Abstract
Purpose
Worldwide, patients experience difficulties accessing elective surgical care. This study examined the perceived health, social, and functional impacts of elective surgical cancellations and postponements in Canada.
Methods
We analyzed a subset of aggregate data from the Canadian Community Health Survey (CCHS) annual components from 2005 to 2014. Multivariable logistic regressions examined associations between past-year non-emergency surgical cancellations/postponements and perceived impacts of waiting for surgery (e.g., worry/stress/anxiety, pain, loss of work, loss of income, deterioration of health, relationships suffered).
Results
Among those who experienced a cancellation or postponement of a past-year non-emergency surgery (weighted n = 256,836; 11.8%), 23.5% (weighted n = 60,345) indicated their life was affected by waiting for surgery. After adjusting for type of surgery, year, and sociodemographics, those who experienced a surgical cancellation or postponement had increased odds of reporting their life was affected by waiting for surgery (adjusted odds ratio [aOR], 2.67; 99% confidence interval [CI], 1.41 to 5.1); in particular, they reported greater deterioration of their health (aOR, 3.47; 99% CI, 1.05 to 11.4) and increased dependence on relatives/friends (aOR, 2.53; 99% CI, 1.01 to 6.3) than those who did not have a cancellation or postponement.
Conclusion
Results highlight the multifaceted perceived impacts of surgical cancellations/postponements. These findings suggest there is a need for improvements in reducing elective surgical cancellations and postponements. Results may also inform the development of targeted interventions to improve patients’ health and quality of life while waiting for surgery.
Keywords: surgery, cancellations and postponements, perceived impacts
Résumé
Objectif
Partout dans le monde, les patients ont de la difficulté à accéder aux soins chirurgicaux non urgents. Cette étude a examiné les impacts de santé, sociaux et fonctionnels perçus des annulations et des reports de chirurgies non urgentes au Canada.
Méthode
Nous avons analysé un sous-ensemble de données agrégées à partir des composantes annuelles de l’Enquête sur la santé dans les collectivités canadiennes (ESCC) colligées de 2005 à 2014. Des régressions logistiques multivariées ont examiné les associations entre les annulations / reports de chirurgies non urgentes de l’année précédente et les impacts perçus d’une attente pour une chirurgie (par ex., inquiétude/stress/anxiété, perte de travail, perte de revenus, détérioration de la santé, impact sur les relations interpersonnelles).
Résultats
Parmi les personnes ayant subi une annulation ou un report d’une chirurgie non urgente au cours de l’année précédente (n pondéré = 256 836; 11,8 %), 23,5 % (n pondéré = 60 345) ont indiqué que leur vie avait été affectée par l’attente d’une chirurgie. Après avoir ajusté les données pour tenir compte du type de chirurgie, de l’année et des données sociodémographiques, la probabilité que les personnes ayant vécu une annulation ou un report de chirurgie rapportent que leur vie avait été affectée par l’attente d’une chirurgie était plus élevée (rapport de cotes ajusté [RCA], 2,67; intervalle de confiance [IC] 99 %, 1,41 à 5,1); plus particulièrement, ces personnes rapportaient davantage de détérioration de leur santé (RCA, 3,47; IC 99 %, 1,05 à 11,4) et une dépendance accrue à l’aide de leurs amis/familles (RCA, 2,53; IC 99 %, 1,01 à 6,3) que les personnes n’ayant pas vécu d’annulation ou de retard.
Conclusion
Ces résultats soulignent les facettes multiples des impacts perçus des annulations et reports de chirurgie. En outre, ils démontrent qu’il est nécessaire d’apporter des améliorations pour réduire les annulations et reports des chirurgies non urgentes. Ces résultats pourraient également aider à mettre au point des interventions ciblées pour améliorer la santé et la qualité de vie des patients en attente d’une chirurgie.
