Introduction
Managing the millions of children and adolescents who are either overweight or obese has become a major challenge for the healthcare community. In 1997, an Expert Committee was convened by the Maternal and Child Health Bureau of the Health Resources and Services Administration (HRSA), Department of Health and Human Services, (DHHS) to develop guidelines for healthcare providers.1 In 2005, the American Medical Association, in cooperation with HRSA and the Center for Disease Control and Prevention, created an Expert Committee to update those initial guidelines.2 And in 2008, the Agency for Healthcare Research and Quality of the HHS came out with an Evidence-Based/Technology Assessment entitled “The Effectiveness of Weight Management Programs in Children and Adolescents.”3
In addition to these government-sponsored guidelines, recommendations for management of overweight and obesity in this population have been issued by multiple other organizations. The one directive they all have in common is that a multicomponent program that focuses on physical activity, diet, and behavioral change should be the first line of treatment offered.
Alt-text: Unlabelled box
This article highlights the evidence-based data, presents the various ways in which this multicomponent approach can be implemented, and includes the roles of school programs and bariatric surgery as weight management options.
Family-based sessions
Family-based group sessions coordinated by a registered dietitian (RD/RDN) are a crucial part of multicomponent interventions.
The Academy of Nutrition and Dietetics, which issued its Pediatric Weight Management Evidence-Based Guidelines in 2015, has reported positive weight status outcomes, both shorter-term (6 months) and longer-term (12 months), when group pediatric weight management sessions and family participation are coordinated.4 , 5
Alt-text: Unlabelled box
Individual family and mixed-format (which includes some time with individual families and some group time) approaches have been found to be superior to group-only approaches as per the latest US Preventative Services Task Force (USPSTF) recommendations.6 However, including some group sessions may offer the opportunity for social support and improve cost effectiveness.7 The dose of treatment has a strong impact on success. Multicomponent behavioral interventions of moderate (26–75 h of treatment contact per year) to high intensity (> 75 h) for obese children and adolescents, ages six and older, have been shown to yield short term improvements in up to 12 months. Obtaining a qualitative assessment of a patient's diet with a particular focus on dietary patterns thought to be linked to excess energy intake and adiposity is recommended, as intervening with these patterns can significantly reduce intake and potentially improve nutritional status.8 Tailoring interventions by considering patient and family motivation, as well as readiness for change, is optimal. The family-based approach can be modified based on the age of the patient and the degree of parental involvement. It should be noted that family involvement has been shown to be less effective when the patients are older teens.9
Behavioral treatments
At the heart of behavioral treatment for obesity is determining what behaviors are modifiable and what therapies to use to help patients achieve the needed modifications. Motivational Interviewing (MI), which is a patient-centered counseling style, has been shown to be effective in primary care settings.10 A dietitian should be included, as the RDN's knowledge and skill base are critical in the ongoing process of addressing the diverse needs of clients and families.4 , 10
Cognitive behavioral management and gradual stepwise change have been explored in depth for childhood and adolescent obesity treatment. Individuals get acclimated to recommended changes over time by making adjustments in their dietary patterns and food environment and by learning to set limits on eating unhealthy food.
Alt-text: Unlabelled box
Short-term goals are established in order to lead to long-term habits that change the way individuals and their families think about food. Cognitive Behavioral Therapy (CBT) focuses on breaking the negative cycle that is a part of weight-related difficulties in obesity, the “maladaptive daily patterns, cognition that is distorted, and problematic behaviors” cited by Wilfley et al.11 It allows for a restructuring of daily patterns. Bloom et al. explores utilizing a form of CBT known as CBT-AF to address appetite awareness and cues for eating.12 CAAT is an adapted version used with children and adolescents to sensitize them to recognize and respond to internal appetite cues such as hunger and satiety in order to improve their self-regulation of energy intake. Results of one study showed a significant reduction in body mass index (BMI) for children in a CAAT group compared to those in a control group. However, this impact was only studied short term. The researchers concluded that CAAT holds promise as a treatment modality since overweight and obese children are often less effective in regulating food intake compared to normal weight children.13 , 14
In the Transtheoretical Model of Change, in which change occurs in stages, the readiness of parents for personal change, as well as their readiness to help their children make changes, becomes a pivotal factor for success in a weight management program.15 Tailored messages to parents may help modulate their “decisional balance,” (the value of making behavioral changes versus the value of not making any changes) and contribute to the likelihood of treatment success for their children. Yet influencing parents so as to influence their children in terms of weight management behaviors can be a challenge. Weight loss is a “complex behavior” which encompasses two separate “domains” of change– eating habits and physical activity. Although these are often considered together, each carries unique challenges with respect to perceived confidence and readiness for change.16 , 17 In a cross-sectional study with a convenience sample of parents (or guardians) of children attending a tertiary care pediatric obesity clinic, parents completed surveys initially and again on follow up visits to assess their readiness for change.16 Those in the action/maintenance state of change were more likely to be actively making changes to multiple eating behaviors–i.e. availability of sugar-sweetened beverages (SSBs) and salty snacks, and in physical activity patterns–i.e. reaching recommended levels of increased activity and limiting screen time. Their children were more likely to be more physically active and to consume less fast food and more fruits and vegetables than the children of parents in the other stages of change.16 Parents who believed their own weight was a health problem were less ready to make changes to their children's diet.18 These authors suggest that maintaining both parent and patient motivation should be a focal point of treatment and that this may entail a variety of approaches, such as using texting or other electronic devices to assess the stage of change for readiness and decisional support.18
Mobile health interventions and telemedicine
Use of mobile health technology as an adjunct to behavioral based weight management strategies is becoming more common.
Alt-text: Unlabelled box
Chen and researchers reported on a convenience sample of self-identified Chinese-American adolescents with BMI ≥ 85th percentile who participated in a culturally focused intervention called Smart Start.19 It provided general health education, wearable fitness trackers, online educational modules, and tailored biweekly text messages. A benefit in outcome occurred in both the control and intervention groups. However, over a six month period, the intervention group, as compared to the control group, had “statistically greater changes” in BMI that were associated with less fast food intake, a lower intake of SSBs, and an increase in physical activity levels and decreased sedentary behavior.19 Overall, mobile health use has shown mixed benefits for weight management in adolescents and young adults.20 Other mobile health initiatives have resulted in weight loss in the experimental groups that was not sustained21 , 22 or have displayed no further benefits above that of the standard care group.23 Researchers have thus noted limited evidence of efficacy of mobile health interventions as a stand-alone treatment modality.24
The impact of combining the mobile health approach with components of behavior based interventions has been examined by Cueto et al.25 They evaluated the original Kurbo app (circa 2014) before it became Kurbo WW.26 Designed to promote behavior change and encourage healthy lifestyle choices, it used the evidence-based traffic light diet approach27 and Kurbo health coaching through the incorporation of behavior substitutions and habit formation.28 Although Kurbo includes components of behavior-based interventions proven successful in pediatric and adolescent weight management, it has come under fire for promoting behaviors that can be perceived as overly restrictive and potentially promoting eating disorder behaviors.29 Questions have been raised based on degree of weight loss in young subscribers and whether adequate monitors are in place to determine that degree. Prior studies have warned about the potential for “growth velocity to be negatively impacted when caloric intake is restricted,” and thus growth velocity must be followed carefully during and after weight loss in children and younger adolescents, and medical supervision may be warranted.30 , 31
Other combined interventions utilizing mobile health apps have yielded partial success. One 12-month technology-based program for adolescents with Type 2 diabetes “was not sufficient to produce weight loss with the combination of web intervention and group sessions and telephone follow up, but improvements in sedentary behavior and use of behavior change strategies expected to lead to behavior change was evidenced.”32
Telemedicine, in theory, should be able to compensate for some of the barriers that prevent access to and utilization of family based comprehensive behavioral interventions for child and adolescent obesity.33 These barriers include time, transportation, access, cost, scheduling challenges, stigmatization, language barriers and more.34, 35, 36, 37 Rural populations have been studied for feasibility and satisfaction with telemedicine treatment approaches, and results have been comparable to standard treatment outcomes.38 Urban populations can face similar barriers to attendance of programs held in hospitals or university medical settings– delays in acquiring care, fear of being judged based on native language or residency, and possible stigmatization.39 Consequently, there have been studies here too (even prior to the COVID-19 pandemic) regarding the incorporation of telemedicine as a supplemental arm of treatment modalities involving group sessions and mixed formats with medical staff including physicians, nurse practitioners (NPs), nurses, psychologists, family counselors, dietitians, physical therapists, exercise specialists, and social workers.38 , 39 With the dramatic increase in the use of telemedicine brought about by the COVID-19 pandemic, this modality of treatment will certainly be utilized and studied considerably more in the upcoming months and years.
