Abstract
Background
Few data are available on the characteristics of inpatient treatment and subsequent outpatient treatment for depression in Germany. In this study, we aimed to characterize the inpatient and outpatient treatment phases, to determine the rates of readmission and mortality, and to identify risk factors.
Methods
We carried out a descriptive statistical analysis of routine administrative data from a large health-insurance carrier (BARMER). All insurees aged 18 to 65 who were treated in 2015 as inpatients on a psychiatry and psychotherapy service or on a psychosomatic medicine and psychotherapy service with a main diagnosis of depression were included in the analysis. Risk factors for readmission and death were determined with the aid of mixed logistic regression.
Results
Of the 22 893 patients whose data were analyzed, 78% had been hospitalized on a psychiatry and psychotherapy service and 22% on a psychosomatic medicine and psychotherapy service. The median length of hospital stay was 42 days. Follow-up care in the outpatient setting failed to conform with the recommendations of the pertinent guidelines in 92% of the patients with a main diagnosis of severe depression during hospitalization, and in 50% of those with moderate depression. 21% of the patients were readmitted within a year. The mortality at one year was 961 per 100 000 individuals (adjusted for the age and sex structure of the German population), or 3.4 times the mortality of the population at large. In the regression model, more treatment units during hospitalization and subsequent treatment with psychotherapy were associated with a lower probability of readmission, while longer hospitalization with subsequent pharmacotherapy or psychotherapy was associated with lower mortality.
Conclusion
The recommendations of the national (German) S3 guidelines for the further care of patients who have been hospitalized for depression are inadequately implemented at present in the sectored structures of in- and outpatient care in the German health care system. This patient group has marked excess mortality.
Depression is one of the most common and most debilitating illnesses worldwide (1). It causes significant individual suffering (2) and is associated with increased mortality, due to suicide and comorbidities (3). In Germany, about three per cent of patients with depression are currently treated on an inpatient basis (4). After discharge from hospital, the risks of suicide (5, 6), recurrence and—if the patient does not achieve remission—chronification are increased (7, 8). To achieve complete remission or to prevent a chronic or recurrent course of the illness as well as suicide, the German National Disease Management Guideline (“S3 guideline”) recommends adequate follow-up care in the form of remission-stabilizing maintenance therapy. In patients with severe depression, treatment should consist of a combination of pharmacotherapy and psychotherapy. In patients with moderate depression, pharmacological or psychotherapeutic treatment alone, depending on the patient’s preference, is sufficient (9). These guideline recommendations are supported by the highest level of evidence (grade of recommendation “A”), i.e. they are based on multiple randomized controlled trials. Analyzes of routine health insurance data as well as surveys assessing the outpatient care of patients with depression found evidence of care deficits (4, 10– 13). Data on the characteristics of inpatient treatment of depression in Germany and the current state of follow-up outpatient treatment are scarce, making it difficult to assess the required health policy measures in the context of the current health policy debates about mental health care. Therefore, our study addresses—based on the routine data set of BARMER, a large German health insurer, covering more than 9 million persons in Germany—the following questions:
How and for how long are patients with a depressive episode treated in a hospital/department of psychiatry and psychotherapy or a hospital/department of psychosomatic medicine and psychotherapy?
Is the follow-up outpatient treatment guideline-adherent?
What are the annual readmission and mortality rates and
by which sociodemographic, illness-related or treatment-related variables are they influenced?
Methods
From the about 9.4 million persons insured with BARMER in 2015, those were selected who were between 18 and 65 years of age and discharged from psychiatric-psychotherapeutic or psychosomatic-psychotherapeutic inpatient treatment with an ICD-10 diagnosis of F32.x (major depressive disorder, single episode) or F33.x (major depressive disorder, recurrent). If the patient was discharged in 2015, the inpatient stay was regarded as an index stay. Subsequent to discharge, a 365-day observation interval was defined during which guideline-adherent follow-up treatment with medication and psychotherapy as well as readmission and mortality rates were assessed (short version, see eMethods).
Results
Characteristics of the index population
22 893 of the approximately 9.4 million persons insured with BARMER (equaling a one-year prevalence of an inpatient stay of 0.25%) fulfilled the inclusion criteria (= index population). 66% (n = 15 059) were females. The age median was 47 years (range 47). 39% (n = 8991) of the index population were registered in a city (>100 000 inhabitants).
Characteristics of the index hospital treatment
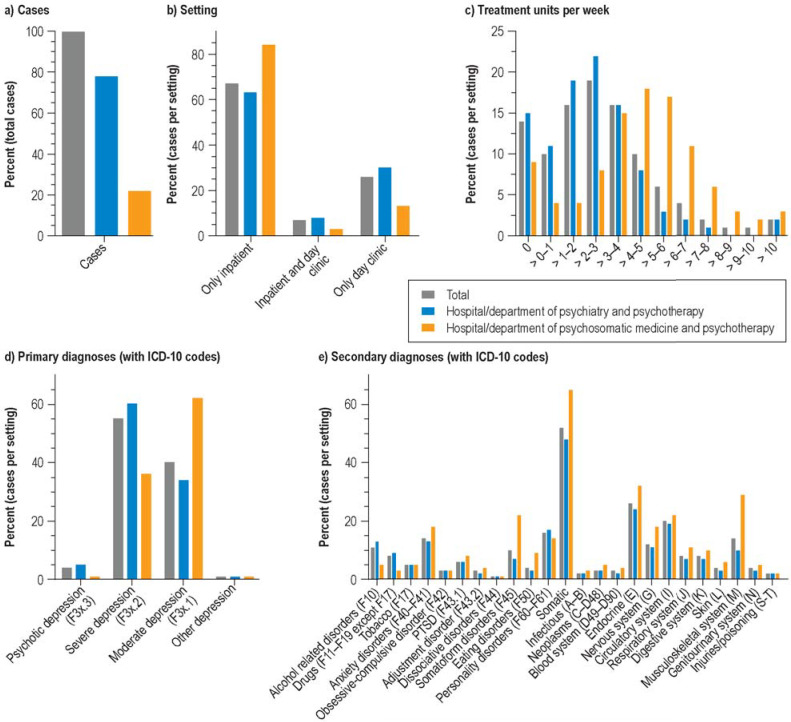
The median length of inpatient stay was 42 days (minimum 1, maximum 816). At discharge from the index stay, 78% (n = 17 799) of the index population were treated in a hospital/department of psychiatry and psychotherapy and 22% (n = 5094) in a hospital/department of psychosomatic medicine and psychotherapy. Figure 1 and eTable 1 provide an overview of the distribution of cases (Figure 1a). What was striking was the small proportion of day-clinic treatment, especially in psychosomatic medicine (Figure 1b), and a significantly higher treatment density by physicians/psychologists in hospitals/departments of psychosomatic medicine and psychotherapy compared to hospitals/departments of psychiatry and psychotherapy, (Figure 1c), where, however, the vast majority of patients with severe or psychotic depression were treated (Figure 1d). With regard to secondary diagnoses, there were no major differences between the two types of hospitals/departments (Figure 1a).
Figure 1.
