Abstract
Objective Coracoid osteolysis has been described as a possible complication after the Latarjet procedure. The aim of the present study was to investigate the incidence and risk factors associated to coracoid graft osteolysis and to correlate them with clinical results.
Methods A retrospective review of 38 Latarjet procedures was conducted. Computed tomography (CT) scans were obtained from all of the patients before and at least 1 year after the surgery. Coracoid osteolysis was evaluated and correlated to preoperative factors, namely: age, smoking status, and preoperative glenoid bone loss. The patients were divided into 2 groups: A (no or minor bone resorption) and B (major or total bone resorption). The functional outcome was determined by the Rowe score.
Results Coracoid graft osteolysis occurred in 22 cases (57.8%). The mean preoperative glenoid defect was 22.8% in group A, and 13.4% in group B ( p = 0.0075). The mean ages of the subjects in both groups were not significantly different. Smoking did not seem to affect the main outcome either, and no correlation was found between graft osteolysis and postoperative range of motion, pain, or Rowe score. There were no cases of recurrent dislocations in our sample, although four patients presented with a positive anterior apprehension sign.
Conclusion Bone resorption of the coracoid graft is present in at least 50% of the patients submitted to the Latarjet procedure, and the absence of significant preoperative glenoid bone loss showed to be the only risk factor associated with severe graft osteolysis, even though this did not influence significantly the clinical outcome.
Keywords: joint instability, shoulder dislocation, shoulder joint, bone resorption, osteolysis
Introduction
In the last years, many articles have been published about the results of the bone block procedure described by Latarjet for the treatment of anterior glenohumeral instability. 1 2 3 4 Even with some modifications from surgeon to surgeon, the main principle of the surgery remains the coracoid transfer through the subscapularis tendon. 1 5 6 7 It has become the treatment of choice in the settings of osseous deficiencies > 20% of the glenoid surface area, of revision surgery, and of athletes who practice high-risk contact sports, even in the setting of limited osseous deficiency. 8 For the achievement of the best result and less complications, it is mandatory to position the graft properly with the goal of healing between the coracoid process and the glenoid in a flush position. 9 10 11 12 Even after bone union, coracoid bone graft resorption can occur. This phenomenon has been reported, and some authors have considered that it might be associated with shoulder pain and recurrent dislocation. 3 4 11 13 Di Giacomo et al., 14 were one of the first authors to report the location and amount of coracoid graft osteolysis after the Latarjet procedure using computed tomography (CT) scan analysis. He also published another study, which states that patients with preoperative glenoid bone loss (> 15%) underwent less osteolysis when compared with those with lesser defects. 15 He theorized that in patients without glenoid bone loss, there is lack of mechanical stimuli from the humeral head in certain areas of the graft, which may contribute to the resorption of the coracoid. The purpose of the present study was to evaluate the incidence of bone graft osteolysis after the Latarjet procedure and to correlate it with age, smoking, and the presence of preoperative glenoid bone loss. Our hypothesis was that, as previously described, bone graft osteolysis is more pronounced in cases without glenoid bone loss.
Materials and Methods
Study Population
This is a retrospective observational study of 72 patients submitted to surgery for anterior shoulder instability using the Latarjet procedure, between May 2012 and August 2016. The inclusion criteria were availability of a preoperative and of at least a 1-year postoperative CT scan and physical examination at a minimum of 2 years postoperatively. Cases with a major deviation from the most commonly used technique (such as the congruent arc technique), those that had to be reoperated for hardware removal, or those in which the graft did not heal promptly were excluded. All of the patients gave written consent to participate in the study, and approval from the ethics committee of the institute was granted.
The main outcome studied was osteolysis of the coracoid graft, classified in 4 types according to Zhu et al. 16 ( Table 1 ). According to this classification, we divided the subjects in two groups, A (no or minor resorption) and B (major or total resorption). This was compared with several exposures, namely the amount of glenoid bone loss before surgery, tobacco use, the use of suture anchors, and age. We have also searched for correlation between graft resorption and postoperative clinical results using the Rowe score, visual analogue scale, and range of motion. Variables were obtained from pre- and at least 1-year postoperative CTs. Range of motion was obtained from physical examination, and pain was registered using the visual analogue scale. These results were registered in a Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) spreadsheet and the statistical analysis was performed using the Real Statistics software package (Charles Zaionitz).
