Abstract
Purpose
We present the case of a 49-year old female who underwent bilateral exchange of a supplementary trifocal sulcus-fixated intraocular lens (IOL) to correct a residual refractive error. Six months beforehand, she had been treated for hyperopia, astigmatism and presbyopia with a duet procedure to create reversible trifocality.
Observations
Refractive lens exchange with combined implantation of a monofocal toric IOL into the capsular bag and a trifocal supplementary IOL into the ciliary sulcus (duet procedure) had been performed in both eyes. Decreased uncorrected distance visual acuity due to the refractive outcome of −0.75 diopter sphere (DS)/-0.25 diopter cylinder (DC)x10° for the right eye and −1.0DS for the left eye as well as the perception of photic phenomena were inacceptable for the patient. In the second operations, we exchanged the supplementary IOLs to correct the residual refractive error and achieve the target refraction of emmetropia. UDVA increased from 0.50 logMAR in both eyes prior to the IOL exchange to −0.22 logMAR in the right eye and −0.20 logMAR in the left eye. Binocular uncorrected near and intermediate visual acuity were −0.10 logMAR and 0.00 logMAR respectively after exchanging the sulcus-fixated supplementary IOLs, allowing for complete spectacle independence.
Conclusions
This case demonstrates one of the most important benefits of the duet procedure: the possibility, if necessary, to easily remove or exchange the supplementary IOL from the ciliary sulcus. The duet procedure offers a safe treatment option in the event of postoperative complications like residual refractive error or intolerance to a multifocal optic.
Keywords: Duet procedure, Reversible trifocality, Supplementary IOL, Spectacle independence, Cataract surgery, Refractive lens exchange
1. Introduction
Supplementary intraocular lenses (IOLs) designed specifically for implantation into the ciliary sulcus are available in monofocal, toric, and diffractive multifocal versions. They can be used to correct postoperative refractive errors or to create multifocality in already pseudophakic eyes without the need to exchange the monofocal IOL implanted into the capsular bag. Multifocal supplementary IOLs can also be used to create reversible multifocality for patients with an uncertainty regarding the individual's tolerance of a multifocal optic. In these cases, a monofocal IOL is implanted into the capsular bag and a supplementary multifocal IOL is implanted into the ciliary sulcus during one surgery, which is also referred to as primary duet procedure.1 If the patient is impaired by the side effects of the multifocal optic or develops a condition in which the multifocal optic is disadvantageous, such as macular degeneration, glaucoma or retinal detachment, the supplementary IOL can be removed relatively easily. Until recently, only bifocal supplementary IOLs have been available for the Duet procedure.2, 3 Diffractive bifocal lenses, however, are functionally inferior to trifocal lenses, primarily due to the lack of intermediate focus.2, 3 Since activities such as PC work, and the use of smartphones and tablets require good intermediate vision and these activities have become increasingly important in recent years, patients who want to be independent of glasses will oftentimes not accept bifocal lenses. The Sulcoflex trifocal IOL was recently introduced by Rayner Intraocular Lenses Ltd. (Worthing, West Sussex, UK) and is a supplementary IOL that makes reversible trifocality possible for the first time.2,3
In this report, we present a case in which the trifocal sulcus fixated IOL was exchanged six months after surgery to correct for a postoperative refractive error. The supplementary IOL was removed and exchanged easily and this underlines the claim that the Duet procedure can indeed provide trifocality, which is reversible, if needed.
2. Case report
A 49-year-old woman presented to our clinic with bilateral hyperopia, astigmatism and presbyopia, and the wish for spectacle independence. The patient felt particularly impaired by wearing varifocal glasses during her work as a nurse. Her uncorrected distance visual acuity (UDVA) was 0.50 logMAR for both eyes and corrected distance visual acuity (CDVA) was 0.00 logMAR for both eyes, with a manifest refraction (MR) of +1.5 diopters sphere (DS)/−0.25 diopters cylinder (DC) x165° for the right eye and a MR of +1.5 DS/-0.25 DC x175° for the left eye. Table 1 summarizes the results for visual acuity testing at different distances. Slit lamp examination showed no pathological findings of the anterior segments and a clear lens in both eyes. Funduscopy and OCT examination showed no pathological findings for the right eye, but in the left eye revealed slight retinal pigment epithelial changes (without edema) of the macula. Endothelial cell density was 2915/mm2 for the right eye and 2772/mm2 for the left eye.
