Abstract
Purpose
Young adults are at high risk for increases in loneliness and mental health problems during the COVID-19 pandemic. The present study examined increases in loneliness in a young adult sample, for whom increases were greater, and association with increases in depression and anxiety.
Method
Data from 564 young adults (ages 22–29, 60.7% women) were collected in January 2020 (pre-pandemic) and April/May 2020 (during pandemic).
Results
Loneliness increased from January to April/May and changes in loneliness were greater for females, those with higher perceived social support in January, and those with greater concerns about the pandemic's social impacts. Depression (but not anxiety) increased during this time with changes in loneliness accounting for much of the increase in depression.
Conclusions
Intervention strategies with young adults need to address loneliness and feelings of reduced social support during this time, especially for those who may have had greater disruption in their social lives.
Keywords: Young adult, COVID-19, Loneliness, Depression, Mental health, USA
Implications and Contribution.
Young adults are at risk for increased loneliness and depression during the COVID-19 pandemic. Screening and interventions targeting loneliness are warranted and may have important downstream effects on mental health, particularly for women, those with social support but may feel distant/less supported during pandemic, and those with pandemic-related social concerns.
The COVID-19 pandemic and resulting mitigation policies (e.g., shelter-in-place) are associated with immediate and unprecedented impacts on multiple facets of life including mental health. This may be especially true for young adults who are undergoing a critical time of interpersonal development, education, and career building. Young adults particularly are at high risk for mental health problems including depression and anxiety during the pandemic [1,2], although most studies have not examined within-person changes from before to during the pandemic.
A time-sensitive priority is understanding mechanisms that account for increases in mental health symptoms [3]. Some studies suggest the prevalence of loneliness has stayed relatively stable, or increased slightly, during the COVID-19 pandemic [2,4], with young adults reporting the highest levels. Cross-sectionally, lonely individuals are nearly 7 times more likely to meet clinical criteria for moderate to severe depression symptoms compared to nonlonely individuals [5]. The present study examined the extent to which loneliness increased during the pandemic, who is at greater risk for increases in loneliness (e.g., gender, social support; COVID-19–specific stressors), and whether loneliness explains increases in depression and anxiety among young adults.
Methods
Participants and procedures
Participants include a community sample of young adults recruited for a longitudinal study on social role transitions and alcohol use in Seattle, WA, in 2015–2016 mainly via social media, newspaper, and community advertisements (see [6]). Study inclusion included being between 18 and 23 years old at screening, drinking alcohol for 1+ times in the past year, living within 60 miles of study offices, and coming in for identification verification and consent. Study procedures include completing a baseline survey, 24 consecutive months of online surveys, and a final online survey 30 months postbaseline (completed on August 2017–July 2018, depending on the enrollment date). Recently, 767 participants (out of 778 who began the monthly survey) were invited to complete two supplemental online assessments in January and April/May 2020 ($15 for completion of each). Completion rates were 75.6% in January (conducted on January 6–30 to get updated contact information, current social role statuses, substance use, and mental health) and 72.0% in April/May (conducted on April 21-May 18 to get an update during the COVID-19 pandemic).
A total of 564 young adults (mean age = 25.1 [standard deviation = 1.9]; 60.7% women; 30% sexual minority; 54.5% white non-Hispanic, 18.8% Asian non-Hispanic, 18.2% other race non-Hispanic, 8.6% Hispanic any race; 70.9% completed 4-year college) were included in the present analyses. The institutional review board of the University of Washington approved the human subjects research, and information statements with all elements of consent were included at the beginning of the January and April/May surveys.