Characteristics of inpatient index treatment. PTSD, posttraumatic stress disorder
eTable 1. Characteristics of inpatient index treatment (data for Figure 1).
| eTable 1b – Length of hospital stay and treatment setting of index treatment | |||||||||
| Total | Psychiatry | Psychosomatic medicine | |||||||
|
LOS* Median |
N | % |
LOS* Median |
N | % |
LOS* Median |
N | % | |
| Total | 42 | 22 893 | 100 | 42 | 17 799 | 100 | 43 | 5 094 | 100 |
| Only inpatient | 38 | 15 418 | 67 | 34 | 11 143 | 63 | 42 | 4 275 | 84 |
| Only day clinic | 51 | 5967 | 26 | 51 | 5289 | 30 | 52 | 682 | 13 |
| Inpatient + day clinic combined | 80 | 1508 | 7 | 82 | 1 371 | 8 | 70 | 137 | 3 |
| of these inpatient | 44 | ||||||||
| of these day clinic | 30 | ||||||||
| eTable 1c – Treatment units of index treatment | |||||||||
| Total | Psychiatry | Psychosomatic medicine | |||||||
| Median | N | % | Median | N | % | Median | N | % | |
| 0 | 3.5 | 3135 | 14 | 2.4 | 2669 | 15 | 4.9 | 466 | 9 |
| > 0–1 | 2215 | 10 | 2021 | 11 | 194 | 4 | |||
| > 1–2 | 3574 | 16 | 3347 | 19 | 227 | 4 | |||
| > 2–3 | 4352 | 19 | 3954 | 22 | 398 | 8 | |||
| > 3–4 | 3649 | 16 | 2902 | 16 | 747 | 15 | |||
| > 4–5 | 2316 | 10 | 1380 | 8 | 936 | 18 | |||
| > 5–6 | 1437 | 6 | 576 | 3 | 861 | 17 | |||
| >6–7 | 909 | 4 | 341 | 2 | 568 | 11 | |||
| > 7–8 | 419 | 2 | 109 | 1 | 310 | 6 | |||
| > 8–9 | 224 | 1 | 59 | 0 | 165 | 3 | |||
| > 9–10 | 140 | 1 | 60 | 0 | 80 | 2 | |||
| > 10 | 523 | 2 | 381 | 2 | 142 | 3 | |||
| eTable 1d – Primary diagnoses of index treatment | |||||||||
| Total | Psychiatry | Psychosomatic medicine | |||||||
| N | % | N | % | N | % | ||||
| F3x.3 – Psychotic depression | 877 | 4 | 841 | 5 | <50 | 1 | |||
| F32.3 | 358 | 2 | 344 | 2 | <50 | <1 | |||
| F33.3 | 519 | 2 | 497 | 3 | <50 | <1 | |||
| F3x.2 – Severe depression | 12 550 | 55 | 10 714 | 60 | 1 836 | 36 | |||
| F32.2 | 5201 | 23 | 4599 | 26 | 602 | 12 | |||
| F33.2 | 7349 | 32 | 6115 | 34 | 1 234 | 24 | |||
| F3x.1 – Moderate depression | 9270 | 40 | 6093 | 34 | 3 177 | 62 | |||
| F32.1 | 4018 | 18 | 2840 | 16 | 1 178 | 23 | |||
| F33.1 | 5252 | 23 | 3253 | 18 | 1 999 | 39 | |||
| Remainder | 196 | 1 | 151 | 1 | <50 | 1 | |||
| eTable 1e – Secondary diagnoses of index treatment | |||||||||
| Total | Psychiatry | Psychosomatic medicine | |||||||
| N | % | N | % | N | % | ||||
| Alcohol related disorders (F10) | 2473 | 11 | 2234 | 13 | 239 | 5 | |||
| Drugs (F11–F19)** | 1754 | 8 | 1581 | 9 | 173 | 3 | |||
| Tobacco (F17) | 1188 | 5 | 912 | 5 | 276 | 5 | |||
| Anxiety disorders (F40–F41) | 3276 | 14 | 2342 | 13 | 934 | 18 | |||
| Obsessive-compulsive disorder (F42) | 598 | 3 | 449 | 3 | 149 | 3 | |||
| PTSD (F43.1) | 1472 | 6 | 1072 | 6 | 400 | 8 | |||
| Adjustment disorder (F43.2) | 647 | 3 | 441 | 2 | 206 | 4 | |||
| Dissociative disorders (F44) | 266 | 1 | 196 | 1 | 70 | 1 | |||
| Somatoform disorders (F45) | 2368 | 10 | 1225 | 7 | 1143 | 22 | |||
| Eating disorders (F50) | 968 | 4 | 494 | 3 | 474 | 9 | |||
| Personality disorders (F60–F61) | 3750 | 16 | 3053 | 17 | 697 | 14 | |||
| Somatic | 11 924 | 52 | 8596 | 48 | 3328 | 65 | |||
| Infectious (A–B) | 542 | 2 | 401 | 2 | 141 | 3 | |||
| Neoplasms (C–D48) | 779 | 3 | 546 | 3 | 233 | 5 | |||
| Blood system (D49–D90) | 586 | 3 | 402 | 2 | 184 | 4 | |||
| Endocrine (E) | 5853 | 26 | 4217 | 24 | 1636 | 32 | |||
| Nervous system (G) | 2820 | 12 | 1925 | 11 | 895 | 18 | |||
| Circulatory system (I) | 4501 | 20 | 3388 | 19 | 1113 | 22 | |||
| Respiratory system (J) | 1874 | 8 | 1319 | 7 | 555 | 11 | |||
| Digestive system (K) | 1786 | 8 | 1297 | 7 | 489 | 10 | |||
| Skin (L) | 921 | 4 | 616 | 3 | 305 | 6 | |||
| Musculoskeletal system (M) | 3305 | 14 | 1834 | 10 | 1471 | 29 | |||
| Genitourinary system (N) | 833 | 4 | 598 | 3 | 235 | 5 | |||
| Injuries/poisoning (S–T) | 512 | 2 | 393 | 2 | 119 | 2 | |||
| eTable 1f – Comorbidity indices according to the Royal College of Surgeons Charlson Score (RCS) | |||||||||
| Total | Psychiatry | Psychosomatic medicine | |||||||
| Mean | SD | Mean | SD | Mean | SD | ||||
| RCS Charlson score | 0.157 | 0.449 | 0.157 | 0.455 | 0.159 | 0.430 | |||
**except F17 – Tobacco*LOS, length of stay
Severity-adapted guideline-adherent follow-up treatment
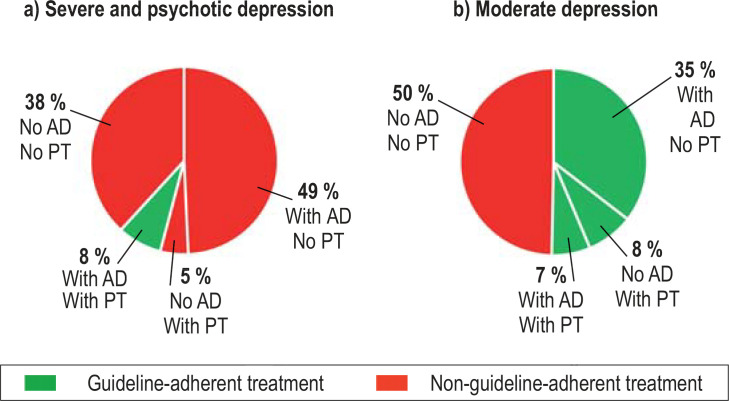
With regard to the severity-adapted guideline recommendations, 92% (n = 12 395) of the patients with severe depression did not receive guideline-adherent follow-up treatment with a combination of pharmacotherapy and psychotherapy (Figure 2a). Of the patients with moderate depression, 50% (n = 4605) did not receive guideline-adherent follow-up treatment with either medication or psychotherapy (Figure 2b).
Figure 2.
Guideline-adherent follow-up treatment
AD, antidepressant; PT, psychotherapy
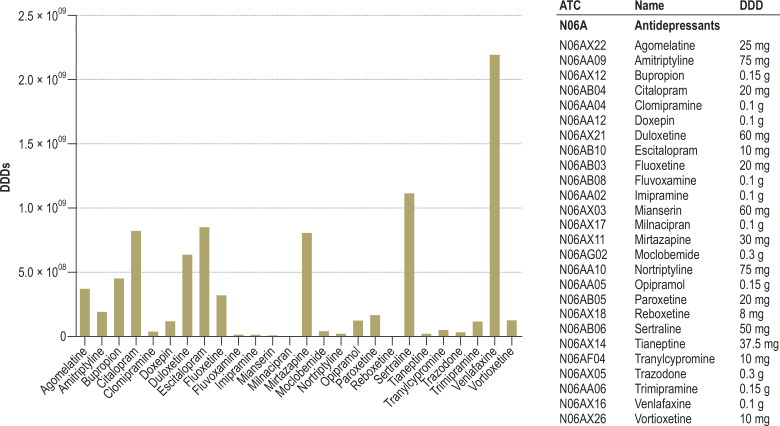
The analysis of outpatient pharmacotherapy found that 84% of the 13 427 patients with severe depression (F3X.2 or F3X.3) and 70% of the 9270 patients with moderate depression (F3X.1), filled at least one antidepressant prescription during the follow-up year. However, only 57% (n = 7651) and 42% (n = 3908) of the patients with moderate depression and severe depression, respectively, were given a prescription—as recommended in the guideline—during the first quarter after discharge and, where appropriate, follow-up prescriptions with defined daily doses (DDDs) sufficient for a period of at least four months For an overview of the DDDs of the prescribed substances see the eFigure.
eFigure.
