Abstract
Objective The present study verified, through a systematic review with meta-analysis, the effects of a rehabilitation, physical training program for the treatment of pain and muscle strength in knee osteoarthritis (OA).
Methods We analyzed studies published between 2008 and 2018 referenced at the Medline (National Library of Medicine) database, selecting 7 randomized controlled clinical trials about exercise programs to improve pain and muscle strength in patients with knee OA with Physiotherapy Evidence Database (PeDro) score higher than 8. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) systematization was used to prepare this review, and a meta-analysis was carried out to obtain mathematical evidence the outcomes of physical exercise on pain.
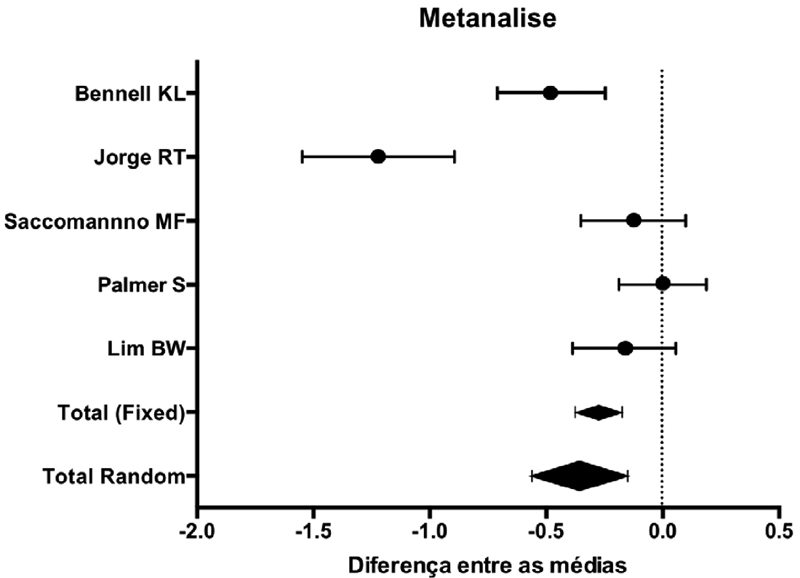
Results The studies included in the analysis contained a total of 934 participants aged 40 to 73 years-old, with 34.90% males. Most of the exercise sets offered in OA treatment had a significantly positive outcome result in both criteria, but mainly for pain relief (statistically significant difference, p < 0.003).
Conclusion We infer that there was an improvement of pain in all articles that performed muscle strengthening, but there is still an obstacle to the protocols used.
Keywords: pain, muscle strength, osteoarthritis of knee, exercise and movement techniques
Introduction
Population aging has grown all over the world, increasing the health challenges, especially with regard to the large number of conditions affecting the elderly. Among them, osteoarthritis (OA) stands out. 1 According to Framingham, OA is the second cause of work absenteeism and the main cause of disability in the elderly. 2
Osteoarthritis is as a degenerative and progressive non-inflammatory joint disease consisting of articular cartilage degradation and subchondral bone alterations. 3 This condition affects the normal synchronous movement of the joint, resulting in pain, stiffness, muscular strength deficit, and joint instability, which can reduce the individual's functional mobility and lead to functional loss. 4 However, it is believed that OA does not result from the aging process, but from biochemical changes and biomechanical stresses affecting joint cartilage. 5 6
As such, it is known that knee OA mostly affects females, since, anatomically, in females, the cartilage of this region is thinner, with smaller area and volume, resulting in an increased shear force at the site. 7
In a randomized controlled trial, Nguyen et al. 8 have shown that exercise therapy is successful in improving the physical performance of patients with knee OA and severe comorbidities. In line with this information, the updated 2014 guidelines from the Osteoarthritis Research Society International (OARSI) considered rehabilitation as the main treatment for OA. Through a meta-analysis, OARSI concluded that exercise therapy associated with strength training and aerobic activity reduced pain and improved the individual's physical function. 8 9
In a systematic review, Lange et al. 10 evaluated the efficacy of resistance training in the management of knee OA. They observed a general improvement in the symptoms and physical performance of the patients; in addition, these authors verified that more than half of the included studies reported success in the application of resistance training as physical function and muscular strength, which improved significantly when compared to the groups receiving standard care. 9 10
Tanakar et al., 11 in a systematic review with meta-analysis of randomized clinical trials, pointed out that aerobic exercises associated with non-weight-bearing strengthening exercises were more effective in relieving pain in short-term activities. However, the literature reports that balance exercises, endurance training and aerobic exercises are associated with pain reduction, stiffness relief, and physical function improvement in patients with knee OA. 12 13 14 15
As such, we need to understand the efficacy of physical training over knee OA impact factors. There are several evidences 12 13 16 17 on the benefits of some knee OA rehabilitation methods, but the ideal treatment regimen for each condition is still in question. These rehabilitation methods include physical training using methods or programs to promote, maintain or restore the physical and physiological well-being of an individual. 18
Thus, this study aims to verify controlled and randomized studies through a systematic review of the effects of a rehabilitation, physical training program for pain management and muscle strength in knee OA.
