Abstract
Introduction
Prone position is known to improve mortality in patients with acute respiratory distress syndrome (ARDS). The impact of prone position in critically ill patients with coronavirus disease of 2019 (COVID-19) remains to be determined. In this review, we describe the mechanisms of action of prone position, systematically appraise the current experience of prone position in COVID-19 patients, and highlight unique considerations for prone position practices during this pandemic.
Methods
For our systematic review, we searched PubMed, Scopus and EMBASE from January 1, 2020, to April 16, 2020. After completion of our search, we became aware of four relevant publications during article preparation that were published in May and June 2020, and these studies were reviewed for eligibility and inclusion. We included all studies reporting clinical characteristics of patients admitted to the hospital with COVID-19 disease who received respiratory support with high-flow nasal cannula, or noninvasive or mechanical ventilation and reported the use of prone position. The full text of eligible articles was reviewed, and data regarding study design, patient characteristics, interventions and outcomes were extracted.
Results
We found seven studies (total 1899 patients) describing prone position in COVID-19. Prone position has been increasingly used in non-intubated patients with COVID-19; studies show high tolerance and improvement in oxygenation and lung recruitment. Published studies lacked a description of important clinical outcomes (e.g., mortality, duration of mechanical ventilation).
Conclusions
Based on the findings of our review, we recommend prone position in patients with moderate to severe COVID-19 ARDS as per existing guidelines. A trial of prone position should be considered for non-intubated COVID-19 patients with hypoxemic respiratory failure, as long as this does not result in a delay in intubation.
Keywords: Acute respiratory distress syndrome (ARDS), COVID-19, Epidemic, Pandemic, Prone position
Key Summary Points
| Prone position improves mortality in patients with acute respiratory distress syndrome (ARDS), though its role in the treatment in critically ill COVID-19 patients remains to be determined. |
| Prone position has been increasingly used in non-intubated patients with COVID-19, and studies show high tolerance and improvement in oxygenation and lung recruitment. |
| Published COVID-19 studies describing the use of prone position lacked a description of important clinical outcomes (e.g., mortality, duration of mechanical ventilation). |
| A trial of prone position should be considered for non-intubated COVID-19 patients with hypoxemic respiratory failure, as long as this does not result in a delay in intubation. |
Digital Features
This article is published with digital features, including [list digital features available e.g. a summary slide and video abstract], to facilitate understanding of the article. To view digital features for this article go to 10.6084/m9.figshare.13007978.
Introduction
The coronavirus disease of 2019 (COVID-19) has infected almost 29 million people worldwide, with more than 900,000 deaths (case fatality rate of 3.2%) [1]. Case fatality rates of approximately 50% have been reported among critically ill patients [2]. A significant proportion of patients admitted to the intensive care unit (ICU) had severe hypoxemic respiratory failure requiring mechanical ventilation (MV) [3, 4]. Encouraging data demonstrate that the use of steroids is associated with a reduction in mortality in COVID-19 patients requiring respiratory support [5, 6]. However, supportive care with MV remains the cornerstone of intensive care management in these patients [7, 8]. One of the main adjunctive strategies in patients with acute respiratory distress syndrome (ARDS) who require MV is prone position. Given the benefits of prone position in moderate to severe ARDS [9], the Surviving Sepsis Campaign and World Health Organization (WHO) guidelines [10, 11] recommend prone position for 12–16 h a day for adults and children with severe COVID-19 ARDS.
The main aims of this narrative review are to (1) describe the mechanisms of action and summarize the current evidence for prone position in severe respiratory failure, in particular ARDS; (2) systematically review the current collective experience regarding prone position in critically ill COVID-19 patients; and (3) highlight unique considerations for prone position practices during the COVID-19 pandemic.
Mechanism of Action and Benefit of Prone Position
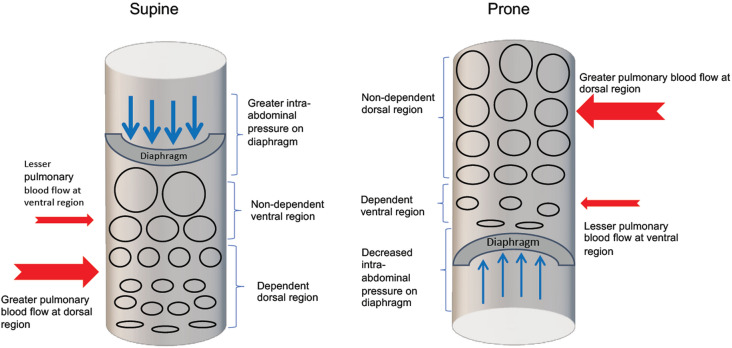
In ARDS, prone position improves oxygenation through changes in the distribution of alveolar ventilation and blood flow, improved matching of local ventilation and perfusion, and reduction in regions of low ventilation/perfusion ratios (Fig. 1) [12–14]. In addition, prone position may reduce the risk of ventilator-induced lung injury (VILI) and promote the complementary benefits of high positive end expiratory pressure (PEEP) [15, 16]. Prone position leads to a decrease in barotrauma and atelectrauma via a few mechanisms: reduction in hyperinflation; mitigation of overdistension of well-ventilated alveoli during the use of PEEP; and reduction in regional shear strain from cyclical opening and closing of small airways [15, 16]. Some advantages of prone position compared with the supine position are shown in Table 1.
