Abstract
Very few cases of spontaneous otorrhagia (SO) following nonotolaryngologic surgery have ever been reported in surgical literature and none in radiographic. Of the surgical cases reported, SO occurred in the perioperative period following laparoscopic surgeries in the Trendelenburg position. We report the first case of spontaneous bilateral otorrhagia which presented as bilateral external auditory canal masses following endovascular surgery and open decompressive laparotomy in a 60-year-old male with a prior history of hypertension and smoking. We seek to inform radiologists that SO can present on neck imaging as external auditory canal masses as a complication of nonotolaryngologic surgery away from the imaged field of view.
Keywords: Otorrhagia, Spontaneous, Otolaryngology, Endovascular Surgery, Laparotomy
Case report
A 60-year-old male smoker hypertensive patient was initially seen at an outside institution with a chief complaint of sudden onset epigastric pain which radiated to his back. A computed tomography (CT) of the abdomen was performed which showed an infrarenal abdominal aortic aneurysm with a mural hematoma. During his stay in the outside emergency department he became hypotensive requiring transfusion, receiving 8 units of packed red blood cells and 2 units of fresh frozen plasma. His blood pressure stabilized, and he was subsequently transferred to our institution for urgent surgery. The patient had no history of prior otorrhagia, ear infections, or ear surgery.
At our institution, the patient underwent an emergent endovascular repair of the ruptured abdominal aortic aneurysm. Following endovascular surgery, the patient underwent open decompressive laparotomy for intra-abdominal compartment syndrome secondary to an intra-abdominal hematoma. The patient received intraoperatively 10 units of packed red blood cells (pRBCs), 5 units of fresh frozen plasma, 2 units of platelets, and 4 L of crystalloids.
During the laparotomy the patient developed unexpected bleeding within his bilateral ear canals and the procedure was terminated. The patient was transferred to the SICU intubated and sedated.
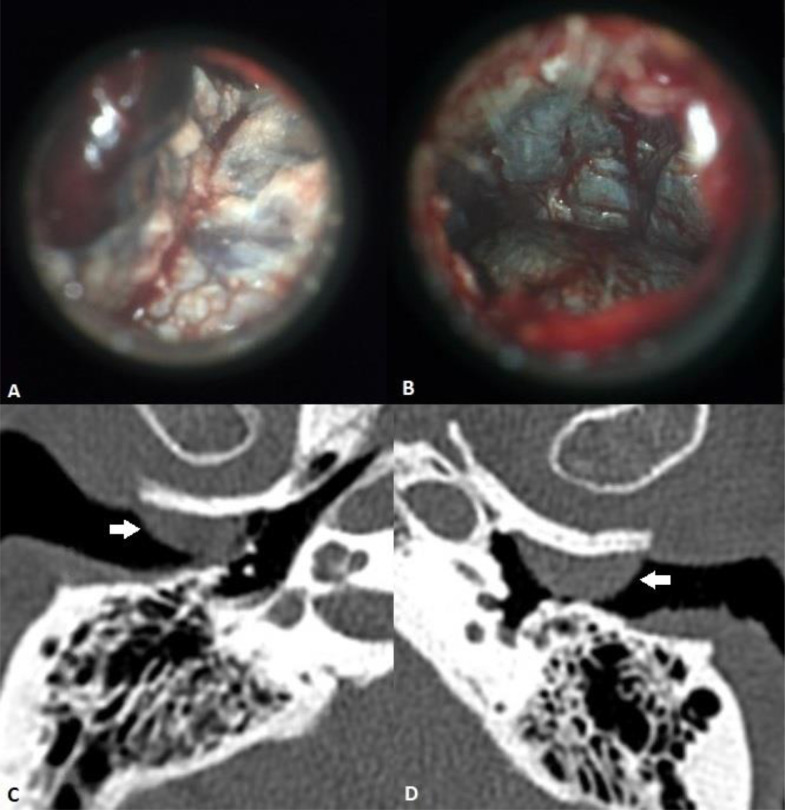
The following morning ENT consult revealed bilateral hemotympanum, tympanic membrane perforations and otorrhagia (Figs. 1 A and B). A CT examination of the temporal bones was requested to rule out alternative underlying middle ear lesions, vascular malformations, glomus tumors, or temporal bone fractures. Noncontrast CT temporal bones (Fig. 1 C and D), demonstrate well-defined, broad-based soft tissue lesions in the bilateral external auditory canals consistent with hemorrhage. There was no aberrant vascular anatomy, soft tissue abnormality or bony erosion. The patient was subsequently discharged from the hospital without further otolaryngologic complications.
Fig. 1.
Right (A) and left (B): Otoscopic images of bilateral hemotympanum and tympanic membrane perforations. Right (C) and left (D): Axial temporal bone CT images show bilateral circumscribed soft tissue masses in the external auditory canals (arrows) consistent with hematomas.
On subsequent audiology clinic visit 2 months later, the patient had bilateral symmetric mild-to-moderately severe sensorineural hearing loss consistent with presbycusis and normal tympanometry. The patient denied any otalgia, recurrent otorrhagia, or subjective loss in hearing. Otoscopic examination revealed dried blood products in the external auditory canal.
Discussion
This is the first report of spontaneous otorrhagia (SO) during nonotolaryngologic surgery in the radiologic literature. Most reported cases occurred after laparoscopic surgery and in the Trendelenburg position, and are described in surgical, anesthesiology, and otology journals. Our case is the third reported to occur in the supine position, with nonlaparoscopic surgery, and the first to happen after endovascular surgery.