Table 1.
Visual acuity results and refraction before and after surgery. UDVA: uncorrected distance visual acuity, CDVA: corrected distance visual acuity, UNVA: uncorrected near visual acuity, DCNVA: distance corrected near visual acuity, CNVA: corrected near visual acuity, UIVA: uncorrected intermediate visual acuity, DCIVA: distance corrected intermediate visual acuity, OD: right eye, OS: left eye, bin.: binocular.
| preoperatively |
3 months after first surgery |
3 months after second surgery (final result) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OD | OS | bin. | OD | OS | bin. | OD | OS | bin. | |
|
UDVA 4 m |
0.50 | 0.50 | 0.50 | 0.20 | 0.10 | 0.06 | −0.22 | −0.20 | −0.30 |
| Manifest refraction | +1.5/-0.25/165° | +1.5/-0.25/175° | −0.75/-0.25/10° | −1.0/−/− | plano | plano | |||
|
CDVA 4 m |
0.00 | 0.00 | −0.10 | −0.10 | −0.08 | −0.20 | |||
|
UNVA 40 cm |
1.00 | 0.90 | +0.90 | 0.08 | 0.14 | 0.00 | 0.04 | 0.00 | −0.10 |
|
DCNVA 40 cm |
0.80 | 0.70 | +0.60 | 0.32 | 0.30 | 0.18 | |||
| Near addition | +2.0 D | +2.0 D | +1.0 D | +1.0 D | +1.0D | +1.0D | |||
|
CNVA 40 cm |
−0.04 | −0.10 | −0.10 | 0.00 | 0.04 | 0.00 | −0.10 | −0.10 | −0.10 |
|
UIVA 80 cm |
0.04 | 0.04 | −0.10 | 0.00 | −0.02 | 0.00 | |||
|
DCIVA 80 cm |
0.00 | 0.10 | −0.08 | ||||||
The biometry performed with the IOL Master 700 (Carl Zeiss Meditec, Jena, Germany) revealed bilateral corneal astigmatism of −1.34 D x179° for the right eye and −1.37 D x2° for the left eye. The axial lengths were 22.74 mm and 22.85 mm for the right and left eye, respectively.
The patient was informed about different therapeutic options including IOL implantation and the possible complications, risks, benefits and costs of IOL surgery. Considering the retinal pigment epithelial changes in the left eye we recommended a Duet procedure that could be reversed in case of a further deterioration of retinal function: thus, the clear crystalline lens would be removed followed by implantation of a monofocal toric IOL into the capsular bag, targeting for emmetropia, and the implantation of a supplemental trifocal IOL, the Sulcoflex trifocal 703F, with an IOL power of +0.0 D into the ciliary sulcus in the same surgery procedure. The Sulcoflex trifocal 703F IOL is a single piece hydrophilic IOL with a diffractive design and an intermediate addition of +1.75 D and a near addition of +3.5 D. It is available from −3.0 D to +3.0 D in half-diopter steps and from −1.0 D to +1.0 D in quarter-diopter steps. After careful consideration, the patient decided to opt for this procedure.