Worldwide, elective surgery patients are faced with lengthy waiting times and cancellations. Studies have established rates of elective surgical cancellations ranging from 9 to 44%, with variations according to type of surgery and country.1–7 The 2018 Fraser Institute Report highlights that surgical patients across Canada experience longer waiting times than deemed “clinically reasonable”, ranging from approximately one week longer than reasonable for general surgeries to approximately ten weeks longer than reasonable for orthopedic surgeries.8
Lengthy surgical waiting times have adverse impacts on patients. For example, among orthopedic surgery patients in Canada and Spain, a wait time longer than six months was associated with greater patient dissatisfaction, increased preoperative anxiety and depressed mood, poorer preoperative quality of life, and reduced physical functioning compared with a wait time of less than six months.9,10 Research has also shown negative emotional impacts of waiting for general surgery, including stress, anxiety, frustration, and anger.11,12 Other Canadian studies have found that increased surgical wait times were associated with less improvement in postoperative outcomes (e.g., physical functioning, pain).13,14 In addition, among a Canadian sample of cardiac surgery patients, waiting longer than 97 days was associated with worse pre- and postoperative quality of life, a higher incidence of adverse postoperative events, and a greater likelihood of not returning to work postoperatively.15
Despite extant research on health-related correlates of waiting for surgery, and high rates of surgical cancellations, little is known about the perceived impact of elective surgical cancellations. To our knowledge, no Canadian population-based research to date has established an estimate of elective surgical cancellations or examined patient-reported impacts of those cancellations. Using population-based data, we aimed to understand the health, social, and functional impacts of elective surgical cancellations in Canada. This is a timely study in light of growing recognition of the importance of integrating patient-reported outcomes into healthcare research,16,17 and research showing associations between patient-reported outcomes with objective health outcomes.18 Further, the aims of this study align with the Canadian anesthesia research guidelines, which highlight patient-oriented research as a priority.19 Finally, given the high rates of non-emergent surgical delays and cancellations related to the coronavirus disease pandemic, this research provides insight into some of the broader implications for patients. Considering the limited research in this area, the current study is an exploratory epidemiological examination of relationships between surgical cancellations and postponements with perceived impacts of waiting for elective surgery (e.g., worry/stress/anxiety, pain, deterioration of health, increased dependence on relatives/friends, and loss of work).
Methods
Sample
We analyzed protected aggregate data from the annual components of the Canadian Community Health Survey (CCHS) from 2005 to 2014, maintained at the Research Data Centre in Winnipeg, Manitoba. Access to these data requires security clearance and project approval. The CCHS is an annual, cross-sectional, population-based survey, conducted by Statistics Canada.20 Multistage sampling using three sampling frames selected participants for recruitment, including the Labour Force Survey area frame, telephone number lists, and random digit dialling. Approximately 65,000 Canadians, aged 12 years and older, are surveyed on an annual basis; however, prior to 2007, data were collected from approximately 130,000 individuals every second year. Trained personnel administered the CCHS to consenting participants using computer-assisted interviews. Participants were excluded if they were active members of the Canadian Armed Forces, lived on a Canadian reserve, or were institutionalized. The Manitoba Research Data Centre provided clearance for the use of these data for the current research. Additional details regarding the survey methodology and ethical approval for these surveys have been published elsewhere.20–22
Measures
Non-emergency surgery
As part of the CCHS module on access to healthcare services (ACC), participants were asked whether they required any non-emergency surgery in the past 12 months: “In the past 12 months, did you require any non-emergency surgery?”. Those who responded “yes” were asked what type of surgery they required, as part of the waiting times (WTM) module: “What type of surgery did you require?” (cardiac, cancer, hip/knee, cataract/eye, hysterectomy, gall bladder, other). For those who had multiple past-year surgeries, participants were prompted to respond regarding their most recent surgery. Of note, some participants were still waiting for surgery at the time of the survey across all years included.
Surgical cancellation or postponement
Within the WTM module, participants who required a past-year non-emergency surgery were asked whether their surgery had been cancelled or postponed: “Was your surgery cancelled or postponed at any time?”.
Impacts of waiting for surgery
Also as part of the WTM module, those who required a past-year non-emergency surgery were asked whether they felt affected as a result of waiting for surgery: “Do you think that your health, or other aspects of your life, have been affected in any way due to waiting for this surgery?” (referred to as “life affected total”). Those who responded “yes” were then asked, “How was your life affected as a result of waiting for surgery?”. Participants were permitted to endorse multiple responses, including: worry/anxiety/stress, worry/stress for family/friends, pain, problems with activities of daily living, loss of work, loss of income, increased dependence on relatives/friends, increased use of over-the-counter drugs, overall health deteriorated/condition got worse, health problem improved, personal relationships suffered, other (we excluded “health problem improved” due to insufficient cell sizes). Participants were asked these questions regardless of whether or not they endorsed a surgical cancellation/postponement, with the understanding that all participants undergoing non-emergency surgery waited for surgery. CCHS ACC and WTM modules were both optional; subsequently, only certain provinces responded to these modules each year (see Appendix).
Sociodemographic characteristics
Participants self-reported their age (12–34, 35–49, 50–64, 65+ yr), sex (male, female), marital status (married/common law, widowed/separated/divorced, single), race/ethnicity (White, other), income (< $60,000, $60,000+), and urbanicity (urban, rural). These variables were included in regression models as covariates to account for the variability in impacts of waiting for surgery according to sociodemographic disparities.13
Analytic strategy
Analyses were restricted to those who had a past-year non-emergency surgery. Weighted cross-tabulations assessed the frequency of each impact of waiting for surgery among those who experienced a surgical cancellation/postponement and those who did not. Multivariable logistic regressions examined associations between surgical cancellations/postponements (independent variable; reference = no cancellation/postponement) and impacts of waiting for surgery (dependent variable; each assessed individually). We included an unadjusted model, a model adjusting for type of surgery (i.e., cardiac, cancer, hip/knee, cataract/eye, hysterectomy, gall bladder, other) and year (i.e., 2005–2014; assessed categorically), and a final model additionally adjusting for sociodemographics (i.e., age, sex, marital status, race/ethnicity, income, urbanicity). We computed 99% confidence intervals (CI) and used an alpha cut-off of < 0.01 for regressions to correct for multiple comparisons.