Study measures
Past month loneliness was measured with the three-item Loneliness Scale [7] including feeling “that you lack companionship”, “left out”, and “isolated from others” (α = .80). Past month depression (“Little interest or pleasure in doing things”; “Feeling down, depressed, or hopeless”; α = .88) and anxiety (“Feeling nervous, anxious, or on edge”,“Not being able to stop or control worrying”; α = .88) were measured with the Patient Health Questionnaire-4 [8]. Perceived Social Support was measured with the 12-item Multidimensional Scale of Perceived Social Support [9] in January (mean of 12 items; α = .91) and dichotomized for analyses based on the median of the total score (Low: <55; High: 55+) for ease of interpretation. COVID-19–related social concerns (“making you feel isolated or alone”, “placing a strain on your social life”, “placing a strain on relationships with those you live with”) was assessed in the April/May survey (mean of three items; α = .70) and dichotomized based on the median (low: <1.67; high: 1.67+), again, for ease of interpretation.
Analytic plan
We used mixed-effects models to assess changes in loneliness and mental health outcomes from January to April/May, adjusted for sex, sexual orientation, age in January, dummy codes for race/ethnicity, and education completed as of January. In separate models, we assessed whether changes in loneliness varied by sex, perceived social support in January, and perceived social concerns due to the pandemic by testing interaction terms for study wave by each of these three moderators (e.g., wave-x-sex) in separate models. To assess whether changes in loneliness explained changes in mental health outcomes, we assessed how the parameter for study wave changed when loneliness was further included in models as a time-varying covariate. Analyses were run in R version 3.6 using the “lme4” package [10].
Results
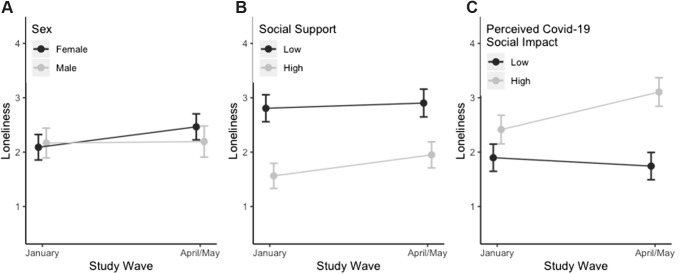
Descriptive statistics for demographic and moderator variables are presented in a Supplemental Table S1 available online. Table 1 shows mean levels of loneliness and mental health outcomes in January and April/May and results for change over time from models. Full model results including coefficients for all covariates are provided in Supplemental Tables S2–S4. There was a statistically significant increase in loneliness from January to April/May. Changes in loneliness appeared to vary significantly by sex, perceived social support, and social concerns related to the pandemic (Figure 1 ). There was a steeper increase in loneliness in females compared to males (interaction-p = .018); in those with higher compared to lower perceived social support in January (interaction-p = .045), although those with lower social support had noticeably higher levels of loneliness at both time points; and in those reporting higher compared to lower levels of concerns about the pandemic's impact on social concerns in April/May (interaction-p <.001).
Table 1.
Mean level of loneliness, depression, and anxiety in January and April/May 2020 and model-based estimates for study wave
| Outcome | January |
April/May |
b or CR | p-value | 95% CI |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||
| Loneliness | 2.26 (1.84) | 2.53 (1.89) | .25 | <.001 | .11, .39 |
| Depression | 1.63 (1.67) | 1.86 (1.59) | 1.13 | .013 | 1.03, 1.24 |
| Anxiety | 2.12 (1.77) | 2.05 (1.76) | .96 | .386 | .88, 1.05 |
CI = confidence interval; SD = standard deviation.
aFor depression and anxiety, a negative binomial distribution was specified to estimate count ratios (CRs) describing the proportional change due to a 1-unit increase in the covariate. Covariates included sex, sexual orientation, age in January, dummy codes for race/ethnicity, and education completed as of January. Range of scores for each of the outcomes was 0–six at each study visit.
Figure 1.
Model-predicted loneliness and 95% confidence intervals in January 2020 and April/May 2020 by (A) sex, (B) perceived social support, and (C) concerns about COVID-19 pandemic on social relationships. Y-axis range reflects 1 standard deviation above and below the mean.
There was a statistically significant increase in depression symptoms. Changes in loneliness appeared to account for much of the increase in depression as the count ratios for study wave was attenuated and no longer statistically significant after inclusion of loneliness in the model (count ratio = 1.07; p-value = .171). There was no statistically significant change in anxiety symptoms over time and, thus, we did not further test the role of loneliness in explaining changes in anxiety.