Methods
The most relevant studies originally published in English at the MEDLINE (National Library of Medicine), Scientific Electronic Library Online (SciELO), and Latin American and Caribbean Literature in Health Science database (LILACS) databases between January 2008 and December 2018 were included in our analysis. To select studies with the highest scientific evidence, only randomized controlled clinical trials (RCTs) were used for the bibliographic review. The search for scientific papers contained the following combinations of keywords: movement techniques exercise , knee osteoarthritis AND pain AND muscle strength AND proprioception training , as well as their variations at Medical Subject Headings (MeSH).
Inclusion and exclusion criteria are shown in Box 1 .
Box 1. Inclusion and exclusion criteria.
| Inclusion criteria |
| Study design: randomized controlled clinical trials |
| Intervention: exercise programs for pain and muscular strength improvement in patients with knee osteoarthritis |
| Only in human subjects |
| Language: English |
| Studies performed at the last 10 years |
| Exclusion criteria |
| Intervention: unclear, poorly described or inadequate |
| Publication form: only abstracts |
| Main variables analyzed |
| Knee pain |
| Muscle strength |
The studies were selected by two independent reviewers; those not related to the review subject or presenting some kind of bias were excluded. To verify the validity of eligible randomized trials, pairs of reviewers working independently and reliably determined the adequacy of randomization regarding exercise protocols performed by the control and intervention groups.
Next, the abstracts of the selected papers were analyzed to identify those meeting the inclusion and exclusion criteria. Papers that did not have any of the study outcomes, did not address knee OA, did not have a specific group, or did not perform any type of exercise, in addition to those that were study protocols, were excluded.
The relevant papers were submitted to a final evaluation according to their score in the Physiotherapy Evidence Database (PEDro) scale to help researchers quickly identify which ones have internal validity and enough statistical information for results interpretation. To be eligible for this systematic review, a minimum PEDro score of eight was required. In addition, the scale proposed by Jadad et al. 19 was employed. This scale consists of 5 criteria, ranging from 0 to 5 points, and a score lower than 3 indicates that the study has low methodological quality and that its results will hardly be extrapolated for other scenarios.