Table 1. Zhu et al. 16 classification of postoperative coracoid bone resorption (4 grades based on axial computed tomography scan). Bone resorption classified with the highest grade between the two screws .
| Grade 0 (no resorption): The cone of the screw head is buried in the coracoid bone graft |
| Grade I (minor resorption): Only the screw head is exposed outside the bone graft. |
| Grade II (major resorption): Part of the screw shaft is exposed outside the graft. |
| Grade III (total resorption): The screw head and shaft are both totally exposed, with all of the coracoid bone graft absorbed, and no bone is left on the glenoid neck. |
Surgical Technique
The surgery was performed under general anesthesia combined with an interscalene block. The patients were placed in the beach chair position. A surgical incision was made starting from the coracoid process and extending ∼ 7 cm inferiorly. Through the deltopectoral interval, the coracoid process was osteotomized with a curved osteotome. The subscapularis tendon was divided horizontally along the muscle fiber at the level of the lower one-third of the width of the tendon. A vertical incision was made at the anterior joint capsule. Both the coracoid graft and the glenoid neck were decorticated before fixation with 2 screws (3.5 mm cortical or 4.0 mm cancellous) without any specific guide. According to the preference of the surgeons, the anterior capsule was reattached to the anterior inferior rim of the native glenoid with one bioabsorble Gryphon suture anchor (Depuy Synthes, Warsaw, IN, USA) or sutured to the stump of the coracoacromial ligament, or it was not reattached at all. A sling protected the shoulder for 4 weeks postoperatively. Passive range of motion was started at 2 weeks, and daily activity was allowed at 4 weeks. Strengthening of the shoulder was initiated 3 months after the surgery.
Radiographic Imaging
Images were obtained with a Philips Brilliance 64-slice CT scanner (Philips, Amsterdam, Netherlands) at, 250 mA, 120 Kvp, and slice thickness of 1mm). Preoperative glenoid bone loss was measured on a three-dimensional (3D) reconstruction en face view of the glenoid with the humeral head subtracted. The percentage of the glenoid bone loss was measured using the surface area method by the Image J software (National Institutes of Health, Bethesda, MA, USA) using the concept of the “best-fit circle.” 17 18 19 20 The postoperative CT scan was performed after a minimum of 1 year. Healing, position, and resorption of the graft were assessed. Healing was confirmed by bridging with bone between the bone block and the glenoid. The presence of a complete radiolucent line between the graft and the glenoid represented a nonunion, and the case was excluded. If the lateral cortex of the coracoid was > 1 mm medial or lateral to the articular surface of the glenoid, then the position of the coracoid was defined as medial or lateral overhanging position, respectively. Otherwise, if the lateral cortex of the coracoid was within 1 mm of the glenoid surface, the position of the coracoid was defined as flush. The classification system described by Zhu et al. 16 was used to evaluate coracoid graft resorption ( Table 1 ).
Statistical Evaluation
