar]
- 12.Dutton M. Dutton's Orthopaedic Examination, Evaluation, and Intervention (4th Edition). New Yord: McGraw-Hill Education: 2017 [Google Scholar]
- 13.Cook CE, Hegedus EJ. Orthopedic Physical Examination Tests (2nd Edition). Upper Saddle River, New Jersey: Pearson Eduction, Inc: 2013 [Google Scholar]
- 14.Mehta SP, Fulton A, Quach C, et al. Measurement properties of the lower extremity functional scale: A systematic review. J Orthop Sports Phys Ther. 2016;46(3):200-16. [DOI] [PubMed] [Google Scholar]
- 15.Helms ER, Cronin J, Storey A, et al. Application of the repetitions in reserve-based rating of perceived exertion scale for resistance training. Strength Cond J. 2016;38(4):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zourdos MC, Klemp A, Dolan C, et al. Novel resistance training-specific rating of perceived exertion scale measuring repetitions in reserve. J Strength Cond Res. 2016;30(1):267-75. [DOI] [PubMed] [Google Scholar]
- 17.Gravare Silbernagel K, Crossley KM. A proposed return-to-sport program for patients with midportion Achilles tendinopathy: Rationale and implementation. J Orthop Sports Phys Ther. 2015;45(11):876-886. [DOI] [PubMed] [Google Scholar]
- 18.Alfredson H, Pietila T, Jonsson P, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26(3):360-366. [DOI] [PubMed] [Google Scholar]
- 19.Young MA, Cook JL, Purdam CR, et al. Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br J Sports Med. 2005;39(2):102-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malliara P, Cook J, Purdam C, et al. Patellar tendinopathy: Clinical diagnosis, load management, and advice for challenging case presentations. J Orthop Sports Phys Ther. 2015;45(11):1-33. [DOI] [PubMed] [Google Scholar]
- 21.Jensen MP, Miller L, Fisher LD. Assessment of pain during medical procedures: a comparison of three scales. Clin J Pain. 1998;14:343-349 [DOI] [PubMed] [Google Scholar]
- 22.Childress MA, Beutler A. Management of chronic tendon injuries. Am Fam Physician. 2013;87(7):486-90 [PubMed] [Google Scholar]
- 23.Bohm S. Mersmann F. Arampatzis A. Human tendon adaptation in response to mechanical loading: A systematic review and meta-analysis of exercise intervention studies on healthy adults. Sports Medicine – Open. 2015;1(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diehl P, Gollwitzer H, Schauwecker J, et al. Conservative treatment of chronic tendinopathies. Orthopade. 2014;43(2):183-193. [DOI] [PubMed] [Google Scholar]
- 25.Bennett A, Watson T, Simmonds J. The efficacy of the use of manual therapy in the management of tendinopathy: A systematic review. Br J Sports Med. 2014;48:A11-A12. [Google Scholar]
- 26.Rauseo C. The rehabilitation of a runner with iliopsoas tendinopathy using an eccentric-biased exercise: A case report. Int J Sports Phys Ther. 2017;12(7):1150-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cushman D, Rho ME. Conservative treatment of subacute proximal hamstring tendinopathy using eccentric exercises performed with a treadmill: A case report. J Orthop Sports Phys Ther. 2015;45(7):557-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sato K, Nimura A, Yamaguchi K, et al. Anatomical study of the proximal origin of hamstring muscles. J Orthop Sci. 2012;17(5):614-618. [DOI] [PubMed] [Google Scholar]
- 29.Levy GM, Lucas P, Hope N. Efficacy of a platelet-rich plasma injection for the treatment of proximal hamstring tendinopathy: A pilot study. J Sci Med Sport. 2019;22:247-252. [DOI] [PubMed] [Google Scholar]
- 30.Davenport KL, Campos JS, Nguyen J, et al. Ultrasound-guided intratendinous injections with platelet-rich plasma or autologous whole blood for treatment of proximal hamstring tendinopathy. J Ultrasound Med. 2015;34:1455-1463. [DOI] [PubMed] [Google Scholar]
- 31.Fader RR, Mitchell JJ, Traub S, et al. Platelet-rich plasma treatment improves outcomes for chronic proximal hamstring injuries in an athletic population. Muscles, Ligaments Tendons J. 2014;4(4):461-466. [PMC free article] [PubMed] [Google Scholar]
- 32.Franchini M, Cruciani M, Mengoli C, et al. Efficacy of platelet-rich plasma as conservative treatment in orthopaedics: A systematic review and meta-analysis. Blood Transfus. 2018;16:502-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neilsen RD, Ronnow L, Rasmussen S, et al. A prospective study on time to recovery in 254 injured novice runners. PLoS One. 2014;9(6):e99877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lempainen L, Johansson K, Banke IJ, et al. Expert opinion: Diagnosis and treatment of proximal hamstring tendinopathy. Muscles, Ligaments Tendons J. 2015;5(1):23-28. [PMC free article] [PubMed] [Google Scholar]