Results
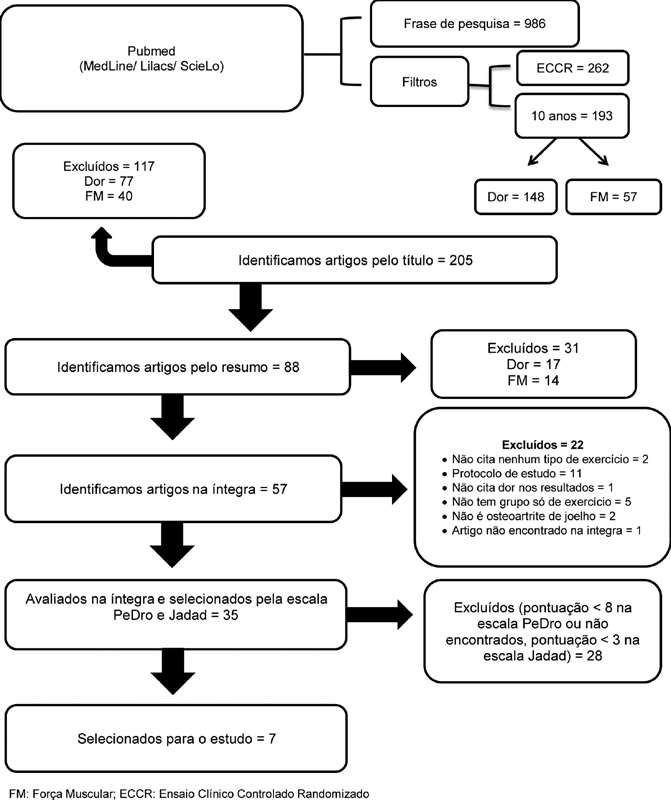
Based on the previously described keywords, 986 papers were selected from the MedLine, Lilacs, and ScieLo databases. After applying all inclusion and exclusion criteria, 35 papers were read and evaluated using the PEDro and the Jadad scales. Seven papers were considered relevant for our systematic review, as shown in Figure 1 .
Fig. 1.
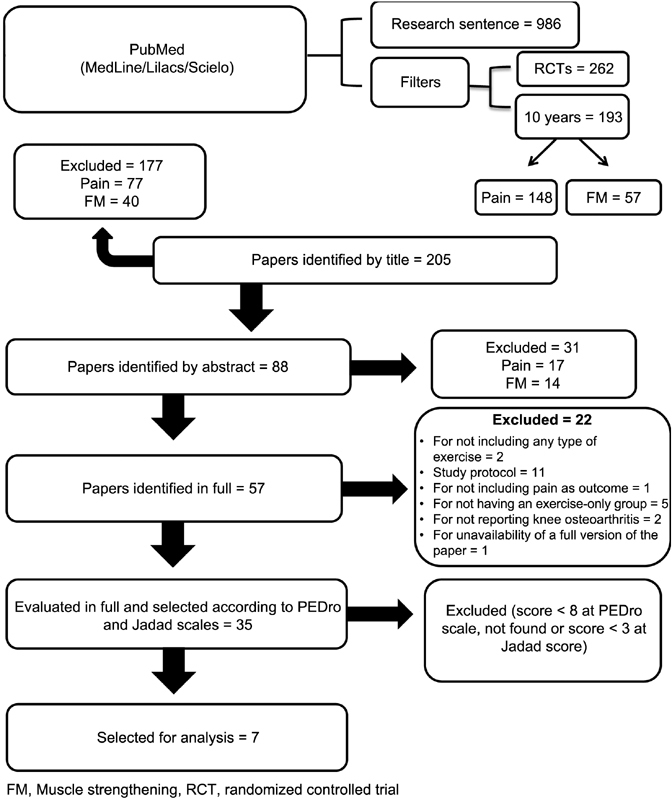
Flow chart.
Tables 1 and 2 show the PEDro and Jadad scores of the 7 studies included in this systematic review, with a minimum score of 8 points in 11 papers and 3 points in 5 papers, respectively.
Table 1. Physiotherapy Evidence Database scale.
| PEDro Scale | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | C10 | C11 | Score |
| Boon-Whatt Lim et al., 2008 33 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
| K.L. Bennell et al., 2010 25 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
| G. Kelley Fitzgerald et al., 2011 20 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 8/10 |
| Saccomanno MF et al., 2016 21 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
| Palmer S et al., 2014 22 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 8/10 |
| Holsgaard-Larsen A et al., 2017 23 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
| Jorge RT et al., 2015 24 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8/10 |
Abbreviation: PEDro, Physiotherapy Evidence Database.