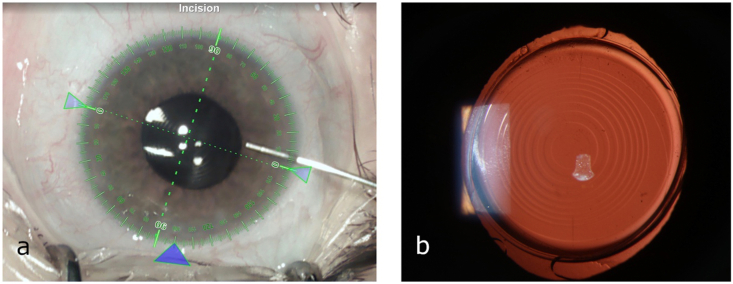
The patient underwent femtosecond laser-assisted phacoemulsification with a LensX Laser (Alcon Laboratories Inc., Fort Worth, TX, USA), followed by implantation of a Rayner RayOne toric RAO610T IOL (Rayner Intraocular Lenses, Ltd., Worthing, West Sussex, UK), with a calculated IOL power of +21.5DS/+1.0DC in both eyes. To calculate the required IOL power of the monofocal toric IOLs, the data from optical biometry (IOL Master 700, Carl Zeiss Meditec, Jena, Germany) was entered into the Raytrace premium IOL calculator (Rayner Intraocular Lenses Ltd., Worthing, West Sussex, UK). We targeted the IOL power closest to plano but on the minus side. We implanted the monofocal toric IOLs into the capsular bag with an axial alignment of 80° for the right eye and 93° for the left eye using the Verion digital marking system (Alcon, Fort Worth, TX, USA) to align the implants. Fig. 1 shows intraoperative images of the first surgery. After implanting the lenses into the capsular bag, we implanted a supplementary IOL, the Rayner Sulcoflex trifocal 703F (Rayner Intraocular Lenses, Ltd., Worthing, West Sussex, UK) with +0.0 D lens power into the ciliary sulcus of each eye to create a trifocal optic. Surgery was performed on the right eye first and on the left eye two days later. The intra-operative and postoperative courses were without complications.
Fig. 1.
Intraoperative images of the right eye during the initial surgery using a digital marking system. (a) After the refractive lens exchange with implantation of a toric IOL into the capsular bag and (b) after the implantation of the trifocal Sulcoflex IOL into the ciliary sulcus. The diffractive rings of the supplementary IOL can be seen clearly in this image.
At the three-month postoperative examination, we noted an unsatisfactory uncorrected distance visual acuity arising from a residual refractive error: UDVA was +0.20 logMAR for the right eye and +0.10 logMAR for the left eye. CDVA was −0.10 logMAR with a MR of −0.75 DS/-0.25 DCx 10° for the right eye and −0.08 logMAR with a MR of −1.0DS for the left eye. Table 1 summarizes the results for visual acuity testing at different distances. In addition, the patient complained about photic phenomena causing problems when driving at night. We discussed different options with the patient to improve the result, including exchanging the trifocal sulcus fixated IOL or corneal refractive surgery to correct the residual refractive error. The patient agreed to a contact lens trial simulating the postoperative result of a correction of the residual refractive error, and she reported she was satisfied with the visual impression during the trial. The patient was also informed that the problematic dysphotopsia might be resolved by removal of the trifocal supplementary IOL and replacement with a monofocal sulcus-fixated IOL solely to correct the refractive error, but that this would be at the expense of spectacle independence at near and intermediate distance. Because of the results obtained in the contact lens trial, the patient decided for exchanging the supplementary trifocal IOL for the same type of supplementary trifocal IOL, however, with an appropriate IOL power to achieve emmetropia. The required IOL power of the new supplementary trifocal IOL was calculated from the manifest refraction using the Raytrace premium IOL calculator and targeting the IOL power closest to plano but on the minus side.
Six months after the initial surgery, the patient underwent another round of surgery on both eyes, to exchange the plano (0.0D) Sulcoflex Trifocal 703F with a lens of the same model that had an IOL power of −1.0D. The IOL exchange was performed on the right eye first and 5 days later on the left eye. Fig. 2a shows an intraoperative image of the right eye acquired after the IOL exchange. These second surgeries on both left and right eyes were uneventful, without any positional changes of the capsular-bag fixated toric IOLs.
Fig. 2.
(a) Intraoperative image of the right eye, acquired after the IOL exchange. (b) Photo in retroillumination at the 3 months follow-up visit showing the final result.
At the follow-up visit three months after the IOL exchange, the patient was satisfied with the result. Fig. 2b shows the anterior segment of the right eye 3 months after the IOL exchange. We found an UDVA of −0.22 logMAR for the right eye and −0.20 logMAR for the left eye. The MR was plano for both eyes. Table 1 shows the results for visual acuity testing at far, intermediate and near distance. We found good functional results in all distances. Fig. 3 shows the binocular defocus curve at 3 months postoperatively, illustrating the three foci created by the trifocal optic. The endothelial cell density remained stable with a postoperative value of 2714/mm2 and 2336/mm2 for the right and left eye respectively.
Fig. 3.
