Abstract
This study updates a previous report of the estimated number of excess deaths in the US during the coronavirus disease 2019 (COVID-19) pandemic through August 1, 2020, and describes causes of those deaths and temporal relationships with state lifting of coronavirus restrictions.
Previous studies of excess deaths (the gap between observed and expected deaths) during the coronavirus disease 2019 (COVID-19) pandemic found that publicly reported COVID-19 deaths underestimated the full death toll, which includes documented and undocumented deaths from the virus and non–COVID-19 deaths caused by disruptions from the pandemic.1,2 A previous analysis found that COVID-19 was cited in only 65% of excess deaths in the first weeks of the pandemic (March-April 2020); deaths from non–COVID-19 causes (eg, Alzheimer disease, diabetes, heart disease) increased sharply in 5 states with the most COVID-19 deaths.1 This study updates through August 1, 2020, the estimate of excess deaths and explores temporal relationships with state reopenings (lifting of coronavirus restrictions).
Methods
Death data for 2014-2020 and population counts for the 50 states and the District of Columbia were obtained from the National Center for Health Statistics3,4 and US Census Bureau,5 respectively. Death counts from March 1, 2020, through August 1, 2020, were taken from provisional, unweighted data released on September 9, 2020.3 Connecticut and North Carolina were excluded due to missing data. A hierarchical Poisson regression model, described elsewhere,1 was used to predict expected deaths based on historic norms. COVID-19 deaths included those in which COVID-19 was cited as an underlying or contributing cause. Data for deaths not attributed to COVID-19 were only available for underlying causes of death, including Alzheimer disease, heart disease, and 10 other grouped causes, defined elsewhere.1 Reopening dates were obtained from the New York Times.6
To confirm the validity of observed increases in non–COVID-19 deaths, the Joinpoint regression program (version 4.8.0.1; Statistical Research and Applications Branch, National Cancer Institute) was used to specify the weeks (joinpoints) when slopes changed (as measured by the annual percentage change [APC]) and their statistical significance (2-sided test, .05 threshold). To estimate dispersion in the epidemic curve for each state, the number of consecutive weeks during which 90% of excess deaths occurred (ED90) was calculated. All calculations were performed in SAS (version 9.4; SAS Institute) and R (version 3.6.1; The R Foundation).
Results
Between March 1 and August 1, 2020, 1 336 561 deaths occurred in the US, a 20% increase over expected deaths (1 111 031 [95% CI, 1 110 364 to 1 111 697]). The 10 states with the highest per capita rate of excess deaths were New York, New Jersey, Massachusetts, Louisiana, Arizona, Mississippi, Maryland, Delaware, Rhode Island, and Michigan. The states with the highest per capita rate of excess deaths changed from week to week (Video). The increase in absolute deaths in these states relative to expected values ranged from 22% in Rhode Island and Michigan to 65% in New York (Table). Three states with the highest death rates (New Jersey, New York, and Massachusetts) accounted for 30% of US excess deaths but had the shortest epidemics (ED90 < 10 weeks). States that experienced acute surges in April (and reopened later) had shorter epidemics that returned to baseline in May, whereas states that reopened earlier experienced more protracted increases in excess deaths that extended into the summer (Figure).
Table. Excess Deaths From March 1, 2020, to August 1, 2020, US and Selected States.
