Abstract
Despite the fact that universal inclusion is a basic principle of the Sustainable Development Goals, the inclusion of persons with disabilities in humanitarian interventions and development policies remains elusive. Persons with disabilities face high risks of poverty, poor nutrition, limited inclusion in labor markets and poor mental health as a result. Stigma is likely to play a negative role in this regard and yet, no study has investigated the impact of stigma on depression and self-esteem of persons with disabilities. To address this gap in the literature, we conducted in June 2017 a random sample disability case control household study in Soweto, a township in Johannesburg, South Africa. Using propensity score analysis and structural equation modeling, we investigated the relationship between disability, stigma, depression and self-esteem controlling for socioeconomic covariates. Our main empirical results showed that stigma significantly mediates the association between disability and higher depression on the one hand and between disability and lower self-esteem on the other. This mediating effect exists even after controlling for age, gender, marital status, education, employment and wealth. We also found strong direct associations between disability and depressive mood, somatic indicators and negative feelings such as unhappiness and low self-esteem. Unemployment aggravates depression and low self-esteem while low education worsens self-esteem only. In addition, depression exacerbates low self-esteem. Both unemployment and low education are more common among persons with disabilities aggravating the disability, depression, poor self-esteem nexus. Similarly, persons with disabilities who are more likely to be depressed are also at higher risk of low self-esteem. These results point to a vicious reinforcing circle of exclusion from society, despair and self-deprecation, which could prove difficult to break. Substantial psycho-social support and anti-stigma policies anchored in local cultural values, engaging persons with disabilities and their communities, are required to break this vicious circle.
Keywords: Depression, Disability, Middle income country, Propensity score matching, Self-esteem, Stigma, Soweto, South Africa, Structural equation modelling
Highlights
-
•
Disability is associated with high depression and low self-esteem in South Africa.
-
•
Stigma partially mediates links between disability, depression and self-esteem.
-
•
Unemployment exacerbates depression and low self-esteem.
-
•
Education increases self-esteem.
-
•
Anti-stigma policies are needed to achieve Sustainable Development Goals for all.
Credit author statement
Jean-Francois Trani, Conceptualization, Methodology, Software, Investigation, Writing - original draft, Formal analysis, Validation, Writing - review & editing, Funding acquisition, Supervision. Jacqueline Moodley, Conceptualization, Methodology, Investigation, Writing - review & editing, Funding acquisition, Project administration. Paul Anand, Conceptualization, Writing - review & editing. Lauren Graham, Conceptualization, Writing-reviewing and editing. May Thu Thu Maw, Software, Formal analysis, Visualization.
1. Introduction
Despite the central, transformative promise of “Leave No One Behind” of the UN's 2030 Agenda for Sustainable Development and its Sustainable Development Goals (SDGs), the inclusion of persons with disabilities as a priority group for all humanitarian interventions and development policies and programs remains, largely, a work in progress. In 2018 it was estimated that one billion people live with some form of disability, and that 80% of these individuals live in low- or middle-income countries (World Health Organization and World Bank 2011), where they face more severe hardship than any other group of individuals (United Nations Department of Economic and Social Affairs 2018). Five years into the SDGs, little has been achieved in terms of the inclusion of persons with disabilities. Such individuals still face particularly high rates of poverty (SDG1) and hunger (SDG2). In addition and related, they experience high levels of unemployment or work in precarious, part time jobs making it almost impossible to earn a decent income (SDG8) (Lamichhane and Okubo 2014; Mizunoya and Mitra 2013).
Why is the achievement of these fundamental development goals so challenging for persons with disabilities? Scholars and disability activists have argued that the mere fact of physical difference is not the central issue as the medical model suggests, rather there are numerous additional social, economic and environmental barriers that compound the circumstances of living with a disability (Pfeiffer 2001). As a result, a growing body of literature has sought to understand why and how these barriers serve to deny the opportunities and rights of persons with disabilities (Abberley 1987; Oliver 1996). According to the social model of disability, social barriers are not merely negative attitudes of members of society towards persons with disabilities but occur within broader structural contexts shaped and defined by policies as well as cultural, social and religious norms that also delineate stigma within a given context (Oliver 1990).
This study employs the definition of stigma proposed by Link and Phelan (2001), which describes stigma as the relationship between negative attitudes or prejudice resulting from negative stereotypes of society fueled by cultural beliefs towards a discriminated group. Public stigma, prejudice and discrimination voiced and practiced by the general population (Corrigan 2004) have been shown to result in social exclusion by precluding social interaction (Buljevac et al., 2012; Meininger 2010; Reidpath et al., 2005) and access to treatment (Halter 2004). Furthermore, it contributes to negative health outcomes for members of stigmatized groups (Evans-Lacko et al., 2012; Hatzenbuehler et al., 2014; Lukachko et al., 2014; Miller et al., 2011).
An emerging body of literature has shown that persons with disabilities are facing public stigma in various spheres of life, reducing what Amartya Sen and others refer to as “capabilities”. Capabilities are the practical “opportunities” that a person is free to pursue to enhance their well-being (Sen 1992 p.7; Anand et al., 2009). According to the capability approach (CA), disability can be conceptualized as deprivation of capabilities due to poor capacities to convert resources into valued activities or states (’conversion factors' such as the impairment itself). Additionally, disabilities can arise from a scarcity of assets and resources, as well as negative environmental circumstances resulting in a reduced quality of life (Burchardt 2004; Mitra 2006; Tellez et al., 2016). Stigma has the potential to reduce individuals’ capabilities and disempower them by reducing their agency – that is an ability “to choose between different styles and ways of living” (Sen, 2009 p. 227). Stigma has been found to compromise friendships and intimate relationships (Green 2003), constrain healthcare use (Maulik and Darmstadt 2007) (Trani et al., 2017), limit access to education (Cooney et al., 2006; Bakhshi et al., 2018) and confine opportunities for employment (Trani et al., 2018). Often, friends and particularly family members of stigmatized individuals are faced with stigma by association resulting in avoiding contact with or hiding the stigmatized individual (Pryor and Reeder 2011). Finally, structural stigma, defined by Pryor and Reeder (2015) as institutions and mainstream ideological paradigms perpetuating and enforcing public stigma, result in further exclusion from the public sphere (Pryor and Reeder, 2015).
Stigma may negatively influence mental wellbeing. A substantial body of literature exists about the ways in which the stigma of conditions such as schizophrenia, mood disorders, substance disorders or HIV-AIDS and self-stigma combine to create depression, demoralization on one hand and lower self-esteem on the other (Livingston and Boyd 2010; Mills et al., 2019; Pellet et al., 2019). Furthermore, it has been shown that depression and self-esteem are directly connected (Mruk 2006). In particular, it has been shown that self-stigma, the expression of the internalization of prejudice and discrimination manifested in the general population, is detrimental to persons with mental illness particularly when it affects individuals who possess other ‘discrediting’ attributes such as gender, cast, ethnicity, race, sexual orientation or religion (Corrigan et al., 2005; Rüsch et al., 2006). Self-stigma results in a higher risk of depression and lower self-esteem as people anticipate, endorse and internalize stereotypes and apply negative beliefs to themselves. The feeling of shame about their condition increases and can be prominent when seeking external assistance such as medical treatment (Conner et al., 2010; Corrigan et al., 2006; Luoma et al., 2012). Indeed, the behavioral consequences of such feelings can be sufficiently powerful that some programs to treat mental disorders may even unintentionally use and promote self-stigma, for instance in the case of substance abuse disorders (Corrigan et al., 2017). Corrigan et al., (2017) mentioned for instance the ‘Twelve step’ program that encourages individuals having substance disorders to admit their incapacity to control their addiction.
Despite the negative consequences of stigma, there is scant research into disability-related stigma and its association with depression and self-esteem. Research is often limited to some types of disabilities such as developmental or learning disabilities and focuses on High Income Countries (Ali et al., 2015b; Chan et al., 2017; Zhang et al., 2014). Studies in Low or Middle Income Countries (LMICs) have investigated subjective well-being or quality of life of persons with disabilities (Uppal 2006), or the public stigma of disability and access to services (Mulumba et al., 2014; Parsons et al., 2015). Very few studies have engaged with disability, stigma and mental distress such as anxiety and depression (Trani et al., 2016) and none have sought to investigate the connection to self-esteem. Similarly, no studies have investigated the connection between depression associated with a disability and public stigma.
In South Africa, structural stigma (Hatzenbuehler and Link 2014) has been shown to be associated with intellectual disability and aggravated by ethnicity (being Black South African compared to White) as well as socioeconomic status (Ali et al., 2015a). A recent small-scale study also demonstrated how stigma negatively affected intimate partner relationships, creating the exploitation and dehumanization of women with disabilities (van der Heijden et al., 2019a; Van der Heijden et al., 2019b). Elsewhere, Hussey et al. (2017) established that a major barrier to the implementation of the health and rehabilitation articles of the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD) in South Africa was stigma associated with disabilities (Hussey et al., 2017). In addition, it has been found that neglect and a lack of respect for various rights —to education, healthcare, employment, voting and security— resulted from stigma on the basis of impairment for persons with psychosocial disabilities (Mahomed 2016). Stigma has even been found to explain the unwillingness of non-disabled people to engage romantically with persons with physical disabilities (Hunt et al., 2018). However, no study to date of which we are aware has investigated the impact of stigma on depression and self-esteem of persons with disabilities. This research lacuna is alarming given the potential harm to persons with disabilities, in the form of depression and low self-esteem, resulting from discrimination.