Prescribed defined daily doses (DDDs) of the various antidepressants
For the outpatient follow-up treatment, it was found that only 33% (n = 4428) and 37% (n = 3474) of the patients with severe and moderate depression, respectively, received one hour of psychotherapy within the one-year observation interval at all. Only 12% (n = 1676) and 15% (n = 1376) of patients with severe and moderate depression, respectively, received the first hour of psychotherapy within the first quarter after discharge and at least eight hours of psychotherapy during the one-year observation interval, as recommended in the guideline.
The interval between discharge from hospital and the first hour of psychotherapy was assessed in the 4311 patients who had not received psychotherapy in the year prior to hospital admission. Among these patients, the median interval between discharge and start of psychotherapy was 111 days (95% confidence interval: [106; 115]). Psychotherapy was primarily individual therapy with cognitive behavioral therapy (55%) or psychodynamic psychotherapy (43%), whereas psychoanalysis and group therapy played only a marginal role (table 1).
Table 1. Outpatient psychotherapy in the observation interval.
| Cases* | Service items | |||
| N | % | N | % | |
| Total | 7951 | 100 | 218 254 | 100 |
| CBT individual | 4335 | 55 | 103 084 | 47 |
| CBT group | 108 | 1 | 2014 | 1 |
| PP individual | 3403 | 43 | 89 380 | 41 |
| PP group | 174 | 2 | 4866 | 2 |
| AP individual | 273 | 3 | 17 416 | 8 |
| AP group | <50 | <1 | 1494 | 1 |
*In one index patient, several types of psychotherapy may have been billed during the observation interval, resulting in a total >100% AP, analytical psychotherapy; PP, psychodynamic psychotherapy; CBT, cognitive behavioral therapy
eTable 3 shows whether a specialist or general practitioner/internist was consulted during the first quarter of treatment in the observation interval.
eTable 3. Follow-up treatment by specialist*1 or general practitioner/internist*2.
| eTable 3a – In the entire index year at least one service provided by specialist or general practitioner | |||||||
| Specialist *1 | General practitioner *2 | ||||||
| n | % | n | % | ||||
| Number n and % of index population | 12 672 | 55 | 4276 | 19 | |||
| eTable 3b – In the first quarter after discharge at least one service provided by specialist or general practitioner | |||||||
| Specialist *1 | General practitioner *2 | ||||||
| n | % | n | % | ||||
| Number n and % of index population | 9659 | 42 | 2235 | 10 | |||
| eTable 3c – Medication and psychotherapy if in the first quarter after discharge at least one service was provided by specialist or general practitioner | |||||||
| Inpatient primary diagnosis | Treatment | Total | Specialist *1 | General practitioner *2 | |||
| n | % | n | % | n | % | ||
| Severe depression | Total | 13 427 | 100 | 5879 | 100 | 1302 | 100 |
| AD | 6619 | 49 | 3197 | 54 | 587 | 45 | |
| PT | 644 | 5 | 316 | 5 | 88 | 7 | |
| AD + PT | 1032 | 8 | 680 | 12 | 81 | 6 | |
| (–) | 5132 | 38 | 1686 | 29 | 546 | 42 | |
| Moderate depression | Total | 9270 | 100 | 3780 | 100 | 933 | 100 |
| AD | 3289 | 35 | 1585 | 42 | 284 | 30 | |
| PT | 757 | 8 | 363 | 10 | 89 | 10 | |
| AD + PT | 619 | 7 | 389 | 10 | <50 | 5 | |
| (–) | 4605 | 50 | 1443 | 38 | 511 | 55 | |
*1 Specialist: Neurology and psychiatry, psychiatry and psychotherapy, psychosomatic medicine and psychotherapy;
*2 General practitioner: General practice, physician/medical practitioner internist, pediatrician (family physician)
Cases in the specialist category may also have received additional services from their general practitioner.
Included in the general practitioner category are only those cases which have not received additional specialist services
AD, antidepressant; AD + PT, antidepressant + psychotherapy; PT, psychotherapy; (–), neither antidepressant nor psychotherapy green: guideline-adherent treatment
red: non-guideline-adherent treatment
Readmissions
During the observation interval, 21% (n = 4798) of the index population were readmitted to inpatient or day-patient psychiatric-psychotherapeutic or psychosomatic treatment, 5% (n = 1103) twice or more. To evaluate whether guideline-adherent follow-up treatment helps to prevent readmission, we looked for evidence of risk factors of readmission in the second half of the year after discharge, using a multi-level regression model. In the random intercept null model, hospital and region explained a substantial proportion of the variation with regard to readmission. In the three-level regression model, older age was a sociodemographic factor that increased the likelihood of readmission. With regard to disease-related factors, the primary diagnosis of severe depression and the secondary diagnoses of personality disorder, posttraumatic stress disorder, obsessive-compulsive disorder, addiction or alcohol-related disorders significantly increased the likelihood of readmission in the model. With regard to treatment-related factors, the likelihood of readmission increased with treatment in a hospital/department of psychiatry and psychotherapy as well as with guideline-adherent follow-up treatment with antidepressants. In contrast, more treatment units during index treatment and guideline-adherent psychotherapeutic follow-up treatment decreased the likelihood of readmission. McFadden’s Pseudo R2 was 0.03; the predictors thus explained a moderate proportion of the variation beyond the hospital-related and regional variation (14) (table 2).
Table 2. 3-level regression model readmission in the second half of the year after discharge.
| Variable | Covariance parameter estimate | Standard error | ||
| Random intercepts of the null model | ||||
| Hospital | 0.09 | 0.02 | ||
| Region (post code 2 digits) | 0.02 | 0.01 | ||
| Random intercepts of the predictor model | ||||
| Hospital | 0.04 | 0.02 | ||
| Region (post code 2 digits) | 0.02 | 0.01 | ||
| Variable | Odds ratio*1 | F value | p | |
| Fixed effects of the predictor model | ||||
| Sociodemographic factors | ||||
| – Age (per year) | 1.00 | [1.00; 1.01] | 14.42 | 0.0001 |
| – Male sex | 0.95 | [0.85; 1.05] | 1.18 | 0.2769 |
| Illness-related factors | ||||
| – Secondary diagnosis personality disorder (F60–F61) | 1.70 | [1.51; 1.90] | 82.11 | <0.0001 |
| – Secondary diagnosis posttraumatic stress disorder (F43.1) | 1.53 | [1.30; 1.81] | 25.81 | <0.0001 |
| – Primary diagnosis severe depression (F3x.2–F3x.3) | 1.50 | [1.35; 1.66] | 55.26 | <0.0001 |
| – Secondary diagnosis obsessive-compulsive disorder (F42) | 1.32 | [1.01; 1.72] | 4.18 | 0.0408 |
| – Secondary diagnosis drugs (F11–F19 except F17) | 1.28 | [1.09; 1.51] | 9.19 | 0.0024 |
| – Secondary diagnosis alcohol-related disorders (F10) | 1.21 | [1.05; 1.39] | 6.75 | 0.0094 |
| – Secondary diagnosis dissociative disorder (F44) | 1.13 | [0.77; 1.65] | 0.37 | 0.5456 |
| – Secondary diagnosis somatoform disorders (F45) | 1.09 | [0.93; 1.28] | 1.16 | 0.2816 |
| – Charlson index (somatic comorbidities) | 1.09 | [0.99; 1.20] | 2.82 | 0.0931 |
| – Secondary diagnosis tobacco (F17) | 1.07 | [0.87; 1.31] | 0.43 | 0.5097 |
| – Secondary diagnosis anxiety disorders (F40–F41) | 0.99 | [0.87; 1.14] | 0.01 | 0.9042 |
| – Secondary diagnosis eating disorders (F50) | 0.92 | [0.72; 1.18] | 0.39 | 0.5322 |
| – Secondary diagnosis adjustment disorders (F43.2) | 0.75 | [0.53; 1.05] | 2.78 | 0.0953 |
| Treatment-related factors | ||||
| – Guideline-adherent follow-up treatment with antidepressants | 1.49 | [1.35; 1.64] | 63.13 | <0.0001 |
| – Treatment in hospital/department of psychiatry*2 | 1.30 | [1.12; 1.51] | 11.97 | 0.0005 |
| – Length of stay (per day) | 1.00 | [1.00; 1.00] | 0.19 | 0.6603 |
| – Treatment units (per 25 min TU per week) | 0.96 | [0.95; 0.98] | 14.94 | 0.0001 |
| – Guideline-adherent follow-up treatment with psychotherapy | 0.78 | [0.67; 0.90] | 10.67 | 0.0011 |
*1 95% confidence intervals*2 As opposed to hospital/department of psychosomatic medicine TU, treatment unit
Mortality
Within the observation period, 1.1% (n = 256) of the index population died. The result was adjusted with regard to age and sex to the German general population aged 18 to 65 years (15). With 961/100 000 population, the one-year mortality was 3.4-times higher compared to the age- and sex-matched general population (282/100 00). The cause for mortality is not recorded in the available data. In the random intercept null model, “hospital“, but not “region”, explained variation in mortality. In the 3-level regression model, with regard to fixed effects, age and male sex as sociodemographic risk factors, a primary diagnosis of severe depression as well as psychiatric secondary diagnoses and severe somatic comorbidities (represented by the Charlson index) as illness-related factors, and treatment in a hospital/department of psychiatry and psychotherapy as treatment-related factors were associated with an increased likelihood of mortality. By contrast, prolonged length of inpatient stay and (at least minimal) antidepressant and psychotherapeutic follow-up treatment decreased the likelihood of mortality. McFadden’s Pseudo R2 was 0.16; the predictors thus explained a significant proportion of the variation beyond the hospital-related and regional variation (14) (Table 3a, b).