Analyses were conducted using SPSS and STATA statistical software.23,24 Data were weighted and analyses employed 500 bootstrap weights (from each annual CCHS component) for variance estimation to account for the complex survey and sampling design; weights were developed by Statistics Canada and applied as recommended. Please refer to the CCHS User Guide (for years 2005–2014) for additional information regarding sampling, weighting, and bootstraps.
Results
Among those who completed the optional CCHS module on ACC (weighted n = 42,245,996), 7.2% (weighted n = 3,052,072) endorsed a past-year non-emergency surgery. Of those who endorsed a past-year non-emergency surgery and were asked about surgical cancellations/postponements within the module on WTM (weighted n = 2,169,690), 11.8% (weighted n = 256,836) indicated their surgery had been cancelled/postponed. Several participants were still waiting for surgery across all years included (weighted n = 132,717) at the time of survey administration. As shown in Table 1, participants who experienced a surgical cancellation/postponement were primarily between the ages of 35 and 64 (59.2%), White (87.4%), and married (71.1%), with a household income of less than $60,000 (51.5%), and living in an urban area (83.3%). There was a similar proportion of males (49.4%) and females (50.6%) who experienced a cancellation/postponement. These individuals waited, on average, over 65 days longer for surgery than those who did not experience a cancellation/postponement (121.6 days vs 55.8 days; t = 6.7, P < 0.001), and on average, individuals who experienced a cancellation/postponement and noted being affected by waiting for surgery endorsed 2.5 types of impacts of waiting. Differences also emerged in rates of cancellations/postponements according to type of surgery (Χ2 = 44.5, P < 0.001); cancellations/postponements were highest for those who had gall bladder surgery (23.3%) and lowest for those who had cancer surgery (6.5%; see Figure).
Figure.
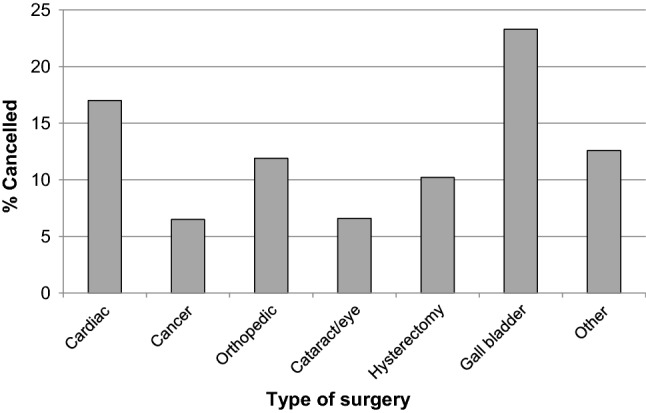
Surgical cancellations according to type of surgery
Table 1.
Sample characteristics of those who experienced a past-year non-emergency surgical cancellation/ postponement and those who did not
| Past-year non-emergency surgery and asked about surgical cancellation/postponement: n = 2,169,690 | Chi-square | ||
|---|---|---|---|
| Yes cancellation/postponement | No cancellation/postponement | ||
| n(%) | 256,836 (11.8) | 1,912,854 (88.2) | |
| Age, yr | 19.3*** | ||
| 12–34 (young adults) | 55,625 (21.7) | 483,932 (25.3) | |
| 35–49 (middle-aged adults) | 82,149 (32.0) | 481,306 (25.2) | |
| 50–64 (young-old adults) | 69,809 (27.2) | 486,129 (25.4) | |
| 65+ (older adults) | 49,253 (19.2) | 461,487 (24.1) | |
| Sex | 6.4* | ||
| Male | 126,775 (49.4) | 842,180 (44.0) | |
| Female | 130,061 (50.6) | 1,070,674 (56.0) | |
| Race/ethnicity | 0.2 | ||
| White | 215,067 (87.4) | 1,591,208 (86.7) | |
| Other | 31,116 (12.6) | 243,503 (13.3) | |
| Marital status | 6.1 | ||
| Married/common law | 181,735 (71.1) | 1,264,166 (66.1) | |
| Widowed/separated/divorced | 32,072 (12.5) | 279,319 (14.6) | |
| Single | 41,926 (16.4) | 368,519 (19.3) | |
| Income, $ | 2.1 | ||
| < 60,000 | 81,603 (51.5) | 678,275 (55.1) | |
| ≥ 60,000 | 76,827 (48.5) | 552,396 (44.9) | |
| Urbanicity | 0.7 | ||
