Highlights
-
•
Acute presentation of Congenital Morgagni hernia in elderly is extremely rare.
-
•
Congenital Morgagni hernia can present with acute small bowel obstruction.
-
•
Early surgical intervention in case of strangulation is required to decrease mortality.
Keywords: Small bowel obstruction, Congenital diaphragmatic hernia, Morgagni hernia, Hernia repair
Abstract
Introduction
Congenital Diaphragmatic hernia (CDH) is a condition in which there is a defect in the diaphragm present at the time of birth. Morgagni hernia is one of the two most common types of CDH which constitutes 2%–4% of diaphragmatic hernias. They mostly remain silent or discovered as an incidental finding on radiological studies. Symptomatic adult Morgagni hernias are extremely rare.
Presentation of case
Elderly woman presented with a 1-day history of abdominal pain, vomiting, and acute onset of respiratory distress. There was no history of trauma to the chest or abdomen. After initial resuscitation, a Chest x-ray was performed which showed bowel shadow under the right hemidiaphragm. She then underwent computed tomography (CT), which showed a defect in the right hemidiaphragm and segment of herniated small bowel loop with fecalization into the thoracic cavity. After initial resuscitation, she underwent laparotomy, reduction of bowel loops, and primary repair of the hernia defect. Postoperatively she remained well and was discharged on 4th post-operative day.
Discussion
Congenital diaphragmatic hernia occurs in 1 out of every 4000–5000 live births. A majority of the patients will be diagnosed either antenatally or will present with respiratory distress in the neonatal period. Presentation in adults is extremely rare and mostly characterized by abdominal pain, vomiting, intestinal obstruction with some acute respiratory distress, at the background of insignificant past medical history. Surgical management is the mainstay of treatment in symptomatic cases.
Conclusion
CDH of Morgagni type can present uncommonly in adults with symptoms. A good history and clinical examination along with aid of chest x-ray and CT scan should establish the diagnosis. Early surgical intervention is key to prevent ischemia and later gangrene of intestinal content.
1. Introduction
Congenital diaphragmatic hernia (CDH) is a birth defect where there is a hole in the diaphragm (the large muscle that makes the anatomical boundary between pleural and peritoneal cavities). This defect can serve as a potential opening through which organs in the abdomen (such as intestines, stomach, and liver) can move into the chest. Its incidence is 1 in 4000–5000 live births [1]. Congenital diaphragmatic hernias are often classified by their position. A Bochdalek hernia is a defect in the posterio-lateral part of the diaphragm. The majority of congenital diaphragmatic hernias are of this type. A Morgnani hernia is a defect involving the anterior part of the diaphragm. This type of congenital diaphragmatic hernia accounts for approximately 2–4 percent of cases [2]. Major complications of CHD are seen in newborn babies where herniation of abdominal contents is associated with pulmonary hypoplasia and breathing difficulties, mostly found in former variant [3]. We report a rare case of Morgagni type of CDH, as per the SCARE checklist [4], presenting in an elderly female with features of complete small bowel obstruction.
2. Presentation of case
A 72-year-old Asian woman presented with a 1-day history of abdominal pain, vomiting, and acute onset of respiratory distress. There was no history of trauma to the chest or abdomen. In her past medical history, she was a known case of hypertension and asthma and was on inhalers for the last 5 years. She had bilateral knee replacements for advanced Osteoarthritis in past. She had an insignificant family history. She did not have a prior history of similar complaints in past and was never picked up in past with any congenital defect in the diaphragm.
General physical examination revealed an elderly female, awake alert, and oriented, with a heart rate of 106 beats/minute, blood pressure of 160/94 mmHg, and respiratory rate of 28 breaths/minute. Focused abdomen examination showed a distended abdomen with mild epigastric tenderness and hypoactive gut sounds. A digital rectal examination was unremarkable.