Fig. 1.
Schematic showing the changes in ventilation and perfusion in supine and prone positions. In the supine position, alveoli at the dependent dorsal region are collapsed (flattened ovals) resulting in decreased ventilation due to the compressive forces exerted by the ventral region lung tissues as well as the increased (thicker blue arrows) intra-abdominal pressure transmitted to the diaphragm. Greater pulmonary blood flow (thicker red arrow) and decreased ventilation at the dorsal region led to greater ventilation/perfusion mismatch. In the prone position, without the weight of the compressive forces of the ventral region and decreased intra-abdominal pressure (thinner blue arrows), alveoli at the now non-dependent dorsal region are recruited (bigger circles) and coupled with greater pulmonary blood flow (thicker red arrow) at the dorsal region, there is now better ventilation/perfusion matching thereby resulting in better oxygenation
Table 1.
Advantages and disadvantages of prone position
| Advantages | Disadvantages |
|---|---|
| Reduction in ventral-dorsal transpulmonary pressure difference resulting in: | Increased incidence of pressure sores, tracheal tube obstruction and dislodgement of thoracostomy tubes |
| Increase in ventilation homogeneity | |
| Decrease in ventral alveolar over-inflation and dorsal alveolar collapse | |
| Reduction in ventilator-induced lung injury as a result of reduction in alveolar distension | Increased manpower needed to turn patient to prone |
| Improved ventilation/perfusion matching due to reduction in compressive forces as well as greater pulmonary blood flow at non-dependent dorsal lung region | Contraindicated in patients with unstable spinal or pelvic fractures, open chest or abdomen, central cannulation of extracorporeal membrane oxygenation or ventricular assist devices, pregnant women in 2nd and 3rd trimesters |
| Inability to immediately perform procedures such as intubation and chest compression for patient in the prone position |
Early trials [17, 18] showed no mortality benefit with the use of prone position in adults with ARDS but provided valuable information for the targeted application of prone position. This culminated in a landmark PROSEVA randomized controlled trial (RCT) [19], which showed a reduction in 28-day mortality in patient with severe ARDS treated with prone position and lung protective ventilation strategies [16% (38/237) vs. 33% (75/229) in the prone and supine groups, respectively (P < 0.001)]. Following this, three meta-analyses showed a reduction in mortality with the use of prone position [20] particularly in those with early implementation [21], prolonged adaption of at least 12 h [13, 21] and in patients with severe hypoxemia [21] or moderate to severe ARDS [13]. These studies have resulted in a strong recommendation [9] for prone position for more than 12 h per day for adults with severe ARDS. These recommendations are currently echoed in World Health Organization (WHO) [11], Surviving Sepsis [10] guidelines and expert opinion [22] in the management of COVID-19 ARDS.
Systematic Review of Current Use of Prone Position in COVID-19 Patients
In this subsection, we examine the association between the use of prone position and clinical outcomes (e.g., mortality and duration of MV) and physiological changes (e.g., improvement in oxygenation, lung recruitability) that have been reported in patients with COVID-19.