Table 3a. 3-level regression model—random intercepts of the null model and predictor model.
| Variable | Covariance parameter estimate | Standard error |
| Random intercepts of the null model | ||
| Hospital | 0.38 | 0.11 |
| Region (post code 2 digits) | 0 | – |
| Random intercepts of the predictor model | ||
| Hospital | 0.25 | 0.11 |
| Region (post code 2 digits) | 0 | 0 |
Table 3 b. 3-level regression model mortality—<sociodemographic, illness- and treatment-related factors.
| Variable | Odds ratio*1 | F value | p | |
| Fixed effects of the predictor model | ||||
| Sociodemographic factors | ||||
| – Male sex | 1.8 | [1.39; 2.34] | 19.24 | <0.0001 |
| – Age (per year) | 1.05 | [1.04; 1.07]) | 66.21 | <0.0001 |
| Illness-related factors | ||||
| – Charlson index (somatic comorbidities) | 1.77 | [1.52; 2.06] | 53.21 | <0.0001 |
| – Primary diagnosis severe depression (F3x.2–F3x.3) | 1.71 | [1.26; 2.32] | 11.78 | 0.0006 |
| – Secondary diagnosis drugs (F11–F19 except F17) | 1.70 | [1.15; 2.50] | 7.21 | 0.0073 |
| – Secondary diagnosis obsessive-compulsive disorder (F42) | 1.57 | [0.68; 3.63] | 1.12 | 0.2905 |
| – Secondary diagnosis alcohol related disorders (F10) | 1.51 | [1.11; 2.05] | 7.01 | 0.0081 |
| – Secondary diagnosis adjustment disorders (F43.2) | 1.25 | [0.60; 2.62] | 0.35 | 0.5542 |
| – Secondary diagnosis somatoform disorders (F45) | 1.20 | [0.75; 1.93] | 0.59 | 0.4405 |
| – Secondary diagnosis personality disorder (F60–F61) | 1.05 | [0.71; 1.54] | 0.05 | 0.8169 |
| – Secondary diagnosis posttraumatic stress disorder (F43.1) | 0.95 | [0.50; 1.78] | 0.03 | 0.8664 |
| – Secondary diagnosis anxiety disorders (F40–F41) | 0.79 | [0.50; 1.25] | 1.06 | 0.3037 |
| – Secondary diagnosis tobacco (F17) | 0.76 | [0.44; 1.30] | 1.00 | 0.3165 |
| – Secondary diagnosis eating disorders (F50) | 0.66 | [0.21; 2.11] | 0.49 | 0.4837 |
| – Secondary diagnosis dissociative disorder (F44) | 0.44 | [0.06; 3.26] | 0.64 | 0.4250 |
| Treatment-related factors | ||||
| – Treatment in hospital/department of psychiatry*2 | 2.69 | [1.52; 4.75] | 11.58 | 0.0007 |
| – Treatment units (TU) (per 25 min TU per week) | 1.00 | [0.96; 1.03] | 0.08 | 0.7772 |
| – Length of stay (per day) | 0.99 | [0.98; 0.99] | 23.34 | <0.0001 |
| – Minimal antidepressant follow-up treatment | 0.53 | [0.40; 0.71] | 18.61 | <0.0001 |
| – Minimal psychotherapy follow-up treatment | 0.29 | [0.18; 0.45] | 29.87 | <0.0001 |
*1 95% confidence intervals
*2 As opposed to hospital/department of psychosomatic medicine
To obtain evidence of preventative effects of guideline-adherent treatment, we initially planned to repeat the regression analysis using the more extensive indicators “guideline-adherent medication“ and “guideline-adherent psychotherapy“ for the deaths that occurred during the second half of the year after discharge; however, none of the patients who died during the second half of the year received guideline-adherent treatment during the first half of the year.
Discussion
Inpatient treatment
The routine data of BARMER show that in Germany inpatient treatment of depression was provided by hospitals/departments of psychiatry and psychotherapy in three of four patients. In 2015, the number of beds was 50 972 in psychiatry (without addiction) to 10 439 in psychosomatic medicine (16). The hospitals/departments of psychiatry and psychotherapy primarily treated patients with severe and psychotic depression, while the hospitals/departments of psychosomatic medicine primarily treated patients with moderate depression. However, treatment density was considerably lower in hospitals/departments of psychiatry and psychotherapy compared to hospitals/departments of psychosomatic medicine. This is due to the requirements of the approximately 30-year-old German Psychiatry Personnel Regulation Act (PsychPV, Psychiatrie-Personalverordnung) which limits the possibilities to provide intensive and guideline-adherent psychotherapy (17, 18). Since staffing in hospitals/departments of psychosomatic medicine is usually not regulated by the PsychPV, in this setting one full-time physician/psychologist is only responsible for the treatment of half as many patients compared to hospitals/departments of psychiatry (19, 20). With 42 days, the length of stay was overall shorter compared to, for example, the situation 15 years ago (21). In the light of the goal to promote the integration of patients into their living environment and the comparable low costs of this care strategy, it is surprising that treatment in day clinics, especially in hospitals/departments of psychosomatic medicine, is the exception, not the rule.
Follow-up outpatient treatment
After discharge, only 8% of patients with severe depression and 50% of patients with moderate depression received guideline-adherent follow-up treatment. In the group of patients with severe depression, only 12% received the follow-up treatment with psychotherapy recommended in the guidelines. The study data did not allow to determine the exact reasons behind this finding. The important role of structural deficits in the German healthcare system, causing this long interval of 16.7 weeks until the start of treatment, is highlighted by the information of the Federal Chamber of Psychotherapists (BPtK, Bundespsychotherapeutenkammer) that nationwide the mean waiting time for a space in psychotherapy is 19.9 weeks, with a high patient preference for this treatment modality (22). These long intervals are of concern because data from the British healthcare system show that with waiting times of more than four weeks the chance of a positive effect of outpatient psychotherapy decreases considerably (23). Structural support could be provided by improved coordination between hospitals, specialists in psychiatry and psychotherapy/general practitioners and guideline psychotherapists (24– 26). Furthermore, although group therapy could expand the psychotherapy offering to compensate for the lack of resources, this rarely happens in Germany, according to chambers of psychotherapists because of bureaucratic hurdles (27).