Table 2. Jadad scale.
| Items | Boon-Whatt Lim et al., 2008 32 | K.L. Bennell et al., 2010 24 | G. Kelley Fitzgerald et al., 2011 19 | Sacco manno MF et al., 2016 20 | Palmer S et al., 2014 21 | Holsgaard-Larsen A et al., 2017 22 | Jorge RT et al., 2015 23 |
|---|---|---|---|---|---|---|---|
| Was the study described as randomized? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Was there a description of randomization? Was it adequate? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Were there comparisons and results? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Was there a description of comparisons and results? Were they adequate? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Was there a description of withdrawals and dropouts? | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| TOTAL | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
The studies included in the analysis contained a total of 934 participants aged 40 to 73 years-old, with 34.90% of the subjects being male. The studies evaluated the effectiveness of an exercise set for knee OA management, and some compared the exercises with other treatment techniques, which took place over a mean period of 12 weeks. The analyzed variables were pain and muscle strength, and most exercises sets for OA treatment led to significantly positive outcomes for both variables, but mainly pain, as shown in Table 3 .
Table 3. Summary of studies and their main results on muscle strength and knee pain.
| Study | SAMPLE | GI | GC | Duration | Analyzed variables | ||||
|---|---|---|---|---|---|---|---|---|---|
| SAMPLE | MEN | AGE | GROUPS | PAIN | MUSCLE STRENGTH | ||||
| Lim et al., 2008 33 | 107 | 48 | 53–73 years old | GI: 54 GC: 53 |
Quadriceps strengthening with weighted shin sleeves and Theraband | No intervention | 12 weeks | Significant pain improvement in the group with better knee alignment | NA |
| K.L. Bennell et al., 2010 25 | 102 | 51 | 62–73 years old | GI: 51 GC: 51 |
Hip strengthening l (quadriceps adduction, external rotation, extension and isometry) | No intervention | 12 weeks | Pain improvement in GI compared to GC | Significant hip and quadriceps strength improvement compared to the control group |
| G. Kelley Fitzgerald et al., 2011 20 | 183 | 61 | 63–73 years old | GI:92 GC: 91 |
The agility and disturbance group received the same standard exercise program with the addition of training techniques on agility and disturbance | Standard exercise program: an exercise program including muscle stretching, strengthening and walking on a treadmill | 4 years and 2 months | Both groups presented modest improvements, but with no significant differences between them | NA |
| Saccomanno MF et al., 2016 21 | 165 | 44 | 40–70 years-old | GI-1: 53 GI-2:53 GC: 51 |
GI-1: three hyaluronic acid (HA) injectionsGI- 2: HA injections + knee exercises | Knee exercises | 6 months | At the 1 st month, GI-2 scores were significantly better compared to GI-1. GC and GI-2 presented a significant reduction at the 1 st and the 6 th month | NA |
| Palmer S et al., 2014 22 | 224 | 83 | 60–72 years old | GI:73 GC-1: 74 GC-2: 77 |
Active TENS (continuous mode, – 110 Hz, 50 µs) + knee exercises | GC-1: fictional TENS + knee exercises GC-2: knee exercises (30 minutes of education + 30 minutes of exercises) | 6 weeks | Each score from each group significantly improved over time | NA |
| Holsgaard-Larsen A et al., 2017 23 | 93 | 39 | 40–70 years old | GI: 47 GC: 46 |
Warming up (10 minutes), functional, proprioceptive training, resistance strengthening and cooling down | Information about analgesic and anti-inflammatory agents | 8 weeks | There were no significant differences between groups | NA |
| Jorge RT et al., 2015 24 | 60 | NA | 40–70 years old | GI: 29 GC:31 |
Warming up, 5 minutes at bike. Progressive resistance exercise (knee extension/flexion and hip adduction and abduction with light weights). | No intervention | 13 weeks | Pain in the GI group was significantly lower in 45 and 90 days | Significant differences for hip adduction between groups from T0 until the end of the study |
Abbreviations: GC, control group; GI, intervention group; NA, not analyzed; TENS, transcutaneous electrical neural stimulation; T0, initial time.