Methods
Search Strategy and Selection Criteria
We included all studies of patients with COVID-19 who received respiratory support with high-flow nasal cannula (HFNC), noninvasive ventilation (NIV) or MV and reported the use of prone position and our primary outcome, mortality. We limited our search to January 1, 2020 (the day after the first cases were reported to WHO) to April 16, 2020. After the search was completed, we became aware of four relevant publications that were published in May and June 2020; these studies were reviewed for eligibility and inclusion. As the search was not repeated after April 16, 2020, we recognize that this may introduce selection bias. We did not use language restrictions, but we excluded articles which were unpublished, had not been peer reviewed, case reports and case series with fewer than 10 patients, expert guidance, commentaries, guidelines and protocols for management. We searched the following major medical databases (PubMed, Scopus and EMBASE) with the following keywords: “SARS-CoV-2” OR “SARS-CoV2” OR “SARSCoV-2” OR “SARSCov2” OR “Coronavirus disease 2019” OR “Novel coronavirus” OR “Novel coronavirus 2019” OR “2019 nCoV” OR “COVID-19” OR “Wuhan coronavirus” OR “Wuhan pneumonia” OR “2019-nCoV” OR “COVID-19” OR “covid19” OR “covid 19”. We used text keywords rather than MeSH and Emtree terms as the indexing of the varied terms to COVID-19 was still in progress at the time. Two authors independently reviewed all abstracts and at least one author reviewed the full text for inclusion. Any disagreements were resolved by consensus with a third reviewer. Articles were selected for full-text review if the abstract contained keywords such as “critically ill”, “intensive care”, “respiratory support” “high flow nasal cannula” “non-invasive ventilation” and “mechanical ventilation”. Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia, was used to identify and remove duplicates (available at http://www.covidence.org). This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Analysis
At least one of the authors reviewed the full text of eligible articles and extracted data on study design, patient characteristics [e.g., age, number of females, PaO2/FiO2 ratio, oxygenation index (OI), oxygen saturation index (OSI), clinical severity scores including Sequential Organ Failure Assessment (SOFA) and Acute Physiology And Chronic Health Evaluation II (APACHE II) score], interventions (respiratory support, FiO2, ventilator parameters, use of prone position, duration and timing of prone position, extracorporeal membrane oxygenation (ECMO), outcomes (mortality, duration of MV) and adverse events associated with prone position. A priori, provided there were sufficient studies, we planned to perform a meta-analysis to assess the association of prone positioning with improvement in PaO2/FiO2 ratio, duration of MV and mortality.
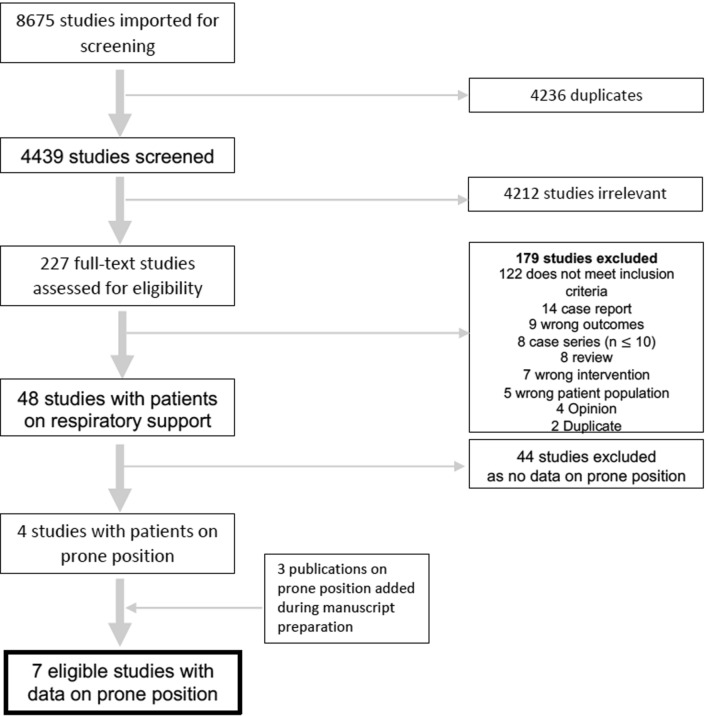
Results
We retrieved 8675 references (Fig. 2), of which 4236 were duplicates. We identified seven articles [23–30] describing prone position in COVID-19 patients receiving respiratory support with HFNC, NIV or MV (Table 1). Six of seven studies were observational [23–29], and one was a prospective feasibility study [30]. Six studies [23, 24, 26, 28–30] included only adult patients, and five were single-center studies [23, 26, 28–30]. Three studies included ICU patients alone [23, 26, 27], three included only non-intubated patients outside the ICU setting [28–30] and one study included both ICU and non-ICU patients [24]. Six of seven studies involved a small number of adult patients [23, 24, 26, 28–30] (Table 1). Only one study [27] included a large cohort of 1591 patients and included adult and pediatric patients. The included studies were clinically heterogenous, and there was a paucity of description of clinical outcomes in relation to prone position, precluding us from performing a meta-analysis and providing a pooled effect estimate of the impact of the prone position on clinically important outcomes.
Fig. 2.
Study selection for systematic review of the prone position in COVID-19 patients
Outcomes
Three of seven studies [28–30] reported on the tolerability of prone position in awake non-intubated patients, all reporting high tolerance (63–83.9%).
Three studies reported changes in oxygenation with prone position [28–30]. In a single center study of 24 awake non-intubated patients with hypoxemic acute respiratory failure [28], 6/24 (25%) patients showed greater than 20% increase in PaO2 (compared with baseline) during prone position. Similarly, in a study of 15 patients with poor response to NIV (PEEP 10 cm H2O and FiO2 of 0.6) all patients showed improvement in SpO2 and PaO2/FiO2 (P < 0.001) with prone position [29]. In a third study of 56 patients on oxygen supplementation or continuous positive airway pressure support, oxygenation substantially improved from supine to prone position (PaO2/FiO2 ratio 180.5 mmHg [SD 76.6] vs. 285.5 mmHg [112.9] in supine and prone positions, respectively; P < 0.0001) [30]. In two studies, improvement in oxygenation was maintained after resupination in half of those who showed improvement with prone position [28, 30] although this change was not significant when compared with oxygenation prior to prone position.