Mobile apps have proved an engaging way to involve children in health behavior changes,40 allowing for delivery of health information in a portable, “entertaining” way.41, 42, 43 These apps are capable of promoting some of the expert recommendations for healthy eating and physical activity, including setting goals/limits and reducing intake of SSBs, but they often do not go deeper into behavior change. One app, Hyperant™, utilized a set of “Hyper Activity Cards™” to give children ideas for health-promoting behaviors including physical activity, healthy eating, and sleep.44 However, it only provides user messages without offering the opportunity for interaction. In a meta-analysis of mobile health technologies for self-monitoring, Darling et al. concluded that self-monitoring techniques using mobile health technologies have a small but significant effect on weight status in children and adolescents.45
Population health initiatives
A more “macro approach” for educating and guiding children, adolescents, their families and guardians is called for to achieve greater success in maintaining better health and weight management. Several such programs are described below.
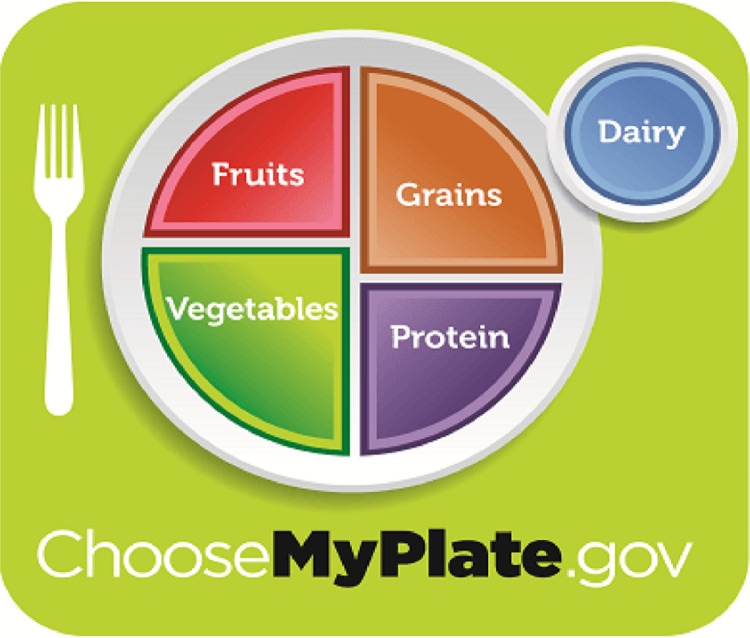
The ChooseMyPlate teaching initiative from the U.S. Department of Agriculture (USDA) came out of the need for a vehicle to effectively and “with maximum visibility” communicate the 2010 Dietary Guidelines for Americans (DGAs) in order to foster a healthier lifestyle.46 Using print and online resources to engage the public, it was translated into several languages, incorporated into health curriculum resources created for nutrition education for children and adults, and promoted to nutrition communicators, educators and the food industry, calling upon them to “get the message out.”47, 48, 49 Its message: “Americans can achieve a healthier weight by eating more of some foods,” was thought to be one that consumers could embrace. When one's plate has a larger proportion of lower calorie vegetables, they, in essence, “crowd out’ the more calorically dense other foods on the plate like refined grains and high fat proteins. Thus, adding foods, rather than taking away foods, can result in a calorie deficit. Designed to “impact behavior during meal planning” and “perception during meal consumption,” this initiative aimed to be seen by individuals and groups as a positive way of collectively altering energy balance.
ChooseMyPlate calls for a shift in consumption patterns. It emphasizes less processed foods and more of whole grains, lower fat and non-fat dairy items over full-fat varieties, water in place of SSBs, and protein alternatives, including leaner meats. Along with less saturated fat and added sugars, lower sodium options are promoted.
Alt-text: Unlabelled box
Central to this multimodal plan is the plate icon (Fig. 1 ) that replaces the Food Guide Pyramid as both visual cue and accepted standard.48 , 49 The most current recommendations, as per MyPlate, MyWins (see below), directs people to “find your healthy eating style and maintain it for a lifetime” by making half of the meal plate fruits and vegetables (varying the veggies and focusing on whole fruits), making a quarter of the plate grains (half of them whole grains), and making the remaining quarter of the plate proteins (varying the protein routine). Individuals are advised to move to low-fat or fat-free milk or yogurt for dairy intake, which is depicted alongside on the right of the icon's plate. The “right mix” is based on variety, amount, and nutrition content.
Fig. 1.
Choose MyPlate Graphic. Source: www.choosemyplate.gov.
The original MyPlate teaching campaign was revamped to reflect changes in the updated DGAs (2015–2020). MyPlate, MyWins, launched in 2015, strongly focuses on food patterns. It added the concept of “a healthy eating style” which can be achieved with “small changes” to promote the goal of getting individuals to realize that “what you eat and drink over time matters and can help you be healthier now, and in the future,” messaging that reflected the evolving emphasis of the DGAs. The public was encouraged to be more engaged and active in their health, and was invited to virtually share personal experiences with MyPlate, MyWins on social media using #MyPlateMyWins.
The present day ChooseMyPlate.gov website includes printable materials, images, and graphics available as downloadable PDFs, JPGs, and other files—all in the public domain so that no permission is required to print, reproduce, or use them. Resources have grown to include a host of topics, from meal planning and food safety to physical activity and seasonal resources. Information continues to be available in diverse formats like toolkits, quizzes, infographics, and videos.
Researchers out of the Behavioral Health and Nutrition Department at the University of Delaware used MyPlate to test whether peer education improved self-efficacy, perceptions and attitudes toward healthy eating, and physical activity.50 , 51 They concluded that peer education could promote improved knowledge and attitudes about MyPlate among college students and increase their self-efficacy, helping them make healthier decisions with regard to food and food intake. The pilot First Year Experience course curriculum developed at the university became mandatory coursework for all incoming freshmen.41
A Florida study of elementary school children whose families qualified for federal assistance via the Supplemental Nutrition Assistance Program (SNAP), utilized the six-lesson Youth Understanding MyPlate (YUM) curriculum to teach the students through grade specific activities. The children reported an increase in intake of fruits and vegetables, grains, low-fat/fat-free dairy, healthy snacks, eating breakfast, and physical activity, compared to baseline.52
5-2-1-0 Let's Go! is another nationally recognized program that aims to create environments supporting healthy choices, healthy habits, and healthy living within a multi-setting model.53, 54, 55, 56 Developed in Maine in 2006 by a group of professionals on a mission to tackle childhood obesity by using evidence-based tools and strategies, it has expanded and gained momentum through its strong, far-reaching program and campaign designed to reach out to families “where they live, learn, work, and play.”53 Its premise is that if children and families are exposed to the same health message in multiple places across their community, and if those places have policies and environments that support healthy choices, then children and families will be more likely to adopt those behaviors and maintain them in their daily lives.
The foundation for change as modeled in the 5-2-1-0 healthy habits message is based on the following daily measures: 5 or more fruits and vegetables, 2 h or less of recreational screen time (TV/computers to be kept out of the bedroom and no screen time under the age of 2), 1 h or more of physical activity, and 0 sugary drinks and more water intake (Fig. 2 ).
Fig. 2.
5-2-1-0 Healthy Habits Message. Source: www.letsgo.org.
Alt-text: Unlabelled box
Though this message has been found to increase awareness and healthy behaviors, it remains to be seen if that will translate to concrete behavioral changes.