Results were recorded in an Excel spreadsheet, and statistical testing was performed using the Real Statistics tool. Subjects were divided in the two groups, and normality was assessed using the Shapiro-Wilk test. Continuous variables with a normal distribution were compared using the Student t-test (preoperative glenoid defects). Non-normal distribution variables were compared using the Mann-Whitney test (age and Rowe score). Categorical data with small samples were compared using the direct Fischer test (suture anchor use and smoking)
Results
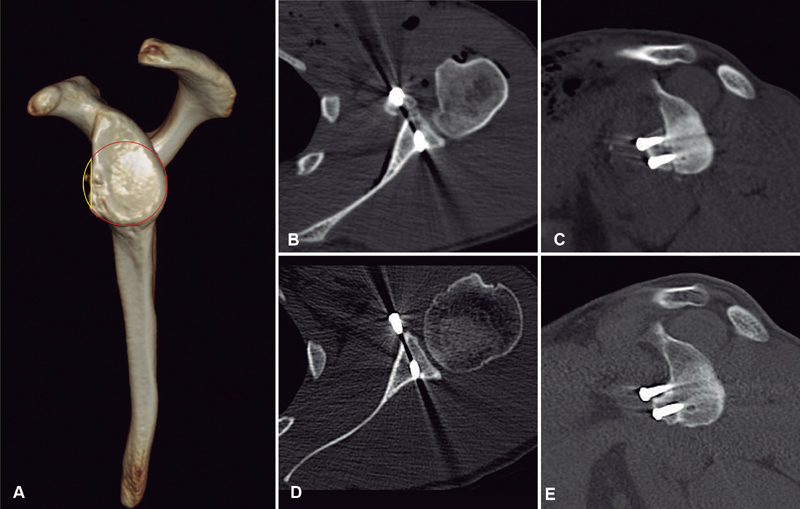
Out of the initial 72 patients included in the study, 13 were excluded for lack of preoperative exams, and 11 for lack of postoperative exams. Three patients were excluded for undergoing implant removal during revision surgery in the 1 st year. Two presented with graft nonunion, and in six, the coracoid was placed with the concave inferior surface facing the joint (the congruent arc technique). After exclusions, 38 shoulders in 37 patients remained. Their mean age was 33 years old (21 to 67 years old), 32 were male, and 5 were female. The mean size of the preoperative glenoid defect was 20% (0–34%). A total of 27 cases showed a bony Bankart lesion, and 10 had bone erosion. One case had no defect. In 11 cases, the anterior capsule was reattached to the glenoid with one anchor. In nine cases, no anchor was used, and the capsule was sutured to the stump of the coracoacromial ligament or to the head of the screw (seven and two cases, respectively). In the final 18 cases, no capsule reattachment was performed. The postoperative CT evaluation was performed at a mean follow-up of 27 months (12 to 72 months). The position of the graft was considered optimal in 34 cases. Three were considered medial, and one was considered lateral. According to the classification system by Yi-Ming Zhu et al., 16 graft resorption occurred in 22 cases (57.8%), with 11 type I, 8 type II, and 3 type III. In all of the cases, more severe resorption occurred in the superior part of the graft around the superior screw ( Fig. 1 ). Hence, the groups were composed of 27 cases in group A (grades 0 and I), and of 11 cases in group B (grades II and III). The mean preoperative glenoid defect observed was 22.8% in group A, and 13.4% in group B ( p = 0.0075) ( Table 2 ). The mean age of the subjects in both groups were not significantly different: 32 and 35.8 years old in groups A and B, respectively. No correlation was found between graft osteolysis and suture anchor use for capsular repair (6/27 versus 5/11), postoperative range of motion, pain, or Rowe score (88.3 versus 89) ( p = 0.46) Smoking did not seem to affect the main outcome either, although we had only two smoking subjects in each group. There were no cases of recurring instability in our sample, although four patients presented with a positive anterior apprehension sign, all in group A ( Table 3 ).
Fig. 1.
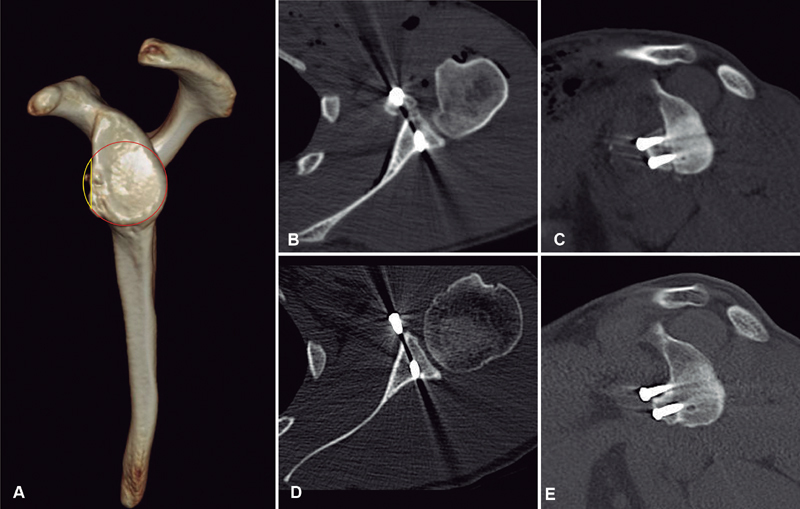
(A) Preoperative three-dimensional reconstruction computed tomography scan of the glenoid. The anterior glenoid defect border (yellow) and circumference of the perfect circle (red) outlined. Percentage bone loss = (defect surface area/surface area of the perfect glenoid circle) × 100%. (B,C) Immediate postoperative axial and sagittal view computed tomography scan. (D,E) Computed tomography scan 42 months after surgery showing grade III resorption of the superior part of the coracoid graft.