Binocular defocus curve 3 months after the IOL exchange. The curve shows the three foci of the trifocal supplementary IOL.
3. Discussion
While it is often stated that one of the most important benefits from duet procedure is the reversibility of the procedure,2, 3, 4, 5 to our knowledge, there are no published cases of patients who underwent an IOL exchange of a supplementary sulcus fixated IOL. We observed good functional results in our patient for all distances without any complications from exchanging the supplementary IOL.
Polypseudophakia, the use of more than one IOL per eye, was first performed in patients needing a very high IOL power, outside the normal manufacturing power-range. To achieve the desired target refraction, two IOLs were implanted into the capsular bag.6 This “piggybacking” technique, has been associated with interlenticular opacification, a complication attributed to the same pathomechanism as the development of secondary cataract.7,8 Apart from that, capsular contraction after the implantation of two IOLs into the capsular bag could also cause a hyperopic shift.9 To prevent these problems, it was suggested that only one IOL should be implanted into the capsular bag and a second IOL should be placed in the ciliary sulcus. However, implanting a capsular-fixation design of IOL in this anatomical location can give rise to pigment dispersion and elevate the intraocular pressure (IOP). Modern supplementary IOLs are specifically designed in their material, haptic angulation and optic curvature to allow implantation into the ciliary sulcus while preventing interaction with both the primary IOL in the capsule and avoiding contact with iris tissue, thus avoiding interlenticular opacification, elevated IOP and hyperopic shift.10
The main concerns when using sulcus fixated IOLs are the decentration or tilting of the IOL, leading to a decreased image quality and complications from ciliary-body contact such as pigment dispersion, iris transillumination defects and elevated IOP. These complications have been described after the implantation of single piece acrylic (SPA) IOLs into the ciliary sulcus.11,12 SPA IOLs are principally designed for capsular bag implantation and can cause long term complications when placed in the ciliary sulcus. Therefore it is recommended to choose an IOL specifically designed for implanting into the ciliary sulcus.13 An important feature of supplementary IOLs is the changed optical design, away from the biconvex to the convex-concave design. The concave posterior optic surface shape prevents interlenticular opacification by providing space between the supplementary lens and the primarily implanted IOL. Furthermore, the optic and haptic edges of the IOL are either rounded or the haptics are completely round to prevent pigment abrasion at the iris. Such implants are made of hydrophilic acrylate, because this material shows a better uveal compatibility,14,15 which is especially of importance because of the direct proximity to the iris.16
The supplementary IOLs that are specifically designed to be used in the sulcus to create polypseudophakia are, the Sulcoflex IOLs by Rayner Intraocular Lenses Ltd., (Worthing, West Sussex, UK) and the 1stQ Add-On IOLs by 1stQ Deutschland GmbH (Mannheim, Germany).1 These lenses are available as monofocal and monofocal toric IOLs, to correct refractive errors including postoperative astigmatism. Even after careful preparation of a cataract surgery, a deviation from the target refraction can occur. Supplementary IOLs that are designed for implantation into the ciliary sulcus of pseudophakic eyes proved to be a safe and effective option to correct postoperative refractive errors.17, 18, 19 They are successfully used in children and adolescent patients.20 Performing cataract surgery in children can be challenging as the growth of the eye inevitably leads to a change in refraction.21 The implantation of a supplementary IOL in this scenario is a promising treatment option, as it is suggested the lenses can be easily exchanged as the eye ages and intraocular dimensions change.
There are also supplementary multifocal IOLs available that can be used to create a multifocal optic in already pseudophakic eyes. This is a promising option for patients seeking spectacle independence in all distances, as trifocal IOLs can offer good functional results for far, near and intermediate distance.22,23 They provide a better optical quality than monofocal IOLs at near distance and are superior to bifocal and monofocal IOLs at intermediate distance.24,25 Trifocal IOLs can improve the near and intermediate reading acuity.26 However, both bifocal and trifocal diffractive IOLs can cause photic phenomena and reduce contrast sensitivity.27 It was also shown that negative effects on the optical quality from decentration are more severe in diffractive than in monofocal IOLs.28 Only patients without ocular pathologies are considered to be good candidates for multifocal optics, and usually providing multifocal IOL means additional costs for the patients. Therefore, these lenses are usually only offered to a select group of patients.29 It was shown that the secondary implantation of a multifocal supplementary IOL after standard cataract surgery is a safe and efficient option to achieve spectacle independence in patients with pseudo-presbyopia.30,31
The multifocal version can also be used to create multifocality that can be easily reversed if the patient does not tolerate the side effects of the multifocal IOL.