In order to address this research gap, we conducted a household survey in June 2017 in Thulani and Doornkop, Soweto —two poor townships on the outskirts of the city of Johannesburg, South Africa— to measure a mediating model between disability, stigma, depression and self-esteem using validated and reliable scales. We hypothesized that disability is negatively associated with self-esteem and positively associated with depression. Additionally, we tested a mediation model that examined whether discrimination and stigma accounts for the hypothesized relationship between disability, depression and anxiety.
This paper contributes to the literature by (i) reporting on a new household survey of persons with disabilities (n = 191) and matched controls (n = 196) to understand connections between stigma, depression and self-esteem using validated and reliable scales in a developing country context; (ii) providing a test for the hypothesis that low self-esteem is connected to depression in persons with disabilities; (iii) providing a test for a mediation model to investigate whether discrimination and stigma contribute to the hypothesized relations between disability and depression and anxiety; and (iv) providing insight into the importance of public policies and programs addressing the stigma of disability to improve mental well-being of persons with disabilities.
2. Methods
2.1. Study design and setting
Between June 1st and 31st of 2017, we carried out a two-stage cluster case control survey. At the first stage, we randomly selected 40 census enumeration areas (CEA) out of a total of 73 in two wards of Soweto, Thulani and Doornkop, in Johannesburg. We calculated a sample size of 1915 households considering an estimated rate of prevalence of severe disability of 5% or less (World Health Organization and World Bank 2011), a severe stigma score estimated at 10%, a limit of statistical significance = 0.01 (with 99% confidence intervals), an average household size of 4, a 5% precision, an estimated design effect of 2 and a 20% non-response among households. At stage two, we randomly selected 50 households in each enumeration area for a total of 2000 households. Households were selected by rotating a pointer at the GPS centre of the CEA to identify the first household and looking for the next nearest front door —the closest front door to the front door of the household just visited— and for each of the remaining 49 households. 84% of heads of household agreed to participate in the study. In the resultant 1677 participant households, we interviewed all heads of household to identify adults for disability using the Washington Group Short Set of Questions on Disability (Madans et al., 2011). We identified 191 adults over 18 years old with a disability using a cutoff criterion as explained below (p.8) and 196 adults without a disability, matching in age (±5 years), gender and place of residence (living within the same block in a household without anyone having a disability) (See Fig. 1 ).
Fig. 1.
Household case control study sampling stages.
2.2. Data collection
We interviewed heads of household about demographic and socioeconomic characteristics of all household members, disability status, household living standards, income and social grants. In addition, persons with disabilities and the matched controls were interviewed about capabilities (Sen 1999), health and rehabilitation, depression and self-esteem, stigma, labor market participation and social cohesion. Disability, stigma, depression and self-esteem scales have already been used in South Africa but were nevertheless tested and validated for content in Soweto. All scales were translated and back translated in Zulu by translators working independently. Fieldworkers were trained over a two-day period and worked closely with field supervisors and two of the authors to assure the quality of the data.
2.3. Measures
2.3.1. Exposure: disability
A binary exposure variable was created based on disability identified using the Washington Group on Disability Statistics (WG) short set disability measure for censuses and surveys (Madans et al., 2011). The WG short questionnaire has already been used and validated in South Africa (Eide et al., 2015; Schneider 2009). It is composed of six questions about difficulties (seeing, hearing, walking or climbing, remembering or concentrating, self-care such as washing all over or dressing and communicating for instance understanding or being understood by others) associated with a health problem. Response categories are: “no - no difficulty”; “yes - some difficulty”; “yes - a lot of difficulty”; “yes - cannot do at all”. Disability was reported by the head of household for all household members. Information was corroborated with the same questions asked directly to the person with disabilities or a caregiver in cases where difficulties in communication existed. Following the WG experts’ approach, we considered individuals as having a disability if they selected “yes - a lot of difficulty” or “yes - cannot do at all” on any of the six questions. Individuals who selected “no - no difficulty” or “yes - some difficulty” were considered non-disabled.
2.3.2. Mediator: discrimination and stigma
Discrimination and stigma were measured using the psychometrically validated 22-item Unfair treatment subscale of the 35-item Discrimination and Stigma Scale (DISC) (Brohan et al., 2013). We looked —yet could not find at the time of the study— a stigma scale more specifically addressing disability, possibly in South Africa or in a Southern African context. Unfortunately, to the best of our knowledge, there were no reliable, validated disability stigma scales measuring discrimination (Palad et al., 2016). In previous research, we used locally developed stigma scales (Trani et al., 2016). For this study, we adopted the DISC since it showed good construct validity and provided good evidence of cross-cultural validity in a study in Nigeria (Oshodi et al., 2014). Nigeria is certainly a different African country from South Africa but shares some similar socioeconomic patterns in terms of economic disparities, level of development, ethnic and racial diversities. We adapted the DISC and conducted content and face validity tests in Soweto.
The DISC focuses on issues of behaviors and discrimination faced by persons with disabilities in various areas of life such as relationships (with friends, neighbors, intimate partner), housing, education, marriage, work, public transportation, welfare benefits, religious practices, social life, interaction with police, interaction with healthcare professionals, parenting, and personal safety (such as being a victim of verbal abuse, physical abuse and assault). To check for face validity, each respondent was asked to provide an example of unfair treatment for each of the DISC items. They would also provide a rating of unfair treatment they eventually endured in each area of life on a four-point Likert scale (not at all, a little, moderately, and a lot). A “not applicable” choice was offered in case an item happened to be irrelevant for a respondent (for instance if a respondent never started a family, the item “Have you been treated unfairly in starting a family or having children?” would be irrelevant to them). The total score —between 22 and 88— is calculated by simply adding the 22 items. For the present study, we also tested the mean score from 1 to 4 by dividing the total score by the number of items. We followed the strategy for the analysis elaborated by Brohan et al. (2013) following a previous approach used with the Internalized Stigma of Mental Illness (ISMI) scale (Brohan et al., 2013; Brohan et al., 2010). The approach fixes a reference to the DISC Unfair treatment subscale midpoint of 1.5. Four categories are therefore determined to interpret the DISC mean scores: 0 to 1 is minimal discrimination; 1–1.5 is low discrimination; 1.5–2 is moderate discrimination; and 2 and above is considered high discrimination. We further calculated and tested a dummy variable composed of two categories of low (score below 2) and high stigma (score between 2 and 4) for sensitivity analysis. The internal consistency measured by Cronbach's alpha was 0.87 indicating an overall very good fit in our study.
2.3.3. Outcome: depression and self-esteem
Intensity of depression was measured using the Center for Epidemiologic Studies Depression Scale Revised (CES-D-R 10), a self-report measure composed of 10 items assessing symptoms of depression in the last week. The CES-D-R 10 was derived from the original 20-item CES-D (Radloff 1977). It has been revised to better capture general dysphoria and reflects primary symptoms of a major depressive episode (Eaton et al., 2004). Later, the instrument was validated for the measurement of depression (Van Dam and Earleywine 2011). The CES-D-R 10 has been validated in South Africa among Zulu, Xhosa and Afrikaans populations (Baron et al., 2017). The CES-D-R 10 is constituted of three items on depressive mood (feel depressed, fearful and lonely), five items on somatic complaints (bothered by things, trouble with focus, trouble with activity, restless sleep and lack of energy) and two on positive feelings (positive feeling for the future and happiness). Each item ranges from “rarely or none of the time” (score of 0) to “all of the time” (score of 3). The total score —between 0 and 30— is calculated by adding the 10 items. Any respondent scoring 10 or above is considered depressed with the intensity of depression rising with the score. The internal consistency in the present study was 0.79.
Self-esteem was assessed using the Rosenberg's 10-item Self-Esteem Scale composed of five positive and five negative questions about feelings of self-worth. The scale constitutes an uni-dimensional factor structure which was easy to use, quick to administer and has been validated in many cultural contexts including South Africa (Baranik et al., 2008; Corwyn 2000; Makhubela and Mashegoane 2017; Westaway et al., 2015). All items were answered using a 4-point Likert scale design ranging from “strongly agree” to “strongly disagree”. For the present study, the internal consistency was 0.76.
2.3.4. Potential confounders: individual characteristics
We included a series of covariates in the present study: (i) the participants' socio-demographic characteristics, including gender (male; female), age (continuous) and marital status (married including living with partner; or not married combining separated or widow and single or never married) (Parnes et al., 2009); (ii) aspects of socioeconomic background including participants' level of education (no schooling; or schooling combining different levels of education: lower than secondary, secondary schooling and higher schooling), participants’ employment status (employed including self-employed; or unemployed including people actually not working but actively looking for a job and immediately available to work but also people outside the labor force such as young people, older adults and adults busy with household chores not looking for a job) and level of wealth measured by a welfare index (Amuri et al., 2011). The welfare index was calculated using polychoric principal component analysis (PCA) based on durable goods owned by the household and food security (Kolenikov and Angeles 2009). Durable goods included type of dwelling (house in bricks vs. informal dwelling), water source (piped water in dwelling vs. no piped water outside or public tap), energy for cooking, heating and lighting (electric and gas vs. paraffin, wood or coal), type of toilet (own flush toilet inside the dwelling vs. own flush outside or pit latrine). Level of food insecurity was composed of four levels (always enough food, sometimes not enough, often not enough or always not enough). The index is constructed using the first factor of the PCA, which explained 69% of the total variance indicating the robustness of the one-factor structure. We compare the wealthier 20% to the rest of the population in our models. We controlled for the effect of these covariates on the exposure-mediator confounding, mediator-outcome confounding and exposure-outcome confounding using sensitivity analysis techniques to explore and rule out alternative assumptions and biases (Vanderweele 2010; Vanderweele and Chiba 2014).