| Urban | 214,005 (83.3) | 1,568,792 (82.0) | |
| Rural | 42,831 (16.7) | 344,062 (18.0) | |
| Type of surgery | 44.5*** | ||
| Cardiac | 11,025 (4.3) | 53,935 (2.8) | |
| Cancer | 7,978 (3.1) | 115,624 (6.1) | |
| Orthopedic | 16,448 (6.4) | 122,083 (6.4) | |
| Cataract/eye | 16,067 (6.3) | 227,542 (11.9) | |
| Hysterectomy | 4,095 (1.6) | 35,943 (1.9) | |
| Gall bladder | 10,627 (4.1) | 34,931 (1.8) | |
| Other | 190,415 (74.2) | 1,320,770 (69.1) | |
| Wait time for surgery (days) | 121.6 (9.6)a | 55.8 (2.1)a | 6.7***b |
Values represent the n (%) of each sociodemographic characteristic and type of surgery among those who did and did not experience a surgical cancellation/postponement
aValues represent M (SE) = mean with standard error; bValues represent t statistic
*P < 0.05, **P < 0.01, ***P < 0.001
Among those who endorsed a past-year surgical cancellation/postponement, 23.5% (95% CI, 17.5 to 30.9; weighted n = 60,345) reported their life was affected by waiting for surgery; in comparison, 10.9% (95% CI, 9.7 to 12.2; weighted n = 207,391) of individuals who did not experience a cancellation/postponement indicated their life was affected by waiting for surgery. Common types of impacts for individuals who experienced cancellations/postponements included pain (10.8%; 95% CI, 7.1 to 16.2; weighted n = 27,784), worry/stress/anxiety (10.6%; 95% CI, 7.4 to 15.0; weighted n = 27,246), and problems with activities of daily living (8.8%; 95% CI, 5.4 to 13.9; weighted n = 22,467); these impacts were prevalent among 6.2% (95% CI, 5.2 to 7.4; weighted n = 118,746), 5.6% (95% CI, 4.6 to 6.7; weighted n = 106,085), and 4.2% (95% CI, 3.4 to 5.3; weighted n = 81,007) of those who did not experience cancellations/postponements, respectively. Less common impacts for individuals who experienced cancellations/postponements included loss of income (1.4%; 95% CI, 0.7 to 2.8; weighted n = 3,488), personal relationships suffered (1.7%; 95% CI, 0.8 to 3.4; weighted n = 4,341), and increased use of over-the-counter drugs (3.2%; 95% CI, 1.4 to 7.0; weighted n = 8,233); these impacts were prevalent among 1.4% (95% CI, 0.9 to 2.2; weighted n = 26,604), 1.1% (95% CI, 0.6 to 1.9; weighted n = 20,930), and 1.5% (95% CI, 1.0 to 2.4; weighted n = 28,877) of those who did not experience cancellations/postponements, respectively (note: weighted n values for impacts among the no cancellation/postponement group are larger than those in the cancellation/postponement group because of the large majority [> 88%] not experiencing a cancellation/postponement; however, as evident by the weighted percentage, most impacts were more prevalent among the cancellation/postponement group).
In the most stringent model of multivariable logistic regressions, those who experienced a surgical cancellation/postponement had significantly increased odds of indicating their life was affected by waiting for surgery (adjusted odds ratio [aOR], 2.67; 99% CI, 1.41 to 5.1; P < 0.001) than those who did not experience a cancellation/postponement. In particular, these individuals had significantly increased odds of endorsing overall health deterioration (aOR, 3.47; 99% CI, 1.05 to 11.4; P = 0.007) and increased dependence on relatives/friends (aOR, 2.53; 99% CI, 1.01 to 6.3; P = 0.009) as a result of waiting for surgery (see Table 2).
Table 2.