Discussion
The present study aimed to analyze the efficacy of an exercise program in the treatment of knee OA, with pain and muscle strength being the main outcomes addressed. Our results demonstrate that a rehabilitation program that includes strengthening of a particular muscle group has positive effects on pain.
The quadriceps femoris, ischium cruralis, psoas major, gluteus maximus and medius, gastrocnemius, fascia lata tensor, long adductor, short adductor, gracilis, adductor magnus, and sartorius are the most evidenced muscles in this systematic review. 20 21 22 23 24 25
Among the muscles cited in rehabilitation programs, the main focus is on the femoral quadriceps. Its strengthening is commonly indicated in the treatment and progression of OA because it has a static and dynamic chondroprotective effect on the knee joint, and its weakness can generate joint overload, resulting in pain and instability. 26 According to O'Reilly et al., 27 there is an inverse relationship between quadriceps muscle strength in OA patients and pain reports, that is, the higher the muscle strength, the lower the pain. 27 28 However, the muscle at its greatest power may increase the shear force, or the compressive force, within the joint, which may increase the pain in the knee affected by OA; as such, when the joint is in a more flexed position, the muscle becomes more relaxed and these forces decrease over the joint, increasing the patient's comfort and reducing muscle activation. 29 30 The literature still discusses the relationship between the femoral quadriceps muscle and knee OA, and it is controversial whether muscle weakness contributes to the pathology or the pathology causes muscle weakness. 31 32
The joint kinematic imbalance resulted from mechanical factors may also influence the cause and progression of knee OA because alignment plays an important role in determining articular loads distribution, minimizing the impact effect; so, it is postulated that increased muscle strength is a major cause of impact, pain reduction and disability. As such, one needs to understand the influence of poor joint alignment in the treatment of OA. Lim et al. 33 showed that quadriceps strengthening in a group of patients with severe knee misalignment caused worsening of pain compared to the control group, but not in the group presenting better joint alignment. In addition, these authors noted that quadriceps strengthening did not improve knee alignment, showing that a 3% increase in quadriceps strength worsened knee misalignment by 1 degree. This finding is not necessarily in line with our results, but it highlights the importance of observing the joint alignment before starting a strengthening program to obtain positive outcomes, especially regarding pain. 34
Range of motion is also an important issue in joint treatment success, since patients with chronic knee OA may be subjected to immobilization or inactivity due to pain, resulting in joint capsule contractures and adaptive shortening. 35 Assuming that more elongated muscles have greater torque, the benefits of stretching programs exceed alignment and muscle balance. Hence, stretching therapy as an adjunctive treatment would be a favorable technique to be included in an exercise program for OA management. Both proprioceptive neuromuscular facilitation (PNF) and static stretching show excellent results, but PNF stretching was more effective than static stretching exercises. 35 36 Only three of the papers included in the present review had stretching exercises in their programs. 21 23 33
Most studies included in this review address, in addition to strengthening, balance and proprioceptive techniques. However, only Fitzgerald et al. 20 evaluated these techniques separately, and found no significant evidence that these exercises improve pain and muscle strength in OA patients. This finding does not corroborate the study by Diracoglu et al., 37 who compared kinesthesia and balance exercises or only strengthening exercises in women with knee OA, obtaining positive outcomes on muscle strength, quality of life, and the physical function scale, according to the WOMAC questionnaire.