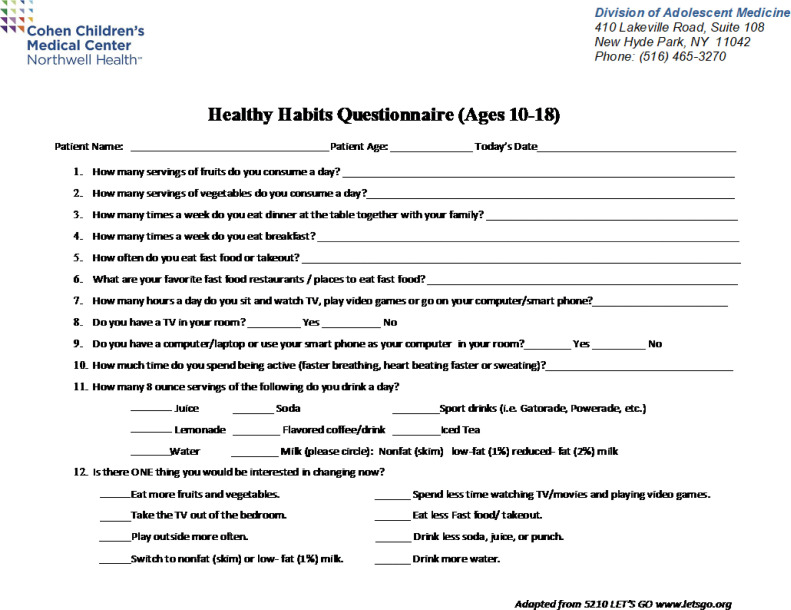
Many pediatric and primary care offices across the country have started to implement 5-2-1-0 Let's Go! into their practices to potentially impact the health of their patients, as have hospital-based specialty programs. The POWER Kids Weight Management Program of Cohen Children's Medical Center at Northwell Health is the authors’ multidisciplinary program for overweight and obese children and adolescents, 8 to 18 years of age. In advance of meeting with program staff or at the initial assessment by the program's registered dietitian nutritionist (RDN), prior to any interventions, the patient or the parent/guardian is asked to fill out a Healthy Habits Questionnaire adapted from and directly correlated to the 5-2-1-0 Let's Go! program (Fig. 3 ). One version is for children up to 9 years of age, another for 10 to 18- year-olds, and both are available in Spanish as well as English. This POWER Kids questionnaire uses a modified food- frequency survey style to ask questions regarding food and beverages and includes other questions that address time allocation for activity and sedentary pursuits as well as family meal patterns and access to TV. What emerges are overall patterns, habits, and choices, ending with a glimpse as to what the child or adolescent is willing to change. Answers to the questions help guide the direction of behavioral, nutritional, and exercise interventions. Focusing on domains where program participants exhibit deficiencies, while reinforcing already established positive health-related behaviors, helps to pave the path to successful weight management. The goal is to use the 5-2-1-0 message to encourage the children and adolescents in the program to develop healthy habits that can positively impact what would otherwise be their trajectory for further excess weight gain and the associated co-morbidities of obesity.
Fig. 3.
Healthy Habits Questionnaire for ages 10-18 (adapted for use in POWER Kids Program from 5210 Let's Go www.letsgo.org).
Let's Move is the comprehensive initiative launched in 2010 by former First Lady Michelle Obama the same day that President Barak Obama signed the memorandum creating the Task Force on Childhood Obesity.
Alt-text: Unlabelled box
In partnership with the Alliance for a Healthier Generation, it is dedicated to solving the problem of obesity “within a generation” so that “children born today will grow up healthier and be able to pursue their dreams.”57 The focus is on creating a healthy start for children, empowering parents and caregivers, providing healthy food in schools, improving access to healthy affordable foods, and increasing physical activity. One of its many ambitious goals is the commitment to giving children a voice and a presence. Families are encouraged to recognize that children can create healthy lunches from their own kitchens and express their unique preferences as to what “healthy eating” translates into for them. The Healthy Lunchtime Challenge has drawn representatives from every state and territory in the United States, and the accumulation of recipes from the annual challenges is accessible online as “historical material.”57
The Let's Move! Outside program, developed to bridge the growing disconnect between young people and the great outdoors, and to emphasize the need for active play, has been adopted by the YMCA of the USA, through its Youth Development Division, using programs and services shown to be instrumental in their diabetes prevention program (DPP) trials.58 Eligible children and adolescents, ages 5–17, representing a wide variety of socioeconomic backgrounds, were recruited for a randomized computer-assisted intervention that included their families, to assess whether eliminating financial barriers to YMCA membership could encourage increased physical activity in the environment of a supportive family.59 Extensive resources were available to those who utilized the services. All participants and their parents and guardians were scheduled to attend 4 nutrition classes administered by a Registered Dietitian (RD) and to return for evaluation at 2, 4, 6, 9, and 12 months. Children were randomized to nutrition class only (n = 39) or nutrition class and free family YMCA membership (n = 44). Nutrition classes did not differentiate between those in the control and treatment groups. Of the 36 evaluable participants randomized to treatment, only 27 ever visited the YMCA, with a median of 5 visits reported. Overall attendance at scheduled study-related visits was poor. Only 2 participants in each group attended all 6 scheduled visits. For nutrition classes, at least 1 class was attended by 67% of the treatment group, but only 30% of controls. Attendance in the nutrition classes led to improvements in nutritional intake for both groups. Four participants in the control group and 1 in the treatment group achieved the target reduction of 2 BMI percentile points. There was a positive, but very small, relationship for YMCA attendees between the number of visits and the loss of either BMI or weight, which was not statistically significant.
Another major initiative promoting physical activity and healthy eating among children (in this case, as young as kindergarten and through 12th grade) that has been studied and evaluated is the NFL Play 60 FitnessGram Partnership Project, led by teachers in school settings across 32 National Football League franchise markets. (Its two most popular programs are Fuel Up to Play 60, in collaboration with the United States Dairy Association (USDA), and the NFL Play 60 Challenge created in conjunction with American Heart Association (AHA). The latter has its own app which originally allowed users to choose an avatar with which to complete a course through a virtual outdoor park while listening to health promoting messages like “make sure you drink enough water today” (it no longer includes an “in the game” motion sensor but still gauges and delivers health concepts.) The longitudinal impact of NFL Play 60 programming was measured using data based on students from 497 schools who completed FitnessGram assessments annually, starting in 2011 through 2015. For schools that participated in the program, annual improvements in aerobic capacity were significantly greater for both girls and boys, compared with non-programming schools. Both girls and boys in participating schools showed annual improvement in BMI Healthy Fitness Zone achievement. Students in schools that implemented the program for the entire 4 years tended to have better improvements in aerobic capacity than those in schools enrolled for only 2 or 3 years.60
It is fair to say that each of the national initiatives described in this section had some impact on nutrition and physical activity for many children and adolescents but that the impact was modest for most and minimal for many. Going forward, it can prove useful to combine the messages of these multiple programs into one unified message that can be promoted throughout the country in a way that will strengthen their message and thereby yield a stronger effect on the nutritional and physical activity patterns for the youth of the nation.
Impacting habitual dynamics
Advances in technology have brought about the proliferation of electronic devices now available to children and adolescents who are spending long durations of time in sedentary activities involving handheld devices and video consuls. Current guidelines call for limiting sedentary screen time to 2 h or less.61 Among the many concerns being addressed is that increased time on electronics/screen time becomes a potential source of additional energy intake.
In a clever harnessing of this dynamic, health professionals are exploring the use of electronics and gaming for getting children to be more physically active. Games like Wii/WiiU, Xbox Connect, Nintendo, and variations of them have offered small promise. Active video games can acutely increase light to moderate physical activity. However, they are unlikely to impact increased habitual activity or significantly decrease sedentary behaviors.62 Rose et al. in their systematic review of digital interventions for improving diet and physical activity behaviors in adolescents, struggled with the heterogenicity of studies not being conducive to a meta-analysis and urged setting up future research initiatives in digital health as a cost-effective medium for health promotion.63
A great deal of thought and programing is being directed to creating challenges and monitoring progress with physical activity. And sometimes the unexpected turns up with great outcomes. For a time in 2016, the Pokémon Go app set off a frenzy of interest in walking, sometimes long distances, to find and catch Pokémon avatars.64 An estimated 9–21 million people used the app and increased their daily step count, with some reaching as many as 15,000 steps a day.65
Step challenges have worked well in the adult population with competitions awarding badges, status recognition, and prizes for accumulating steps. In the early 2000s portable watches that were affordable and fashionable were introduced for use in tracking steps. Prior to this, they had only been available at research grade.
Studies exploring step tracking have shown promising results in that a positive feedback loop is established, whereby accumulating steps reinforces continuation of the activity.
Alt-text: Unlabelled box
Efforts at encouraging step initiatives in children and adolescents hone in on impacting their motivation, which is often lacking.66 Research on how to encourage more physical activity among children and adolescents yields findings on how to most effectively use pedometers in combination with other treatment modalities. Organizations including the American Medical Association (AMA) and the United States Preventive Services Task Force (USPSTF), along with healthcare organizations and professionals abroad, have recommended counseling to promote increased physical activity.67 Pedometers, which are inexpensive and wearable devices, can provide children with objective ways to self-monitor their physical activity. Several studies of weight management interventions have shown that children can successfully increase their step count from baseline as part of an intervention.68 Yet these studies fail to consistently demonstrate a significant change in BMI percentile from controlled conditions.68 , 69 Staiano et al. were able to demonstate weight loss in groups of children issued pedometers as part of a 10-week, family-based weight management intervention which included physical activity, nutrition, and behavior modification (as well as money compensation).68 Those in the group issued pedometers and a step count goal increased their daily step count, as well as reduced their BMI and BMI z score significantly more than those issued a pedometer without a step goal count. Both groups saw a reduction in BMI and an increase in step count from baseline. These same children issued pedometers (with or without a step count goal) had increased subjective health and increased health-related quality of life.