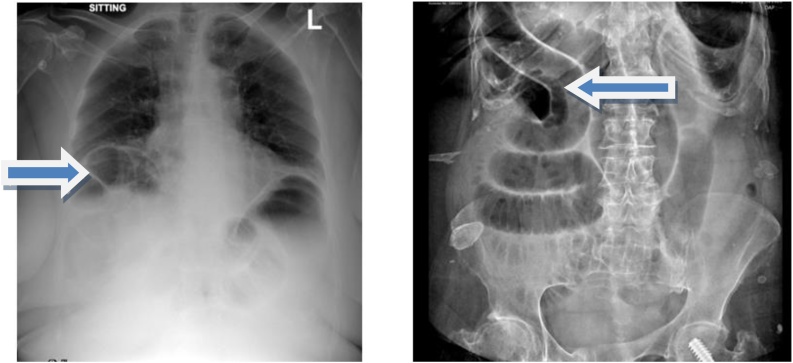
A chest x-ray was done which showed bowel shadow under right Hemi-diaphragm, suggestive of Chilaiditi syndrome, while abdominal plain x-ray showed multiple dilated small bowel loops with the absence of air in the rectum. (Fig. 1a, b). Her baseline workup showed blood urea nitrogen of 8 mg/dl and creatinine of 0.7 mg/dl. She underwent Contrast-enhanced CT Scan (CECT) of chest and abdomen which showed herniation of a segment of the distal ileal loop into the thorax in the right anterior parasternal location through a right side diaphragmatic defect, consistent with Morgagni hernia, the neck of the hernia measured approximately 3.3 cm and the segment of herniated small bowel loop was dilated with fecalization in it. The maximum diameter of the herniation bowel loop was 3.5 cm suggestive of closed-loop obstruction. The terminal ileum and large bowel were largely collapsed (Fig. 2a,b).
Fig. 1.
a, b) Chest and abdominal radiographs demonstrate Chilaiditi syndrome and bowel obstruction, respectively.
Fig. 2.
a and b) Axial and Coronal views of contrast-enhanced abdominal CT scan showing an entrapped bowel loop in right hemithorax suggestive of Morgagni diaphragmatic hernia.
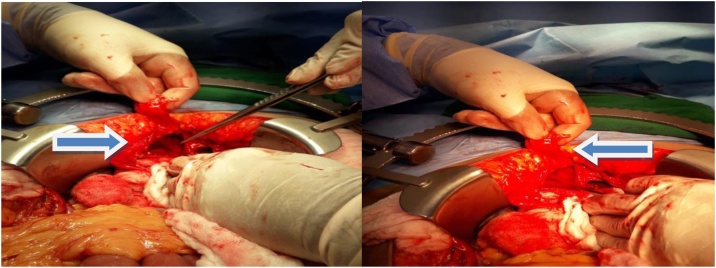
She was initially resuscitated with intravenous fluids and a nasogastric tube in an emergency room which resulted in some relief of her symptoms and her pulse of 84 beats/minute. The patient was taken for emergency operation by general surgery team lead by Consultant general and emergency surgeon, where exploratory laparotomy was performed from xiphisternum up to 1 cm below the umbilicus. Intraoperative findings include herniation of a viable segment of proximal ileum through a defect of approximately 4 cm in the anterior portion of the right hemidiaphragm (Fig. 3a,b). The small bowel was run from Duodenojejunal flexure (DJ) flexure up to an ileocecal junction and large bowel was inspected and no other cause of mechanical bowel obstruction was identified. The later hernia sac was excised and hernia defect was closed with 5 figure of eight interrupted sutures using prolene 1. 28 Fr chest drain was placed in the right thoracic cavity through the same hernia defect. As repair was tension-free, no mesh was used.
Fig. 3.
a) Demonstrates a defect in the anterior half of the right hemidiaphragm. b) Showed hernia sac.
The post-operative period was uneventful. Her nasogastric tube was removed on the first postoperative day and was allowed orally on postoperative day 2, chest drain was removed on postoperative day 4 and she was discharged on the evening of 4th postoperative day when she was tolerating regular diet and had normal bowel movements. In a subsequent follow-up, the patient was doing well, and a repeat chest X-ray was grossly normal.