| Jurisdiction | Expected deaths (95% CI)a | Observed deaths (ratio of observed/expected) | Excess deaths | COVID-19 deathsb | Excess deaths attributed to COVID-19, %b | ED90 | |
|---|---|---|---|---|---|---|---|
| No. (95% CI) | Mortality rate per 100 000 population | ||||||
| United Statesc | 1 111 031 (1 110 364-1 111 697) | 1 336 561 (1.20) | 225 530 (224 864 to 226 197) | 72 | 150 541 | 67 | 18 |
| Alabama | 21 236 (21 148-21 325) | 25 172 (1.19) | 3936 (3847 to 4024) | 81 | 2071 | 53 | 17 |
| Alaska | 1823 (1809-1837) | 1851 (1.02) | 28 (14 to 42) | 4 | 0 | 0 | 18 |
| Arizona | 25 309 (25 209-25 409) | 32 780 (1.30) | 7471 (7371 to 7571) | 104 | 3933 | 53 | 17 |
| Arkansas | 13 105 (13 040-13 169) | 14 326 (1.09) | 1221 (1157 to 1286) | 41 | 585 | 48 | 16 |
| California | 110 296 (110 069-110 524) | 127 298 (1.15) | 17 002 (16 774 to 17 229) | 43 | 10 388 | 61 | 18 |
| Colorado | 16 615 (16 539-16 692) | 19 479 (1.17) | 2864 (2787 to 2940) | 50 | 1782 | 62 | 17 |
| Delaware | 3752 (3727-3777) | 4651 (1.24) | 899 (874 to 924) | 93 | 482 | 54 | 18 |
| District of Columbia | 2521 (2503-2540) | 3428 (1.36) | 907 (888 to 925) | 129 | 675 | 74 | 14 |
| Florida | 87 139 (86 935-87 343) | 101 389 (1.16) | 14 250 (14 046 to 14 454) | 67 | 8517 | 60 | 17 |
| Georgia | 35 149 (35 027-35 270) | 41 107 (1.17) | 5958 (5837 to 6080) | 57 | 3830 | 64 | 18 |
| Hawaiid | 4881 (4850-4913) | 4828 (0.99) | −53 (−85 to −22) | −4 | 0 | 0 | 17 |
| Idaho | 5819 (5783-5855) | 6377 (1.10) | 558 (522 to 594) | 32 | 178 | 32 | 19 |
| Illinois | 43 413 (43 276-43 550) | 54 014 (1.24) | 10 601 (10 464 to 10 738) | 83 | 7037 | 66 | 16 |
| Indiana | 27 441 (27 337-27 545) | 31 250 (1.14) | 3809 (3705 to 3913) | 57 | 2991 | 79 | 16 |
| Iowa | 12 410 (12 348-12 472) | 13 416 (1.08) | 1006 (944 to 1068) | 32 | 922 | 92 | 16 |
| Kansas | 10 892 (10 836-10 948) | 11 545 (1.06) | 653 (597 to 709) | 22 | 394 | 60 | 18 |
| Kentucky | 19 687 (19 603-19 772) | 21 280 (1.08) | 1593 (1508 to 1677) | 36 | 815 | 51 | 18 |
| Louisiana | 18 974 (18 891-19 056) | 24 026 (1.27) | 5052 (4970 to 5135) | 108 | 3820 | 76 | 18 |
| Maine | 6144 (6107-6181) | 6273 (1.02) | 129 (92 to 166) | 10 | 64 | 50 | 18 |
| Maryland | 20 282 (20 196-20 368) | 26 091 (1.29) | 5809 (5723 to 5895) | 96 | 3859 | 66 | 16 |
| Massachusetts | 24 301 (24 205-24 397) | 32 562 (1.34) | 8261 (8165 to 8357) | 120 | 7886 | 95 | 9 |
| Michigan | 40 057 (39 926-40 188) | 48 854 (1.22) | 8797 (8666 to 8928) | 88 | 5866 | 67 | 15 |
| Minnesota | 18 633 (18 550-18 715) | 20 530 (1.10) | 1897 (1815 to 1980) | 34 | 1635 | 86 | 14 |
| Mississippi | 12 885 (12 821-12 949) | 15 989 (1.24) | 3104 (3040 to 3168) | 104 | 1753 | 56 | 17 |
| Missouri | 26 409 (26 308-26 510) | 28 580 (1.08) | 2171 (2070 to 2272) | 35 | 1280 | 59 | 18 |
| Montana | 4297 (4269-4325) | 4379 (1.02) | 82 (54 to 110) | 8 | 26 | 32 | 21 |
| Nebraska | 6911 (6871-6952) | 7447 (1.08) | 536 (495 to 576) | 28 | 315 | 59 | 17 |
