To the editor:
The incidence and impact of coronavirus disease 2019 (COVID-19) has varied enormously across the globe. The pandemic has negatively impacted organ donation and transplantation in countries that have experienced high rates of infection, including the United States, France, and the United Kindgom, all reporting >50% reductions in transplant activity.1 , 2 Australia has experienced a significantly lower incidence of COVID-19 (Table 1 ). Despite this, the impact on organ transplantation has been significant.
Table 1.
Country-specific epidemiology of coronavirus disease 2019 as of September 23, 2020
| Country | Population (in millions) | Cases | Deaths | Fatality rate per 1000 cases | Incidence rate per 100,000 population | Mortality rate per 100,000 population |
|---|---|---|---|---|---|---|
| United States | 328,240 | 6,361,265 | 190,859 | 30 | 1938 | 58 |
| Spain | 46,755 | 525,549 | 29,516 | 56 | 1124 | 63 |
| France | 67,064 | 383,718 | 30,805 | 80 | 572 | 46 |
| United Kingdom | 66,797 | 354,292 | 41,683 | 118 | 530 | 62 |
| Canada | 37,742 | 134,295 | 9196 | 68 | 356 | 24 |
| Australia | 25,522 | 26,524 | 788 | 30 | 104 | 3 |
Cases of COVID-19 were first detected in Australia in late January 2020 and from March 18 the incidence had exceeded 100 cases per day. Given data from China and Europe revealing exponential increases, overwhelming demand for intensive care unit beds and ventilators and rapidly rising cumulative mortality from COVID-19, Australia anticipated similar outcomes.
Australia’s National Incident Room was engaged, and public health policies to support case detection, contact tracing, quarantine, social distancing, and hand hygiene were implemented nationally. Health care facilities prepared for a surge of hospital admissions to manage severe cases of COVID-19.
The Australian Organ and Tissue Authority and the Transplantation Society of Australia and New Zealand formed the National Transplantation and Donation Rapid Response Taskforce—COVID-19 (Taskforce), including experts in transplantation, organ donation, infectious diseases, and data analytics. The Taskforce was charged with devising and coordinating a national approach to transplantation and donation during the pandemic. Concerned that early posttransplant acquisition of COVID-19 may produce severe disease and mortality, and that growing case numbers in hospitals may limit capacity and compromise safety of donation and transplantation, during March, the Taskforce recommended suspension of all adult kidney transplantation. Urgent heart, lung, liver, and pediatric transplantation continued, following case-by-case assessment of risks and benefits.3 Early communication between donation and transplant clinicians was recommended to minimize futile donor work-ups. All recommendations were implemented nationally.
By mid-April, incident cases had fallen below 20 per day and intensive care unit capacity was uncompromised. The Taskforce recommended resumption of usual donation and transplantation activity on April 24, subject to precautions including donor and recipient screening for COVID-19, which was approved by all government Chief Medical Officers and implemented by all state-based health jurisdictions.
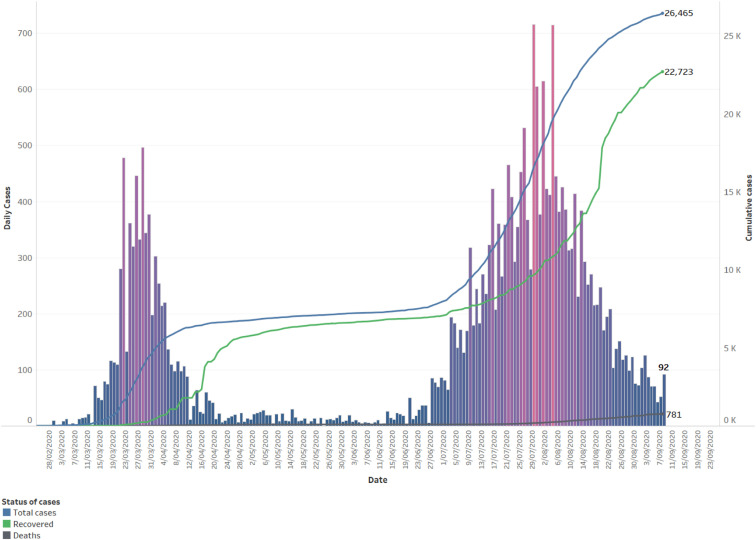
Following suppression of the initial outbreak in March and April 2020, a second wave occurred, primarily in Victoria (Figure 1 ). A jurisdictional response occurred, primarily addressed by public health measures including case detection, contact tracing, and containment via “lock down” border closures and strict travel restrictions. Donation and transplantation services continued but remain impacted by logistical barriers to transportation of organs, medical teams, and patients. Further isolated “outbreaks” are expected for the foreseeable future.
Figure 1.
Daily count and total coronavirus disease 2019 cases since February 20, 2020, by date and status: Australia.
Consequent to COVID-19, kidney transplantation activity is down 27% compared with in 2019, with lesser reductions in liver (8%) and lung (12%). Heart (26%) and pancreas (32%) transplant activity have increased, as seen elsewhere.2 COVID-19 infections have been reported in 19 kidney transplant recipients in Australia, yielding an incidence of 0.15%, similar to the 0.103% seen among the general population, and 1 death in a multimorbid 70-year-old recipient. Ten dialysis patients have contracted COVID-19, 6 of whom died as a result. COVID has been rare among recipients of nonrenal organs. A further impact has been the fear and uncertainty experienced by transplant recipients, those waiting for transplantation, and their carers, both through news of COVID-19 and also resulting from the temporary suspension of transplantation.4
Taken within a global context, the demonstrable negative impact of COVID-19 on donation and transplantation in Australia has been less than that reported for countries with higher caseloads.1 , 2 However, the pattern of impact has been similar2 and remains significant to patients and health systems alike. Despite a lesser impact to date, answers to the same questions posed by more heavily impacted countries are required here too: Is it safer to be transplanted or to remain on dialysis? Can COVID-19 be transmitted by organ transplantation? What treatments are effective, and what are the outcomes of COVID-19 in immunosuppressed patients? Can immunity to COVID-19 be acquired through infection or vaccination, will it be protective, is it durable, and does any of this apply to immunosuppressed populations? Despite differences in global COVID-19 epidemiology, for the organ donation and transplant communities, the questions are essentially the same.
Acknowledgments
Data for COVID-19 epidemiology in Australian dialysis and transplant recipient, the Australian general population, and selected countries were obtained from Stephen McDonald at Australian and New Zealand Dialysis and Transplantation Registry (ANZDATA), Australian Federal Government, and Johns Hopkins University, respectively.
References
- 1.Loupy A., Aubert O., Reese P. Organ procurement and transplantation during the COVID-19 pandemic. Lancet. 2020;395:e95–e96. doi: 10.1016/S0140-6736(20)31040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manara A., Mumford L., Callaghan C.J. Donation and transplantation activity in the UK during the COVID-19 lockdown. Lancet. 2020;396:465–466. doi: 10.1016/S0140-6736(20)31692-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stock P.G., Wall A., Gardner J. for the TTS Ethics Committee. Ethical issues in the COVID era: doing the right thing depends on location, resources, and disease burden. Transplantation. 2020;104:1316–1320. doi: 10.1097/TP.0000000000003291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guha C., Tong A., Baumgart A. Suspension and resumption of kidney transplantation programmes during the COVID-19 pandemic: perspectives from patients, caregivers and potential living donors–a qualitative study. Transpl Int. 2020;33:1481–1490. doi: 10.1111/tri.13697. [DOI] [PMC free article] [PubMed] [Google Scholar]