Multifocal optics can cause a reduced contrast sensitivity and photic phenomena such as halo and glare32 and it is difficult to predict if a patient will be impaired by these effects. But even in patients with healthy eyes at the time of the implantation who tolerate the multifocal IOL well, the development of ocular conditions resulting in a loss of function, such as retinal detachment, glaucoma or age-related macular degeneration may cause a problem in the future. In cases of intolerance to side effects from a multifocal optic, the only treatment option is the explantation of the IOL.33 The explantation of an IOL from the capsular bag can lead to the rupture of the posterior capsular bag and vitreous loss.34 If this complication occurs, a sulcus fixated or iris-fixation lens has to be used. The refractive outcome is rather difficult to predict in these cases.35 Postoperative complications after IOL explantation include corneal decompensation, glaucoma and macular edema.36 Therefore, with patients wishing for spectacle independence, it is desirable to offer a safer solution than a capsular-bag fixated multifocal IOL that is going to be difficult to explant in any one of these scenarios. We have already published about the promising results after duet procedure with a multifocal supplementary IOL. We observed good functional results for far, near and intermediate in one case after implanting a trifocal supplementary IOL.4,5 Another patient was implanted with the bifocal version of the IOL and achieved good results for near and far distances.37 In patients with high myopia, the target refraction for the capsular-bag fixated IOL can even be set to −2.5D, to optimize for near distance in case of the necessity to explant the supplementary IOL. Then an adequate IOL power of the sulcus-fixated multifocal IOL can be chosen to achieve emmetropia in this case.37 In a recent laboratory study, our research group demonstrated that the optical quality after duet procedure with a supplementary multifocal IOL is comparable to the optical quality of a single multifocal capsular-fixation IOL, and the optical performance tests show a high tolerance to the decentration of the supplementary IOL.38 Prager et al. examined the centration of sulcus-fixated supplementary IOLs in polypseudophakic eyes and found a significantly better centration of the supplementary IOLs than for the capsular bag-fixated IOLs.39 Our results from optical performance testing are confirmed in clinical studies. Liekfeld et al. and Schrecker et al. both used the capsular bag-fixated Aspira-aAY IOL (HumanOptics AG, Erlangen, Germany) in combination with the sulcus-fixated Diff-sPB IOL (HumanOptics AG, Erlangen, Germany) in one group and the standard multifocal IOL Diffractiva-s (HumanOptics AG, Erlangen, Germany) in the other group. In both studies, the visual outcomes of patients who underwent duet procedure were equivalent to those implanted with a standard bifocal IOL.4,5 In a similar study by Muñoz et al. patients underwent secondary implantation of a sulcus-fixated IOL Acri. LISA 536D multifocal IOL, (Carl Zeiss Meditec AG, Jena, Germany) in one eye and in the other eye a standard multifocal IOL, Acri. LISA 376D multifocal IOL (Carl Zeiss Meditec AG, Jena, Germany), was implanted into the capsular bag. They found comparable results for both techniques.40
Thus, visual results can be achieved with the duet procedure that are equally good as those when implanting a single multifocal IOL into the capsular bag. However, the approach with two IOLs in one eye has the advantage that the second IOL can be removed or exchanged very easily, as described in our case report.
4. Conclusions
This case demonstrates one of the main benefits from duet procedure: The option to easily remove or exchange the supplementary IOL if necessary. The implantation of a monofocal or monofocal toric IOL into the capsular bag and of a supplementary trifocal IOL into the ciliary sulcus in one surgery is a safe procedure to create reversible trifocality. It should prove advantageous in cases where patients seek spectacle independence, but there is uncertainty regarding the patient's eventual tolerance of multifocal optics. Reversibility may also be of advantageous in healthy eyes where patients develop diseases later in their life, when multifocality could be a hindrance (eg, macular degeneration or glaucoma).