| Nevada | 10 799 (10 743-10 856) | 12 194 (1.13) | 1395 (1338 to 1451) | 46 | 888 | 64 | 17 |
| New Hampshire | 5025 (4993-5057) | 5694 (1.13) | 669 (637 to 701) | 49 | 373 | 56 | 17 |
| New Jersey | 30 044 (29 934-30 153) | 48 048 (1.60) | 18 004 (17 895 to 18 114) | 202 | 14 043 | 78 | 9 |
| New Mexico | 7590 (7546-7633) | 8771 (1.16) | 1181 (1138 to 1225) | 56 | 671 | 57 | 16 |
| New York | 62 948 (62 779-63 116) | 103 811 (1.65) | 40 863 (40 695 to 41 032) | 209 | 31 996 | 78 | 8 |
| North Dakota | 2989 (2968-3010) | 3144 (1.05) | 155 (134 to 176) | 20 | 60 | 39 | 15 |
| Ohio | 49 491 (49 344-49 638) | 55 946 (1.13) | 6455 (6308 to 6602) | 55 | 3379 | 52 | 18 |
| Oklahoma | 15 448 (15 376-15 520) | 17 189 (1.11) | 1741 (1669 to 1813) | 44 | 639 | 37 | 19 |
| Oregon | 15 094 (15 023-15 165) | 16 217 (1.07) | 1123 (1052 to 1194) | 27 | 338 | 30 | 20 |
| Pennsylvania | 53 964 (53 809-54 118) | 63 070 (1.17) | 9106 (8952 to 9261) | 71 | 7595 | 83 | 14 |
| Rhode Islande | 4299 (4271-4327) | 5239 (1.22) | 940 (912 to 968) | 89 | 979 | 104 | 12 |
| South Carolina | 20 479 (20 392-20 566) | 24 488 (1.20) | 4009 (3922 to 4096) | 79 | 1877 | 47 | 19 |
| South Dakota | 3368 (3345-3391) | 3549 (1.05) | 181 (158 to 204) | 21 | 103 | 57 | 20 |
| Tennessee | 30 810 (30 698-30 922) | 33 999 (1.10) | 3189 (3077 to 3301) | 47 | 1191 | 37 | 19 |
| Texas | 83 179 (82 982-83 376) | 100 951 (1.21) | 17 772 (17 575 to 17 969) | 62 | 10 026 | 56 | 16 |
| Utah | 7865 (7820-7910) | 8818 (1.12) | 953 (908 to 998) | 30 | 311 | 33 | 20 |
| Vermont | 2383 (2366-2400) | 2561 (1.07) | 178 (161 to 195) | 28 | 31 | 17 | 20 |
| Virginia | 28 020 (27 915-28 126) | 32 582 (1.16) | 4562 (4456 to 4667) | 54 | 2394 | 52 | 19 |
| Washington | 23 393 (23 299-23 487) | 25 803 (1.10) | 2410 (2316 to 2504) | 32 | 1505 | 62 | 19 |
| West Virginia | 9332 (9282-9383) | 9495 (1.02) | 163 (112 to 213) | 9 | 74 | 46 | 17 |
| Wisconsin | 22 212 (22 120-22 305) | 23 991 (1.08) | 1779 (1686 to 1871) | 31 | 964 | 54 | 19 |
| Wyoming | 1919 (1904-1933) | 2079 (1.08) | 160 (146 to 175) | 28 | 0 | 0 | 18 |
Abbreviations: COVID-19, coronavirus disease 2019; ED90, number of consecutive weeks during which 90% of total excess deaths occurred.
Seasonally adjusted death counts predicted by regression model.
COVID-19 deaths include deaths in which COVID-19 was identified as the underlying cause of death or a contributing cause (among multiple causes).
The US total was calculated as the sum of results for 48 states and the District of Columbia. Data for Connecticut and North Carolina were omitted because of delays in reporting.
Hawaii experienced “negative” excess deaths because observed deaths were lower than would be predicted based on historic norms.
Likely due to observed deaths being less than predicted, COVID-19 deaths in Rhode Island exceeded the estimate for excess deaths.
Figure. Excess Deaths From March to July 2020 in Selected States.