With regard to follow-up treatment with medication, again significant deficits were identified. Only 57% of patients with severe or psychotic illness received medication for an adequate period of time and in adequate doses—and the indicator chosen for this study represents a very conservative estimate. The available data did not allow conclusions about to what extent this was due to patient concerns about long-term medication use or physicians not adhering to the guideline recommendations.
Readmissions
The association of comorbidities and advanced age with less favorable courses is consistent with the findings reported in the literature (28). The finding that patients treated in a hospital/department of psychiatry and psychotherapy are at a higher risk of readmission can be explained by differences in the patient mix and the more acute treatment setting. The association between inpatient treatment intensity and readmission rates identified in the regression model raises the question of the adequacy of staffing in hospitals/departments of psychiatry and psychotherapy. After discharge, patients receiving follow-up treatment with psychotherapy have a lower risk of readmission in the model, indicating the importance of implementing this guideline recommendation. The finding that guideline-adherent follow-up treatment with medication is associated with an increased likelihood of readmission in the model seems counterintuitive, but may be explained by the fact that the indication for consistent treatment with medication is stricter in patients with more severe illness who consequently are at a greater risk of relapse and recurrence. Alternatively, the finding could be explained by the rebound phenomenon which is triggered by improper discontinuation of antidepressant treatment and has only recently been reported in the literature (29).
Mortality
Deaths are a key outcome measure of high clinical relevance which is available in the routine data. This study found a mortality rate which was higher than expected. In the year following discharge from hospital after inpatient treatment of depression, the mortality rate was 3.4 times higher compared to the general population. Instead of the expected 65 deaths among 22 893 persons in the general population, 151 more persons died in the (adjusted) index sample of this study. It can be assumed that mortality was reliably recorded in the available dataset. While factors such older age, male sex, severity of depression, combined addictions, the Charlson index, and treatment in a hospital/department of psychiatry and psychotherapy can be used to identify high-risk populations, treatment-related factors highlight the risk of increased mortality associated with a lack of follow-up treatment with psychotherapy and medication as well as shorter inpatient stays. Of particular concern was the finding that none of the patients who died in the second half of the year after discharge had received guideline-adherent treatment in the first six months.
Limitations
By analyzing administrative health insurance data, large populations and the reality of treatment can be explored over time outside of studies. A disadvantage of routine data is the limited validity of the diagnoses, especially of the severity grading used in this study. Since this study focused on patients who were treated in a specialist hospital or department, a higher validity at least of mental health diagnoses can be assumed; on the other hand, this focus also allowed to capture the reality of outpatient treatment of some of the most severely affected patients. By combining inpatient stays, this study provides a more realistic view on readmissions and the length of hospital stays than previous studies. Since health insurance providers are not allowed to have access to further clinical variables, indicators have to be used to make these accessible. Thus, treatment reality may differ in individual cases. Furthermore, analyzes of routine data can only describe the existing care situation. The regressions performed on the administrative data can only indicate plausible relationships, but do not allow for causal interpretations. In addition, the relationships identified in the regression models are only valid, even on the basis of correlative interpretation, if no unconsidered confounders with substantial effects on the studied outcomes are present. Due to the relatively low number of events compared to the complexity of the statistical models, some results may show bias. Furthermore, it should be taken into account that “guideline adherence” could only be operationalized very broadly in this study, because guidelines, although making general recommendations, explicitly allow to deviate from these recommendations and to take into account factors when making individualized decisions that extend beyond illness severity.
Conclusion
Despite its methodological limitations, which need to be considered, our study reveals potential shortcomings in the care of patients undergoing inpatient treatment. Inpatient treatment in specialist hospitals and departments of psychiatry and psychotherapy was characterized by lower treatment intensity compared to specialist hospitals and departments of psychosomatic medicine and psychotherapy, despite the higher proportion of patients with severe depression and the fact that in the model, intensification of inpatient treatment could counteract readmissions. In addition, longer inpatient stays were associated with reduced mortality risk in the model. Furthermore, our study shows deficits of the follow-up treatment with medication and psychotherapy. Only in a minority of patients, the current guideline recommendations were implemented, despite the fact that in regression models the recommended follow-up treatment could reduce the likelihood of readmissions and death. These results underscore the high relevance of current efforts in research, professional and health policy to improve healthcare structures in a way that enables guideline-adherent treatment in an inpatient care setting independent of the type of hospital/department and in outpatient care within the currently existing sectored structures.
Supplementary Material
eMethods
Index population and index hospital treatment
Via a secured VPN tunnel, the authors (H.F.W., J.S., U.M.) had access to the BARMER Data Warehouse. From the about 9.4 million persons insured with BARMER in 2015, those were selected who were between 18 and 65 years of age in 2015 and discharged from psychiatric-psychotherapeutic or psychosomatic-psychotherapeutic inpatient treatment with an ICD-10 diagnosis of F32.x (major depressive disorder, single episode) or F33.x (major depressive disorder, recurrent). It is common that patients undergoing prolonged inpatient treatment are occasionally discharged for a short period of time (for example, in case of a long weekend due to a public holiday, transitions between treatment settings or as a discharge on a trial basis to test prolonged exposure to stress). Since these events would confound the information about the length of inpatient stay and readmission rates, we combined hospital stays to one hospital stay if with the same institution identification code (unique for a specific hospital/department) the interval between discharge and readmission was <10 days, or if with different institution identification codes (for example, transfers due to the area of responsibility in care psychiatry) the interval between discharge and readmission was <3 days. This combined hospital stay with first discharge in 2015 was then regarded as the index stay. We defined the observation interval as a period of 365 days after discharge. Consequently, data from the years 2014, 2015 and 2016 were used. Only persons insured with BARMER during the entire observation interval or who died during the interval or during the index hospital stay were included. Based on the list of cities with more than 100 000 inhabitants in 2011 (30) and the available first 3 digits of the postal code of the place of residence of the patients, a patient’s place of residence was classed as a “city“. In order to estimate the density of treatment provided by physicians and psychotherapists during the index hospital stay, the since 2013 obligatory OPS codes for treatment units were obtained. Treatment units are contacts of ≥ 25 minutes reported in 25-minute increments. For group therapies, the contact period is divided by the number of participants.
Outpatient follow-up treatment with medication
The outpatient follow-up treatment with medication during the observation interval was assessed using the Anatomical Therapeutic Chemical (ATC) codes for antidepressants and the prescribed defined daily doses (DDDs) of the WHO (efigure). The day a prescription was filled and the treatment period achievable with one DDD per day were used to estimate the possible medication treatment period covered by a prescription. Follow-up prescriptions were regarded as continuous if they were filled within 7 days after the end of the period covered by the previous prescription. Hospital stays during the observation interval were recognized and included as a time interval with prescription. In order to assess whether a “guideline-adherent treatment with medication” had been administered, the first prescription in the first quarter after discharge (immediate prescription could not be made a requirement because of the possibility that a patient kept a stock of medication at home) and a continuous supply for four months (since the national clinical practice (S3) guideline on unipolar depression requires continuation of pharmacotherapy after remission for at least 4 to 9 months [9]) were used as an indicator. In the regression analysis of mortality, it was regarded as “minimal medication“ if at least one prescription for an antidepressant was filled during the observation interval.
Outpatient follow-up treatment with psychotherapy
In order to assess whether a guideline-adherent treatment with psychotherapy had been administered and to evaluate the type of psychotherapy and its provision in an individual therapy or a group therapy setting, the billed fee scale items (FSIs) were analyzed, based on the catalogues of the 2014/2015 Uniform Value Scale (EBM) of the National Association of Statutory Health Insurance Physicians (KBV) (31). For the FSI numbers, see etable 3. Since evidence from psychotherapy research indicates that measurable changes occur only after eight treatment sessions (32), the indicator “guideline-adherent psychotherapy“ was assessed as positive if treatment with psychotherapy was started or continued in the first quarter after discharge and if at least eight treatment sessions (without probationary sessions and biographical history taking) were billed. If at least 1 hour of psychotherapy was billed, it was regarded as “minimal psychotherapy”. In order to assess the interval between discharge and start of treatment and to select only patients for this who actually started a new therapy and did not just continue a treatment that had already been approved, only those patients who did not have a psychotherapy fee scale item billed in the year prior to the hospital stay were selected for this analysis.