4.1. Patient consent
Patient consent to publish an account of this case was not obtained as our report does not contain any information that could lead to the identification of the patient. Retrospective review of this case was done in accordance with the Declaration of Helsinki.
Funding
The Department of Ophthalmology of the University of Heidelberg was supported by the Klaus Tschira Foundation. T. Yildirim is funded by the Physician-Scientist Program of the Heidelberg University, Faculty of Medicine.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Declaration of competing interest
GUA and RK receive research grants, travel grants and lecture fees from Rayner and Alcon. The following authors have no financial disclosures: IDB, TMY, CM.
Acknowledgements
Donald J. Munro made a contribution to the review of the report.
References
- 1.Manzouri B., Dari M.-L., Claoué C. Supplementary IOLs: monofocal and multifocal, their applications and limitations. Asia Pac J Ophthalmol. 2017;6:358–363. doi: 10.22608/APO.2017110. [DOI] [PubMed] [Google Scholar]
- 2.Khoramnia R., Yildirim T.M., Son H.-S., Łabuz G., Mayer C.S., Auffarth G.U. Duet procedure to achieve reversible trifocality. Ophthalmologe: Z Dtsch Ophthalmol Ges. 2020;117(10):999–1004. doi: 10.1007/s00347-020-01096-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khoramnia R., Yildirim T., Son H., Łabuz G., Mayer C., Auffarth G. Correction to: duet procedure to achieve reversible trifocality. Ophthalmologe: Z Dtsch Ophthalmol Ges. 2020;117(10):1005. doi: 10.1007/s00347-020-01109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schrecker J., Kroeber S., Eppig T., Langenbucher A. Additional multifocal sulcus-based intraocular lens: alternative to multifocal intraocular lens in the capsular bag. J Cataract Refract Surg. 2013;39:548–555. doi: 10.1016/j.jcrs.2012.10.047. [DOI] [PubMed] [Google Scholar]
- 5.Liekfeld A., Ehmer A., Schröter U. Visual function and reading speed after bilateral implantation of 2 types of diffractive multifocal intraocular lenses: add-on versus capsular bag design. J Cataract Refract Surg. 2015;41:2107–2114. doi: 10.1016/j.jcrs.2015.10.055. [DOI] [PubMed] [Google Scholar]
- 6.Gayton J.L., Sanders V.N. Implanting two posterior chamber intraocular lenses in a case of microphthalmos. J Cataract Refract Surg. 1993;19:776–777. doi: 10.1016/s0886-3350(13)80349-5. [DOI] [PubMed] [Google Scholar]
- 7.Gayton J.L., Apple D.J., Peng Q. Interlenticular opacification: clinicopathological correlation of a complication of posterior chamber piggyback intraocular lenses. J Cataract Refract Surg. 2000;26:330–336. doi: 10.1016/s0886-3350(99)00433-2. [DOI] [PubMed] [Google Scholar]
- 8.Werner L., Apple D.J., Pandey S.K. Analysis of elements of interlenticular opacification. Am J Ophthalmol. 2002;133:320–326. doi: 10.1016/s0002-9394(01)01405-2. [DOI] [PubMed] [Google Scholar]
- 9.Hesse R.J. Refractive changes produced by capsule contraction after piggyback acrylic intraocular lens implantation. J Cataract Refract Surg. 2002;28:2229–2230. doi: 10.1016/s0886-3350(02)01278-6. [DOI] [PubMed] [Google Scholar]
- 10.Amon M. Correcting refractive surprises following cataract surgery. Cataract Refract Surg Today Eur. 2009:56–59. [Google Scholar]
- 11.Chang D.F., Masket S., Miller K.M. Complications of sulcus placement of single-piece acrylic intraocular lenses: recommendations for backup IOL implantation following posterior capsule rupture. J Cataract Refract Surg. 2009;35:1445–1458. doi: 10.1016/j.jcrs.2009.04.027. [DOI] [PubMed] [Google Scholar]