2.4. Statistical analysis
Descriptive analysis was conducted in Stata 15 to profile the sample and to provide frequencies, means, and standard deviations among the study variables.
Despite having matched persons with and without disabilities in the field, we observed substantial differences in the underlying characteristics of the two groups of persons with disabilities and controls as well as between groups expressing high and low stigma. To further ensure that comparisons were made on similar individuals, we used propensity score matching (PSM) to evenly balance the distributions of observable confounding factors across the groups of individuals with and without disabilities for the associations between disability and stigma, depression and self-esteem as well as between stigma and depression and stigma and self-esteem (Austin 2011; Rosenbaum and Rubin 1983). The method does not impose a specific functional form assumption on how disability results in stigma nor does it need any specific identification on the model errors (Blundell and Costa Dias 2002).
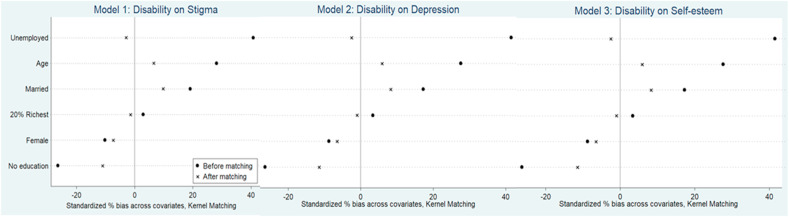
We estimated a propensity score for each individual representing their probability of being stigmatized, depressed or having a low self-esteem, conditional on a set of observed covariates that are recognized to predict both treatment assignment and disability status (Models 1, 2 and 3). We included the following covariates —age, gender, marital status, level of education, employment status and welfare status— as defined above. These were expected to be balanced between persons with and without disabilities in each model (Austin 2010). Similarly, we estimated a propensity score for the probability to be depressed and have a low self-esteem when exposed to stigma, conditional on the same set of covariates with the addition of the disability status (Models 4 and 5). We then matched recipients and non-recipients on the propensity score using the Gaussian kernel matching method with 0.06 bandwidths to minimize the mean squared error of the estimated treatment effect which maximizes use of information for matches with closest match while minimizing information from those which are further away from each other. We reproduced the matching process using four other matching algorithms: nearest neighbor matching (with a 1:1 ratio, and a 0.20 caliper), radius matching with and without replacement and local linear matching (Austin 2010; Caliendo and Kopeinig 2008; Stuart et al., 2009). The balancing tests show that propensity score matching using the Gaussian kernel estimator removes most of the bias between the treatment and non-treatment groups: In all analyses, Rubin's B is below 25%, Rubin's R is within 0.5 and 2 and the percentage bias is below 10% for all covariates (Fig. 2, Fig. 3 ) (Rubin 2001). We interpreted any remaining difference in the outcomes as the average treatment effect on the treated (ATT), the group of persons with disabilities.
Fig. 2.
Balance results of the propensity-score matching for the sample for Model 1: Disability on Stigma, Model 2: Disability on Depression and Model 3: Disability on Self-esteem, Model 4. Stigma on Depression and Model 5. Stigma on Self-esteem.
Fig. 3.
Balance results of the propensity-score matching for the sample for Model 4. Stigma on Depression and Model 5. Stigma on Self-esteem.
Formally, we defined where i represents individual and X represents a vector of confounders, T represents an indicator variable denoting the treatment assignment —having a disability or not in Models 1,2,3 and facing stigma with a score above 2 or not in Models 4 and 5. equals zero () for control subjects and one () for treated subjects. Yi (0) represents the potential outcome of the control group, and Yi (1) of the treated. For each subject, the effect of treatment is , the average treatment effect conditional on the covariates (Xi = x) for the whole sample will be E[] while the specific average treatment effect of the treated (ATT) will be defined as E[{[] –[]}|T = 1] (Imbens 2004, 2015).
Stata 15 was used to conduct the PSM analyses (Stuart et al., 2009). In order to assess the robustness and validity of our model results, we conducted sensitivity analysis in which we modified the stratification of the main socioeconomic characteristics: education in three categories (no schooling, lower than secondary, secondary schooling and higher), welfare index in three categories (20% poorest, 60% middle, 20% richest). We also tested whether our results were sensitive to an alternative specification of the outcome variable, where stigma, depression and self-esteem were dummy instead of continuous variables.
Finally, structural equation modeling (SEM) was used to examine the possibility of a mediation and direct effect of the main model of disability on depression and self-esteem. Structural equation modeling is effective in modeling the possible mediation effect of stigma between disability and depression and self-esteem and effectively addresses the risk of bias from measurement error (Robins and Greenland 1992; Vansteelandt 2009). Mplus version 8.2 was used to conduct the SEM analyses (Muthén et al., 2018).
We fit a series of structural equation models using the maximum likelihood procedure χ2 test as well as the comparative fit index (CFI significant for >0.95), the root mean square error of approximation (RMSEA significant at <0.05) and the Tucker-Lewis Index (TLI significant for >0.95) (Hu and Bentler 1999; Steiger 2007). We tested the hypothesis of mediation taking a series of steps. First, we used the maximum likelihood parameter estimates with conventional standard errors and chi-square test statistic (ML) in Mplus which allows for the estimation of standard errors for indirect effects with both continuous mediators and categorical outcomes. It provides a statistical test for mediation in a path analysis, that estimates a system of equations without latent variables but in which all of the variables were observed (Muthén et al., 2018). Second, we sequentially tested the proposed five pathways i.e. the different relationships between our variables of interest in our mediation model: the exposure variable disability status, the mediator stigma and the two outcomes depression and self-esteem. We tested the “a path” from our exposure X-variable (disabled vs. non-disabled status) to the hypothesized mediator variable (level of stigma). We then tested the “b path” from our exposure X-variable (disability status) to the first outcome Y1-variable (level of depression), as well as the “c path” from the exposure X-variable (disability status) to the second outcome Y2-variable (level of self-esteem). Then, we tested the “d path” and the “e path” from the mediator (stigma) to respectively Y1-variable (depression) and Y2-variable (self-esteem). Finally, we tested the complete mediation model, simultaneously estimating the five paths. We estimated the total effect between disability and depression and self-esteem not accounting for stigma. The indirect effect in our mediation model was defined as the effect of being disabled on the outcomes of being depressed and having a lack of self-esteem as mediated by stigma and was referred to as the mediated effect. The mediator-specific indirect effects were the product of the three coefficients for the corresponding “a path” and “d path” and “e path” that trace the indirect influence of the X-variable respectively on the Y1-variable and Y2-variable. The direct effects (b and c paths) in our models were the effect of being disabled on depression and self-esteem respectively after accounting for the indirect effect. The “f path” is a specific effect of depression on self-esteem. The mediated effect can be categorized as partial or full (Muthén et al., 2018). Partial mediation happens when the indirect effect is statistically significant though the direct effect is reduced in magnitude but remains significant, while in full mediation the direct effect is no longer significant. For the complete model, we obtained bias-corrected bootstrapped standard errors and confidence intervals for all path coefficients along with the indirect effects estimate (the product respectively of the a and d path and a and e path) and used the confidence intervals to evaluate the statistical significance of each effect (MacKinnon 2008).
We included gender, age, education level, marital status, employment status and welfare level as covariates for all estimated models. To check for robustness, we calculated the structural equation model introducing some different stratifications of the model according to different age groups (18–40 years old, 41–60 years old and above 60), education levels (lower than secondary, secondary schooling and higher), welfare levels (poorest 20%, middle 60% and richest 20%) and for alternative specification of the mediator stigma (mild below 2, moderate 2 to 3 and severe above 3) and of the outcomes level of depression (not depressed score below 10 and depressed score above 10) and self-esteem (low score 10–20, moderate 21–30 and high self-esteem 31–40). Our results were not altered.
The study has received ethical approval from the human research protection office at Washington University in St Louis and from the Institutional Review Board at University of Johannesburg, and all participants gave informed consent.
3. Results
3.1. Descriptive statistics
Demographic, socioeconomic and mental health characteristics of the sample are presented in Table 1 . Participants were all adults aged between 18 and 89 years (= 50.44, SD = 0.87) and participants with disabilities were on average slightly older (approximately 4 and a half years) than participants without disabilities. About 60% of both groups were female. All participants were Black South African. Around two-thirds (63.1%) of the entire sample had secondary school education or higher. Unemployment was significantly higher among participants with disabilities (50%) than those without disabilities (43%) as might be expected. The mean stigma score was 1.53 (SD = 0.53) across both groups. Only 9.9% (n = 19) of the non-disabled group experienced high discrimination (i.e. stigma score of 2 and above), as compared to 24.4% of the participants in the disability group (n = 46). The overall sample had a mean depression score of 11.81 (SD = 5.93). Persons with disabilities were almost twice as likely to indicate being depressed (48.2%) than persons without disabilities (24.5%). Participants with disabilities had a lower average self-esteem score ( = 26.19, SD = 4.67) compared to participants without a disability (= 28.49, SD = 3.46).