Associations between surgical cancellations/postponements and impacts of waiting for surgery
| Impacts of waiting for surgery | Weighted n (%) of each impact | OR (99% CI) | aOR1 (99% CI) | aOR2 (99% CI) | |
|---|---|---|---|---|---|
| No cancellation/ postponement |
Yes cancellation/ postponement |
Surgical cancellation/postponement | |||
| Life affected total |
207,391 (10.9) |
60,345 (23.5) |
2.52 (1.49 to 4.28)*** |
2.44 (1.41 to 4.24)*** |
2.67 (1.41 to 5.1)*** |
| Pain |
118,746 (6.2) |
27,784 (10.8) |
1.83 (0.97 to 3.47) |
1.71 (0.89 to 3.31) |
1.78 (0.85 to 3.72) |
| Worry/stress/anxiety |
106,085 (5.6) |
27,246 (10.6) |
2.02 (1.16 to 3.52)** |
1.92 (1.10 to 3.35)** |
1.47 (0.76 to 2.85) |
| Problems with ADLs |
81,007 (4.2) |
22,467 (8.8) |
2.17 (1.02 to 4.60)** |
2.07 (0.98 to 4.37) |
2.12 (0.94 to 4.78) |
| Overall health deteriorated |
54,105 (2.8) |
19,207 (7.5) |
2.77 (0.91 to 8.4)* |
2.78 (0.87 to 8.8) |
3.47 (1.05 to 11.4)** |
| Worry/stress for family/friends |
40,862 (2.1) |
11,833 (4.6) |
2.21 (0.93 to 5.3) |
2.12 (0.95 to 4.75) |
1.99 (0.81 to 4.94) |
| Increased dependence on relatives/friends |
26,560 (1.4) |
10,295 (4.0) |
2.96 (0.98 to 8.9) |
2.89 (1.03 to 8.1)** |
2.53 (1.01 to 6.3)** |
| Loss of work |
35,811 (1.9) |
9,062 (3.5) |
1.91 (0.53 to 6.9) |
1.79 (0.47 to 6.9) |
– |
| Increased use of over-the-counter drugs |
28,877 (1.5) |
8,233 (3.2) |
2.16 (0.57 to 8.2) |
2.04 (0.62 to 6.6) |
2.02 (0.81 to 5.0) |
| Personal relationships suffered |
20,930 (1.1) |
4,341 (1.7) |
1.55 (0.45 to 5.4) |
– | – |
| Loss of income |
26,604 (1.4) |
3,488 (1.4) |
0.98 (0.31 to 3.05) |
– | – |
| Other |
26,693 (1.4) |
9,366 (3.7) |
2.67 (0.82 to 8.7) |
2.55 (0.89 to 7.2) |
– |
Note. Reference group = no cancellation/postponement; Weighted n (%) = prevalence of each dependent variable among those who did and did not experience a surgical cancellation/postponement; OR = unadjusted odds ratio; aOR1 = adjusted odds ratio, controlling for type of surgery and year; aOR2 = adjusted odds ratio, controlling for type of surgery, year, and sociodemographics (i.e., age, sex, marital status, race/ethnicity, income, urbanicity); CI = confidence interval; ADLs = activities of daily living. – = could not compute estimates because of small cell sizes. **P < 0.01, ***P < 0.001
Discussion
To our knowledge, this is the first study to examine patient-reported health, social, and functional impacts of waiting for surgery associated with non-emergent surgical cancellations and postponements, using population-based data. Results revealed nearly one quarter of individuals who experienced a surgical cancellation/postponement indicated their life was affected by waiting for surgery; this represents over double the number of individuals endorsing an impact among those whose surgery was not cancelled or postponed. These results highlight the broad implications of surgical cancellations/postponements. Results also underscore the importance of targeted interventions both to reduce cancellation/postponement rates and to provide additional supports to patients while they are waiting for surgery.
Although, to our knowledge, no previous population-based estimates exist of the proportion of patients with surgical cancellations whose lives were impacted, prior research with smaller samples has yielded estimates of 20–45% endorsing emotional and financial impacts of cancellations.25,26 More recently, a study examining nearly 400 patients who experienced a surgical cancellation revealed that over 30% reported extreme emotional impacts (e.g., extreme sadness, stress, anger) and nearly 60% reported moderate concern about their deteriorating health condition as a result of the cancellation.27 The lower value from the current study may reflect the fact that the majority of patients eventually underwent surgery, meaning the adverse impacts of their surgical cancellations/postponements may have been less salient at the time of the survey.
Participants with surgical cancellations/postponements in the current study endorsed poorer physical health, increased functional impairments, and worse psychological functioning than those who did not experience surgical cancellations/postponements. For example, over 10% of those who experienced a cancellation/postponement endorsed increased pain (10.8%) and mental health symptoms (e.g., worry/stress/anxiety; 10.6%) related to waiting for surgery, compared with only 5–6% of those who did not experience a cancellation/postponement. Of concern, several prior studies have shown that preoperative mental health symptoms and pain are associated with greater surgical complications and poorer postoperative quality of life.28–30 Taken together, these results highlight the potential adverse impact of surgical cancellations/postponements on perioperative outcomes and the need for improvements in patient care during the waiting period for elective surgery.