Ostendorf et al. examined what leads some people to be consistent exercisers and demonstrated that weight loss maintainers weren't using continuous calorie restriction to maintain their weight.70 Instead, the weight loss maintainers had a much higher energy burn from exercise despite eating approximately the same number of calories per day as the control participants with overweight/obesity. It takes a significant time commitment to achieve the level of activity observed in these weight-loss maintainers. In a commentary on the role of exercise, Martin and Church challenge researchers to identify the physiological, psychological, and environmental factors that help people maintain weight loss through large amounts of exercise so that strategies can be implemented for future weight loss maintenance success. The benefits of exercise cannot be argued. Regular exercise can lower stress, moderate anxiety, and improve overall quality of life; however, there is great variation in these outcomes.71
Targeting the agent of change
Knowing that parents can be effective in modulating childhood obesity by serving as role models for children's eating and physical activity behavior, and knowing the positive impact parental involvement in childhood obesity efforts carries, Golan and Crowl compared targeting parents exclusively for treatment with a child-only intervention.72 Group sessions were utilized in this family-based health center intervention treatment, with parents attending 14 one-hour support and educational sessions that started as weekly, became biweekly, and then took place once every six weeks with clinical dietitians delivering the topics. Two similar groups were established, with 15 families participating in each, discussing such topics as limited responsibilities, nutrition education, eating and activity behavior modification, decreasing stimulus exposure, parental modeling, problem-solving, cognitive restructuring, and coping with resistance. Parents were encouraged to practice an authoritative parenting style as opposed to an authoritarian style.71 In authoritative parenting, “parents are both firm and supportive and then assume a leadership role in the environmental change with appropriate granting of child autonomy,” whereas in the authoritarian style, child feeding practices are controlled by the adults.73, 74, 75, 76, 77 Children in the child-only group were prescribed a 1500 calorie per day diet and participated in 30 one-hour group sessions led by a clinical dietitian. Two similar groups were held with 15 children allocated to each. The first 7 sessions were conducted weekly and the remainder were held biweekly for the period of one year.
At the end of the intervention, 35% of children in the parents-only group reached a non-obese status, compared to 14% in the child-only group. At the one-year follow-up, or one year after program termination, the weight loss in the children of the parent-only group was statistically significant compared with that of the child-only group. At the two-year follow-up, there was a mean reduction in overweight of 15% in children of the parent-only group and an increase of 2.9% in children of the child-only group. At the seven-year follow-up, both treatment conditions demonstrated substantial weight loss. However, the mean reduction of overweight status was 29% in children of the parent-only group and 20.2% in those of the child-only group; 60% of children of the parent-only group, compared with only 31% of children of the child-only group, were in a non-obese status. Seven years after program termination, two (6.6%) of the girls from the child-only group reported eating disorder symptoms (both bingeing and purging); none of the children in the parent-only group reported any eating disorder symptoms.
Family-based programs require the family to be involved. With more families having both parents in the workforce, present-day parents are less available to their children, which makes it difficult for children and adolescents waiting for them to provide a source of physical activity, to engage them in physical activity, or to accompany them to physical activity. Parents are less able to enroll in family-based weight management programs if their work schedules conflict with their ability to use free time to participate.78
Interventions targeting overweight and obese children and adolescents that require a large time commitment, a commitment from family members, travel to the intervention location, and potential cost may be poorly received and underutilized. Solutions to some of these challenges could be reached with innovative restructuring, telehealth, or a mixed model that may evolve over time.78
Behavior modification-dietary focus
Clearly there are potentially modifiable behaviors and perceptions that are associated with improving overweight and obesity. These include decreasing fast food intake, the amount of screen time, on and off dieting, depressive symptoms, low self-esteem, and weight teasing, on the one hand, as well as increasing fruit and vegetable intake through home availability and having more family meals, plus participating in moderate to vigorous physical activity.79 They are the behaviors most targeted in nutrition interventions using medical nutritional therapy (MNT) by an RD as part of a comprehensive weight management program. Increased frequency of RD visits has been associated with improved BMI outcomes in obese youth participating in these programs: “The probability of success exceeded 78% with ≥ one RD visit per month versus 43% with minimal RD exposure.”80
Both the Choose MyPlate and the 5-2-1-0 education initiatives target these potentially modifiable behaviors. In conjunction with each other, they can have a synergistic effect. Healthcare professionals can use these tools together to impact behavior change sessions and establish simple lifestyle goals.
Many adolescents engage in extreme weight control behaviors and that number has greatly increased over time, as innumerable studies have shown. One population-based survey of adolescents attending middle and high schools in 1998–99 and again in 2008–09 by Project Eating and Activity Among Teens and Young Adults assessed personal, psychological, behavioral, and socio-environmental factors believed to play a role in obesity. It showed that informing adolescents and young adults that increased dieting is associated with the persistence of obesity may help motivate adolescents to use more healthful means of weight management.81 , 82 This study reemphasizes the crucial importance of promoting healthy eating, improving the quality of the home food environment, and increasing physical activity as a means of preventing unhealthy weight loss behaviors.
The Weight Management and Healthy Living 2015 survey from the Hartman Group83 found that consumers are more interested in lasting changes and lifelong healthy eating than in crash dieting. It demonstrated that a campaign like MyPlate, with its message that individuals can achieve a healthier weight by eating more of some foods and less of others, can have utility in helping consumers make lifestyle changes that prove formidable.
Studies on energy density by B. J. Rolls suggest that decreasing energy density reduces energy intake, independent of the macro nutrient mix, because of effects on satiety.84 The indication is that diets of low energy density, which are typically rich in vegetables, fruits, legumes, and minimally processed grain products, allow individuals to consume “satisfying portions of food,” while simultaneously reducing their energy intake.84 This concept has been used in her best-selling book series Volumetrics and made into a diet plan.85
Another approach which has been used in many interventions is the “traffic light” or “stoplight diet,” which groups foods based on their nutrient quality and calorie density such that “red foods” should be consumed rarely, “yellow foods” infrequently, and “green foods” most often.27
Alt-text: Unlabelled box
It is predicated on the idea that children can learn to substitute lower energy-dense healthy foods for less healthy higher energy-dense foods and that parents can facilitate this transition via increasing access to healthy foods and decreasing access to less healthy foods by altering food purchasing and food storage habits for the family at large.86
School-based interventions
The vast number of children and adolescents in the United States attend public schools. Health and wellness policies and programs have traditionally been an important part of the daily curriculum of the majority of these schools. During the 20th century, mandatory physical education classes and nutrition programs, including the National School Lunch Program (NSLP) and the School Breakfast Program (SBP), were implemented to address problems including “food insecurity.” The current obesity epidemic among children and adolescents in the United States has stimulated the further involvement of local, state, and federal agencies in an attempt to use public schools as a venue to combat this problem. In 2004, the U.S. federal government mandated that all school districts participating in the federal meal program create a school wellness program by establishing a committee that includes individuals impacted by this problem. Legislation also required the development of nutrition standards for meals and snacks served in schools, as well as the setting up of goals for physical education. The Healthy Hunger-Free Act, passed in 2010, required school districts to measure policy implementation and make these results publicly available. What follows here is a look at the impact of some of these and other programs implemented by the schools.
Approximately 12.2 million public school students from low-income homes are provided a nutritious breakfast as part of the federal School Breakfast Program (SBP), which was established in 1966 and permanently authorized in 1975. Studies have shown that this may be associated with improved academic performance and a reduction in the number of students affected by food insecurity.87 , 88
Alt-text: Unlabelled box
The number of students participating in the SBP is less than half of those participating in the National School Lunch Program (NSLP). To increase participation in the SBP, the federal government allows school districts to serve Breakfast in the Classroom (BIC).89 In New York City, more than 70% of public-school students qualify for free or reduced-price meals. Researchers reported in 2013 on the impact of BIC on the percentage of children going without morning food, the number of locations where food was consumed, and the estimated calories each child consumed. Comparisons were made between schools that offered BIC and those that did not. Results showed that students in BIC schools were significantly more likely to eat more than once in the morning and, on average, ate an estimated 95 additional calories each morning.89 A similar study in the Philadelphia public school system, completed and published in 2018, found that BIC did not affect the combined incidence of overweight and obesity among public school students.90 However, an increasing incidence and prevalence of obesity among the students was noted.