To measure each of these outcomes, all authors opted for evaluation tools such as the WOMAC questionnaire and the visual analogue scale (VAS). The WOMAC questionnaire is an easy-to-apply, low-cost and specific instrument for knee OA composed of three domains, namely, pain, stiffness, and functionality. 38 Meanwhile, the VAS is a numerical instrument, with scores ranging from 0 to 10, with 10 cm in length, to validate pain sensation; greater VAS scores reflect increased pain levels. 30
Confronting each evaluation instrument, we can observe that when the evaluation of a specific question is required, as in OA, the VAS scale and the WOMAC questionnaire become very subjective; however, since WOMAC specifies momentary pain only in knee OA, it is most satisfactory for this type of evaluation. 30 38
Based on common evidence aspects, we conclude that for a rehabilitation program to be beneficial in the treatment of OA, it should satisfactorily evaluate knee joint misalignment and subsequently develop a treatment plan tailored to the needs of each patient. This evaluation will guide the therapist in the formulation of a physical training program focusing on the appropriate muscular group.
Our results indicate that an ideal program would include isometric and quadriceps femoris and crural ischial muscles isotonic strengthening exercises, especially quadriceps isotonic strengthening, crural and gastrocnemius ischial muscles dynamic stretching and proprioception and balance exercises.
The studies analyzed present some limitations, including the lack of a detailed description of the interventions, the load used, and the evolution of the exercises, mainly in relation to muscular stretches, thus hampering the final elaboration of an adequate physical training program. The duration of the intervention was very variable, not allowing us to reach a consensus about the ideal time to treat OA. The long-term benefits of therapy exercises and possible OA prevention are not yet known due to the lack of studies on these effects.
Another limitation observed is the absence of a gold standard instrument for muscle strength evaluation, such as the use of a dynamometer, compromising the quantitative analysis of this variable. We believed that the lack of such gold standard may be caused by reduced availability and high cost of evaluation devices.
Conclusion
This analysis shows that all papers examining the role of muscle strengthening in the treatment of OA reported pain improvement; however, the protocols used were not properly described, making it difficult to establish a specific physical exercise program for the treatment of knee OA. In addition, only two papers evaluated muscular strength, maybe due to the difficulty in measuring/using an appropriate instrument.
Conflicts of Interest The authors declare that there is no conflict of interest.
Trabalho desenvolvido na Faculdade de Ciências Médicas e da Saúde de Juiz de Fora, Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brasil.
Work developed at Faculdade de Ciências Médicas e da Saúde de Juiz de Fora, Hospital e Maternidade Therezinha de Jesus, Juiz de Fora, MG, Brazil.
Referências
- 1.van der Pas S, Castell M V, Cooper C. European project on osteoarthritis: design of a six-cohort study on the personal and societal burden of osteoarthritis in an older European population. BMC Musculoskelet Disord. 2013;14:138. doi: 10.1186/1471-2474-14-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Felson D T. The epidemiology of knee osteoarthritis: results from the Framingham Osteoarthritis Study. Semin Arthritis Rheum. 1990;20(03) 01:42–50. doi: 10.1016/0049-0172(90)90046-i. [DOI] [PubMed] [Google Scholar]
- 3.Lane N E, Brandt K, Hawker G. OARSI-FDA initiative: defining the disease state of osteoarthritis. Osteoarthritis Cartilage. 2011;19(05):478–482. doi: 10.1016/j.joca.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Conn V S, Hafdahl A R, Minor M A, Nielsen P J. Physical activity interventions among adults with arthritis: meta-analysis of outcomes. Semin Arthritis Rheum. 2008;37(05):307–316. doi: 10.1016/j.semarthrit.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Kerkhof H J, Bierma-Zeinstra S M, Arden N K. Prediction model for knee osteoarthritis incidence, including clinical, genetic and biochemical risk factors. Ann Rheum Dis. 2014;73(12):2116–2121. doi: 10.1136/annrheumdis-2013-203620. [DOI] [PubMed] [Google Scholar]