In order to assess whether a guideline-adherent follow-up treatment had been provided, the two indicators “guideline-adherent medication“ and “guideline-adherent psychotherapy” were combined to satisfy the severity-adapted guideline requirements.
Outpatient follow-up treatment by a general practitioner or specialist
Using the billed cases as well as FSI codes it was assessed whether in the first quarter after discharge a specialist visit (specialist groups: neurology and psychiatry, psychiatry and psychotherapy, psychosomatic medicine and psychotherapy) or a general practitioner/internist visit (physician groups: general practice, physician/medical practitioner internist, pediatrician [general practitioner]) occurred. Cases in the specialist category may also have received additional services from their general practitioner. In the general practitioner category appear only those cases which did not receive additional specialist services (etable 3).
Readmissions in the second half of the observation year
For the indicator “readmissions”, all inpatient and day-patient admissions to psychiatric and psychosomatic facilities during the observation interval were counted. These stays were combined based on the same criteria used for the index stay. In order to identify risk factors of readmission to inpatient or day-patient psychiatric-psychotherapeutic or psychosomatic care (including for another diagnosis), we chose a random-intercept multilevel model of logistic regression for the categorical indicator “readmission in the second half of the observation year”. As random intercepts we first tested the variables hospital/department (in the text “hospital“, n = 527) as well as regional variances, using two-digit postal codes (in the text “region”, n = 95), in the null model. As fixed effects (predictors), the continuous variables age, hospital length of stay, and treatment units per week (as defined above), as well as the somatic comorbidities of the Charlson comorbidity index in the version of the Royal College of Surgeons were included. This current index awards one point for each diagnosis present in the following categories: myocardial infarction (ICD-10 codes I21, I22, I23, I252), congestive heart failure (I11, I13, I255, I42, I43, I50, I517), peripheral vascular disease (I70–I73, I770, I771, K551, K558, K559, R02, Z958, Z959), cerebrovascular disease (G45, G46, I60–I69), dementia (A810, F00–F03, F051, G30, G31), chronic lung disease (I26, I27, J40–J45, J46, J47, J60–J67, J684, J701, J703), connective tissue disease (M05, M06, M09, M120, M315, M32–M36), liver disease (B18, I85, I864, I982, K70. K71, K721, K729, K76, R162, Z944), diabetes mellitus (E10–E14), hemiplegia or paraplegia (G114, G81–G83), kidney disease I12, I13, N01, N03, N05, N07, N08, N171, N172, N18, N19, N25, Z49, Z940, Z992), malignancies (C00–C26, C30–C34, C37–C41, C43, C45–C58, C60–C76, C80–C85, C88, C90–C97), metastasized solid tumors (C77–C79), AIDS (B20–B24). Unlike other indices, the Charlson comorbidity index does not include age and the separately analyzed psychiatric comorbidities (33). The following categorical variables were included: sex, presence of a primary diagnosis of severe depression, treatment in a psychiatric facility (as opposed to psychosomatic), guideline-adherent treatment with antidepressants or psychotherapy as defined above, the psychiatric comorbidities of alcohol-related disorder (ICD-10 F10), other addictions (F11–F19 without F17), tobacco dependence (F17), anxiety disorder (F40–F41), obsessive-compulsive disorder (F42), PTSD (F43.1), adjustment disorder (F43.2), dissociative disorders (F44), somatoform disorders (F45), eating disorders (F50), and personality disorders (F60–F61). In addition, we calculated McFadden’s R squared to estimate the variation explained by the predictors other than the variation on the hospital and regional level. To be able to reliably estimate the likelihood function despite the multilevel structure of the data, we modelled the region and hospital allocations as fixed effects.
Mortality during the observation interval
The death data in the accessible data set are based on copies of death certificates or letters of the German pension insurance institution about the death of the person insured; thus, they can be considered reliable. We also chose a 3-level regression model to identify the risk factors of mortality (however, the intercept of region was 0) to ensure comparability. This model included the same variables we used for the indicator “readmissions“, except for the use of the indicators “minimal antidepressant treatment“ and “minimal psychotherapy“ instead of the indicators “guideline-adherent treatment with medication“ and “guideline-adherent treatment with psychotherapy“ in the first half of the year after discharge. The reason for this change was that the described indicators of guideline-adherent treatment with medication and psychotherapy would have confounded the results because of the time criteria and potential death during these time intervals.
Statistical analysis and ethical considerations
A significance level of p = 0.05 was used (two-sided). Because of the explorative nature of this study, no correction for multiple testing was applied. For analysis and statistics, SAS Enterprise Edition 7.1. was used on the servers of the BARMER Data Warehouse. For data protection reasons, only the publication of group results with large numbers is permitted. In order to protect individual affected persons from being identified, all N numbers <50 were reported as <50 in the result presentation. The authors are bound to this procedure under a contract with BARMER.
According to a statement of the Rhineland-Palatinate Medical Association, this study which uses administrative routine data does not require special approval by the ethics committee.
Key Messages.
78% of all patients, especially with severe and psychotic depression, received inpatient treatment in hospitals/departments of psychiatry and psychotherapy where the treatment provided by physicians and psychotherapists was considerable less intensive compared to the treatment that could be offered in hospitals/departments of psychosomatic medicine and psychotherapy.
In hospitals/departments of psychosomatic medicine and psychotherapy, primarily patients with moderate depression were treated, in most cases on an inpatient basis and rarely in day clinics.
After discharge, 92% of patients with severe depression did not receive the outpatient follow-up treatment with combined pharmacotherapy and psychotherapy recommended in the German clinical practice (S3) guideline on unipolar depression.
21% of patients with depression were readmitted within one year after discharge; in the regression model, more intensive treatment und follow-up treatment with psychotherapy were associated with a lower likelihood of readmission.
The standardized one-year mortality rate was 3.4 times as high as the rate for the general population. In the sample of 22 893 affected persons, 151 persons more died than would have been expected in the general population. Treatment-related risk factors for this phenomenon included, among others, a lack of follow-up treatment with medication and psychotherapy.
eTable 2. Included fee scale items (FSIs) from the Uniform Value Scale (EBM, Einheitlicher Bewertungsmaßstab) of the National Association of Statutory Health Insurance Physicians (KBV, Kassenärztliche Bundesvereinigung) 2015/2016.
| FSI code | Name |
| 35200 | PP short-term therapy, individual therapy |
| 35201 | PP long-term therapy, individual therapy |
| 35202 | PP short-term therapy, large group |
| 35203 | PP long-term therapy, large group |
| 35210 | AP individual therapy |
| 35211 | AP large group |
| 35220 | CBT short-term therapy, individual therapy |
| 35221 | CBT long-term therapy, individual therapy |
| 35222 | CBT short-term therapy, small group |
| 35223 | CBT long-term therapy, small group |
AP, analytical psychotherapy;
PP, psychodynamic psychotherapy;
CBT, cognitive behavioral therapy
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest statement Mr. Wiegand received co-authorship fees from Springer Medizin Verlag.
The remaining authors declare no conflict of interest.