Table 1.
Characteristics of sample.
| Characteristics | Persons without disabilities (n = 196) | Persons with disabilities (n = 191) | Total (n = 387) | P value |
|---|---|---|---|---|
| Social-demographic characteristics | ||||
| Gender: | ||||
| Male | 76 (39%) | 83 (43%) | 159 (41%) | p < 0.349 |
| Female | 120 (61%) | 108 (57%) | 228 (59%) | |
| Age | ||||
| mean (SD) | 48.11(16.26) | 52.84 (17.54) | 50.44 (17.05) | p < 0.006 |
| Education: | ||||
| No Schooling | 14 (7.1%) | 31 (16.2%) | 45 (11.6%) | p < 0.003 |
| Lower than secondary | 44 (22.5%) | 54 (28.3%) | 98 (25.3%) | |
| Secondary Schooling and higher | 138 (70.4%) | 106 (55.5%) | 244 (63.1%) | |
| Employment: | ||||
| Employed | 44 (22.5%) | 16 (8.4%) | 60 (15.5%) | p < 0.0001 |
| Self-employed | 15 (7.6%) | 9 (4.7%) | 24 (6.2%) | |
| Too young/old for employment | 53 (27.0%) | 71 (37.2%) | 124 (32.0%) | |
| Unemployed | 84 (42.9%) | 95 (49.8%) | 179 (46.3%) | |
| Marital Status: | ||||
| Married/Engaged/Living with partner | 60 (31%) | 75 (39%) | 135 (35%) | p < 0.177 |
| Separated/Widow | 37 (19%) | 35 (18%) | 72 (19%) | |
| Single/Never married | 99 (51%) | 81 (42%) | 180 (47%) | |
| Welfare index | ||||
| mean (SD) | −0.09(1.13) | −0.10(1.26) | −0.05(1.19) | p < 0.456 |
| Mental Health characteristics | ||||
| Stigma Score | ||||
| mean (SD) | 1.41 | 1.66 | 1.53(0.53) | P < 0.0001 |
| Stigma Score Categories | ||||
| less than 2 | 172 (90%) | 142 (76%) | 314 (83%) | P < 0.0001 |
| More than 2 | 19 (9.9%) | 46 (24.4%) | 65 (17%) | |
| Self-Esteem | ||||
| mean (SD) | 28.49 (3.46) | 26.19 (4.67) | 27.31(4.24) | P < 0.0001 |
| Self-Esteem Categories: | ||||
| Score 10-20 | 2 (1%) | 16 (8%) | 18 (5%) | P < 0.0001 |
| Score 21-30 | 146 (74%) | 146 (76%) | 292 (75%) | |
| Score 31-40 | 48 (29%) | 29 (15%) | 77 (20%) | |
| Depression | ||||
| mean (SD) | 9.96 (4.77) | 13.70 (6.40) | 11.81 (5.93) | P < 0.0001 |
| Depression Categories: | ||||
| Not Depressed (<10) | 148 (75.5%) | 99 (51.8%) | 247 (63.8%) | P < 0.0001 |
| Depressed (≥10) | 48 (24.5%) | 92 (48.2%) | 140 36.2%) | |
Note: Welfare index is calculated from the welfare indicators which includes the following durable goods: type of dwelling, water source, energy for cooking, heating and lighting, type of toilet, level of food insecurity.
3.2. Propensity score matching analysis
Table 2 shows that the average stigma score was significantly higher by 0.25 points (p < 0.001) for persons with disabilities compared to persons without disabilities. Persons with disabilities also had a depression score of 3.3 points higher on average than persons without disabilities (p < 0.001) while their self-esteem score was 2.1 points lower (p < 0.001), after controlling for gender, age, level of education, marital status, employment status and the welfare index. Participants who had a high discrimination score (above 2) in our sample had significantly higher depression scores (4.6 points, p < 0.001) and lower self-esteem scores (1.6 points, p < 0.01) on average. Table 3 displays results of the sensitivity analysis.
Table 2.
Average treatment effect of disability on stigma, depression and self-esteem and stigma on depression and self-esteem.
| MODEL 1 Disability on Stigma ATT°(95%CI) | MODEL 2 Disability on Depression ATT°(95%CI) | MODEL 3 Disability on Self-esteem ATT°(95%CI) | MODEL 4 Stigma on Depression ATT°(95%CI) | MODEL 5 Stigma on Self-esteem ATT °(95%CI) | |
|---|---|---|---|---|---|
| PSM Matching Results | |||||
| Kernel matching | 0.253***(0.118, 0.388) | 3.337***(1.990, 4.684) | −2.055***(-2.847, -1.263) | 4.581***(3.038, 6.126) | −1.641**(-2.668, -0.615) |
| Nearest neighbors matching: | 0.261***(0.141, 0.381) | 2.676***(1.197, 4.154) | −1.452*(-2.691, -0.213) | 4.453***(2.212, 6.694) | −1.906*(-3.669, -0.143) |
| Radius matching replacement | 0.252***(0.134, 0.371) | 3.387***(2.315, 4.458) | −2.087***(-2.867, -1.308) | 4.685***(3.227, 6.504) | −1.791**(-2.889, -0.693) |
| Radius matching without replacement | 0.252***(0.151, 0.356) | 3.387***(2.311, 4.462) | −2.087***(-2.812, -1.363) | 4.865***(3.221, 6.510) | −1.791***(-2.759, -0.823) |
| Local linear regression matching: | 0.252***(0.156, 0.349) | 3.266***(2.005, 4.527) | −1.938***(-2.696, -1.179) | 4.529***(2.791, 6.269) | −1.543*(-2.729, -0.357) |
Note: °Average Treatment Effect on the Treated; *p < 0.05, **p < 0.01, ***p < 0.001. Note: We used logit regression for the matching models and the matching variables are binary covariates included Female (ref=Male), No education (ref=Education), Married (ref=Unmarried), Work (ref=Employed), 20% Richest (ref=80%non-richest) and Age.
Table 3.
Sensitivity analysis: Average treatment effect of disability on stigma, depression and self-esteem and stigma on depression and self-esteem.
| MODEL 1 Disability on Stigma ATT°(95%CI) | MODEL 2 Disability on Depression ATT°(95%CI) | MODEL 3 Disability on Self-esteem ATT°(95%CI) | MODEL 4 Stigma on Depression ATT°(95%CI) | MODEL 5 Stigma on Self-esteem ATT °(95%CI) | |
|---|---|---|---|---|---|
| Kernel Matching | |||||
| Sensitivity Analysis Model 1# | 0.249(0.162–0.336) | 3.278(2.007–4.550) | −1.998(-2.878, −1.118) | 4.586(2.805, 6.368) | −1.589(-3.059, −0.120) |
| Sensitivity Analysis Model 2+ | 0.148(0.079–0.218) | 0.202(0.111–0.293) | −0.226(-0.360, −0.092) | 0.227(0.106, 0.348) | −0.136(-0.341, 0.068) |
Note: °Average Treatment Effect on the Treated estimated from sensitivity analysis with kernel matching.#Model 1 estimated ATT by using the continuous outcome with categorical covariates age in quantile group (18–41, 42–60, 61–89), gender (male and female), education (lower than secondary, secondary schooling and higher, secondary schooling and higher), work (unemployed and employed) marital status (single, married, divorced), welfare index (20% poorest, 60% middle, 20% richest).+Model 2 estimated ATT by using binary outcomes and binary covariates except age (continuous variable) included Female (ref=Male), No education (ref=Education), Married (ref=Unmarried), Work (ref=Employed), 20% Richest (ref=80%non-richest).
3.3. Mediation effect analysis
Table 4 displays the model results for the different independent paths. Having a disability was directly and significantly predictive of depression (b path) and low self-esteem (c path). But for the “a path” measuring the effect of disability on stigma, “d path” and “e path”, the effect of stigma on respectively depression and self-esteem show that the effect was partially indirect through the mediation of discrimination caused by stigma and measured by unfair treatment.
Table 4.
Structural equation model “a path” from disabled vs. non-disabled samples to stigma, “b path” from disability to depression, “c path” from disability to self-esteem, “d” path from stigma to depression, and “e path” from stigma to self-esteem and “f path” from depression to self-esteem.
| a Path | b Path | c Path | d path | e path | f path | |
|---|---|---|---|---|---|---|
| Estimate | 3.864*** | 2.143** | −1.618*** | 0.268*** | −0.09** | −6.884*** |
| Standardized Estimate | 0.958 | 0.554 | 0.446 | 0.031 | 0.025 | 1.094 |
Note: Regression results are adjusted for age, gender, marital status, level of education, employment status and welfare index. *p < 0.05, **p < 0.01, ***p < 0.001.