In the one study which assessed lung recruitment, there was an improvement in recruitability in the prone compared with supine position [26]. In 12 mechanically ventilated patients, prone position performed over periods of 24 h when PaO2/FiO2 was persistently lower than 150 mmHg resulted in higher proportion of patients that achieved lung recruitment (13/36 vs. 1/17 in the prone and non-prone groups, respectively, P = 0.02) [26]. The investigators also reported an increase in PaO2/FiO2 ratio though this was not statistically significant (182 ± 140 in prone vs. 120 ± 61 in supine).
Two studies did not report clinical characteristics and outcomes of patients treated specifically with prone position [23, 27]. Only four of seven studies [25, 26, 29, 30] reported mortality in patients treated with prone position. Reported mortality rates ranged from 6.7% to 100% [25, 26, 29, 30]. However, these studies which reported mortality lacked control groups and did not adjust for clinically significant patient characteristics or severity of illness. One study reported no difference in the subsequent need for intubation in patients who responded to prone position compared with those who did not [30]. None of the studies examined prone position with duration of MV. No serious adverse events were reported in any of the included studies [23, 25–30].
Discussion
Increasing Use of Prone Position in Awake Non-Intubated Patients
There is an increasing use of prone position in non-intubated patients with and without COVID-19. COVID-19 patients are often treated with NIV or HFNC as the initial modality for respiratory support [23, 31]. The benefits of prone position should theoretically apply to spontaneously breathing, non-intubated patients, with improvement in oxygenation while delaying or even avoiding the need for intubation. Collective evidence and the physiological basis of the prone position in ARDS have encouraged several ICUs to incorporate prone position into their management of non-intubated COVID-19 patients [10, 32]. Indeed, we became aware of four studies that were published after completion of our search that described the use of the prone position in non-intubated COVID-19 patients [28–30, 33]. Three of these studies met our inclusion criteria and were included in our systematic review [28–30]. The fourth study did not fit the inclusion criteria of our review as patients were on low-flow or non-rebreather mask oxygen therapy alone [33]. In this latter study, 19/25 (76%) patients responded to prone position with improvement in SpO2 > 95% within 1 h [33]. Additionally, patients who showed improvement in SpO2 > 95% with the prone position, showed a lower intubation rate of 37% (n = 7), compared with 83% (n = 5) in those whose SpO2 remained < 95% 1 h after prone position (mean difference in intubation rate was 46%; 95% CI 10–88%) [33].
Studies conducted in non-COVID-19 patients with acute respiratory failure showed similarly promising results, although the effect on important clinical outcomes such as mortality and ventilator-free days remain unexplored [34–36]. A retrospective study [34] comparing oxygenation (PaO2/FiO2) pre-, during, and post (6–8 h)-prone position in 15 non-intubated adult patients with non-COVID-19-associated hypoxemic acute respiratory failure showed that oxygenation was significantly higher during prone position, with the same PEEP and FiO2 throughout the duration of the prone position (PaO2/FiO2 124 ± 50 mmHg, 187 ± 72 mmHg, and 140 ± 61 mmHg, during pre-, prone, and post steps, respectively, P < 0.001). However, the oxygenation improvement did not persist after return to the supine position, and this was postulated to be secondary to unstable recruitment of dorsal lung regions. The tolerance rate was high (41/43 prone position procedures, 95%), with no significant adverse effects. In a prospective observational study of 20 patients with non-COVID-19-associated moderate to severe ARDS [35], 11/20 (55%) patients avoided intubation when treated with a short duration of prone position (1.8 h ± 0.7, mean of 2.4 ± 1.5 times/day) combined with NIV and HFNC, compared with the expected intubation rate of 75% in patients with moderate to severe ARDS from prior published studies, although this reduction was not statistically significant and did not meet the predetermined threshold of 40% reduction set by the authors. Of this cohort, eight patients (73%) had moderate and three (27%) had severe ARDS, and the addition of prone position to HFNC and NIV resulted in an increase of 25–35 mmHg in PaO2/FiO2. A few case reports demonstrated similar findings of improved oxygenation in non-intubated patients post-lung transplantation [36, 37].