Table 2. Characteristics of groups A and B.
| Group A (grade 0/I) | Group B (grade II/III) | p-value | |
|---|---|---|---|
| Cases | 27 | 11 | |
| Follow-up (months) | 27.9 (12- 67) | 26.9 (12–72) | |
| Preoperative glenoid bone loss (area) | 22.8% (7–34) | 13.4% (0–24) | 0.0075 |
| Age (years old) | 32 | 35.8 | 0.410 |
| Smoking | 2 | 2 | 0.562 |
| Anchor | 6 | 4 | 0.424 |
Table 3. Comparison of the clinical results between groups A and B.
| Group A (grade 0/I) | Group B (grade II/III) | p-value | |
|---|---|---|---|
| Rowe score | 88 (45–100) | 89 (65–100) | 0.46 |
| Forward elevation | 160° (130–180) | 151° (140–160) | 0.175 |
| External rotation | 51° (30–80) | 48° (25–70) | 0.585 |
| Internal rotation | T9 (T6-L1) | T10 (T5-L3) | 0.349 |
| Anterior apprehension | 4 | 0 | 0.309 |
| Recurrence | 0 | 0 |
The coracoid graft was well-positioned and without resorption in all four cases with positive anterior apprehension.
Discussion
The Latarjet procedure has been shown to be a reliable method to prevent recurrent shoulder anterior instability, with many authors reporting successful outcomes. 21 22 23 24 At the same time, few studies mention the condition of coracoid bone resorption. The present study shows that some bone resorption of the coracoid graft is present in at least 50% of the patients submitted to the Latarjet surgery, and that patients with less preoperative glenoid bone loss had more chances of having more severe graft osteolysis. One of the theories related to that finding is that there is lack of mechanical stimuli of the graft in patients with less glenoid bone loss, while patients with a more significant defect would be subjected to maintaining forces when the coracoid replaces the large bone defect (Wolff law). 14 15 Accordingly, we found that in all of the patients, the superior part of the graft had a more pronounced resorption. Our impression is that this may be due to the inferior part of the coracoid being subjected to forces of traction from the conjoined tendon, thus protecting it from resorption. We can also speculate that this part had some contribution of vascularization from the conjoined tendon. Di Giacomo et al. 14 performed a study to determine the location and amount of coracoid graft osteolysis after the Latarjet procedure using CT. He described a classification dividing the coracoid in eight parts and identified more pronounced resorption in the superficial and medial parts. It was the first classification published on this subject, and he believed that the results of resorption were due to mechanical and biological factors. 14 Later, he published a second paper correlating the presence of glenoid bone loss and coracoid graft osteolysis, and identified less osteolysis in patients with significant glenoid bone loss (> 15%). 15
Zhu et al. 16 described a more simple classification system than Giacomo to evaluate the severity of the bone resorption of the transferred coracoid. His classification is based on the amount of resorption seen in the axial CT scan around each of the screws; the resorption is classified with the highest grade between the two screws. In our study, the highest grade was always in the superior screw. He found an incidence of 90.5% of coracoid bone resorption after 1 year, while in our study, using the same classification, we found an incidence of 57.8%. Zhu et al. 16 did not try to correlate the incidence or severity of the resorption with glenoid bone loss, and all of the patients of his series had a preoperative glenoid bone defect > 20%. Haeni et al. 25 performed a prospective study with 15 patients after the arthroscopic Latarjet procedure and found that the superior half of the coracoid undergoes a significant amount of osteolysis after 6 months. One difference from his study was that the resorption was evaluated through 3D CT scans using volumetric analysis. There was no mention of clinical implications or complications due to the resorption. Recently, Zhu et al. 26 published a prospective comparative study between arthroscopic versus open Latarjet, and found less graft resorption in the arthroscopic group. Both groups had no significant difference for the preoperative glenoid bone loss. They attributed this result to a multifactorial cause of resorption, and believed that a better protection of soft tissue during arthroscopic surgery could lead to better preservation of the blood supply of the coracoid. One of the main concerns about osteolysis of the coracoid process is the possible association with worse clinical results; however, until now, no consensus has been achieved. 4 25 A total of 11 patients (29%) of our series had major resorption (grades II and III), but this was not correlated with any difference in functional outcomes or with the risk of recurrence of instability when compared with patients without or with minor resorption. Lunn et al., 27 in a series of patients with failure after the Latarjet procedure, identified graft lysis as a risk factor for recurrence of instability. This can bring a discussion about the importance of the bone block compared with the sling effect of the conjoined tendon in the stability after the Latarjet procedure. 28 29 Our clinical results demonstrated that the presence of resorption was not related to a higher incidence of recurrence. Giacommo et al. 14 15 suggest that the bone block effect might not be the main effect, because of the huge osteolysis that happened in his patients. We could speculate that the osseous contribution for the stability after the Latarjet procedure is more important in cases with larger glenoid bone defects because those are the patients with less osteolysis, as has been demonstrated previously.