- 12.Apple D.J., Mamalis N., Reidy J.J. A comparison of ciliary sulcus and capsular bag fixation of posterior chamber intraocular lenses. Am Intra-Ocular Implant Soc J. 1985;11:44–63. doi: 10.1016/s0146-2776(85)80115-4. [DOI] [PubMed] [Google Scholar]
- 13.Mehta R., Aref A.A. Intraocular lens implantation in the ciliary sulcus: challenges and risks. Clin Ophthalmol. 2019;13:2317–2323. doi: 10.2147/OPTH.S205148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abela-Formanek C., Amon M., Schild G., Schauersberger J., Heinze G., Kruger A. Uveal and capsular biocompatibility of hydrophilic acrylic, hydrophobic acrylic, and silicone intraocular lenses. J Cataract Refract Surg. 2002;28:50–61. doi: 10.1016/s0886-3350(01)01122-1. [DOI] [PubMed] [Google Scholar]
- 15.Richter-Mueksch S., Kahraman G., Amon M., Schild-Burggasser G., Schauersberger J., Abela-Formanek C. Uveal and capsular biocompatibility after implantation of sharp-edged hydrophilic acrylic, hydrophobic acrylic, and silicone intraocular lenses in eyes with pseudoexfoliation syndrome. J Cataract Refract Surg. 2007;33:1414–1418. doi: 10.1016/j.jcrs.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Amon M. Biocompatibility of intraocular lenses. J Cataract Refract Surg. 2001;27:178–179. doi: 10.1016/s0886-3350(01)00742-8. [DOI] [PubMed] [Google Scholar]
- 17.Kahraman G., Amon M. New supplementary intraocular lens for refractive enhancement in pseudophakic patients. J Cataract Refract Surg. 2010;36:1090–1094. doi: 10.1016/j.jcrs.2009.12.045. [DOI] [PubMed] [Google Scholar]
- 18.Basarir B., Kaya V., Altan C., Karakus S., Pinarci E.Y., Demirok A. The use of a supplemental sulcus fixated IOL (HumanOptics Add-On IOL) to correct pseudophakic refractive errors. Eur J Ophthalmol. 2012;22:898–903. doi: 10.5301/ejo.5000156. [DOI] [PubMed] [Google Scholar]
- 19.Falzon K., Stewart O.G. Correction of undesirable pseudophakic refractive error with the Sulcoflex intraocular lens. J Refract Surg. 2012;28:614–619. doi: 10.3928/1081597X-20120809-01. [DOI] [PubMed] [Google Scholar]
- 20.Bikbov M., Bikbulatova A., Mannanova R. First results of add-on IOL Sulcoflex implantation in children and adolescents. Oftal'mokhirurgiya. 2012:22. [Google Scholar]
- 21.Yildirim T.M., Auffarth G.U., Son H.-S., Huber C., Beisse F., Khoramnia R. Bilateral trifocal IOL implantation in a pediatric case of cataract following steroid-therapy for acute lymphoblastic leukemia. Am J Ophthalmol Case Rep. 2019;13:46–49. doi: 10.1016/j.ajoc.2018.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cochener B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J Refract Surg. 2016;32:146–151. doi: 10.3928/1081597X-20160114-01. [DOI] [PubMed] [Google Scholar]
- 23.Khoramnia R., Yildirim T., Tandogan T. Optical quality of three trifocal intraocular lens models: an optical bench comparison. Ophthalmologe: Z Dtsch Ophthalmol Ges. 2018;115:21–28. doi: 10.1007/s00347-017-0573-0. [DOI] [PubMed] [Google Scholar]
- 24.Gatinel D., Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013;39:1093–1099. doi: 10.1016/j.jcrs.2013.01.048. [DOI] [PubMed] [Google Scholar]
- 25.Son H.S., Tandogan T., Liebing S. In vitro optical quality measurements of three intraocular lens models having identical platform. BMC Ophthalmol. 2017;17:108. doi: 10.1186/s12886-017-0460-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Attia M.S., Auffarth G.U., Khoramnia R., Linz K., Kretz F.T. Near and intermediate reading performance of a diffractive trifocal intraocular lens using a reading desk. J Cataract Refract Surg. 2015;41:2707–2714. doi: 10.1016/j.jcrs.2015.06.038. [DOI] [PubMed] [Google Scholar]