Adverse effects such as pressure sores and tube obstruction associated with prone position in ventilated patients [13, 38] were not seen in the aforementioned studies in non-intubated patients with the same level of hypoxemia. However, it is important to note that studies on non-intubated patients utilized a much shorter duration of prone position (median 3 h [34], at least 30 min [35]) than that recommended in patients with severe ARDS [9]. While collective prior studies suggest that prone position in non-intubated patients with acute respiratory failure can result in improved oxygenation and reduced need for MV, whether this strongly applies to non-intubated COVID-19 patients remains to be determined, as only four descriptive studies [28–30, 33] have been published to date, and further trials in non-intubated prone positioning in COVID-19 patients (NCT04383613, NCT04350723) are under way.
Choosing the Right Patient for Prone Position in COVID-19
Despite limited evidence for prone position in COVID-19, certain radiological features in this disease suggest that prone position may benefit these patients. Radiological features unique to COVID-19 include bilateral multifocal lung involvement with ground-glass opacities, with a predilection for peripheral or posterior lung fields [39] and vascular thickening [40, 41]. As the infection progresses, lung findings progress from unilateral multifocal opacities (in the subclinical stage), rapidly evolving to bilateral diffuse ground-glass opacities (in 1 week) followed by transition to a consolidative pattern by the second week of symptoms [42]. Maximal lung involvement on radiological imaging has been found to peak 10 days from onset of symptoms [43]. Given the predilection for posterior lung lobes and bilateral involvement in COVID-19 pneumonia, prone position may allow recruitment of the diseased posterior lobes and may be potentially beneficial in this viral pneumonia. However, it is important to keep in mind that COVID-19 ARDS presents as a spectrum of clinical phenotypes with varying degrees of lung infiltrates, lung recruitability and compliance, and hence heterogenous respiratory mechanics [44], with some patients more or less likely to respond to prone positioning.
Given this clinical heterogeneity, electrical impedance tomography (EIT), a noninvasive imaging tool that can assess lung recruitment in patients with ARDS, may be a useful technique to guide patient selection for the prone position. Studies on adult populations have shown efficacy of EIT as a bedside tool to evaluate regional ventilation and effectiveness of lung recruitment strategies [45, 46]. However, more research on respiratory mechanics, the utility of EIT and the effect of prone position in COVID-19 patients is needed before definitive management guidelines can be established.
Limitations and Alternatives to Prone Position
It is important to consider the feasibility and practicality of prone position, particularly given the resource constraints of the current pandemic. Absolute contraindications to prone position include unstable spinal or pelvic fractures, open chest or abdomen, central cannulation for extracorporeal membrane oxygenation (ECMO) or ventricular assist devices (Table 2). Relative contraindications include raised intracranial or intraocular pressure, uncontrolled seizures, recent cardiac arrhythmias, precarious central line or ECMO cannula, pregnancy in the second or third trimester, and hemodynamic instability or significant coagulopathy [47, 48]. Systematic reviews have demonstrated a higher incidence of pressure sores, tracheal tube obstruction and dislodgement of thoracostomy tubes with prone position [20, 21]. However, implementation by an experienced team with an adequate number of personnel [19] and the use of standardized protocols can minimize adverse events and occupational injuries to healthcare staff [19, 47, 49]. Additionally, many of the contraindications are unlikely in awake non-intubated patients who may be able to prone and then un-prone themselves either independently or with minimal assistance. Considering the evidence to date, we believe that it is worth investigating the therapeutic benefit of the prone position during the current pandemic, particularly when delivered in a standardized manner with appropriate patient selection and dedicated prone position teams.
Table 2.