The full model fit indices indicated excellent model fit: the CFI value for the model was 1.000, the RMSEA was 0.000, the TLI was 1.000 and χ2 = 256.659 (p < 0.0001). Fig. 4 shows a partial mediation model adjusted for covariates. The total effect of being disabled was positive and statistically associated with being depressed (2.143, 95%CI: 1.238–3.081) and low self-esteem (−1.618, 95%CI: −2.328 to −0.860), indicating that persons with disabilities had a significantly higher rate of depression and lower scores of self-esteem than those without disabilities. The direct effect is reduced in magnitude but remained statistically significant, indicating that the effect of disability status on depression and self-esteem was partly mediated by discrimination and stigma. The specific indirect effect along with the “a path” (3.864, 95%CI 2.273–5.403) was positive denoting that persons with disabilities had higher rates of discrimination and stigma, which in turn, corresponded to higher rates of depression (0.268, CI: 0.218–0.318) and lower levels of self-esteem (−0.090, CI: −0.131 to −0.049) (Table 5 ). Levels of stigma significantly reduced with increasing age (−0.073, CI: 0.129–0.024) but was not significantly affected by gender, marital status, education, employment or material wealth (Table 5). Conversely, depression scores increased significantly with age (0.054, CI:0.027–0.082) and considerably with unemployment (1.748, CI:0.766–2.662) (Table 5). Finally, both having no education and being unemployed decreased self-esteem.
Fig. 4.
Path diagram of the structural equation model with standardized path coefficients, testing mediation of stigma on depression and self-esteem.
Table 5.
Detailed Results of the structural equation model.
| Model Results | Estimate | [95% Conf. Interval] | |
|---|---|---|---|
| Direct effects | |||
| “a path” from disabled vs. non-disabled samples to stigma | |||
| Stigma scales on | |||
| Disability status | 3.864*** | 2.273 | 5.403 |
| Age | −0.073* | −0.129 | −0.024 |
| Female+ | 0.449 | −1.104 | 2.084 |
| Married+ | 1.431 | −0.211 | 3.18 |
| No Education+ | −1.059 | −3.694 | 1.915 |
| Work (Unemployed) + | −1.598 | −3.64 | 0.24 |
| Richest+ | 1.796 | −0.253 | 3.813 |
| “b path” from disability to depression | |||
| Depression scales on | |||
| Disability status | 2.143*** | 1.238 | 3.081 |
| Age | 0.054** | 0.027 | 0.082 |
| Female+ | 0.045 | −0.845 | 0.954 |
| Married+ | −0.308 | −1.298 | 0.645 |
| No Education+ | 0.231 | −1.059 | 1.709 |
| Work (Unemployed) + | 1.748** | 0.766 | 2.662 |
| Richest+ | 0.851 | −0.233 | 1.965 |
| “c path” from disability to self-esteem | |||
| Self-esteem scales on | |||
| Disability status | −1.618*** | −2.328 | −0.86 |
| Age | 0.009 | −0.016 | 0.03 |
| Female+ | −0.215 | −0.939 | 0.509 |
| Married+ | 0.46 | −0.274 | 1.19 |
| No Education+ | −1.396* | −2.396 | −0.426 |
| Work (Unemployed) + | −1.426** | −2.273 | −0.594 |
| Richest+ | 0.481 | −0.41 | 1.419 |
| “d path from stigma to depression, | |||
| Stigma scales | 0.268*** | 0.218 | 0.318 |
| “e path” from stigma to self-esteem and | |||
| Stigma scales | −0.090*** | −0.131 | −0.049 |
| “f path” from depression to self-esteem | |||
| Depression with | |||
| Self-esteem | −6.705*** | −8.576 | −5.219 |
Note: +are dummy variables: Female (ref = Male), No education (ref = Education), Married (ref = Unmarried), Work (ref = Employed), 20% Richest (ref = 80% non-richest, is calculated from the welfare index which includes the following durable goods: type of dwelling, water source, energy for cooking, heating and lighting, type of toilet, level of food insecurity), Significant relationships are indicated with a star (*) *p < 0.05, **p < 0.01, ***p < 0.001.
4. Discussion
This study is the first to examine the associations and the pathways between disability, depression and low self-esteem through discrimination and stigma in a Middle-Income Country (MIC). In addition, it uses a representative sample of poor urban Black South African adults with disabilities, living in a township and a demographically matched sample. Our findings show that persons with disabilities face discrimination and stigma which is associated with an increased risk of depression and lower self-esteem even after controlling for age, gender, marital status, level of education, employment status and welfare status. These findings are an important contribution to the literature on the mental health impact of discrimination and stigma associated with disability. Stigma and discrimination associated with disability have been widely analyzed as a barrier to services such as healthcare, education (Bakhshi et al., 2018; Mizunoya et al., 2016), employment (Trani et al., 2018) and social and political participation in LMICs (Parnes et al., 2009). However, only one study has investigated the toll of stigma and discrimination on mental health (Trani et al., 2016) and none on self-esteem of persons with disabilities.
We found a significant relationship between reporting a disability and depressive mood, somatic complaints, negative feelings such as unhappiness and feelings of low self-esteem reported through ten items measuring lack of self-worth (feelings of inability, lack of self-respect and uselessness). The relationship between disability, depression and low self-esteem is partially mediated by discrimination and stigma measured in thirteen facets of a respondents’ life (namely education, marriage, other personal relationships, employment, housing, public transportation, welfare benefit, religious practices, social life, interaction with police, interaction with healthcare professionals, parenting and personal safety). Our findings substantiate the social model of disability which holds the view that, through stigma and discrimination, society is responsible for the systematic exclusion of persons with disabilities from all spheres of life (Oliver 1990; Shakespeare 2006). A direct link also exists between disability, discrimination and low self-esteem. The complexity of this relationship confirms the theory of stigma proposed by Link and Phelan (2001) who showed how labeling and stereotyping a social group, such as persons with disabilities, can lead to discrimination which in turn generates negative outcomes such as depression and diminished self-esteem. Our findings extend previous research which showed that the stigmatization of persons with psychosocial or intellectual disabilities results in distress, withdrawal and experience of low self-esteem (Dagnan and Waring 2004; Livingston and Boyd 2010; Mirza et al., 2009; Zhang et al., 2014). In other words, it is not (just) the impairment in itself but rather the perception of how society welcomes and accommodates disability that influences self-esteem, other forms of self-perception and coping mechanisms of persons with disabilities (Paterson et al., 2012). Finally, our findings also show that disability may result in depression and diminished self-esteem as a significant association exists between these variables in our model, confirming the relevance of the bio-psycho-social model (WHO 2001).
After controlling for all other covariates in the study, socio-demographic factors (particularly gender and marital status) did not add to overall discrimination and its impact on distress and self-worth. Yet, older adults might become more depressed than younger adults due to higher levels of social isolation. Furthermore, dementia that is more prevalent among older adults has been shown to occur together with depression (Brzezińska et al., 2020). In a deprived urban area of South Africa, populated by Black South Africans, disability more than relative poverty, age or gender is the most powerful driver of discrimination, depression and reduced self-esteem. Yet, intersectionality between specific forms of disability —predominantly psychosocial disability— with other identities —being a woman in particular— has been found to be an aggravating factor of discrimination and stigma in some other contexts, including in LMICs (Braathen and Kvam 2008; Goodall et al., 2018; Whittle et al., 2017). In our study, intersectionality did not significantly reinforce the overall effect of labeling and stereotyping associated with disability in general. Further research is needed to determine whether the intersectionality of gender, race, economic status and disability status —or type of disability (such as psychosocial disability) — results in discrimination and stigma in specific domains such as the labor market or in intimate relationships (Van der Heijden et al., 2019b).
Another finding that warrants further comment concerns the evidence that unemployed persons experienced higher levels of depression. Research shows that unemployment is a risk factor for depression in South Africa (Burns et al., 2017; Graham and Mlatsheni, 2015; Tomita and Burns 2013). One possible explanation in the specific case of persons with disabilities could be that negative attitudes and common stereotypes towards persons with disabilities reduce employment opportunities which in turn results in aggravating depressive symptoms although few studies have investigated this complex association (Coetzer et al., 2011; Maja et al., 2011). More generally, results show that unemployment induces low self-esteem in our model while employment is a protective factor, confirming existing literature (De Witte et al., 2012). Yet, previous research has also shown that low self-esteem predicts a significant negative indirect effect of disability, particularly in the case of women, on employment (Nosek et al., 2003). Our finding suggests the existence of a positive feedback loop between employment and self-esteem indicating that working South Africans with or without disabilities have a higher sense of self-worth. By contrast, unemployment increases both depression and self-deprecation of persons with disabilities.
Higher levels of education have been found here to be a protective factor against low self-esteem levels. This result is in contradiction with a study that shows no significant effect of education on self-esteem in the case of women with disabilities in the United States (Nosek et al., 2008). Our study identified that persons with disabilities who had relatively higher material wealth did not report lower discrimination, lower depression or higher self-esteem. Relative material wealth is therefore not a protective factor against stigma of disability and associated distress. One possible explanation is the limited gap in material wealth between rich and poor in Soweto. The existence of a disability grant welfare mechanism might in fact close the gap.
Finally, we note some study limitations. The cross-sectional nature of the data suggests caution in establishing causal relationship (Vanderweele 2012). It might, for example, be fruitful to explore a bidirectional association between disability and depression or low self-esteem. This could take place via stigma and discrimination, the idea being that increased depression and diminished self-worth could aggravate discriminating behaviors from the general population. Longitudinal data, event analysis particularly, would permit this hypothesis to be tested. Second, we could not investigate if stigma and negative outcomes vary according to race and ethnicity because the population of Soweto is nearly entirely (95%) Black African. Finally, the standard measures of discrimination, depression and self-esteem used were self-reported, and the possibility of social desirability bias in all responses cannot be totally excluded.