Later the patient was followed in the clinic after 10 days. She had no active complaint and was fully satisfied with her recovery. Her stitches were removed in the clinic. Later histopathology report showed fibro adipose tissue pieces that measure 10 × 10 cm in aggregate compatible with the diagnosis of the hernia sac.
3. Discussion
Congenital Diaphragmatic hernia (CDH) is a condition in which there is a defect in the diaphragm present at the time of birth. This defect in diaphragm may be present as an isolated lesion or a part of the syndrome [5]. This anatomical defect in diaphragm acts as a potential space that allows abdominal viscera to herniate into the chest cavity. Available literature suggests its incidence of 1 in 4000–5000 live births.
The etiology of CDH largely remains unclear and currently is thought to be multifactorial [6]. The majority of the cases have an isolated diaphragmatic defect presenting with pulmonary hypoplasia and persistent pulmonary hypertension of the newborn (PPHN). Genetic factors, nutritional deficiencies, and environmental factors are attributed to the development of CDH. This condition is often mistakenly taken similar to diaphragmatic eventration, where there is a weakness in muscle bulk of diaphragm without any defect. Diaphragmatic eventration is more common on the right side and is not associated with severe lung hypoplasia. However diaphragmatic agenesis where there is a complete absence of diaphragm is associated with severe lung hypoplasia [7]. Congenital diaphragmatic hernias (CDHs) occur mainly in two locations: the more common type involving, posterior-laterally located foramen of Bochdalek, and less commonly anteriorly located, the foramen of Morgagni [8].
Morgagni hernia is a type of diaphragmatic hernia where the bowel content herniates through an irregular opening first described in 1769 by Italian anatomist and pathologist Giovanni Battista Morgagni) [9]. This type of hernias constitutes only 2%–4% of congenital diaphragmatic hernias and symptomatic adult cases are extremely rare. Such type of hernias mostly remains silent and only come into notice incidentally on investigations performed for other reasons. Rarely, they may present with intestinal obstruction or respiratory symptoms.
Radiological investigations are usually required to establish the diagnosis, assess the contents of the hernia, and evaluate the presence of any associated abnormality. A chest radiograph may reveal an anteromedial mass in Morgagni hernia. A change in the intrathoracic gas pattern may be revealed by repeated chest radiographs. If hernia content includes the stomach, inserting a radio-opaque nasogastric tube will delineate the presence of the stomach in the chest and confirm the diagnosis. The position of herniation and contents is best delineated by the computerized tomographic scan which can also help to rule out differential diagnoses such as a mass in the thoracic cavity, congenital cystic adenomatoid malformation, and the other congenital malformations of lung parenchyma like congenital lobar emphysema [10].
Management of symptomatic or complicated any type of CDH is the surgical repair of hernia using different approaches. Transthoracic approach, transabdominal approach, video-assisted thoracoscopic or laparoscopic techniques, all have been described in the literature. The transabdominal approach makes it easy to reduce the hernia content and repair the defect. It is also regarded as being technically better for repairing bilateral and complicated hernias [8]. The transabdominal approach is mandatory in complications (strangulation, incarceration, or perforation with peritonitis) as the entire abdominal cavity can be inspected. Excision of hernia sac in Morgagni hernia is a debatable issue and hence may largely depend on the skill of the surgeon, the presentation of the individual patient per se, and if surgery can be technically safely guaranteed as in excision of the small sac with no intrathoracic adhesions [8]. Some authors advocate against the excision of hernia sac because of the risk of massive pneumomediastinum, damage to mediastinal structures, and cardiorespiratory complications. Herniorrhaphy is either carried out primarily or in cases in which most of the hemidiaphragm is lacking, using a piece of prosthetic mesh or muscle flap [11]. Primary repair is performed when there is sufficient diaphragm to approximate without tension. The mortality rate for elective surgery has been reported at <4%. However, when the patient presents in an acute state, mortality can be as high as 32%, because of delayed diagnoses or development of severe complications
4. Conclusion
CDH of Morgagni type can present uncommonly in adults. In patients where there is no associated history of thoracoabdominal trauma and have no prior history of abdominal surgery if present with acute onset of complete intestinal obstruction and respiratory distress, the possibility of obstructed diaphragmatic hernia should be in mind. A good history and clinical examination along with aid of chest x-ray and CT scan should establish the diagnosis. Early surgical intervention is key to prevent ischemia and later gangrene of intestinal content.