With a few exceptions, all impacts of waiting for surgery were elevated for those who experienced a cancellation/postponement compared with those who did not. The largest discrepancies between groups emerged for increased dependence on relatives/friends (4.0% vs 1.4%; OR, 2.96) and deterioration in overall health (7.5% vs 2.8%; OR, 2.77), evidenced by the largest effect sizes from the unadjusted regression model; these impacts were also associated with the strongest effects in the fully adjusted model (aOR, 2.53 and 3.47, respectively). The relatively consistent trend of increased adverse impacts for those with surgical cancellations/postponements suggest the impacts assessed are likely interrelated (i.e., do not occur in isolation); in fact, those who experienced a cancellation/postponement and noted being affected by waiting for surgery endorsed 2.5 types of impacts on average. For example, individuals who experience deterioration in their health while waiting for surgery may become less able to function, and subsequently may become more dependent on social support systems (e.g., relatives, friends). Despite the generally consistent elevation across impacts, each impact has unique and notable implications. For example, becoming increasingly dependent on social support systems may be associated with higher rates of caregiver burnout,31 experiencing increased pain may impact activity levels and general mobility,32,33 and increased use of over-the-counter drugs can lead to maladaptive self-medicating practices.34
Although this study produced novel findings, they must be considered alongside some limitations. First, although the CCHS is a population-based survey, results may not generalize to the full Canadian population because of the optional nature of the modules of interest and the exclusion of active members of the Canadian Armed Forces, those living on a Canadian reserve, and institutionalized individuals. Relatedly, because institutionalized individuals (e.g., those who are hospitalized at the time of the survey) were excluded, results may not have captured the full severity of adverse health impacts associated with surgical cancellations/postponements. Second, we were unable to determine whether results differ according to the province of residence because of limited participation in the modules of interest, or whether there are differences in impacts according to type of surgery because of limited statistical power. Although we were able to examine rates of cancellations according to type of surgery, this analysis was limited to the categories defined by the CCHS, and we were unable to further subcategorize the “other” surgery category. Third, although analyses were focused on non-emergency surgery specifically, we were unable to identify whether or not participants were outpatients or inpatients preoperatively, which would have provided important context to the cancellation/postponement rate.35 Fourth, all variables in this study were assessed by self-report, which may be susceptible to response biases. Nevertheless, patient-reported outcomes (i.e., self-reported) are designed to capture patients’ lived experiences, and research has shown that these subjective measures have utility in understanding outcomes in health research, and how to improve patient healthcare experiences.17 In addition, the current study focused on past-year surgeries, as opposed to lifetime surgeries, which likely limits issues related to recall bias, specifically. Fifth, as indicated, the majority of participants had already undergone surgery at the time of the survey; this may have resulted in a reporting bias, where the adverse impacts of waiting for surgery were underestimated as a result of these experiences being less salient at the time of the survey. Sixth, due to the cross-sectional nature of the CCHS, caution is warranted upon inferring temporality and causality regarding the emergent associations. Finally, it is possible that factors leading to surgical cancellations/postponements directly contributed to the adverse impacts of waiting for surgery, as opposed to the cancellation/postponement having a direct and independent influence on the impacts of waiting.
Despite these limitations, results of this study are in line with the Canadian Anesthesia Research Priority Setting Partnership’s “top 10” priorities, geared toward improving patients’ anesthesia care experiences.19 The current study produced novel findings that have important implications for the healthcare system. Over 85% of elective surgical cancellations are preventable, and cost the United States healthcare system approximately 5,000 USD per cancellation, totalling millions of dollars per year36,37 (to our knowledge, these rates have not been estimated using Canadian data). In addition to systemic costs, results from this study highlight the multifaceted perceived impacts of surgical cancellations/postponements. These results outline the need for reductions in elective surgery cancellations and postponements, as well as improved support for patients who are affected by these cancellations and postponements. Results also underscore the importance of developed interventions to reduce preventable cancellations. For example, research has shown that improved preoperative anesthesia interviews,38 modifications to surgical scheduling procedures,39 and increased communication between healthcare professionals and surgical patients40 can help reduce elective surgical cancellation rates. Further investigation is warranted to address additional strategic intervention opportunities for reducing surgical cancellation rates. Finally, results may inform the development of targeted interventions to improve patients’ health status and quality of life while waiting for surgery, which may have positive implications for the healthcare system. Further research is warranted to understand other health-related impacts of patient difficulties accessing surgical care and how these impacts translate to health status and potential complications at the time of surgery.
Acknowledgments
Author contributions
Jordana Sommer and Renée El-Gabalawy contributed to all aspects of this manuscript including study conception and design, analysis and interpretation of data, and drafting the article. Eric Jacobsohn contributed to study conception, interpretation of data, and drafting the article.
Acknowledgements
Although the research and analysis are based on data from Statistics Canada, the opinions expressed do not represent the views of Statistics Canada or the Canadian Research Data Centre Network (CRDCN). Dr. El-Gabalawy is funded by University of Manitoba Start-Up Funding and Ms. Sommer receives doctoral funding through the Canadian Institutes of Health Research.
Disclosures
None.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Gregory L. Bryson, Deputy Editor-in-Chief, Canadian Journal of Anesthesia.