Discussion
Results indicate loneliness may be an important mechanism for increases in depressive symptoms during this pandemic; not surprising as public health social/physical distancing mandates had an immediate and fundamental shift for Americans' social lives.
Consistent with the findings from national samples [2] but in contrast to others [4], we found small, yet statistically significant, increases in loneliness from January to April/May. Women showed steeper increases in loneliness, as well as young adults who had higher social support in January, and those with greater concerns about COVID-19's impact on their social relationships. It is possible those with stronger social networks had greater disruptions to their social lives, and subsequently felt greater increases in loneliness. However, those with lower social support did report highest levels of loneliness in both January and Spring, suggesting the need for prevention/interventions to directly target social support and feelings of reduced support resulting from the pandemic. The lack of increase in anxiety was unexpected; however, anxiety levels remained elevated at both time points. In both January and April/May, the prevalence of clinically elevated symptoms of anxiety (31.2% and 29.8%, respectively) and depression (22.5% and 25.2%) were higher than national averages with young adults [11]. Note, generalizability may be limited due to the limited racial/ethnic diversity of the study sample, the online recruitment approach, the high proportion of college graduates, and the sample originating from the Pacific Northwest.
The trajectory of worsening loneliness and mental health symptoms, although relatively small, is concerning as the negative behavioral health impacts from pandemic are expected to peak up to 9 months after the initial outbreak [12]. Screening for loneliness and interventions may be warranted to promote well-being and enhance resilience (e.g., adaptive coping strategies; increasing connection and feelings of connectedness while maintaining public health mitigation strategies), which could reduce the possible deleterious impact COVID-19 could have on mental health [3].
Acknowledgments
The authors would like to thank Dr. Devon Abdallah and Rose Lyles-Riebli for their help and coordination in data collection. They would like to thank their colleagues Theresa Walter and Drs. Megan Patrick and Devon Abdallah for their consultation on our measures.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Disclaimer: The content of this manuscript is solely the responsibility of the author(s) and does not necessarily represent the official views of the University of Washington, National Institute on Alcohol Abuse and Alcoholism and the National Institutes of Health.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2020.08.009.
Funding Sources
Data collection and manuscript preparation was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (R01AA022087, PI: C. M. Lee and R01AA027496, PI: C. M. Lee) and funds provided by the University of Washington Department of Psychiatry and Behavioral Sciences and the Arthur Elzey Research Fund to CML. JMC acknowledges partial support from the National Institute on Alcohol Abuse and Alcoholism (R34AA028074).
Supplementary Data
References
- 1.Centers for Disease Control National Center on Health Statistics. Mental health: Household pulse survey. https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm Available at:
- 2.McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holmes E.A., O'Connor R.C., Perry V.H. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luchetti M., Lee J.H., Aschwanden D. The trajectory of loneliness in response to COVID-19. Am Psychol. 2020 doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Killgore W.D., Cloonen S.A., Taylor E.C., Dailey N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290:113117. doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patrick M.E., Rhew I.C., Duckworth J.C. Patterns of young adult social roles transitions across 24 months and subsequent substance use and mental health. J Youth Adolesc. 2020;49:869–880. doi: 10.1007/s10964-019-01134-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res Ageing. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kroenke K., Spitzer R.L., Williams J.B., Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 9.Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. J Pers Assess. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 10.Bates D., Maechler M., Bolker B. 2018. Package ‘lme4’. Version, 1, 17. [Google Scholar]
- 11.Eisenberg D., Golberstein E., Gollust S.E. Help-seeking and access to mental health care in a university student population. MedCare. 2007;45:594–601. doi: 10.1097/MLR.0b013e31803bb4c1. [DOI] [PubMed] [Google Scholar]
- 12.Washington State Department of Health July update: Statewide high-level analysis of forecasted behavioral health impacts from COVID-19. https://www.hca.wa.gov/assets/program/covid-19-statewide-summary-forecast-of-bh-impacts-20200624.pdf Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.