A limited number of patients and short follow-up are some of the limitations of the present study. Although we could not identify a negative effect on the clinical outcome of the patients with more severe graft resorption, concerns about this issue still exist. Therefore, we recommend caution when performing Latarjet procedures in cases without significant glenoid bone loss, taking into consideration that the superior part of the graft has more chances of resorption, and an optimal screw position should be ensured.
Conclusion
The present study shows that some bone resorption of the coracoid graft is present in at least 50% of the patients submitted to the Latarjet surgery, and that the absence of a significant preoperative glenoid defect seems to be the only risk factor associated with more severe graft osteolysis, even though no significant clinical significance was found in these cases.
Conflict of Interests The authors have no conflict of interests to declare.
Observação
Comitê de Revisão Institucional (IRB) – Plataforma Brasil, número CAAE 68193617.8.0000.5273.
Trabalho desenvolvido no Departamento de Cirurgia do Ombro e Cotovelo, Instituto Nacional de Traumatologia e Ortopedia - Ministério da Saúde (INTO-MS), Rio de Janeiro, RJ, Brasil.
Note
Institucional Review Board (IRB) – Plataforma Brasil CAAE number 68193617.8.0000.5273.
Work developed at the Department of Shoulder and Elbow Surgery, Instituto Nacional de Traumatologia e Ortopedia, Ministério da Saúde (INTO-MS), Rio de Janeiro, state of Rio de Janeiro, Brazil.
Referências
- 1.Boileau P, Thélu CÉ, Mercier N. Arthroscopic Bristow-Latarjet combined with bankart repair restores shoulder stability in patients with glenoid bone loss. Clin Orthop Relat Res. 2014;472(08):2413–2424. doi: 10.1007/s11999-014-3691-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.da Silva L A, da Costa Lima A G, Kautsky R M. Evaluation of the results and complications of the Latarjet procedure for recurrent anterior dislocation of the shoulder. Rev Bras Ortop. 2015;50(06):652–659. doi: 10.1016/j.rboe.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hovelius L, Sandström B, Sundgren K. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I--clinical results. J Shoulder Elbow Surg. 2004;13(05):509–516. doi: 10.1016/j.jse.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Mizuno N, Denard P J, Raiss P. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg. 2014;23(11):1691–1699. doi: 10.1016/j.jse.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Hovelius L, Körner L, Lundberg B. The coracoid transfer for recurrent dislocation of the shoulder. Technical aspects of the Bristow-Latarjet procedure. J Bone Joint Surg Am. 1983;65(07):926–934. [PubMed] [Google Scholar]
- 6.Ikemoto R Y, Murachovisky J, Nascimento L G. Results from Latarjet surgery for treating traumatic anterior shoulder instability associated with bone erosion in the glenoid cavity, after minimum follow-up of one year. Rev Bras Ortop. 2015;46(05):553–560. doi: 10.1016/S2255-4971(15)30411-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Latarjet M. [Treatment of recurrent dislocation of the shoulder] Lyon Chir. 1954;49(08):994–997. [PubMed] [Google Scholar]
- 8.Shaha J S, Cook J B, Song D J. Redefi “critical” bone loss in shoulder instability. Am J Sports Med. 2015;43(07):1719–1725. doi: 10.1177/0363546515578250. [DOI] [PubMed] [Google Scholar]
- 9.Athwal G S, Meislin R, Getz C. Short-term complications of the arthroscopic Latarjet procedure: a North American experience. Arthroscopy. 2016;32(10):1965–1970. doi: 10.1016/j.arthro.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 10.Casabianca L, Gerometta A, Massein A. Graft position and fusion rate following arthroscopic Latarjet. Knee Surg Sports Traumatol Arthrosc. 2016;24(02):507–512. doi: 10.1007/s00167-015-3551-6. [DOI] [PubMed] [Google Scholar]