In 2003, Arkansas became one of the first states to pass legislation to specifically address the epidemic of obesity. It required annual body mass index (BMI) screenings for all public school students, elimination of elementary school students’ access to vending machines, and creation of physical education and nutrition standards via district physical activity and nutrition committees along with input from a Child Health Advisory committee.91 , 92 A study published in 2018 assessing the effectiveness of this policy concluded that it was very unlikely that the Arkansas Act was having an impact on preventing adolescent overweight and obesity.93
California began BMI screening during the early part of the first decade of the 21st century. The state collected BMI data annually on fifth, seventh, and ninth grade students. Parental notification of the results was optional. In 2001, BMI results were sent to 35% of parents or guardians, which rose to 52% in 2008. Notification in fifth and/or seventh grade on subsequent BMI z scores, when compared to no notification, showed no significant difference in reducing the prevalence of obesity among this population of students.94
One state that offered a program that achieved better success is Massachusetts. In a pair-matched, cluster-randomized, and controlled school-based trial using a convenience sample of six public high schools, eligible 9th to 11th graders were recruited to participate in “Lookin Good Feelin Good,” a school nurse-delivered counseling intervention with one-on-one sessions conducted over two months during the school day, during non-academic classes held in the privacy of the school nurse's office.95 The 5-3-2-1-0 approach was used “to support making five behavioral changes” by utilizing cognitive behavioral techniques to facilitate changes in self-management behaviors through health knowledge and the development of positive outcome expectations, self-control, and behavioral capacity skills and self-efficacy.” Targeted adolescents completed behavioral and physiological assessments at baseline, and at 2-month and 6-month follow-ups. At two months, compared to control participants, this intervention was able to impact both increased intake of breakfast, and decreased total sugar and added sugar intake. While these particular positive results were not maintained at further follow-up, other positive outcomes were noted at 6 months when the adolescents in the intervention were more likely to drink soda less than or equal to one time a day and eat at fast food restaurants less than or equal to one time per week compared to controls. Total calorie intake and calories from fat did not change significantly between groups. Screen time and time spent in moderate to vigorous physical activity were not statistically affected. Although there was no statistically significant difference in BMI, students in the counseling intervention schools experienced favorable improvements in their BMI compared to students in the control schools.95
There are clear factors standing in the way of more successful outcomes. An online survey of U.S. public school administrators completed in 2016 indicates that rarely are evidence-based obesity prevention programs being implemented.92 Many programs focus on students’ weights rather than on healthy lifestyles. Barriers to implementation include lack of funding, time, and training.
The Johns Hopkins Evidence-Based Practice Center completed a study of 124 school-based interventions in 2013 and reported on two kinds of programs that demonstrated high evidence of effectiveness in preventing overweight and obesity in the school-aged population. These are (1) school-based programs that combined physical activity and diet with a home-based component and (2) school-based physical activity and diet interventions that were combined with a home and community component.96
Pharmacotherapy
Medication is only recommended after an unsuccessful attempt at weight loss that includes the adoption of a healthy and age-appropriate diet and an increase in daily physical activity. Presently, five medications are approved for adults in the United States for long-term management of obesity.97 , 98 Weight loss associated with these ranges from approximately 3%–9%. Side effects and adverse reactions are common with each.
For adolescents greater or equal to twelve years of age, the only prescription medication approved by the United States Food and Drug Administration (USFDA) is orlistat. No medication is approved for use in children less than twelve years of age.99, 100, 101
Alt-text: Unlabelled box
Orlistat is a lipase inhibitor that blocks the absorption of fat. It is recommended to be taken with each meal. Although it has been demonstrated to have a good safety profile, side effects can include cramping, excessive gas, oily spotting, fecal urgency, and abdominal pain. Since these side effects occur not infrequently, it can be difficult to maintain compliance with this medication. Studies have shown modest weight loss efficacy when orlistat is used along with a comprehensive weight loss program. In the largest study (n = 539) of orlistat use in combination with diet, exercise, and behavioral modification, a BMI reduction of approximately 2.4%, as compared to a placebo group, was seen over a treatment period of one year.102 The only cardiometabolic benefit seen was a small reduction in diastolic blood pressure. At the present time there are no studies reporting long-term outcomes after cessation of orlistat use.
Phentermine, a norepinephrine reuptake inhibitor, has been approved by the USFDA for short-term use for ages seventeen or older. No randomized clinical trials of phentermine have been conducted in individuals younger than seventeen years. Common side effects observed in adults using this medication include rapid heart rate, high blood pressure, anxiety, insomnia, and headache.
Metformin, a biguanide used predominately for glycemic control in individuals with Type 2 Diabetes Mellitus, has been studied for use in treatment of pediatric obesity along with lifestyle interventions.103 It does not have USFDA approval for this use in children and adolescents at the present time. One systematic review of the benefits and risks of using metformin in treating obesity in this population demonstrated a statistically significant, but very modest, reduction in BMI when combined with lifestyle interventions over the short term. No serious adverse events were reported to occur among individuals in the review. The authors concluded that metformin has not been shown to be clinically superior to other options for treating childhood obesity in the short term.
Bariatric surgery
Bariatric surgery has become an optional treatment for adolescents who are severely obese. In 2004, an Expert Panel of pediatric surgeons and pediatricians made recommendations regarding selection criteria for bariatric surgery in individuals less than eighteen years of age.104 Selection criteria included: (1) failed >6 months of organized attempts at weight management, (2) has attained or nearly attained physiologic maturity, (3) >50 BMI, or >40 BMI with an associated severe co-morbidity (i.e. sleep apnea, diabetes, hypertension), (4) demonstrates commitment to comprehensive medical and psychological evaluations both before and after surgery, (5) agrees to avoid pregnancy for at least a year, (6) is capable of and willing to adhere to nutritional guidelines post-operatively, (7) provides informed consent, (8) demonstrates decisional capacity, (9) has a supportive family environment, and (10) surgery would be done in centers that have experience with bariatric surgery and a team of specialists trained to provide long-term follow-up care of the metabolic and psychosocial requirements of the patient and family.
As an ancillary study of its observational study of adults undergoing bariatric surgery, the National Institute of Diabetes and Digestive and Kidney Diseases (NDDK) created Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS). Funding was provided to five centers in the United States to enroll at least 200 adolescent bariatric surgical patients to serve as a prospective observational cohort study aimed at assessing the clinical, epidemiological, and behavioral parameters in a select population of adolescents undergoing bariatric surgery.105 The majority of surgical procedures completed in the study were either Gastric Bypass (Roux-en Y), which creates a small gastric pouch that is connected directly to the jejunum, bypassing the upper portion of the small intestine, or the Sleeve Gastrectomy, which creates a narrow stomach pouch and removes the rest of the stomach. Research published in 2018 has shown an increasing use of vertical sleeve gastrectomy compared to other surgical procedures.106
Multiple publications from the Teen-LABS study have documented that severely obese adolescents undergoing bariatric surgery, when compared to matched adolescents undergoing medical treatment alone, had better weight loss, improvement in cardiovascular risk markers and better glycemic control.
Alt-text: Unlabelled box
The Teen-LABS researchers also reported identified risks including specific micronutrient deficiencies and the need for an acceptable rate (13%) of additional abdominal procedures.107, 108, 109, 110, 111 Overall similar findings were obtained by Olbers in a prospective nationwide study of 81 Swedish adolescents who were severely obese and underwent Roux-en Y gastric bypass.112 A single study completed by Alqalhtani in Saudi Arabia reviewed the effects of laparoscopic sleeve gastrectomy in 114 children younger than 14 years of age (mean ± SD, 11.2 ± 2.5 years). It was concluded that the procedure resulted in significant weight loss, improved growth, and a resolution of comorbidities, without mortality or significant morbidity.
Teen-LABS researchers recently compared 5-year outcomes of gastric bypass in adolescents with those of adults. They reported that adolescents and adults who underwent gastric bypass surgery had similar significant weight loss 5 years after surgery, but adolescents had a higher rate of remission of hypertension and diabetes following gastric bypass than adults. They also found that abdominal operations and short-term nutritional deficiencies were more common among adolescents than adults following surgery.113 Data from another Teen-LAB study demonstrated that joint pain, physical function, and health-related quality of life improved after bariatric surgery.114
In 2018, the American Society for Metabolic and Bariatric Surgery's (ASMBA) Pediatric Committee updated their recommendations for metabolic and bariatric surgery in children and adolescents following a comprehensive literature search. They proposed that metabolic and bariatric surgery is indicated for the following adolescents: (1) BMI >35 or 120% of the 95th percentile with clinically significant comorbidities (whichever is lower), and (2) BMI >40 or 140% of the 95th percentile (whichever is lower).
Alt-text: Unlabelled box
In addition, the patient and family should demonstrate the ability and motivation to adhere to recommended pre- and post-operative treatment.