References
- 1.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 2.Rubio JM, Olfson M, Pérez-Fuentes G, Garcia-Toro M, Wang S, Blanco C. Effect of first episode axis I disorders on quality of life. J Nerv Ment Dis. 2014;202:271–274. doi: 10.1097/NMD.0000000000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13:153–160. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melchior H, Schulz H, Härter M. Faktencheck Gesundheit. Bertelsmann Stiftung. 2014:1–144. [Google Scholar]
- 5.Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry. 2011;68:1058–1064. doi: 10.1001/archgenpsychiatry.2011.113. [DOI] [PubMed] [Google Scholar]
- 6.Simon GE, VonKorff M. Suicide mortality among patients treated for depression in an insured population. Am J Epidemiol. 1998;147:155–160. doi: 10.1093/oxfordjournals.aje.a009428. [DOI] [PubMed] [Google Scholar]
- 7.Melartin TK, Rytsälä HJ, Leskelä US, Lestelä Mielonen PS, Sokero TP, Isometsä ET. Severity and comorbidity predict episode duration and recurrence of DSM-IV major depressive disorder. J Clin Psychiatry. 2004;65:810–819. doi: 10.4088/jcp.v65n0612. [DOI] [PubMed] [Google Scholar]
- 8.Holma KM, Holma IAK, Melartin TK, Rytsälä HJ, Isometsä ET. Long-term outcome of major depressive disorder in psychiatric patients is variable. J Clin Psychiatry. 2008;69):196–205. doi: 10.4088/jcp.v69n0205. [DOI] [PubMed] [Google Scholar]
- 9.DGPPN, BÄK, KBV, AWMF. S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression - Langfassung, 2. Auflage. Version 5. 2017: 1-238. www.awmf.org/leitlinien/detail/ll/nvl-005.html (last accessed on 16 April 2020) [Google Scholar]
- 10.Wiegand HF, Sievers C, Schillinger M, Godemann F. Major depression treatment in Germany - descriptive analysis of health insurance fund routine data and assessment of guideline-adherence. J Affect Disord. 2016;189:246–253. doi: 10.1016/j.jad.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Gaebel W, Kowitz S, Zielasek J. The DGPPN research project on mental healthcare utilization in Germany: inpatient and outpatient treatment of persons with depression by different disciplines. Eur Arch Psychiatry Clin Neurosci. 2012;262:51–55. doi: 10.1007/s00406-012-0363-2. [DOI] [PubMed] [Google Scholar]
- 12.Trautmann S, Beesdo-Baum K, Knappe S, et al. The treatment of depression in primary care— a cross-sectional epidemiological study. Dtsch Arztebl Int. 2017;114:721–728. doi: 10.3238/arztebl.2017.0721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herzog DP, Wagner S, Ruckes C, et al. Guideline adherence of antidepressant treatment in outpatients with major depressive disorder: a naturalistic study. Eur Arch Psychiatry Clin Neurosci. 2017;267:711–721. doi: 10.1007/s00406-017-0798-6. [DOI] [PubMed] [Google Scholar]
- 14.McFadden D. Quantitative methods for analyzing travel behavior of individuals. Cowles Foundation Discussion Paper No. 474. 1977 [Google Scholar]
- 15.Statistisches Bundesamt. Bevökerungsvorrausberechnung. https://service.destatis.de/bevoelkerungspyramide/#!y=2015&v=2 (last accessed on 16 April 2019) [Google Scholar]
- 16.Statistisches Bundesamt. Gesundheit; Grunddaten der Krankenhäuser - Fachserie 12 Reihe 6.1.1 - 2015. 2016; 1-155. www.destatis.de/GPStatistik/servlets/MCRFileNodeServlet/DEHeft_derivate_00031004/2120611157004.pdf (last accessed on 2 January 2020) [Google Scholar]
- 17.Normann C, Wolff J, Hochlehnert A, et al. Resource use and financing of guideline-adherent psychotherapeutic inpatient care. Nervenarzt. 2015;86:534–541. doi: 10.1007/s00115-015-4309-6. [DOI] [PubMed] [Google Scholar]
- 18.Berger M, Wolff J, Normann C, et al. Guideline-adherent psychiatric-psychotherapeutic hospital care. Nervenarzt. 2015;86:542–548. doi: 10.1007/s00115-015-4310-0. [DOI] [PubMed] [Google Scholar]
- 19.Godemann F, Wolff-Menzler C, Löhr M, et al. Calculating personnel allocation at 100 % implementation of the psychiatry personnel act. Nervenarzt. 2015;86:845–851. doi: 10.1007/s00115-015-4354-1. [DOI] [PubMed] [Google Scholar]
- 20.Friederich HC, Heuft G, Cuntz U, et al. Staffing level: Survey among psychosomatic-psychotherapeutic institutions in Germany. Z Psychosom Med Psychother. 2018;64:334–349. doi: 10.13109/zptm.2018.64.4.334. [DOI] [PubMed] [Google Scholar]
- 21.Härter M, Sitta P, Keller F, et al. Externe Qualitatssicherung bei stationarer Depressionsbehandlung Modellprojekt der Landesarztekammer Baden-Württemberg. Dtsch Arztebl. 2004;101 A 197074. [Google Scholar]
- 22.McHugh RK, Whitton SW, Peckham AD, Welge JA, Otto MW. Patient preference for psychological vs pharmacologic treatment of psychiatric disorders. J Clin Psychiatry. 2013;74:595–602. doi: 10.4088/JCP.12r07757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark DM, Canvin L, Green J, Layard R, Pilling S, Janecka M. Transparency about the outcomes of mental health services (IAPT approach): an analysis of public data. Lancet. 2018;391:679–686. doi: 10.1016/S0140-6736(17)32133-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bermejo I, Hölzel LP, Voderholzer U, van Elst LT, Berger M. Optimal versorgt bei Depression - Freiburger Modell zur Integrierten Versorgung depressiver Erkrankungen. Z Evid Fortbild Qual Gesundhwes. 2012;106:625–630. doi: 10.1016/j.zefq.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Schmid P, Steinert T, Borbé R. Systematische Literaturübersicht zur Implementierung der sektorübergreifenden Versorgung (Regionalbudget, integrierte Versorgung) in Deutschland. Psychiatr Prax. 2013;40:414–424. doi: 10.1055/s-0033-1343192. [DOI] [PubMed] [Google Scholar]
- 26.Deuschle M, Scheydt S, Hirjak D, et al. Track treatment in psychiatry: the CIMH track model to overcome sector boundaries. Nervenarzt. 2020;91:50–56. doi: 10.1007/s00115-019-0704-8. [DOI] [PubMed] [Google Scholar]
- 27.Bundespsychotherapeutenkammer. Ein Jahr nach der Reform der Psychotherapie-Richtlinie - Wartezeiten. 2018 [Google Scholar]
- 28.Hölzel L, Härter M, Reese C, Kriston L. Risk factors for chronic depression—a systematic review. J Affect Disord. 2011;129:1–13. doi: 10.1016/j.jad.2010.03.025. [DOI] [PubMed] [Google Scholar]
- 29.Henssler J, Heinz A, Brandt L, Bschor T. Antidepressant withdrawal and rebound phenomena—a systematic review. Dtsch Arztebl Int. 2019;116:355–361. doi: 10.3238/arztebl.2019.0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Statistisches Bundesamt. Gemeindeverzeichnis-Sonderveröffentlichung Gebietsstand: 31.12.2011. 2013 Jul pp. 1-5. www.destatis.de/DE/Themen/Laender-Regionen/Regionales/Gemeindeverzeichnis/Administrativ/05-staedte.html (last accessed on 16 April 2019) [Google Scholar]
- 31.Kassenärztliche Bundesvereinigung. Einheitlicher Bewertungsmaßstab (EBM) Berlin; 2015: 1-1546. www.kbv.de/html/arztgruppen_ebm.php#content2403 (last accessed on 16 April 2020) [Google Scholar]
- 32.Lambert NJ. Bergin and Garfield‘s handbook of psychotherapy and behavior change. New Jersey: John Wiley & Sons. 2013 [Google Scholar]
- 33.Armitage JN, van der Meulen JH. Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg. 2010;97:772–781. doi: 10.1002/bjs.6930. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
Index population and index hospital treatment
Via a secured VPN tunnel, the authors (H.F.W., J.S., U.M.) had access to the BARMER Data Warehouse. From the about 9.4 million persons insured with BARMER in 2015, those were selected who were between 18 and 65 years of age in 2015 and discharged from psychiatric-psychotherapeutic or psychosomatic-psychotherapeutic inpatient treatment with an ICD-10 diagnosis of F32.x (major depressive disorder, single episode) or F33.x (major depressive disorder, recurrent). It is common that patients undergoing prolonged inpatient treatment are occasionally discharged for a short period of time (for example, in case of a long weekend due to a public holiday, transitions between treatment settings or as a discharge on a trial basis to test prolonged exposure to stress). Since these events would confound the information about the length of inpatient stay and readmission rates, we combined hospital stays to one hospital stay if with the same institution identification code (unique for a specific hospital/department) the interval between discharge and readmission was <10 days, or if with different institution identification codes (for example, transfers due to the area of responsibility in care psychiatry) the interval between discharge and readmission was <3 days. This combined hospital stay with first discharge in 2015 was then regarded as the index stay. We defined the observation interval as a period of 365 days after discharge. Consequently, data from the years 2014, 2015 and 2016 were used. Only persons insured with BARMER during the entire observation interval or who died during the interval or during the index hospital stay were included. Based on the list of cities with more than 100 000 inhabitants in 2011 (30) and the available first 3 digits of the postal code of the place of residence of the patients, a patient’s place of residence was classed as a “city“. In order to estimate the density of treatment provided by physicians and psychotherapists during the index hospital stay, the since 2013 obligatory OPS codes for treatment units were obtained. Treatment units are contacts of ≥ 25 minutes reported in 25-minute increments. For group therapies, the contact period is divided by the number of participants.