APPENDIX
Provinces that completed the ACC and WTM modules according to survey cycle
| Year | ACC module | WTM module |
|---|---|---|
| 2005/2006 | New Brunswick | New Brunswick |
| 2007 | Ontario | Ontario |
| 2008 | New Brunswick | – |
| 2009 | Ontario | Ontario |
| 2010 | Ontario | Ontario |
| 2011 | British Colombia | – |
| 2012 | Newfoundland, New Brunswick, British Colombia | Newfoundland |
| 2013 | Nova Scotia | – |
| 2014 | Newfoundland, Nova Scotia, New Brunswick | Newfoundland |
Provinces had the opportunity to opt out of answering certain modules of the Canadian Community Health Survey; ACC = access to healthcare services; WTM = waiting times
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Argo JL, Vick CC, Graham LA, et al. Elective surgical case cancellation in the Veterans Health Administration system: Identifying areas for improvement. Am J Surg. 2009;198:600–606. doi: 10.1016/j.amjsurg.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Caesar U, Karlsson J, Olsson LE, Samuelsson K, Hansson-Olofsson E. Incidence and root causes of cancellations for elective orthopaedic procedures: a single center experience of 17,625 consecutive cases. Patient Saf Surg. 2014 doi: 10.1186/1754-9493-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seim AR, Fagerhaug T, Ryen SM, et al. Causes of cancellations on the day of surgery at two major university hospitals. Surg Innov. 2009;16:173–180. doi: 10.1177/1553350609335035. [DOI] [PubMed] [Google Scholar]
- 4.Prin M, Eaton J, Mtalimanja O, Charles A. High elective surgery cancellation rate in Malawi primarily due to infrastructural limitations. World J Surg. 2018;42:1597–1602. doi: 10.1007/s00268-017-4356-1. [DOI] [PubMed] [Google Scholar]
- 5.Abeeleh MA, Tareef TM, Hani AB, et al. Reasons for operation cancellations at a teaching hospital: prioritizing areas of improvement. Ann Surg Treat Res. 2017;93:65–69. doi: 10.4174/astr.2017.93.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Appavu ST, Al-Shekaili SM, Al-Sharif AM, Elawdy MM. The burden of surgical cancellations and no-shows: quality management study from a large regional hospital in Oman. Sultan Qaboos Univ Med J. 2016;16:e298–e302. doi: 10.18295/squmj.2016.16.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fayed A, Elkouny A, Zoughaibi N, Wahabi HA. Elective surgery cancelation on day of surgery: an endless dilemma. Saudi J Anaesth. 2016;10:68–73. doi: 10.4103/1658-354X.169479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barua B, Jacques D. Waiting Your Turn: Wait Times for Health Care in Canada, 2018 report. Fraser Institute, 2018. Available from URL : https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2018 (accessed September 2020).
- 9.Lizaur-Utrilla A, Martinez-Mendez D, Miralles-Munoz FA, Marco-Gomez L, Lopez-Prats FA. Negative impact of waiting time for primary total knee arthroplasty on satisfaction and patient-reported outcome. Int Orthop. 2016;40:2303–2307. doi: 10.1007/s00264-016-3209-0. [DOI] [PubMed] [Google Scholar]
- 10.Salci L, Ayeni O, Farrokhyar F, Dao D, Ogilvie R, Peterson D. Impact of surgical waitlist on quality of life. J Knee Surg. 2016;29:346–354. doi: 10.1055/s-0035-1564596. [DOI] [PubMed] [Google Scholar]
- 11.Gregory DM, Temple Newhook J, Twells LK. Patients’ perceptions of waiting for bariatric surgery: a qualitative study. Int J Equity Health. 2013 doi: 10.1186/1475-9276-12-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oudhoff JP, Timmermans DR, Knol DL, Bijnen AB, van der Wal G. Waiting for elective general surgery: impact on health related quality of life and psychosocial consequences. BMC Public Health. 2007 doi: 10.1186/1471-2458-7-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nikolova S, Harrison M, Sutton M. The impact of waiting time on health gains from surgery: evidence from a national patient-reported outcome dataset. Health Econ. 2016;25:955–968. doi: 10.1002/hec.3195. [DOI] [PubMed] [Google Scholar]
- 14.Braybrooke J, Ahn H, Gallant A, et al. The impact of surgical wait time on patient-based outcomes in posterior lumbar spinal surgery. Eur Spine J. 2007;16:1832–1839. doi: 10.1007/s00586-007-0452-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sampalis J, Boukas S, Liberman M, Reid T, Dupuis G. Impact of waiting time on the quality of life of patients awaiting coronary artery bypass grafting. CMAJ. 2001;165:429–433. [PMC free article] [PubMed] [Google Scholar]
- 16.Pezold ML, Pusic AL, Cohen WA, et al. Defining a research agenda for patient-reported outcomes in surgery: using a Delphi survey of stakeholders. JAMA Surg. 2016;151:930–936. doi: 10.1001/jamasurg.2016.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lavallee DC, Chenok KE, Love RM, et al. Incorporating patient-reported outcomes into health care to engage patients and enhance care. Health Aff (Millwood) 2016;35:575–582. doi: 10.1377/hlthaff.2015.1362. [DOI] [PubMed] [Google Scholar]
- 18.Ranganath VK, Strand V. Importance of ‘meeting of the minds’: patient-reported outcomes and MRI. Ann Rheum Dis. 2017;76:473–475. doi: 10.1136/annrheumdis-2016-210058. [DOI] [PubMed] [Google Scholar]
- 19.James Lind Alliance Priority Setting Partnership. Anaesthesia (Canada) Top 10. Available from URL: http://www.jla.nihr.ac.uk/priority-setting-partnerships/anaesthesia-canada/top-10-priorities.htm (accessed September 2020).