Included studies that described prone position in patients with COVID-19, clinical characteristics and outcomes of patients
| Author Date of publication Sample size (n) |
Study outcomes | Age | Respiratory support | ECMOa | Prone position | Mortality (overall) | Mortality (prone) | ||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SDb) | HFNCc n (%) |
NIVd n (%) |
MVe n (%) |
n (%) | n (%) | (n, %) | n | ||
|
Yang et al. 21st Feb 2020 n = 51 |
Primary: 28-day mortality Secondary: need for MV, ARDSf, shock |
59.7 (13.3) | 33 (63) | 29 (55) | 22 (42) | 6 (12) | 6 (12) | 32 (62) | NAg |
|
Ruan et al. 3rd March 2020 n = 150 |
Clinical predictors of outcomes in mild and severe disease | 57.7 (NA) | 41 (27) | 51 (34) | 25 (17) | 7 (5) | 3 (2) | 68 (45) | 3 |
|
Pan et al. 23rd March 2020 n = 12 |
Respiratory mechanics | 59 (9) | 9 (75) | 9 (75) | 3 (25) | 7 (58) | 3 (25) | 1 | |
|
Grasselli et al. 6th April 2020 n = 1591 |
Clinical response in first 6–24 h following ICUh admission | 63 (56–70)m | 0 | 137 (9) | 1150 (72) | 5 (0.3) | 240 (15) | 405 (25) | NA |
|
Elharrar et al. 15th May 2020 n = 24 |
Primary: proportion of responders (PaO2 increase ≥ 20% between before and during PPi) Secondary: PaOj2, PaCOk2, variation before, during and after; feasibility, tolerance, persistent responders |
66.1 (10.2) | 19 (79) | 0 | 5 (20) | 0 | 24 (100) | 0 | 0 |
|
Sartini et al. 15th May 2020 n = 15 |
Respiratory parameters Other: 14-day outcomes (discharged, still treated with prone or intubated) |
59 (6.5) | 0 | 15 (100) | 0 | 0 | 15 (100) | 1 (7) | 1 |
|
Coppo et al. 19th June 2020 n = 56 |
Primary: Variation in oxygenation PaO2/FiOl2 between baseline and resupination Secondary: safety and feasibility of prone position |
57.4 (7.4) | NA | 44 (79%) | 0 | 0 | 56 (100) | 5 (9) | 5 |
aextracorporeal membrane oxygenation, bstandard deviation, chigh-frequency nasal cannula, dnoninvasive ventilation, emechanical ventilation, facute respiratory distress syndrome, gnot available, hintensive care unit, iprone position, jpartial pressure of oxygen, kpartial pressure of carbon dioxide, lfractional concentration of oxygen in inspired air, mmedian (interquartile range)
Anecdotally, “supine chest compression”, achieved by placing a 2-kg weight on bilateral chest walls with the patient in the supine position, was reported as an alternative to prone position in two adults with severe ARDS in whom prone position could not be performed: one patient with polytrauma and another with maxillofacial injury and head injury [50]. Both patients saw an improvement in PaO2/FiO2 within 6 hours of chest wall compression, without major adverse effects or serious complications. The authors postulated that the impediment of the more compliant ventral chest wall by the chest compression technique would result in redistribution of ventilation in favor of the highly perfused dorsal area, hence increasing the ventilation perfusion ratio, similar to the respiratory mechanics of the prone position.
There is an ongoing clinical trial evaluating the effects of supine chest compression on hemodynamics and respiratory parameters in patients with moderate to severe ARDS [51]. Although evidence is lacking to support its use, supine chest compression might be an interesting alternative to prone position, particularly during the COVID-19 pandemic, as it may not require dedicated manpower or an increase in the use of sedatives and paralysis, and has a potentially lower risk of adverse events such as ventilator disconnection or endotracheal-related events, which may in turn reduce the risk of nosocomial spread of infection. Future clinical studies are needed to evaluate the clinical benefits and adverse effects of supine chest compression in patients with ARDS and also in subgroups such as the pediatric population and COVID-19 patients.
Conclusion
Since the start of the pandemic, prone position has gained importance as an adjunctive treatment modality which may not only improve short-term outcomes but also lessen the burden on healthcare resources by improving oxygenation and hence reducing or delaying the need for intubation. However, our systematic review revealed that there was a paucity of rigorous data on the potential efficacy of the prone position in COVID-19 patients. As such, recommendations for utilizing prone position in COVID-19 patients has been extrapolated from previous ARDS studies. The preliminary collective experience seems to suggest that prone position is associated with improvement in lung recruitability [26] as well as improved oxygenation [28–30, 33]. No significant adverse events were reported with the prone position in any of the studies. However, the level of evidence remains low: studies in our review had small sample sizes, were observational in design, and had no comparator groups. As such, there remains a gap in the current evidence for the use of prone position in COVID-19 patients, particularly in non-intubated patients, as well as in relation to clinically significant outcomes such as the need for intubation, mortality and duration of MV. For now, in COVID-19 patients who require MV and meet the criteria for ARDS [52], we recommend the use of prone position as per the Surviving Sepsis Campaign and WHO guidelines [10, 11]. In addition, in our opinion, given the current evidence, a trial of prone position, with close monitoring of clinical parameters, oxygenation and tolerance should be considered for awake, non-intubated COVID-19 patients with hypoxemic respiratory failure, as long as they can be appropriately rescued with intubation and MV if this trial fails, as delay in intubation is in itself associated with increased mortality [53].
COVID-19 disease has resulted in significant and unprecedented demands on healthcare systems around the world. As healthcare systems adapt to the pandemic, it would be an opportune time to design and conduct both high-quality observational studies and RCTs that can elucidate the role of low-cost interventions such as prone positioning, in both intubated and non-intubated patients. At present there are at least 20 registered studies (https://clinicaltrials.gov) which aim to investigate the role of the prone position in COVID-19. An intervention such as this is especially important to investigate, as it is simple, does not require additional costly equipment, and has the potential to help resource-poor facilities to improve clinical outcomes and prevent mortality.