The ASMBA's recommendations regarding contraindications for surgery included: (1) a medical correctable cause of obesity, (2) an ongoing substance abuse problem (within the preceding year), (3) inability to adhere to postoperative dietary and medication regimens as a result of a medical, psychiatric, psychosocial, or cognitive condition, and (4) current or planned pregnancy within 12–18 months of the procedure. At the same time, their guidelines stated that treatment should not be denied to those adolescents with cognitive disabilities, a history of mental illness, a history of eating disorders that are treated, immature bone growth or low Tanner Stage. Their overall conclusion was that surgery was safe and effective in adolescents, and that early intervention can reduce the risk of persistent obesity as well as end organ damage from longstanding comorbidities.115
The American Academy of Pediatrics, as well, has issued guidelines in a policy statement entitled “Pediatric Metabolic and Bariatric Surgery: Evidence, Barriers and Best Practices,” published in 2019.116 They recommended considering the following factors in deciding on surgery: (1) shared decision-making including patient, parents, medical and surgical providers, (2) BMI and comorbidity, (3) physiological, psychological, and developmental maturity, (4) ability to understand risks and benefits and be able to adhere to lifestyle modifications, (5) decision-making capacity, (6) robust family and social supports before and after the procedure. Concluding that there was no evidence to support the application of age-based eligibility, the AAP set forth the following indications for adolescent metabolic and bariatric surgery: (1) Class 2 obesity: BMI I ≥ 35 OR 120% of the 95th percentile for age and sex, whichever is lower, and with an associated clinically significant disease, including obstructive sleep apnea (AHI >5), T2DM, increased intracranial hypertension, NASH, Blount disease, SCFE, GERD, and hypertension, and (2) Class 3 obesity: BMI ≥40, or 140% of the 95th percentile for age and sex, whichever is lower without any associated comorbid conditions.
Summary
Multicomponent programs that focus on diet, behavior-change, and physical acitivity are recommended as the first line of treatment for children and adolescents who are overweight or obese. Treatment should be guided by the patient's developmental, cognitive, and pubertal stage of development. The range of clinicians and environments providing these services is extensive with most services being provided through multidisciplinary tertiary care clinics and providers. These interventions have been proven to be beneficial in achieving small short-term reductions in BMI. Presently, there is both a lack of long-term benefit and evidence that these interventions will reduce the incidence of obesity or the associated cardio-metabolic complications for children and adolescents (and adults) in the future. An almost universal consensus recommends a significant increase in research on all interventions including minority and special-needs populations with coordinated long-term follow-up. School-based programs, pharmacotherapy, and bariatric surgery are additional approaches that are increasingly being utilized for weight loss management; of these, bariatric surgery has been shown to have the greatest success, especially for those with the highest levels of obesity.
References
- 1.Barlow S.E., Dietz W. Obesity evaluation and treatment: expert committee recommendations. Pediatrics. 1998;102:1–11. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 2.Barlow S.E., the Expert Committee Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 3.Whitlock E.P., O.Connor E.A., Williams S.B. Evidence Report/Technology Assessment No.170 (Prepared by the Oregon Evidence-Based Practice Center Under Contract no.290-02-0024). AHRQ Publication No. 08-E014. Agency for Healthcare Research and Quality; Rockville, MD: 2008. Effectiveness of weight management programs in children and adolescents. [Google Scholar]
- 4.Academy of Nutrition and Dietetics. Pediatric Weight Management Evidence-Based Nutrition Practice Guideline. Chicago, IL: 2015. https://www.aneal.org/topic.cfm?menu=5296, accessed Feb. 14, 2020.
- 5.Henry B.W., Ziegler J., Parrott J.S., Handu D. Pediatric weight management evidence-based practice guidelines: components and contexts of interventions. J Acad Nutr Diet. 2018;118:1301–1308. doi: 10.1016/j.jand.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 6.https://www.uspreventiveservicestaskforce.org
- 7.Hayes J.F., Altman M., Coppock J.H. Recent updates on the efficacy of group-based treatments for pediatric obesity. Curr Cardiovasc Risk Rep. 2015;9(4) doi: 10.1007/s12170-015-0443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross M.M., Kolbash S., Cohen G.M., Skelton J.A. Multidisciplinary treatment of pediatric obesity: nutrition evaluation and management. Nutr Clin Pract. 2010;25(4):327–334. doi: 10.1177/0884533610373771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson T. Behavioural treatment of childhood and adolescent obesity. Int J Obes. 1999;23(S2) doi: 10.1038/sj.ijo.0800860. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz R.P., Hamre R., Dietz W.H. Office-based motivational interviewing to prevent childhood obesity. Arch Ped Adolesc Med. 2007;161:495. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 11.Wilfley D.E., Kolko R.P., Kass A.E. Cognitive behavioral therapy for weight management and eating disorders in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20:271–285. doi: 10.1016/j.chc.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bloom T., Sharpe L., Mullan B. A pilot evaluation of appetite-awareness training in the treatment of childhood overweight and obesity: a preliminary investigation. Int J Eat Disord. 2012;46:47–51. doi: 10.1002/eat.22041. [DOI] [PubMed] [Google Scholar]
- 13.Croker H., Cooke L., Wardle J. Appetitive behaviours of children attending obesity treatment. Appetite. 2011;57(2):525–529. doi: 10.1016/j.appet.2011.05.320. [DOI] [PubMed] [Google Scholar]
- 14.Tan C.C., Holub S.C. Children's self-regulation in eating: associations with inhibitory control and parents’ feeding behaviour. J Ped Psychol. 2010;36:340–345. doi: 10.1093/jpepsy/jsq089. [DOI] [PubMed] [Google Scholar]
- 15.Prochaska J.O., Velicer W.F. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 16.Rhee K.E. Parent readiness to change differs for overweight child dietary and physical activity behaviours. J Acad Nutr Diet. 2014;114:1601–1610. doi: 10.1016/j.jand.2014.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rhee K.E. Factors associated with parental readiness to make changes for overweight children. Pediatrics. 2005;116:e94–101. doi: 10.1542/peds.2004-2479. [DOI] [PubMed] [Google Scholar]
- 18.Patrick K., Raab F., Adams M.A. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res. 2009;11:e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen J.-.L., Guedes C.M., Lung A.E. Smartphone-based healthy weight management intervention for Chinese American adolescents: short-term efficacy and factors associated with decreased weight. J Adolesc Health. 2019;64:418. doi: 10.1016/j.jadohealth.2018.08.022. [DOI] [PubMed] [Google Scholar]
- 20.Jacobson M.S., Kohn M. Smart management of a persistently puzzling problem-adolescent obesity. J Adolesc Health. 2019;64:421–422. doi: 10.1016/j.jadohealth.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Svetkey L.P., Batch B.C., Lin P.H. Cell phone intervention for you (CITY): a randomized, controlled trial of behavioral weight loss intervention for young adults using mobile technology. Obes Silver Spring. 2015;23:2133–2141. doi: 10.1002/oby.21226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jensen C.D., Duncombe K.M., Lott M.A. An evaluation of a smartphone-assisted behavioral weight control intervention for adolescents: pilot study. JMIR Mhealth Uhealth. 2016;4:e102. doi: 10.2196/mhealth.6034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nguyen B., Shrewsbury V.A., O'Connor J. Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: the Loozit randomized controlled trial. Int J Obes Lond. 2013;37:468–472. doi: 10.1038/ijo.2012.74. [DOI] [PubMed] [Google Scholar]
- 24.Turner T., Spruijt-Metz D., Wen C.K. Prevention and treatment of pediatric obesity using mobile and wireless technologies: a systematic review. Pediatr Obes. 2015;10(6):403–409. doi: 10.1111/ijpo.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cueto V., Wang C.J., Sanders L.M. Impact of a mobile app-based health coaching and behaviour change program on participant engagement and weight status of overweight and obese children retrospective cohort study. JMIR Mhealth Uhealth. 2019;7(11):e14458. doi: 10.2196/14458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.http://www.kurbo.com
- 27.Epstein L.H., Squires S. Little, Brown; New York, NY: 1988. The Stoplight Diet For Children: An Eight-Week Program For Parents and Children. [Google Scholar]
- 28.Michie S., Richardson M., Johnston M. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 29.https://www.change.org/p/ww-formerly-weight-watchers-ww-remove-childrens-weight-loss-app-that-will-cause–countless-eating-disorders.