The etiology of SO is unclear. Theories include venous hypertension, changes to arterial blood pressure, pneumoperitoneum, and increased middle and inner ear pressures. Contributing factors may include preexisting hypertension, anticoagulation and advanced age, which were present in our case.
In a review and case report published by Aloisi et al, advanced age is suggested as a potential contributing factor. Seven of 10 patients in prior reports were over the age of 59. Our patient was 60 years old [1]. Administration of drugs or factors that may increase the risk of bleeding complications were implicated as well. Our patient's intraoperative INR was 2.51 and may have contributed to the spontaneous otorrhagia [1].
The head-down tilt of Trendelenburg positioning results in an increase in venous return from the lower body because of gravity. There is an increase in central blood volume and mean arterial pressure, with a resultant increase in cardiac output. This may lead to increased venous congestion in the head and neck area, interstitial edema, and vascular congestion [2], [3], [4], [5], [6], [7].
Complications linked to procedures performed in Trendelenburg vary, with the most commonly reported complication involving the head and neck area being otorrhagia [2]. Prolonged deep Trendelenburg positioning has also been associated with increased intraocular pressures, increased optic nerve sheath diameters, and in several reported cases, ischemic optic neuropathy [2,3].
Increases in middle ear pressure may be an alternative mechanism. Vascular congestion in the middle ear canal may lead to desquamation and bleeding [4]. Increases in arterial and venous pressures can cause rupture of subcutaneous capillaries and may result in otorrhagia [5,6].
Impedance of the Eustachian tube's ability to maintain patency between the nasopharynx and middle ear may lead to tympanic membrane rupture. In a case review published by Maerz and Gainsburg [7], a 63-year-old man underwent robotic-assisted laparoscopic prostatectomy with bilateral lymph node dissection and developed right sided otorrhagia and tympanic membrane rupture. The Eustachian tube is partially collapsed at rest and opens via contraction of the tensor veli palatini muscle. Venous congestion from Trendelenburg positioning can cause dysfunction in this mechanism and the pressure equilibrium with the tympanic membrane [7].
Radiologists should be aware that perioperative SO may occur following remote non-otolaryngologic surgery and that their main role is to exclude other causes of otorrhagia. Knowledge of this rare complication will aid in preventing undue investigations and management.
Consent for publication
All patient data has been removed. Images used have no identifying information. No informed consent is required to publish.
Footnotes
Competing interests: The authors have no competing interests/disclosures to report.
Contributor Information
Richard Andrew Teh, Email: r.andrew.teh@gmail.com.
Steven Hoshal, Email: sghoshal@ucdavis.edu.
Gillian L. Hoshal, Email: glhoshal@ucdavis.edu.
Arzu Ozturk, Email: aozturk@ucdavis.edu.
Jennifer Chang, Email: jenchang@ucdavis.edu.
Reza Assadsangabi, Email: assadsangabi@ucdavis.edu.
Vladimir Ivanovic, Email: vivanovic@ucdavis.edu.
Matthew Bobinski, Email: mbobinski@ucdavis.edu.
Osama A. Raslan, Email: oraslan@ucdavis.edu.
References
- 1.Aloisi A, Pesce JE, Paraghamian SE. Bilateral Otorrhagia after robotically assisted gynecologic surgery in the setting of a reduced trendelenburg position and low-pressure pneumoperitoneum: a case report and review of the literature. J Minim Invasive Gynecol. 2017;24(7):1229–1233. doi: 10.1016/j.jmig.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arvizo C, Mehta ST, Yunker A. Adverse events related to Trendelenburg position during laparoscopic surgery: recommendations and review of the literature. Curr Opin Obstet Gynecol. 2018;30:272–278. doi: 10.1097/GCO.0000000000000471. [DOI] [PubMed] [Google Scholar]
- 3.Owens K, Rhoades-Lazenby C. Bilateral otorrhagia discovered at the completion of a robotic bilateral salpingo-oophorectomy. J Gynecol Surg. 2016;32:70–72. doi: 10.1089/gyn.2015.0075. [DOI] [Google Scholar]
- 4.Maerz DA, Beck LN, Sim AJ. Complications of robotic-assisted laparoscopic surgery distant from the surgical site. Br J Anaesth. 2017;118(4):492–503. doi: 10.1093/bja/aex003. [DOI] [PubMed] [Google Scholar]
- 5.Chan R, Cuthbertson D, Jeng Z. Intraoperative ear bleeding with bilateral otorrhagia during laparoscopic sacrocolpopexy. Female Pelvic Med Reconstruc Surg. 2015;21(1):e6–e7. doi: 10.1097/SPV.0000000000000088. [DOI] [PubMed] [Google Scholar]
- 6.Basler K, Malone A, Carmichael M. Spontaneous otorrhagia after laparoscopic pelvic surgery: a report of two cases. J Int Adv Otol. 2017;13(3):434–436. doi: 10.5152/iao.2017.3600. [DOI] [PubMed] [Google Scholar]
- 7.Maerz DA, Gainsburg DM. Tympanic membrane rupture during robotic-assisted laparoscopic prostatectomy. Can J Anesth. 2016;63:772–773. doi: 10.1007/s12630-016-0583-4. [DOI] [PubMed] [Google Scholar]