5. Conclusion and potential policy implications
Understanding the main pathways between disability, stigma, self-esteem and depression has important policy implications for understanding the consequences of being disabled. Negative attitudes towards, and beliefs about, disabilities are associated with discrimination and unfair treatment which induces further depression and low self-esteem. Unemployment also contributes to depression and poor self-esteem while lack of education decreases self-esteem. Unfortunately, persons with disabilities, more often than the general population, face barriers to both education and employment in Soweto.
Nonetheless, South Africa has a unique constitution endorsing equal rights (civil, political, social and economic) for persons with disabilities (Government of South Africa 1996). If rights are politically endorsed, their implementation on a day-to-day basis remains elusive in many areas from access to health care to right to employment (Hussey et al., 2017; Wiggett-Barnard and Swartz 2012). This state of affairs leaves persons with disabilities vulnerable and at the margins of society reinforcing the observed vicious circle of disability, unfair treatment, and poor mental health outcomes.
Physical barriers are obvious but the mental health and social exclusion consequences that follow from stigma and discrimination may be just as harmful. As a result, it should be a priority to fight discrimination. To fight stigma, the existing literature shows that education and interpersonal contact are two effective strategies (Corrigan et al., 2012) with longer lasting effects in the case of contact (Corrigan et al., 2015). Attempts at changing unfair attitudes through showing a protest-based intervention about rights of persons with intellectual disabilities has shown some promise (Walker and Scior 2013). Culturally relevant anti-stigma interventions towards mental illness such as “What matters most” have produced positive effect in HICs (Yang et al., 2014) and could be adapted to LMICs for disability in general. Yet, a recent review of stigma reduction interventions towards mental disorders in LMICs have shown shortcomings in cultural adaptation (Mascayano et al., 2020).
At the micro level, community based rehabilitation (CBR) programs, if genuinely based on empowerment of and ownership by persons with disabilities, their families, representative organizations, and other community members, might constitute a fundamental mechanism for addressing stigma of disability (Elphick 2017). CBR programs actively engage in promoting social participation of persons with disabilities through consistent personal contacts and interaction, and build the feeling of self-worth (Biggeri et al., 2014). They also support access to services and participation in the labor market.
Moreover, at the macro-level, encouraging policy makers to include disability issues in all public policy areas and at all levels of policy processes may promote change. There may be particular opportunities to seize in the COVID-19 pandemic context. Positive change may also benefit from reinforcing the legitimacy of disabled peoples' organizations by systematically promoting their involvement in the development of public policy. No public policy should become law without reference to statutory arrangements for persons with disabilities. Once recognized in law, empowering disabled peoples’ organizations and institutions to implement policy is paramount. New policies addressing the stigma of disability require a variety of systemic, innovative, multipronged, participatory approaches that involve cultural sensitivity and individual interactions. They have the potential to offer psychosocial support to address social exclusion and its consequences for the mental wellbeing of persons with disabilities in South Africa and other LMICs (Department of Social Development 2015). Without such concrete policy actions, the SDGs will be largely irrelevant to persons with disabilities, as were the MDGs before them.
Acknowledgments
The present study was supported by funding from the Institute of Public Health at Washington University in St Louis, Missouri, United States and the University of Johannesburg's Research Committee, South Africa. We thank the inhabitants of Doornkop, Soweto for welcoming our research team and we thank the randomly selected participants for their patience in responding to our interview questions. We also thank Professor Shenyang Guo for his insight and feedback on propensity score matching.
References
- Abberley P. Concept of oppression and the development of a social model of disability. Disabil. Handicap Soc. 1987;2(1):5–19. The. [Google Scholar]
- Ali A. Ethnicity and self-reported experiences of stigma in adults with intellectual disability in Cape Town, South Africa. J. Intellect. Disabil. Res. 2015;59(6):530–540. doi: 10.1111/jir.12158. [DOI] [PubMed] [Google Scholar]
- Ali Afia. Self-reported stigma and symptoms of anxiety and depression in people with intellectual disabilities: findings from a cross sectional study in England. J. Affect. Disord. 2015;187:224–231. doi: 10.1016/j.jad.2015.07.046. [DOI] [PubMed] [Google Scholar]
- Amuri M. Socio-economic status and HIV/AIDS stigma in Tanzania. AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV. 2011;23(3):378–382. doi: 10.1080/09540121.2010.507739. [DOI] [PubMed] [Google Scholar]
- Anand P. The development of capability indicators. Journal of Human Development and Capabilities. 2009;10(1):125–152. [Google Scholar]
- Austin Peter C. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am. J. Epidemiol. 2010;172(9):1092–1097. doi: 10.1093/aje/kwq224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin Peter C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav. Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakhshi Parul, Babulal Ganesh M., Jean-Francois Trani Education and disability in a conflict affected context: are children with disabilities less likely to learn and be protected in Darfur? World Dev. 2018;106:248–259. [Google Scholar]
- Baranik Lisa E. Examining the differential item functioning of the Rosenberg self‐esteem scale Across eight countries 1. J. Appl. Soc. Psychol. 2008;38(7):1867–1904. [Google Scholar]
- Baron Emily, Davies Thandi, Lund Crick. Validation of the 10-item centre for epidemiological studies depression scale (CES-D-10) in Zulu, Xhosa and Afrikaans populations in South Africa. BMC Psychiatr. 2017;17(1):6. doi: 10.1186/s12888-016-1178-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggeri M. Do community-based rehabilitation programmes promote the participation of persons with disabilities? A case control study from Mandya District, in India. Disabil. Rehabil. 2014;36(18):1508–1517. doi: 10.3109/09638288.2013.823244. [DOI] [PubMed] [Google Scholar]
- Blundell R., Costa Dias M. Alternative approaches to evaluation in empirical microeconomics. Portuguese Econ. J. 2002;1:91–115. [Google Scholar]
- Braathen Stine Hellum, Kvam Marit Hoem. Can anything good come out of this mouth?" female experiences of disability in Malawi. Disabil. Soc. 2008;23(5):461–474. [Google Scholar]
- Brohan E. Development and psychometric evaluation of the discrimination and stigma scale (DISC) Psychiatr. Res. 2013;208(1):33–40. doi: 10.1016/j.psychres.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Brohan E. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr. Res. 2010;122(1–3):232–238. doi: 10.1016/j.schres.2010.02.1065. [DOI] [PubMed] [Google Scholar]
- Brzezińska Agnieszka. Depression in dementia or dementia in depression? Systematic review of studies and hypotheses. Curr. Alzheimer Res. 2020;17(1):16–28. doi: 10.2174/1567205017666200217104114. [DOI] [PubMed] [Google Scholar]
- Buljevac M., Majdak M., Leutar Z. The stigma of disability: Croatian experiences. Disabil. Rehabil. 2012;34(9):725–732. doi: 10.3109/09638288.2011.616570. [DOI] [PubMed] [Google Scholar]
- Burchardt T. vol. 19. Routledge; 2004. pp. 735–751. (Capabilities and Disability: the Capabilities Framework and the Social Model of Disability). [Google Scholar]
- Burns Jonathan K., Tomita Andrew, Lund Crick. Income inequality widens the existing income-related disparity in depression risk in post-apartheid South Africa: evidence from a nationally representative panel study. Health Place. 2017;45:10–16. doi: 10.1016/j.healthplace.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caliendo Marco, Kopeinig Sabine. Some practical guidance for the implementation of propensity score matching. J. Econ. Surv. 2008;22(1):31–72. [Google Scholar]
- Chan Yi. Investigating quality of life and self-stigma in Hong Kong children with specific learning disabilities. Res. Dev. Disabil. 2017;68:131–139. doi: 10.1016/j.ridd.2017.07.014. [DOI] [PubMed] [Google Scholar]
- Coetzer R., Carroll E., Ruddle J.A. Depression, anxiety and employment status after traumatic brain injury. Soc. Care Neurodisability. 2011;2(4):200–207. [Google Scholar]
- Conner K.O. Barriers to treatment and culturally endorsed coping strategies among depressed African-American older adults. Aging Ment. Health. 2010;14(8):971–983. doi: 10.1080/13607863.2010.501061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooney G. Young people with intellectual disabilities attending mainstream and segregated schooling: perceived stigma, social comparison and future aspirations. J. Intellect. Disabil. Res. 2006;50(6):432–444. doi: 10.1111/j.1365-2788.2006.00789.x. [DOI] [PubMed] [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. Am. Psychol. 2004;59(7):614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Corrigan P., Schomerus G., Smelson D. Are some of the stigmas of addictions culturally sanctioned? Br. J. Psychiatry. 2017;210(3):180–181. doi: 10.1192/bjp.bp.116.185421. [DOI] [PubMed] [Google Scholar]