- 27.Calladine D., Evans J.R., Shah S., Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Sao Paulo Med J. 2015;133 doi: 10.1590/1516-3180.20151331T2. 68-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tandogan T., Son H.S., Choi C.Y., Knorz M.C., Auffarth G.U., Khoramnia R. Laboratory evaluation of the influence of decentration and pupil size on the optical performance of a monofocal, bifocal, and trifocal intraocular lens. J Refract Surg. 2017;33:808–812. doi: 10.3928/1081597X-20171004-02. [DOI] [PubMed] [Google Scholar]
- 29.Wenzel M., Dick H.B., Scharrer A., Schayan K., Reinhard T. Umfrage von BDOC, BVA, DGII und DOG zur ambulanten und stationären Intraokularchirurgie: ergebnisse für das Jahr 2017. Ophthalmo-Chirurgie. 2018;30:255–266. [Google Scholar]
- 30.Khan M.I., Muhtaseb M. Performance of the Sulcoflex piggyback intraocular lens in pseudophakic patients. J Refract Surg. 2011;27:693–696. doi: 10.3928/1081597X-20110512-01. [DOI] [PubMed] [Google Scholar]
- 31.Schrecker J., Langenbucher A. Visual performance in the long term with secondary add-on versus primary capsular bag multifocal intraocular lenses. J Refract Surg. 2016;32:742–747. doi: 10.3928/1081597X-20160630-02. [DOI] [PubMed] [Google Scholar]
- 32.Dick H.B., Krummenauer F., Schwenn O., Krist R., Pfeiffer N. Objective and subjective evaluation of photic phenomena after monofocal and multifocal intraocular lens implantation. Ophthalmology. 1999;106:1878–1886. doi: 10.1016/S0161-6420(99)90396-2. [DOI] [PubMed] [Google Scholar]
- 33.Kamiya K., Hayashi K., Shimizu K. Multifocal intraocular lens explantation: a case series of 50 eyes. Am J Ophthalmol. 2014;158:215–220. doi: 10.1016/j.ajo.2014.04.010. e1. [DOI] [PubMed] [Google Scholar]
- 34.Marques F.F., Marques D.M., Osher R.H., Freitas L.L. Longitudinal study of intraocular lens exchange. J Cataract Refract Surg. 2007;33:254–257. doi: 10.1016/j.jcrs.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 35.Leysen I., Bartholomeeusen E., Coeckelbergh T., Tassignon M.-J.B. Surgical outcomes of intraocular lens exchange: five-year study. J Cataract Refract Surg. 2009;35:1013–1018. doi: 10.1016/j.jcrs.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 36.Mamalis N., Crandall A.S., Pulsipher M.W., Follett S., Monson M.C. Intraocular lens explantation and exchange: a review of lens styles, clinical indications, clinical results, and visual outcome. J Cataract Refract Surg. 1991;17:811–818. doi: 10.1016/s0886-3350(13)80416-6. [DOI] [PubMed] [Google Scholar]
- 37.Yildirim T., Auffarth G., Son H., Mayer C., Tandogan T., Khoramnia R. Duet procedure in high myopia to achieve reversible multifocality. Klin Monatsblatter Augenheilkund. 2020;237(8):958–960. doi: 10.1055/a-0916-8780. [DOI] [PubMed] [Google Scholar]
- 38.Labuz G., Auffarth G.U., Knorz M.C., Son H., Yildirim T.M., Khoramnia R. Trifocality achieved through polypseudophakia: optical quality and light loss compared with a Single trifocal intraocular lens. J Refract Surg. 2020;36(9):570–577. doi: 10.3928/1081597X-20200715-01. [DOI] [PubMed] [Google Scholar]
- 39.Prager F., Amon M., Wiesinger J., Wetzel B., Kahraman G. Capsular bag–fixated and ciliary sulcus-fixated intraocular lens centration after supplementary intraocular lens implantation in the same eye. J Cataract Refract Surg. 2017;43:643–647. doi: 10.1016/j.jcrs.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 40.Muñoz G., Albarran-Diego C., Belda L., Rohrweck S. Add-on sulcus-based versus primary in-the-bag multifocal intraocular lens: intraindividual study. J Refract Surg. 2014;30:320–325. doi: 10.3928/1081597X-20140422-02. [DOI] [PubMed] [Google Scholar]