- 11.Samim M, Small K M, Higgins L D. Coracoid graft union: a quantitative assessment by computed tomography in primary and revision Latarjet procedure. J Shoulder Elbow Surg. 2018;27(08):1475–1482. doi: 10.1016/j.jse.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Gartsman G M, Waggenspack W N, Jr, O’Connor D P. Immediate and early complications of the open Latarjet procedure: a retrospective review of a large consecutive case series. J Shoulder Elbow Surg. 2017;26(01):68–72. doi: 10.1016/j.jse.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 13.Balestro J C, Young A, Maccioni C. Graft osteolysis and recurrent instability after the Latarjet procedure performed with bioabsorbable screw fixation. J Shoulder Elbow Surg. 2015;24(05):711–718. doi: 10.1016/j.jse.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 14.Di Giacomo G, Costantini A, de Gasperis N. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: a computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg. 2011;20(06):989–995. doi: 10.1016/j.jse.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 15.Di Giacomo G, de Gasperis N, Costantini A. Does the presence of glenoid bone loss influence coracoid bone graft osteolysis after the Latarjet procedure? A computed tomography scan study in 2 groups of patients with and without glenoid bone loss. J Shoulder Elbow Surg. 2014;23(04):514–518. doi: 10.1016/j.jse.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Zhu Y M, Jiang C Y, Lu Y. Coracoid bone graft resorption after Latarjet procedure is underestimated: a new classification system and a clinical review with computed tomography evaluation. J Shoulder Elbow Surg. 2015;24(11):1782–1788. doi: 10.1016/j.jse.2015.05.039. [DOI] [PubMed] [Google Scholar]
- 17.Hamamoto J T, Leroux T, Chahla J. Assessment and Evaluation of Glenoid Bone Loss. Arthrosc Tech. 2016;5(04):e947–e951. doi: 10.1016/j.eats.2016.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huysmans P E, Haen P S, Kidd M. The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elbow Surg. 2006;15(06):759–763. doi: 10.1016/j.jse.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Magarelli N, Milano G, Sergio P. Intra-observer and interobserver reliability of the ‘Pico’ computed tomography method for quantification of glenoid bone defect in anterior shoulder instability. Skeletal Radiol. 2009;38(11):1071–1075. doi: 10.1007/s00256-009-0719-5. [DOI] [PubMed] [Google Scholar]
- 20.Sugaya H, Moriishi J, Dohi M. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85(05):878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80(06):841–852. doi: 10.2106/00004623-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Gordins V, Hovelius L, Sandström B. Risk of arthropathy after the Bristow-Latarjet repair: a radiologic and clinical thirty-three to thirty-five years of follow-up of thirty-one shoulders. J Shoulder Elbow Surg. 2015;24(05):691–699. doi: 10.1016/j.jse.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 23.Lafosse L, Boyle S.Arthroscopic Latarjet procedure J Shoulder Elbow Surg 201019(2, Suppl)2–12. [DOI] [PubMed] [Google Scholar]
- 24.Rosa J RP, Checchia C S, Miyazaki A N. Traumatic anterior instability of the shoulder. Rev Bras Ortop. 2017;52(05):513–520. doi: 10.1016/j.rboe.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haeni D L, Opsomer G, Sood A et al. Three-dimensional volume measurement of coracoid graft osteolysis after arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2017;26(03):484–489. doi: 10.1016/j.jse.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Zhu Y, Jiang C, Song G. Arthroscopic Versus Open Latarjet in the Treatment of Recurrent Anterior Shoulder Dislocation With Marked Glenoid Bone Loss: A Prospective Comparative Study. Am J Sports Med. 2017;45(07):1645–1653. doi: 10.1177/0363546517693845. [DOI] [PubMed] [Google Scholar]
- 27.Lunn J V, Castellano-Rosa J, Walch G. Recurrent anterior dislocation after the Latarjet procedure: outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elbow Surg. 2008;17(05):744–750. doi: 10.1016/j.jse.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Dines J S, Dodson C C, McGarry M H. Contribution of osseous and muscular stabilizing effects with the Latarjet procedure for anterior instability without glenoid bone loss. J Shoulder Elbow Surg. 2013;22(12):1689–1694. doi: 10.1016/j.jse.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 29.Yamamoto N, Itoi E, Abe H. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med. 2009;37(05):949–954. doi: 10.1177/0363546508330139. [DOI] [PubMed] [Google Scholar]