- Corrigan P.W., Kerr A., Knudsen L. The stigma of mental illness: explanatory models and methods for change. Appl. Prev. Psychol. 2005;11(3):179–190. [Google Scholar]
- Corrigan P.W. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr. Serv. 2012;63(10):963–973. doi: 10.1176/appi.ps.201100529. [DOI] [PubMed] [Google Scholar]
- Corrigan P.W., Watson A.C., Barr L. The self-stigma of mental illness: implications for self-esteem and self-efficacy. J. Soc. Clin. Psychol. 2006;25(8):875–884. [Google Scholar]
- Corrigan Patrick, Patrick J., Scott Morris. Do the effects of antistigma programs persist over time? Findings from a meta-analysis. Psychiatr. Serv. 2015;66(5):543–546. doi: 10.1176/appi.ps.201400291. [DOI] [PubMed] [Google Scholar]
- Corwyn R.F. The factor structure of global self-esteem among adolescents and adults. J. Res. Pers. 2000;34(4):357–379. [Google Scholar]
- Dagnan D., Waring M. Linking stigma to psychological distress: testing a social-cognitive model of the experience of people with intellectual disabilities. Clin. Psychol. Psychother. 2004;11(4):247–254. [Google Scholar]
- De Witte Hans, Rothmann Sebastiaan, Jackson Leone TB. The psychological consequences of unemployment in South Africa. S. Afr. J. Econ. Manag. Sci. 2012;15(3):235–252. [Google Scholar]
- Department of Social Development . 2015. White Paper on the Rights Persons with Disabilities. Republic of South Africa. [Google Scholar]
- Eaton William W. Center for epidemiologic studies depression scale: review and revision (CESD and CESD-R) In: Maruish M.E., editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults. Lawrence Erlbaum; Mahwah, NJ: 2004. pp. 363–377. [Google Scholar]
- Eide A.H. Perceived barriers for accessing health services among individuals with disability in four African countries. PloS One. 2015;10(5) doi: 10.1371/journal.pone.0125915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elphick J. University of Johannesburg; 2017. Evaluation of a Community-Based Rehabilitation Programme for Caregivers of Children with Disabilities in a South African Township. [Google Scholar]
- Evans-Lacko S. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol. Med. 2012;42(8):1741–1752. doi: 10.1017/S0033291711002558. [DOI] [PubMed] [Google Scholar]
- Goodall J. Stigma and functional disability in relation to marriage and employment in young people with epilepsy in rural Tanzania. Seizure. 2018;54:27–32. doi: 10.1016/j.seizure.2017.11.016. [DOI] [PubMed] [Google Scholar]
- Government of South Africa . vol. 108. 1996. p. 378. (Constitution of the Republic of South Africa). [Google Scholar]
- Graham Lauren, Mlatshen Cecil. Youth unemployment in South Africa: understanding the challenge and working on solutions. In: De Lannoy A., Sharlene S., Lake L., Smith C., editors. Child Gauge. University of Cape Town; Cape Town: 2016. pp. 51–59. [Google Scholar]
- Green S.E. What do you mean 'what's wrong with her? '" : stigma and the lives of families of children with disabilities. Soc. Sci. Med. 2003;57(8):1361–1374. doi: 10.1016/s0277-9536(02)00511-7. [DOI] [PubMed] [Google Scholar]
- Halter Margaret. The stigma of seeking care and depression. Arch. Psychiatr. Nurs. 2004;18(5):178–184. doi: 10.1016/j.apnu.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler M.L. Structural stigma and all-cause mortality in sexual minority populations. Soc. Sci. Med. 2014;103:33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler M.L., Link B.G. Introduction to the special issue on structural stigma and health. Soc. Sci. Med. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- Hu L.T., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 1999;6:1–55. [Google Scholar]
- Hunt X. Dating persons with physical disabilities: the perceptions of South Africans without disabilities. Cult. Health Sex. 2018;20(2):141–155. doi: 10.1080/13691058.2017.1334964. [DOI] [PubMed] [Google Scholar]
- Hussey M., MacLachlan M., Mji G. Barriers to the implementation of the health and rehabilitation articles of the United Nations convention on the rights of persons with disabilities in South Africa. Int. J. Health Pol. Manag. 2017;6(4):207–218. doi: 10.15171/ijhpm.2016.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbens G.W. Nonparametric estimation of average treatment effects under exogeneity: a review. Rev. Econ. Stat. 2004;86(1):4–29. [Google Scholar]
- Imbens, Guido W. Matching methods in practice: three examples. J. Hum. Resour. 2015;50(2):373–419. [Google Scholar]
- Kolenikov S., Angeles G. Socioeconomic status measurement with discrete proxy variables: is principal component analysis: a reliable answer? Rev. Income Wealth. 2009;55(1):128–165. [Google Scholar]
- Lamichhane K., Okubo T. The nexus between disability, education, and employment: evidence from Nepal. Oxf. Dev. Stud. 2014;42(3):439–453. [Google Scholar]
- Link B.G., Phelan J.C. Conceptualizing stigma. Annu. Rev. Sociol. 2001;27:363–385. [Google Scholar]
- Livingston J.D., Boyd J.E. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc. Sci. Med. 2010;71(12):2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Lukachko A., Hatzenbuehler M.L., Keyes K.M. Structural racism and myocardial infarction in the United States. Soc. Sci. Med. 2014;103:42–50. doi: 10.1016/j.socscimed.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma J.B. Slow and steady wins the race: a randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. J. Consult. Clin. Psychol. 2012;80(1):43–53. doi: 10.1037/a0026070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon David Peter. Routledge; 2008. Introduction to Statistical Mediation Analysis. [Google Scholar]
- Madans Jennifer H., Loeb Mitchell E., Altman Barbara M. Measuring disability and monitoring the UN convention on the rights of persons with disabilities: the work of the Washington group on disability statistics. BMC Publ. Health. 2011;11 doi: 10.1186/1471-2458-11-S4-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahomed F. Stigma on the basis of psychosocial disability: a structural human rights violation. S. Afr. J. Hum. Right. 2016;32(3):490–509. [Google Scholar]
- Maja P.A. Employing people with disabilities in South Africa. South African Journal of Occupational Therapy. 2011;41(1):24–32. [Google Scholar]
- Makhubela Malose, Solomon Mashegoane. Psychological validation of the Rosenberg Self-Esteem Scale (RSES) in South Africa: method effects and dimensionality in black African and white university students. J. Psychol. Afr. 2017;27(3):277–281. [Google Scholar]
- Mascayano F. Including culture in programs to reduce stigma toward people with mental disorders in low- and middle-income countries. Transcult. Psychiatr. 2020;57(1):140–160. doi: 10.1177/1363461519890964. [DOI] [PubMed] [Google Scholar]
- Maulik P.K., Darmstadt G.L. Childhood disability in low- and middle-income countries: overview of screening, prevention, services, legislation, and epidemiology. Pediatrics. 2007;120(Suppl. 1):S1–S55. doi: 10.1542/peds.2007-0043B. [DOI] [PubMed] [Google Scholar]
- Meininger H.P. Connecting stories: a narrative approach of social inclusion of persons with intellectual disability. Alter. 2010;4(3):190–202. [Google Scholar]
- Miller C.T. Community norms about suppression of AIDS-related prejudice and perceptions of stigma by people with HIV or AIDS. Psychol. Sci. 2011;22(5):579–583. doi: 10.1177/0956797611404898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills Harriet. Self-help interventions to reduce self-stigma in people with mental health problems: a systematic literature review. Psychiatr. Res. 2019:112702. doi: 10.1016/j.psychres.2019.112702. [DOI] [PubMed] [Google Scholar]
- Mirza I. Community management of intellectual disabilities in Pakistan: a mixed methods study. J. Intellect. Disabil. Res.: JIDR (J. Intellect. Disabil. Res.) 2009;53(6):559–570. doi: 10.1111/j.1365-2788.2009.01176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra S. The capability approach and disability. J. Disabil. Pol. Stud. 2006;16(4):236–247. [Google Scholar]
- Mizunoya S., Mitra S. Is there a disability gap in employment rates in developing countries? World Dev. 2013;42(1):28–43. [Google Scholar]
- Mizunoya Suguru, Mitra Sophie, Yamasaki Izumi. 2016. Towards Inclusive Education: the Impact of Disability on School Attendance in Developing Countries. [Google Scholar]
- Mruk Christopher JJ. Springer Publishing Company; 2006. Self-esteem Research, Theory, and Practice: toward a Positive Psychology of Self-Esteem. [Google Scholar]
- Mulumba M. Perceptions and experiences of access to public healthcare by people with disabilities and older people in Uganda. Int. J. Equity Health. 2014;13(1) doi: 10.1186/s12939-014-0076-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B.O., Muthén L.K., Asparouhov T. Muthén & Muthén; CA: Los Angeles: 2018. Regression and Mediation Analysis Using Mplus. [Google Scholar]
- Nosek M.A., Hughes R.B., Robinson-Whelen S. The complex array of antecedents of depression in women with physical disabilities: implications for clinicians. Disabil. Rehabil. 2008;30(3):174–183. doi: 10.1080/09638280701532219. [DOI] [PubMed] [Google Scholar]