- 6.Sharma L, Song J, Dunlop D. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69(11):1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Otterness I G, Eckstein F. Women have thinner cartilage and smaller joint surfaces than men after adjustment for body height and weight. Osteoarthritis Cartilage. 2007;15(06):666–672. doi: 10.1016/j.joca.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen C, Lefèvre-Colau M M, Poiraudeau S, Rannou F. Rehabilitation (exercise and strength training) and osteoarthritis: A critical narrative review. Ann Phys Rehabil Med. 2016;59(03):190–195. doi: 10.1016/j.rehab.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 9.McAlindon T E, Bannuru R R, Sullivan M C. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(03):363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Lange A K, Vanwanseele B, Fiatarone Singh M A. Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis Rheum. 2008;59(10):1488–1494. doi: 10.1002/art.24118. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka R, Ozawa J, Kito N, Moriyama H. Efficacy of strengthening or aerobic exercise on pain relief in people with knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2013;27(12):1059–1071. doi: 10.1177/0269215513488898. [DOI] [PubMed] [Google Scholar]
- 12.Levinger P, Dunn J, Bifera N, Butson M, Elias G, Hill K D. High-speed resistance training and balance training for people with knee osteoarthritis to reduce falls risk: study protocol for a pilot randomized controlled trial. Trials. 2017;18(01):384. doi: 10.1186/s13063-017-2129-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mat S, Tan M P, Kamaruzzaman S B, Ng C T. Physical therapies for improving balance and reducing falls risk in osteoarthritis of the knee: a systematic review. Age Ageing. 2015;44(01):16–24. doi: 10.1093/ageing/afu112. [DOI] [PubMed] [Google Scholar]
- 14.Hatfield G L, Morrison A, Wenman M, Hammond C A, Hunt M A. Clinical Tests of Standing Balance in the Knee Osteoarthritis Population: Systematic Review and Meta-analysis. Phys Ther. 2016;96(03):324–337. doi: 10.2522/ptj.20150025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y, Su Y, Chen S. The effects of resistance exercise in patients with knee osteoarthritis: a systematic review and meta-analysis. Clin Rehabil. 2016;30(10):947–959. doi: 10.1177/0269215515610039. [DOI] [PubMed] [Google Scholar]
- 16.Iwamoto J, Sato Y, Takeda T, Matsumoto H. Effectiveness of exercise for osteoarthritis of the knee: A review of the literature. World J Orthop. 2011;2(05):37–42. doi: 10.5312/wjo.v2.i5.37. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Jan M H, Lin C H, Lin Y F, Lin J J, Lin D H. Effects of weight-bearing versus nonweight-bearing exercise on function, walking speed, and position sense in participants with knee osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(06):897–904. doi: 10.1016/j.apmr.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 18.Bartholdy C, Juhl C, Christensen R, Lund H, Zhang W, Henriksen M. The role of muscle strengthening in exercise therapy for knee osteoarthritis: A systematic review and meta-regression analysis of randomized trials. Semin Arthritis Rheum. 2017;47(01):9–21. doi: 10.1016/j.semarthrit.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Jadad A R, Moore R A, Carroll D. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(01):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 20.Fitzgerald G K, Piva S R, Gil A B, Wisniewski S R, Oddis C V, Irrgang J J. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91(04):452–469. doi: 10.2522/ptj.20100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saccomanno M F, Donati F, Careri S, Bartoli M, Severini G, Milano G. Efficacy of intra-articular hyaluronic acid injections and exercise-based rehabilitation programme, administered as isolated or integrated therapeutic regimens for the treatment of knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2016;24(05):1686–1694. doi: 10.1007/s00167-015-3917-9. [DOI] [PubMed] [Google Scholar]