Acknowledgements
We would like to thank our librarian at KK Women’s and Children’s Hospital, Singapore, Miss Peggy Fong Bih Yuh, for her kind assistance in the medical literature search for this review article.
Funding
No funding source or sponsorship was received for this study.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Syeda Kashfi Qadri conducted the search of relevant databases for the systematic review. Syeda Kashfi Qadri, Priscilla Ng, Sin Wee Loh, Theresa Shu Wen Toh and Cheryl Bin Lin reviewed abstracts and full texts for inclusion and performed data extraction for the systematic review. Syeda Kashfi Qadri, Herng Lee Tan, Sin Wee Loh, Theresa Shu Wen Toh, Cheryl Bin Lin and Jan Hau Lee drafted the manuscript. Jan Hau Lee and Syeda Kashfi Qadri contributed to study conception and design, search strategy development, data analysis and revision of the manuscript. Eddy Fan contributed to idea generation, revision of manuscript and feedback.
Disclosures
Eddy Fan has received personal fees from ALung Technologies, Fresenius Medical Care, and MC3 Cardiopulmonary outside the submitted work. Syeda Kashfi Qadri, Priscilla Ng, Theresa Shu Wen Toh, Sin Wee Loh, Herng Lee Tan, Cheryl Bin Lin and Jan Hau Lee have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Open Access
This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
References
- 1.WHO. Coronavirus disease (COVID-19) weekly epidemiological update: World Health Organisation. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200914-weekly-epi-update-5.pdf?sfvrsn=cf929d04_2. Accessed 16 Sept 2020.
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323(16):1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 4.Deng Y, Liu W, Liu K, Fang YY, Shang J, Zhou L, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: a retrospective study. Chin Med J (Engl) 2020;133(11):1261–1267. doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, et al. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA. 2020;324(13):1–13. 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed]
- 6.Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. The RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19 — preliminary report. N Engl J Med. 2020:NEJMoa2021436. 10.1056/NEJMoa2021436
- 7.Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382(19):1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA. 2020;323(16):1582–1589. doi: 10.1001/jama.2020.4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 10.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Crit Care Med. 2020;48(6):e440–e469. doi: 10.1097/CCM.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. [online]. https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf. Accessed 6 Apr 2020.
- 12.Johnson NJ, Luks AM, Glenny RW. Gas exchange in the prone posture. Respir Care. 2017;62(8):1097–1110. doi: 10.4187/respcare.05512. [DOI] [PubMed] [Google Scholar]
- 13.Munshi L, Del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, Meade MO, et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14(Supplement_4):S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- 14.Guérin C. Prone positioning acute respiratory distress syndrome patients. Ann Transl Med. 2017;5(14):289. doi: 10.21037/atm.2017.06.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS with prone positioning. Chest. 2017;151(1):215–224. doi: 10.1016/j.chest.2016.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gattinoni L, Taccone P, Carlesso E, Marini JJ. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med. 2013;188(11):1286–1293. doi: 10.1164/rccm.201308-1532CI. [DOI] [PubMed] [Google Scholar]
- 17.Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345(8):568–573. doi: 10.1056/NEJMoa010043. [DOI] [PubMed] [Google Scholar]
- 18.Taccone P, Pesenti A, Latini R, Polli F, Vagginelli F, Mietto C, et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2009;302(18):1977–1984. doi: 10.1001/jama.2009.1614. [DOI] [PubMed] [Google Scholar]
- 19.Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 20.Sud S, Friedrich JO, Adhikari NK, Taccone P, Mancebo J, Polli F, et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Can Med Assoc J = journal de l’Association medicale canadienne. 2014;186(10):E381–E390. doi: 10.1503/cmaj.140081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bloomfield R, Noble DW, Sudlow A. Prone position for acute respiratory failure in adults. Cochrane Database Syst Rev. 2015;2015(11):CD008095. 10.1002/14651858.CD008095.pub2. [DOI] [PMC free article] [PubMed]