- 30.Southern M.S., Udall Jr J.N., Susskind R.M. Weight loss and growth velocity in obese children after very low-calorie diet, exercise, and behavioral modification. Cta Paediatr. 2000;89:1036–1043. doi: 10.1080/713794562. [DOI] [PubMed] [Google Scholar]
- 31.Figueroa-Colon R., von Almen T.K., Franklin F.A. Comparison of two hypocaloric diets in obese children. Am J Dis Child. 1993;147:160–166. doi: 10.1001/archpedi.1993.02160260050021. [DOI] [PubMed] [Google Scholar]
- 32.Patrick K., Norman G., Davilla P. Outcomes of a 12-month technology-based intervention to promote weight loss in adolescents at risk for type 2 diabetes. JDST. 2013;7(3):759–770. doi: 10.1177/193229681300700322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wen L.M. Effectiveness of childhood treatment through 20 group education sessions over 6 months. Does the attendance of a child matter? JAMA Ped. 2017;171:619–620. doi: 10.1001/jamapediatrics.2017.0658. [DOI] [PubMed] [Google Scholar]
- 34.Mohr D.C., Cuijpers P., Lehman K. Supportive accountability: a model for providing human support to enhance adherence to ehealth interventions. JMIR. 2011;13:e30. doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Janicke D.M., Steele R.G., Gayes L.A. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. J Ped Psychol. 2014;39:809–825. doi: 10.1093/jpepsy/jsu023. [DOI] [PubMed] [Google Scholar]
- 36.Elvsaas I.K.Ø., Giske L., Fure B. Multicomponent lifestyle interventions for treating overweight and obesity in children and adolescents: a systematic review and meta-analyses. J Obes. 2017;2017 doi: 10.1155/2017/5021902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hampl S., Demeule M., Eneli I. Parent perspectives on attrition from tertiary care pediatric weight management programs. Clin Pediatr. 2013;52:513–519. doi: 10.1177/0009922813482515. [DOI] [PubMed] [Google Scholar]
- 38.Cohen G.M., Irby M.B., Boles K. Telemedicine and pediatric obesity treatment: review of literature and lessons learnt. Clin Obes. 2012;2:103–111. doi: 10.1111/j.1758-8111.2012.00050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slusser W., Whitley M., Izadpanah N. Multidisciplinary pediatric obesity clinic via telemedicine within the Los Angeles metropolitan area: lessons learned. Clin Ped. 2016;55:251–259. doi: 10.1177/0009922815594359. [DOI] [PubMed] [Google Scholar]
- 40.Schoffman D.E., Turner-McGrievy G., Jones S.J. Mobile apps for pediatric obesity prevention and treatment, healthy eating, and physical activity promotion: just fun and games? Transl Behav Med. 2013;3:320–325. doi: 10.1007/s13142-013-0206-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jerome D., Baker S., Fang C.-.S. Peer teaching promotes improved knowledge and attitudes about MyPlate and SuperTracker among college students and increases self-efficacy in peer nutrition educators. Creat Educ. 2018;9:979–992. [Google Scholar]
- 42.Winter J., Boushey C.J. Workshop 1: use of technology in dietary assessment. Eur J Clin Nutr. 2009;63:S75–S77. doi: 10.1038/ejcn.2008.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention, Electronic Media Branch, Division of News and Electronic Media, Office of the Associate Director of Communication. The health ommunicator's social media toolkit 2011. https://www.cdc.gov/healthcommunication/ToolsTemplates/SocialMediaToolkit_BM.pdf.
- 44.Wireframe, L. HyperantHyperActivity Cards 2012. http://itunes.apple.com/us/app/hyperant-hyperactivity-cards/id512140657?mt=8.
- 45.Darling K.E., Sato A.F. Systematic review and meta-analysis examining the effectiveness of mobile health technologies in using self-monitoring for pediatric weight management. Child Obes. 2017;13:347–355. doi: 10.1089/chi.2017.0038. [DOI] [PubMed] [Google Scholar]
- 46.Rowe S., Alexander N., Almeida N.G. Translating the dietary guidelines for Americans 2010 to bring about real behavior change. J Am Diet Assoc. 2011;111:28–39. doi: 10.1016/j.jada.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 47.Levine E., Abbatangelo-Gray J., Mobley A. Evaluating MyPlate: an expanded framework using traditional and nontraditional metrics for assessing health communication campaigns. J Nutr Educ Behav. 2012;44:S2–12. doi: 10.1016/j.jneb.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 48.United States Department of Agriculture: Center for Nutrition Policy and Promotion. http://www.cnpp.usda.gov/Publications/MyPlate/Backgrounder.pdf.
- 49.Post R.C. A new approach to dietary guidelines communications: make MyPlate, your plate. Child Obes. 2011;7:349–351. [Google Scholar]
- 50.Nickols-Richardson S.M., Nelson S.A., Corbine M.A. Peer education in childhood and adolescence: evidence-based guidance for impactful programs. J Nutr Educ Behav. 2014;46:S196. [Google Scholar]
- 51.Topp R., Speltz J., Simenz C. Effect of a personal health and fitness course on dietary intake, physical fitness and attitudes toward wellness among college students. J Obes Weight Loss Ther. 2014;4:237. [Google Scholar]
- 52.Coker C., Shelnutt K., Headrick L. Youth understanding MyPlate improves behaviors of elementary school students. J Nutr Educ Behav. 2016;48:S22–S23. [Google Scholar]
- 53.Rogers W.V., Hart P.H., Motyka E. Impact of Let's Go! 5-2-1-0: a community-based, multisetting childhood obesity prevention program. J Pediatr Psychol. 2013;38:1010–1020. doi: 10.1093/jpepsy/jst057. [DOI] [PubMed] [Google Scholar]
- 54.Khalsa A.S., Kharofa R., Ollberding N.J. Attainment of 5-2-1-0 obesity recommendations in pre-school aged children. Prev Med Rep. 2017;8:79–87. doi: 10.1016/j.pmedr.2017.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nicely S., Miller E., del-Teso M. Parents perception of 5-2-1-0 nutrition messaging and child weight status. J Nutr Educ Behav. 2019;51:629–635. doi: 10.1016/j.jneb.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 56.Haughton C.F., Wang M.L., Lemon S.C. Racial/ethnic disparities in meeting 5-2-1-0 recommendations among children and adolescents in the United States. J Pediatr. 2016;175:188–194. doi: 10.1016/j.jpeds.2016.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.https://letsmove.obamawhitehouse.archives.gov.
- 58.Diabetes prevention program reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Duggins M., Cherven P., Carrithers J. Impact of family YMCA membership on childhood obesity: a randomized controlled effectiveness trial. J Am Board Fam Med. 2010;23:323–333. doi: 10.3122/jabfm.2010.03.080266. [DOI] [PubMed] [Google Scholar]
- 60.Bai Y., Saint-Maurice P.F., Welk G.J. The longitudinal impact of NFL PLAY 60 programming on youth aerobic capacity and BMI. Am J Prev Med. 2017;52:311–323. doi: 10.1016/j.amepre.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 61.Office of the United States Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed. Washington, D.C., 2018.
- 62.Leblanc A.G., Chaput J.-.P., McFarlane A. Active video games and health indicators in children and youth: a systematic review. PLoS ONE. 2013;8(6) doi: 10.1371/journal.pone.00065351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rose T., Barker M., Jacob C.M. A systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. J Adolesc Health. 2017;61:669–677. doi: 10.1016/j.jadohealth.2017.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xian Y., Xu H., Xu H. An initial evaluation of the impact of Pokémon GO on physical activity. J Am Heart Assoc. 2017;6(5) doi: 10.1161/jaha.116.005341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Texas A&M University . ScienceDaily; 2016. Health Benefits of Pokémon Go.www.sciencedaily.com/releases/2016/07/160715181715.htm [Google Scholar]
- 66.Brown C.L., Skelton J.A., Perrin E.M. Behaviors and motivations for weight loss in children and adolescents. Obesity. 2015;24:446–452. doi: 10.1002/oby.21370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Piercy K.L., Troiano R.P., Ballard R.M. The physical activity guidelines for Americans. JAMA. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Staiano A.E., Beyl R.A., Hsia D.S. Step tracking with goals increases children's weight loss in behavioral intervention. Child Obes. 2017;13:283–290. doi: 10.1089/chi.2017.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ameryoun A., Sanaeinasab H., Saffari M. Impact of game-based health promotion programs on body mass index in overweight/obese children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Child Obes. 2018;14:67–80. doi: 10.1089/chi.2017.0250. [DOI] [PubMed] [Google Scholar]
- 70.Ostenddorf D.M., Caldwell A.E., Creasy S.A. Physical activity energy expenditure and total daily energy expenditure in successful weight loss maintainers. Obesity. 2019;27:496–504. doi: 10.1002/oby.22373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martin C.K., Church T.S., Thompson A.M. Exercise dose and quality of life. Arch Intern Med. 2009;169:269. doi: 10.1001/archinternmed.2008.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Golan M., Crow S. Targeting Parents exclusively in the treatment of childhood obesity: long-term results. Obes Res. 2004;12:357–361. doi: 10.1038/oby.2004.45. [DOI] [PubMed] [Google Scholar]
- 73.Kirschenbaum D.S., Harris E.S., Tomarken A.J. Effects of parental involvement in behavioral weight loss therapy for preadolescents. Behav Ther. 1984;15:485–500. [Google Scholar]
- 74.Golan M., Weizman A. Familial approach to the treatment of childhood obesity: conceptual model. J Nutr Ed. 2001;33:102–107. doi: 10.1016/s1499-4046(06)60173-5. [DOI] [PubMed] [Google Scholar]
- 75.Kremers S.P., Brug J., Vries H.D. Parenting style and adolescent fruit consumption. Appetite. 2003;41:43–50. doi: 10.1016/s0195-6663(03)00038-2. [DOI] [PubMed] [Google Scholar]
- 76.Satter E. Internal regulation and the evolution of normal growth as the basis for prevention of obesity in children. J Am Diet Assoc. 1996;96:860–864. doi: 10.1016/s0002-8223(96)00237-4. [DOI] [PubMed] [Google Scholar]
- 77.Schmitz K.H., Lytle L.A., Phillips G.A. Psychosocial correlates of physical activity and sedentary leisure habits in young adolescents: the teens eating for energy and nutrition at school study. Prev Med. 2002;34:266–278. doi: 10.1006/pmed.2001.0982. [DOI] [PubMed] [Google Scholar]
- 78.Coates T.J., Killen J.D., Slinkard L.A. Parent participation in a treatment program for overweight adolescents. Int J Eat Disord. 1982;1:37–48. [Google Scholar]
- 79.Watts A.W., Loth K.A., Peterson C. Characteristics of a favorable weight status change from adolescence to young adulthood. J Adolesc Health. 2016;58:403–409. doi: 10.1016/j.jadohealth.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kirk S., Woo W.G., Siegel R.M. Increased frequency of dietitian visits is associated with improved body mass index outcomes in obese youth participating in a comprehensive pediatric weight management program. Child Obes. 2015;11:202–208. doi: 10.1089/chi.2014.0079. [DOI] [PubMed] [Google Scholar]
- 81.Neumark-Sztainer D., Wall M., Story M. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. J Adolesc Health. 2012;50:80–86. doi: 10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Quick V., Wall M., Larson N. Personal, behavioral and socioenvironmental predictors of overweight incidence in young adults: 10-year longitudinal findings. Int J Behav Nutr Phys Act. 2013;10:37. doi: 10.1186/1479-5868-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.http://store.hartman-group.com/content/weight-management-and-healthy-living-2015-report-overview.pdf.