Declaration of Competing Interest
We declare that we have no conflict of interest.
Funding
We did not receive any funding for this study.
Ethical approval
Exemption was soughted from Ethical review committee (ERC) of Aga Khan University Hospital Karachi with ERC no. 2020-5108-11448. ERC letter is attached with this submission.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
The concept of reporting the case, seeking consent, and drafting the main manuscript was done by Dr. Sabah Uddin Saqib.
Dr. Kulsoom Shaikh contributed to collecting and writing patient information which includes presentation in Emergency room.
Dr. Tabish Chwala, the primary attending surgeon, proofread the article and provided the final approval.
All above authors were also part of surgery of patient.
Registration of research studies
This is a case report and was not an experimental or observational study which requires registration. This is not a research study.
Guarantor
Sabah Uddin Saqib, corresponding author will be main guarantor in this study.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgments
Nursing staff of Aga khan Hospital who took care of the patient.
Contributor Information
Sabah Uddin Saqib, Email: Sabah.saqib@aku.edu.
Kulsoom Hamid, Email: Kulsoom.shaikh@aku.edu.
Tabish Umer Chawla, Email: Tabish.chawla@aku.edu.
References
- 1.Lusk L.A., Wai K.C., Moon-Grady A.J., Steurer M.A., Keller R.L. Persistence of pulmonary hypertension by echocardiography predicts short-term outcomes in a congenital diaphragmatic hernia. J. Pediatr. 2015;166(2) doi: 10.1016/j.jpeds.2014.10.024. 251-6 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Longoni M., Pober B.R., High F.A. Congenital diaphragmatic hernia overview. In: Adam M.P., Ardinger H.H., Pagon R.A., Wallace S.E., Bean L.J.H., Stephens K., editors. GeneReviews((R)) 1993. Seattle (WA) [Google Scholar]
- 3.Tovar J.A. Congenital diaphragmatic hernia. Orphanet J. Rare Dis. 2012;7:1. doi: 10.1186/1750-1172-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P. The SCARE 2018 statement: Updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Dumpa V., Chandrasekharan P. StatPearls; Treasure Island (FL): 2020. Congenital Diaphragmatic Hernia. [PubMed] [Google Scholar]
- 6.Chandrasekharan P.K., Rawat M., Madappa R., Rothstein D.H., Lakshminrusimha S. Congenital diaphragmatic hernia - a review. Matern. Health Neonatol. Perinatol. 2017;3:6. doi: 10.1186/s40748-017-0045-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mirza B., Bashir Z., Sheikh A. Congenital right hemidiaphragmatic agenesis. Lung India. 2012;29(1):53–55. doi: 10.4103/0970-2113.92364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kesieme E.B., Kesieme C.N. Congenital diaphragmatic hernia: a review of current concept in surgical management. ISRN Surg. 2011;2011 doi: 10.5402/2011/974041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elfiky A., Daneshvar D., Krzyzak M., Mukherjee I. Adult-onset Morgagni hernia: medical vs surgical management. Cureus. 2019;11(5):e4626. doi: 10.7759/cureus.4626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prabhu S.M., Choudhury S.R., Solanki R.S., Shetty G.S., Agarwala S. Inadvertent chest tube insertion in congenital cystic adenomatoid malformation and congenital lobar emphysema-highlighting an important problem. Indian J. Radiol. Imaging. 2013;23(1):8–14. doi: 10.4103/0971-3026.113612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Testini M., Girardi A., Isernia R.M., De Palma A., Catalano G., Pezzolla A. Emergency surgery due to diaphragmatic hernia: case series and review. World J. Emerg. Surg. 2017;12:23. doi: 10.1186/s13017-017-0134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]