- 22.Matthay MA, Aldrich JM, Gotts JE. Treatment for severe acute respiratory distress syndrome from COVID-19. Lancet Respir Med. 2020;8(5):433–434. doi: 10.1016/S2213-2600(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruan Q, Yang K, Wang W, Jiang L, Song J. Correction to: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(6):1294–1297. doi: 10.1007/s00134-020-06028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan C, Chen L, Lu C, Zhang W, Xia JA, Sklar MC, et al. Lung recruitability in COVID-19-associated acute respiratory distress syndrome: a single-center observational study. Am J Respir Crit Care Med. 2020;201(10):1294–1297. doi: 10.1164/rccm.202003-0527LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elharrar X, Trigui Y, Dols AM, Touchon F, Martinez S, Prud’homme E, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323(22):2336–2338. doi: 10.1001/jama.2020.8255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sartini C, Tresoldi M, Scarpellini P, Tettamanti A, Carcò F, Landoni G, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020;323(22):2338–2340. doi: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coppo A, Bellani G, Winterton D, Di Pierro M, Soria A, Faverio P, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020;8(8):765–774. doi: 10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang K, Zhao W, Li J, Shu W, Duan J. The experience of high-flow nasal cannula in hospitalized patients with 2019 novel coronavirus-infected pneumonia in two hospitals of Chongqing, China. Ann Intensive Care. 2020;10(1):37. doi: 10.1186/s13613-020-00653-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meng L, Qiu H, Wan L, Ai Y, Xue Z, Guo Q, et al. Intubation and Ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology. 2020;132(6):1317–1332. doi: 10.1097/ALN.0000000000003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thompson AE, Ranard BL, Wei Y, Jelic S. Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scaravilli V, Grasselli G, Castagna L, Zanella A, Isgrò S, Lucchini A, et al. Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care. 2015;30(6):1390–1394. doi: 10.1016/j.jcrc.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 35.Ding L, Wang L, Ma W, He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care. 2020;24(1):28. doi: 10.1186/s13054-020-2738-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feltracco P, Serra E, Barbieri S, Persona P, Rea F, Loy M, et al. Non-invasive ventilation in prone position for refractory hypoxemia after bilateral lung transplantation. Clin Transplant. 2009;23(5):748–750. doi: 10.1111/j.1399-0012.2009.01050.x. [DOI] [PubMed] [Google Scholar]
- 37.Feltracco P, Serra E, Barbieri S, Milevoj M, Michieletto E, Carollo C, et al. Noninvasive high-frequency percussive ventilation in the prone position after lung transplantation. Transplant Proc. 2012;44(7):2016–2021. doi: 10.1016/j.transproceed.2012.05.062. [DOI] [PubMed] [Google Scholar]
- 38.Mora-Arteaga JA, Bernal-Ramírez OJ, Rodríguez SJ. The effects of prone position ventilation in patients with acute respiratory distress syndrome. A systematic review and metaanalysis. Med Intensiva. 2015;39(6):359–372. doi: 10.1016/j.medin.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 39.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215(1):87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 40.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, et al. Performance of Radiologists in Differentiating COVID-19 from Non-COVID-19 Viral Pneumonia at Chest CT. Radiology. 2020;296(2):E46–E54. doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19) Radiology. 2020;295(3):715–721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46(6):1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yun L, He HW, Moller K, Frerichs I, Liu D, Zhao Z. Assessment of lung recruitment by electrical impedance tomography and oxygenation in ARDS patients. Medicine (Baltim) 2016;95(22):e3820. doi: 10.1097/MD.0000000000003820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Putensen C, Wrigge H, Zinserling J. Electrical impedance tomography guided ventilation therapy. Curr Opin Crit Care. 2007;13(3):344–350. doi: 10.1097/MCC.0b013e328136c1e2. [DOI] [PubMed] [Google Scholar]
- 47.Dirkes S, Dickinson S, Havey R, O’Brien D. Prone positioning: is it safe and effective? Crit Care Nurs Q. 2012;35(1):64–75. doi: 10.1097/CNQ.0b013e31823b20c6. [DOI] [PubMed] [Google Scholar]
- 48.Bamford P, Denmade C, Newmarch C, Shirley P, Singer B, Webb S, et al. Guidance for: Prone positioning in adult critical care 2019. https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf. Accessed 17 Apr 2020.
- 49.Oliveira VM, Piekala DM, Deponti GN, Batista DCR, Minossi SD, Chisté M, et al. Safe prone checklist: construction and implementation of a tool for performing the prone maneuver. Rev Bras Ter Intensiva. 2017;29(2):131–141. doi: 10.5935/0103-507X.20170023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Samanta S, Soni KD. Supine chest compression: alternative to prone ventilation in acute respiratory distress syndrome. Am J Emerg Med. 2014;32(5):489.e5–489.e6. doi: 10.1016/j.ajem.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 51.ClinicalTrials.gov [Internet]. Antonelli (MD): National Library of Medicine (US). 2020 Jan. Identifier NCT03719937, ArtificiaL Increase in chesT Wall Elastance as an alteRnative to PRONE Positioning in Moderate-to-severe ARDS: a Physiological Study The ALTERPRONE Study. https://clinicaltrials.gov/ct2/show/record/NCT03719937?view=record. Accessed 14 Apr 2020.
- 52.Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 53.Kangelaris KN, Ware LB, Wang CY, Janz DR, Zhuo H, Matthay MA, et al. Timing of intubation and clinical outcomes in adults with acute respiratory distress syndrome. Crit Care Med. 2016;44(1):120–129. doi: 10.1097/CCM.0000000000001359. [DOI] [PMC free article] [PubMed] [Google Scholar]