- Nosek Margaret A. Self-esteem and women with disabilities. Soc. Sci. Med. 2003;56(8):1737–1747. doi: 10.1016/s0277-9536(02)00169-7. [DOI] [PubMed] [Google Scholar]
- Oliver M. Palgrave Macmillan; London: 1990. The Politics of Disablement. [Google Scholar]
- Oliver M. Palgrave Macmillan; Basingstoke: 1996. Understanding Disability: from Theory to Practice. [Google Scholar]
- Oshodi Y.O. Pattern of experienced and anticipated discrimination among people with depression in Nigeria: a cross-sectional study. Soc. Psychiatr. Psychiatr. Epidemiol. 2014;49(2):259–266. doi: 10.1007/s00127-013-0737-4. [DOI] [PubMed] [Google Scholar]
- Palad Y.Y. Scoping review of instruments measuring attitudes toward disability. Disability and Health Journal. 2016;9(3):354–374. doi: 10.1016/j.dhjo.2016.01.008. [DOI] [PubMed] [Google Scholar]
- Parnes P. Disability in low-income countries: issues and implications. Disabil. Rehabil. 2009;31(14):1170–1180. doi: 10.1080/09638280902773778. [DOI] [PubMed] [Google Scholar]
- Parsons J.A., Bond V.A., Nixon S.A. Are we not human?' Stories of stigma, disability and HIV from Lusaka, Zambia and their implications for access to health services. PloS One. 2015;10(6) doi: 10.1371/journal.pone.0127392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson L., McKenzie K., Lindsay B. Stigma, social comparison and self-esteem in adults with an intellectual disability. J. Appl. Res. Intellect. Disabil. 2012;25(2):166–176. doi: 10.1111/j.1468-3148.2011.00651.x. [DOI] [PubMed] [Google Scholar]
- Pellet Joanie. The relationship between self-stigma and depression among people with schizophrenia-spectrum disorders: a longitudinal study. Psychiatr. Res. 2019;275:115–119. doi: 10.1016/j.psychres.2019.03.022. [DOI] [PubMed] [Google Scholar]
- Pfeiffer D. The conceptualization of disability. In: Altman B.M., Barnatt Sharon N., editors. Exploring Theories and Expanding Methodologies: where We Are and where We Need to Go. Elsevier Jai; Oxford: 2001. pp. 29–52. [Google Scholar]
- Pryor J.B., Reeder G.D. HIV-related stigma. In: Hall J.C., Hall B.J., Cockerell C.J., editors. vol. 24. PMPH-USA.2015 The social psychology of HIV infection; Shelton, Connecticut: 2011. pp. 790–806. (HIV/AIDS in the Post-HAART Era: Manifestations, Treatment, and Epidemiology). [Google Scholar]
- Pryor John B., Reeder Glenn D., editors. The Social Psychology of HIV Infection. Psychology Press; 2015. [Google Scholar]
- Radloff Lenore Sawyer. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1(3):385–401. [Google Scholar]
- Reidpath D.D. He hath the French pox': stigma, social value and social exclusion. Sociol. Health Illness. 2005;27(4):468–489. doi: 10.1111/j.1467-9566.2005.00452.x. [DOI] [PubMed] [Google Scholar]
- Robins J.M., Greenland S. Identifiability and exchangeability for direct and indirect effects. Epidemiology. 1992;3(2):143–155. doi: 10.1097/00001648-199203000-00013. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P.R., Rubin D.B. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- Rubin Donald B. Using propensity scores to help design observational studies: application to the tobacco litigation. Health Serv. Outcome Res. Methodol. 2001;2(3–4):169–188. [Google Scholar]
- Rüsch N. Self-stigma, empowerment, and perceived legitimacy of discrimination among women with mental illness. Psychiatr. Serv. 2006;57(3):399–402. doi: 10.1176/appi.ps.57.3.399. [DOI] [PubMed] [Google Scholar]
- Schneider Marguerite. The difference a word makes: responding to questions on ‘disability’ and ‘difficulty’ in South Africa. Disabil. Rehabil. 2009;31(1):42–50. doi: 10.1080/09638280802280338. [DOI] [PubMed] [Google Scholar]
- Sen A.K. Clarendon Press; Oxford: 1992. Inequality Re-examined. [Google Scholar]
- Sen A.K. Oxford University Press; Oxford: 1999. Development as Freedom. [Google Scholar]
- Shakespeare Tom. The social model of disability. The disability studies reader. 2006;2:197–204. [Google Scholar]
- Steiger J.H. Understanding the limitations of global fit assessment in structural equation modeling. Pers. Indiv. Differ. 2007;42(5):893–898. [Google Scholar]
- Stuart Elizabeth A. Using non-experimental data to estimate treatment effects. Psychiatr. Ann. 2009;39(7):719–728. doi: 10.3928/00485713-20090625-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellez Juan. Capability deprivation of people with Alzheimer's disease: an empirical analysis using a national survey. Soc. Sci. Med. 2016;151:56–68. doi: 10.1016/j.socscimed.2015.12.032. [DOI] [PubMed] [Google Scholar]
- Tomita Andrew, Burns Jonathan K. A multilevel analysis of association between neighborhood social capital and depression: evidence from the first South African National Income Dynamics Study. J. Affect. Disord. 2013;144(1–2):101–105. doi: 10.1016/j.jad.2012.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trani J.F., Ballard E., Pena J. Stigma, social exclusion and mental distress of persons with disabilities in Afghanistan. Soc. Sci. Med. 2016;153:258–265. doi: 10.1016/j.socscimed.2016.02.024. [DOI] [PubMed] [Google Scholar]
- Trani J.F., Kumar P., Ballard E., Chandola T. Healthcare access for users with disabilities in Afghanistan: A population based cross sectional time comparison study. Lancet Global Health. 2017;5(8):e828–e837. doi: 10.1016/S2214-109X(17)30251-6. [DOI] [PubMed] [Google Scholar]
- Trani J.F., Brown D., Bakhshi P., Lopez D., Gall F. Disability as deprivation of capabilities: Estimation using a large-scale survey in Morocco and Tunisia and an instrumental variable approach. Soc. Sci. Med. 2018;211:48–60. doi: 10.1016/j.socscimed.2018.05.033. [DOI] [PubMed] [Google Scholar]
- United Nations Department of Economic and Social Affairs . 2018. UN Flagship Report on Disability and Development 2018. [Google Scholar]
- Uppal Sharanjit. Impact of the timing, type and severity of disability on the subjective well-being of individuals with disabilities. Soc. Sci. Med. 2006;63(2):525–539. doi: 10.1016/j.socscimed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Van Dam N.T., Earleywine M. Validation of the center for epidemiologic studies depression scale-revised (CESD-R): pragmatic depression assessment in the general population. Psychiatr. Res. 2011;186(1):128–132. doi: 10.1016/j.psychres.2010.08.018. [DOI] [PubMed] [Google Scholar]
- van der Heijden I., Abrahams N., Harries J. Additional layers of violence: the intersections of gender and disability in the violence experiences of women with physical disabilities in South Africa. J. Interpers Violence. 2019;34(4):826–847. doi: 10.1177/0886260516645818. [DOI] [PubMed] [Google Scholar]
- Van der Heijden I., Harries J., Abrahams N. In pursuit of intimacy: disability stigma, womanhood and intimate partnerships in South Africa. Cult. Health Sex. 2019;21(3):338–351. doi: 10.1080/13691058.2018.1470256. [DOI] [PubMed] [Google Scholar]
- Vanderweele T.J. Bias formulas for sensitivity analysis for direct and indirect effects. Epidemiology. 2010;21(4):540–551. doi: 10.1097/EDE.0b013e3181df191c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderweele T.J. Invited commentary: structural equation models and epidemiologic analysis. Am. J. Epidemiol. 2012;176(7):608–612. doi: 10.1093/aje/kws213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderweele T.J., Chiba Y. Sensitivity analysis for direct and indirect effects in the presence of exposure-induced mediator-outcome confounders. Epidemiology Biostatistics and Public Health. 2014;11(2) doi: 10.2427/9027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vansteelandt S. Estimating direct effects in cohort and case-control studies. Epidemiology. 2009;20(6):851–860. doi: 10.1097/EDE.0b013e3181b6f4c9. [DOI] [PubMed] [Google Scholar]
- Walker J., Scior K. Tackling stigma associated with intellectual disability among the general public: a study of two indirect contact interventions. Res. Dev. Disabil. 2013;34(7):2200–2210. doi: 10.1016/j.ridd.2013.03.024. [DOI] [PubMed] [Google Scholar]
- Westaway Margaret S., Jordaan Esmè R., Tsai Jennifer. Investigating the psychometric properties of the Rosenberg self-esteem scale for south African residents of greater Pretoria. Eval. Health Prof. 2015;38(2):181–199. doi: 10.1177/0163278713504214. [DOI] [PubMed] [Google Scholar]
- Whittle H.J. The land of the sick and the land of the healthy”: disability, bureaucracy, and stigma among people living with poverty and chronic illness in the United States. Soc. Sci. Med. 2017;190:181–189. doi: 10.1016/j.socscimed.2017.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2001. International Classification of Functioning, Disability and Health. [Google Scholar]
- Wiggett-Barnard Cindy, Swartz Leslie. What facilitates the entry of persons with disabilities into South African companies? Disabil. Rehabil. 2012;34(12):1016–1023. doi: 10.3109/09638288.2011.631679. [DOI] [PubMed] [Google Scholar]
- World Health Organization, World Bank . World Health Organization; 2011. World Report on Disability. [Google Scholar]
- Yang L.H. What matters most:” A cultural mechanism moderating structural vulnerability and moral experience of mental illness stigma. Soc. Sci. Med. 2014;103:84–93. doi: 10.1016/j.socscimed.2013.09.009. [DOI] [PubMed] [Google Scholar]
- Zhang Lin. Self-esteem as mediator and moderator of the relationship between stigma perception and social alienation of Chinese adults with disability. Disability and Health Journal. 2014;7(1):119–123. doi: 10.1016/j.dhjo.2013.07.004. [DOI] [PubMed] [Google Scholar]