- 20.Statistics Canada. Canadian Community Health Survey – Annual Component. Canadian Community Health Survey: Ottawa, ON; 2010. Available from URL: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=81424 (accessed September 2020).
- 21.Statistics Canada. Mitigation of risk to respondents of Statistics Canada’s surveys – June 2010; Retrieved from URL: https://www.statcan.gc.ca/eng/rdc/mitigation (accessed September 2020).
- 22.Statistics Canada. Frequently asked questions. 2019. Available from URL: https://www.statcan.gc.ca/eng/rdc/faq#a11a (accessed September 2020).
- 23.IBM Corp. IBM SPSS Statistics for Windows, Version 24.0 2016; Armonk, NY: IBM Corp.
- 24.StataCorp. Stata Statistical Software: Release 14 2015; College Station, TX: StataCorp LP.
- 25.Tait AR, Voepel-Lewis T, Munro HM, Gutstein HB, Reynolds PI. Cancellation of pediatric outpatient surgery: economic and emotional implications for patients and their families. J Clin Anesth. 1997;9:213–219. doi: 10.1016/S0952-8180(97)00032-9. [DOI] [PubMed] [Google Scholar]
- 26.Leslie RJ, Beiko D, van Vlymen J, Siemans DR. Day of surgery cancellation rates in urology: identification of modifiable factors. Can Urol Assoc J. 2013;7:167–173. doi: 10.5489/cuaj.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herrod PJ, Adiamah A, Boyd-Carson H, et al. Winter cancellations of elective surgical procedures in the UK: a questionnaire survey of patients on the economic and psychological impact. BMJ Open. 2019 doi: 10.1136/bmjopen-2018-028753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rasouli MR, Menendez ME, Sayadipour A, Purtill JJ, Parvizi J. Direct cost and complications associated with total joint arthroplasty in patients with preoperative anxiety and depression. J Arthroplasty. 2016;31:533–536. doi: 10.1016/j.arth.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 29.Rodrigues HF, Furuya RK, Dantas RA, et al. Association of preoperative anxiety and depression symptoms with postoperative complications of cardiac surgeries (Portuguese) Rev Lat Am Enfermagem. 2018 doi: 10.1590/1518-8345.2784.3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mier N, Helm M, Kastenmeier AS, Gould JC, Goldblatt MI. Preoperative pain in patient with an inguinal hernia predicts long-term quality of life. Surgery. 2018;163:578–581. doi: 10.1016/j.surg.2017.09.055. [DOI] [PubMed] [Google Scholar]
- 31.Gerain P, Zech E. Informal caregiver burnout? Development of a theoretical framework to understand the impact of caregiving. Front Psychol. 2019 doi: 10.3389/fpsyg.2019.01748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hunter DJ, Riordan EA. The impact of arthritis on pain and quality of life: An Australian survey. Int J Rheum Dis. 2014;17:149–155. doi: 10.1111/1756-185X.12232. [DOI] [PubMed] [Google Scholar]
- 33.Blyth FM, Noguchi N. Chronic musculoskeletal pain and its impact on older people. Best Pract Res Clin Rheumatol. 2017;31:160–168. doi: 10.1016/j.berh.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 34.Ruiz ME. Risks of self-medication practices. Curr Drug Saf. 2010;5:315–323. doi: 10.2174/157488610792245966. [DOI] [PubMed] [Google Scholar]
- 35.Dexter F, Maxbauer T, Stout C, Archbold L, Epstein RH. Relative influence on total cancelled operating room time from patients who are inpatients or outpatients preoperatively. Anesth Analg. 2014;118:1072–1080. doi: 10.1213/ANE.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 36.Pohlman GD, Staulcup SJ, Masterson RM, Vemulakonda VM. Contributing factors for cancellations of outpatient pediatric urology procedures: single centre experience. J Urol. 2012;188(4 Suppl):1634–1638. doi: 10.1016/j.juro.2012.03.111. [DOI] [PubMed] [Google Scholar]
- 37.Al Talalwah N, McIltrot KH. Cancellation of surgeries: integrative review. J Perianesth Nurs. 2019;34:86–96. doi: 10.1016/j.jopan.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 38.Leite KA, Hobgood T, Hill B, Muckler VC. Reducing preventable surgical cancellations: Improving the preoperative anesthesia interview process. J Perianesth Nurs. 2019;34:929–937. doi: 10.1016/j.jopan.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 39.Dawson VJ, Margo J, Blanco N, Munir WM. Reducing cancellations and optimizing surgical scheduling of ophthalmology cases at a veterans affairs medical center. J Healthc Qual. 2019;41:83–90. doi: 10.1097/JHQ.0000000000000187. [DOI] [PubMed] [Google Scholar]
- 40.Lee CM, Rodgers C, Oh AK, Muckler VC. Reducing surgery cancellations at a pediatric ambulatory surgery center. AORN J. 2017;105:384–391. doi: 10.1016/j.aorn.2017.01.011. [DOI] [PubMed] [Google Scholar]