- 22.Palmer S, Domaille M, Cramp F. Transcutaneous electrical nerve stimulation as an adjunct to education and exercise for knee osteoarthritis: a randomized controlled trial. Arthritis Care Res (Hoboken) 2014;66(03):387–394. doi: 10.1002/acr.22147. [DOI] [PubMed] [Google Scholar]
- 23.Holsgaard-Larsen A, Clausen B, Søndergaard J, Christensen R, Andriacchi T P, Roos E M. The effect of instruction in analgesic use compared with neuromuscular exercise on knee-joint load in patients with knee osteoarthritis: a randomized, single-blind, controlled trial. Osteoarthritis Cartilage. 2017;25(04):470–480. doi: 10.1016/j.joca.2016.10.022. [DOI] [PubMed] [Google Scholar]
- 24.Jorge R T, Souza M C, Chiari A. Progressive resistance exercise in women with osteoarthritis of the knee: a randomized controlled trial. Clin Rehabil. 2015;29(03):234–243. doi: 10.1177/0269215514540920. [DOI] [PubMed] [Google Scholar]
- 25.Bennell K L, Hunt M A, Wrigley T V. Hip strengthening reduces symptoms but not knee load in people with medial knee osteoarthritis and varus malalignment: a randomised controlled trial. Osteoarthritis Cartilage. 2010;18(05):621–628. doi: 10.1016/j.joca.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Creamer P, Lethbridge-Cejku M, Hochberg M C. Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology (Oxford) 2000;39(05):490–496. doi: 10.1093/rheumatology/39.5.490. [DOI] [PubMed] [Google Scholar]
- 27.O'Reilly S C, Jones A, Muir K R, Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability. Ann Rheum Dis. 1998;57(10):588–594. doi: 10.1136/ard.57.10.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Avelar Di Sabatino Santos M L, Fabiano Gomes W, Zille de Queiroz B, Brito Rosa NMd, Sirineu Pereira D, Domingues Dias J M.Desempenho muscular, dor, rigidez e funcionalidade de idosas com osteoartrite de joelhoActa Ortop Bras 2011;19(04):
- 29.Schipplein O D, Andriacchi T P. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(01):113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 30.Bolognese J A, Schnitzer T J, Ehrich E W. Response relationship of VAS and Likert scales in osteoarthritis efficacy measurement. Osteoarthritis Cartilage. 2003;11(07):499–507. doi: 10.1016/s1063-4584(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 31.Alnahdi A H, Zeni J A, Snyder-Mackler L. Muscle impairments in patients with knee osteoarthritis. Sports Health. 2012;4(04):284–292. doi: 10.1177/1941738112445726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Segal N A, Glass N A, Felson D T. Effect of quadriceps strength and proprioception on risk for knee osteoarthritis. Med Sci Sports Exerc. 2010;42(11):2081–2088. doi: 10.1249/MSS.0b013e3181dd902e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lim B W, Hinman R S, Wrigley T V, Sharma L, Bennell K L. Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Rheum. 2008;59(07):943–951. doi: 10.1002/art.23823. [DOI] [PubMed] [Google Scholar]
- 34.Foroughi N, Smith R M, Lange A K, Singh M A, Vanwanseele B. Progressive resistance training and dynamic alignment in osteoarthritis: A single-blind randomised controlled trial. Clin Biomech (Bristol, Avon) 2011;26(01):71–77. doi: 10.1016/j.clinbiomech.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 35.Weng M C, Lee C L, Chen C H. Effects of different stretching techniques on the outcomes of isokinetic exercise in patients with knee osteoarthritis. Kaohsiung J Med Sci. 2009;25(06):306–315. doi: 10.1016/S1607-551X(09)70521-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferreira de Meneses S R, Hunter D J, Young Docko E, Pasqual Marques A. Effect of low-level laser therapy (904 nm) and static stretching in patients with knee osteoarthritis: a protocol of randomised controlled trial. BMC Musculoskelet Disord. 2015;16:252. doi: 10.1186/s12891-015-0709-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol. 2005;11(06):303–310. doi: 10.1097/01.rhu.0000191213.37853.3d. [DOI] [PubMed] [Google Scholar]
- 38.Marx F C, Oliveira L M, Bellini C G, Ribeiro M CC. Tradução e validação cultural do questionário algofuncional de Lequesne para osteoartrite de joelhos e quadris para a língua portuguesa. Rev Bras Reumatol. 2006;46(04):253–260. [Google Scholar]