- 84.Rolls B.J. The role of energy density in the overconsumption of fat. J Nutr. 2000;130:268S. doi: 10.1093/jn/130.2.268S. [DOI] [PubMed] [Google Scholar]
- 85.https://www.diet.com/g/vlumetrics.
- 86.Epstein L.H., Paluch R.A., Beecher M.D. Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity. 2008;16:318–326. doi: 10.1038/oby.2007.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Frisvold D.E. Nutrition and cognitive achievement: an evaluation of the school breakfast program. J Public Econ. 2015;124:91–104. doi: 10.1016/j.jpubeco.2014.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bartfeld J.S., Ahn H.M. The school breakfast program strengthens household food security among low-income households with elementary school children. J Nutr. 2011;14:470–475. doi: 10.3945/jn.110.130823. [DOI] [PubMed] [Google Scholar]
- 89.Van Wye G., Seoh H., Adjoian T. Evaluation of the New York City breakfast in the classroom program. Am J Public Health. 2013;103:e59–e64. doi: 10.2105/AJPH.2013.301470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Polonsky HM, Bauer KW, Fisher JO, et al. Effect of a breakfast in the classroom initiative on obesity in urban school-aged children: a cluster randomized clinical trial. JAMA Pediatr. doi:10.1001/jamapediatrics.2018.5531. [DOI] [PMC free article] [PubMed]
- 91.Ickovics J.R., Duffany K.C., Shebl F.M. Implementing school-based policies to prevent obesity: cluster randomized trial. Am J Prev Med. 2019;56:e1–ell. doi: 10.1016/j.amepre.2018.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kenney E.L., Wintner S., Less R.M. Obesity preventions interventions in US public school: are schools using programs that promote weight stigma. Prev Chronic Dis. 2017;14:e142. doi: 10.5888/pcd14.160605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gee K.A. Leveraging the public school system to combat adolescent obesity: the limits of Arkansas's statewide policy initiative. J Adolesc Health. 2018;63:561–567. doi: 10.1016/j.jadohealth.2018.06.006. 88. [DOI] [PubMed] [Google Scholar]
- 94.Madsen K.A. School-based body mass index screening and patient notification: a statewide natural experiment. Arch Pediatr Adol Med. 2011;165:987–992. doi: 10.1001/archpediatrics.2011.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pbert L., Druker S., Gapinski M.A. A school nurse-delivered intervention for overweight and obese adolescents. J School Health. 2013;83:182–193. doi: 10.1111/josh.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang Y., Wu Y., Wilson R.F. Johns Hopkins University Evidence-Based Practice Center; Rockville, MD: 2013. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis. [PubMed] [Google Scholar]
- 97.Khera R., Murad M.H., Chandar A. Association of pharmacological treatment for obesity with weight loss and adverse side effects: a systematic review and meta-analysis. JAMA. 2016;315:2424–2434. doi: 10.1001/jama.2016.7602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sirvastava G., Foz C.F., Kelly A.S. Clinical considerations regarding the use of obesity pharmacotherapy in adolescents with obesity. Obesity. 2019;27:190–204. doi: 10.1002/oby.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Whitlock E.P., O'Connor E.A., Williams S.B. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125:e396–e418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 100.Kelly A.S., Barlow S.E., Rao G. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128:1689–1712. doi: 10.1161/CIR.0b013e3182a5cfb3. [DOI] [PubMed] [Google Scholar]
- 101.Cardel M.H., Jasterboff A.M., Kelly A.S. Treatment of adolescent obesity in 2020. JAMA. 2019;322:1707–1708. doi: 10.1001/jama.2019.14725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chanoine J.P., Hampl S., Jensen C. Effect of orlistat on weight and body composition in obese adolescents. JAMA. 2005;293:2873–2883. doi: 10.1001/jama.293.23.2873. [DOI] [PubMed] [Google Scholar]
- 103.McDonagh M.S., Selph S., Ozpinar A. Systematic review of the benefits and risks of metformin in treating obesity in children aged 18 years and younger. JAMA Pediatr. 2014;168:178–184. doi: 10.1001/jamapediatrics.2013.4200. [DOI] [PubMed] [Google Scholar]
- 104.Inge T.H., Krebs N.F., Garcia V.F. Bariatric surgery for severely overweight adolescents: concerns and recommendations. Pediatrics. 2004;114:217–223. doi: 10.1542/peds.114.1.217. [DOI] [PubMed] [Google Scholar]
- 105.Inge T.H., Zeller M., Hermon C. Teen-longitudinal assessment of bariatric surgery: methodological features of the first prospective multicenter study of adolescent bariatric surgery. J Pediatr Surg. 2007;42:1969–1971. doi: 10.1016/j.jpedsurg.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Griggs C.L., Perez N.P., Goldstone R.N. National trends in the use of metabolic and bariatric surgery among pediatric patients with severe obesity. JAMA Pediatr. 2018;172:1191–1192. doi: 10.1001/jamapediatrics.2018.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ryder J.R., Edwards N.M., Gupta R. Changes in functional mobility and musculoskeletal pain after bariatric surgery in teens with severe obesity: teen-longitudinal assessment of bariatric surgery (Teen-LABS) study. JAMA Pediatr. 2016;170:871–877. doi: 10.1001/jamapediatrics.2016.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Inge T.H., Zeller M., Jenkins T.M. Perioperative outcomes of adolescents undergoing bariatric surgery: the teen-longitudinal assessment of bariatric surgery (Teen-LABS) study. JAMA Pediatr. 2014;168:47–53. doi: 10.1001/jamapediatrics.2013.4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Inge T.H., Courcoulas A.P., Jenkins T.M. Weight loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374:113–123. doi: 10.1056/NEJMoa1506699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Inge T.H., Laffel L.M., Jenkins T.M. Comparison of surgical and medical therapy for type 2 diabetes in severely obese adolescents. JAMA Pediatr. 2018;172:452–460. doi: 10.1001/jamapediatrics.2017.5763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Michalsky M.P., Inge T.H., Jenkins T.M. Cardiovascular risk factors after adolescent bariatric surgery. Pediatrics. 2018;141:1–11. doi: 10.1542/peds.2017-2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Obers T., Beamish A.J., Gronowitz E. Laparoscopic Roux-en Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year Swedish nationwide study. Lancet Diabetes Endocrinol. 2017;5:174–183. doi: 10.1016/S2213-8587(16)30424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Inge T.H., Courcoulas A.P., Jenkins T.M. Five-year outcomes of gastric bypass in adolescents as compared with adults. N Engl J Med. 2019;380:2136–2145. doi: 10.1056/NEJMoa1813909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bout-Tabaku S., Gupta R., Jenkins T.M. Musculoskeletal pain, physical function, and quality of life after bariatric surgery. Pediatrics. 2019;144 doi: 10.1542/peds.2019-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pratt J.S., Browne A., Browne N.T. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14:882–901. doi: 10.1016/j.soard.2018.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Armstrong S.C., Bolling C.F., Michalsky M.P. Pediatric metabolic and bariatric surgery: evidence, barriers, and best practices. Pediatrics. 2019;144 doi: 10.1542/peds.2019-3223. [DOI] [PubMed] [Google Scholar]