Outpatient follow-up treatment with medication
The outpatient follow-up treatment with medication during the observation interval was assessed using the Anatomical Therapeutic Chemical (ATC) codes for antidepressants and the prescribed defined daily doses (DDDs) of the WHO (efigure). The day a prescription was filled and the treatment period achievable with one DDD per day were used to estimate the possible medication treatment period covered by a prescription. Follow-up prescriptions were regarded as continuous if they were filled within 7 days after the end of the period covered by the previous prescription. Hospital stays during the observation interval were recognized and included as a time interval with prescription. In order to assess whether a “guideline-adherent treatment with medication” had been administered, the first prescription in the first quarter after discharge (immediate prescription could not be made a requirement because of the possibility that a patient kept a stock of medication at home) and a continuous supply for four months (since the national clinical practice (S3) guideline on unipolar depression requires continuation of pharmacotherapy after remission for at least 4 to 9 months [9]) were used as an indicator. In the regression analysis of mortality, it was regarded as “minimal medication“ if at least one prescription for an antidepressant was filled during the observation interval.
Outpatient follow-up treatment with psychotherapy
In order to assess whether a guideline-adherent treatment with psychotherapy had been administered and to evaluate the type of psychotherapy and its provision in an individual therapy or a group therapy setting, the billed fee scale items (FSIs) were analyzed, based on the catalogues of the 2014/2015 Uniform Value Scale (EBM) of the National Association of Statutory Health Insurance Physicians (KBV) (31). For the FSI numbers, see etable 3. Since evidence from psychotherapy research indicates that measurable changes occur only after eight treatment sessions (32), the indicator “guideline-adherent psychotherapy“ was assessed as positive if treatment with psychotherapy was started or continued in the first quarter after discharge and if at least eight treatment sessions (without probationary sessions and biographical history taking) were billed. If at least 1 hour of psychotherapy was billed, it was regarded as “minimal psychotherapy”. In order to assess the interval between discharge and start of treatment and to select only patients for this who actually started a new therapy and did not just continue a treatment that had already been approved, only those patients who did not have a psychotherapy fee scale item billed in the year prior to the hospital stay were selected for this analysis.
In order to assess whether a guideline-adherent follow-up treatment had been provided, the two indicators “guideline-adherent medication“ and “guideline-adherent psychotherapy” were combined to satisfy the severity-adapted guideline requirements.
Outpatient follow-up treatment by a general practitioner or specialist
Using the billed cases as well as FSI codes it was assessed whether in the first quarter after discharge a specialist visit (specialist groups: neurology and psychiatry, psychiatry and psychotherapy, psychosomatic medicine and psychotherapy) or a general practitioner/internist visit (physician groups: general practice, physician/medical practitioner internist, pediatrician [general practitioner]) occurred. Cases in the specialist category may also have received additional services from their general practitioner. In the general practitioner category appear only those cases which did not receive additional specialist services (etable 3).
Readmissions in the second half of the observation year
For the indicator “readmissions”, all inpatient and day-patient admissions to psychiatric and psychosomatic facilities during the observation interval were counted. These stays were combined based on the same criteria used for the index stay. In order to identify risk factors of readmission to inpatient or day-patient psychiatric-psychotherapeutic or psychosomatic care (including for another diagnosis), we chose a random-intercept multilevel model of logistic regression for the categorical indicator “readmission in the second half of the observation year”. As random intercepts we first tested the variables hospital/department (in the text “hospital“, n = 527) as well as regional variances, using two-digit postal codes (in the text “region”, n = 95), in the null model. As fixed effects (predictors), the continuous variables age, hospital length of stay, and treatment units per week (as defined above), as well as the somatic comorbidities of the Charlson comorbidity index in the version of the Royal College of Surgeons were included. This current index awards one point for each diagnosis present in the following categories: myocardial infarction (ICD-10 codes I21, I22, I23, I252), congestive heart failure (I11, I13, I255, I42, I43, I50, I517), peripheral vascular disease (I70–I73, I770, I771, K551, K558, K559, R02, Z958, Z959), cerebrovascular disease (G45, G46, I60–I69), dementia (A810, F00–F03, F051, G30, G31), chronic lung disease (I26, I27, J40–J45, J46, J47, J60–J67, J684, J701, J703), connective tissue disease (M05, M06, M09, M120, M315, M32–M36), liver disease (B18, I85, I864, I982, K70. K71, K721, K729, K76, R162, Z944), diabetes mellitus (E10–E14), hemiplegia or paraplegia (G114, G81–G83), kidney disease I12, I13, N01, N03, N05, N07, N08, N171, N172, N18, N19, N25, Z49, Z940, Z992), malignancies (C00–C26, C30–C34, C37–C41, C43, C45–C58, C60–C76, C80–C85, C88, C90–C97), metastasized solid tumors (C77–C79), AIDS (B20–B24). Unlike other indices, the Charlson comorbidity index does not include age and the separately analyzed psychiatric comorbidities (33). The following categorical variables were included: sex, presence of a primary diagnosis of severe depression, treatment in a psychiatric facility (as opposed to psychosomatic), guideline-adherent treatment with antidepressants or psychotherapy as defined above, the psychiatric comorbidities of alcohol-related disorder (ICD-10 F10), other addictions (F11–F19 without F17), tobacco dependence (F17), anxiety disorder (F40–F41), obsessive-compulsive disorder (F42), PTSD (F43.1), adjustment disorder (F43.2), dissociative disorders (F44), somatoform disorders (F45), eating disorders (F50), and personality disorders (F60–F61). In addition, we calculated McFadden’s R squared to estimate the variation explained by the predictors other than the variation on the hospital and regional level. To be able to reliably estimate the likelihood function despite the multilevel structure of the data, we modelled the region and hospital allocations as fixed effects.
Mortality during the observation interval
The death data in the accessible data set are based on copies of death certificates or letters of the German pension insurance institution about the death of the person insured; thus, they can be considered reliable. We also chose a 3-level regression model to identify the risk factors of mortality (however, the intercept of region was 0) to ensure comparability. This model included the same variables we used for the indicator “readmissions“, except for the use of the indicators “minimal antidepressant treatment“ and “minimal psychotherapy“ instead of the indicators “guideline-adherent treatment with medication“ and “guideline-adherent treatment with psychotherapy“ in the first half of the year after discharge. The reason for this change was that the described indicators of guideline-adherent treatment with medication and psychotherapy would have confounded the results because of the time criteria and potential death during these time intervals.
Statistical analysis and ethical considerations
A significance level of p = 0.05 was used (two-sided). Because of the explorative nature of this study, no correction for multiple testing was applied. For analysis and statistics, SAS Enterprise Edition 7.1. was used on the servers of the BARMER Data Warehouse. For data protection reasons, only the publication of group results with large numbers is permitted. In order to protect individual affected persons from being identified, all N numbers <50 were reported as <50 in the result presentation. The authors are bound to this procedure under a contract with BARMER.
According to a statement of the Rhineland-Palatinate Medical Association, this study which uses administrative routine data does not require special approval by the ethics committee.