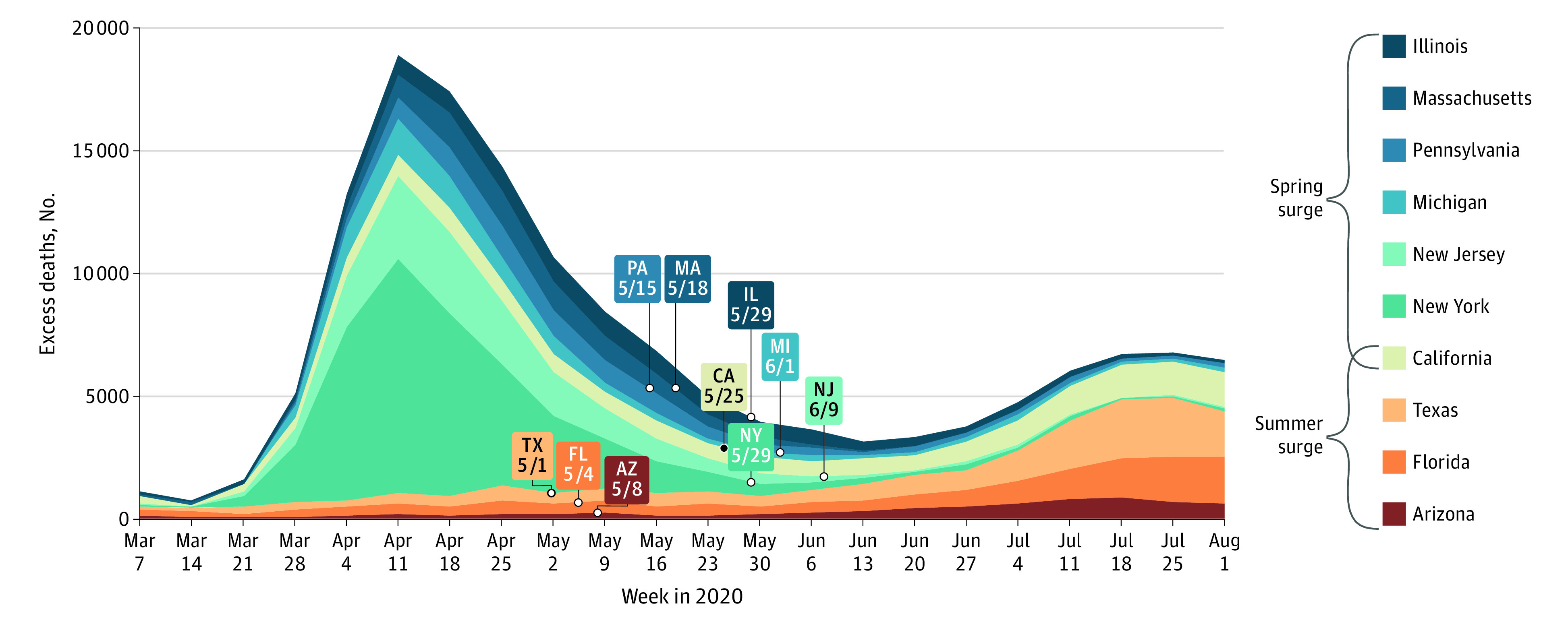
The figure plots weekly excess deaths for the 10 states with the largest number of excess deaths during March-July 2020. Reopening dates refer to the lifting of broad coronavirus disease 2019 restrictions, as reported by the New York Times.6
Video. What States Have Had the Highest Rate of Excess Deaths During the COVID-19 Pandemic?
The animation shows the number of excess deaths (per 100 000 people) that occurred in the US between March and July 2020. Excess deaths are deaths that surpass what is expected based on historical norms. The states with the highest rates of excess deaths have changed from week to week but were generally concentrated in the northeast in the spring and across the sunbelt in the summer. Calculations are based on death counts obtained on September 9, 2020.
Of the 225 530 excess deaths, 150 541 (67%) were attributed to COVID-19. Joinpoint analyses revealed an increase in deaths attributed to causes other than COVID-19, with 2 reaching statistical significance. US mortality rates for heart disease increased between weeks ending March 21 and April 11 (APC, 5.1 [95% CI, 0.2-10.2]), driven by the spring surge in COVID-19 cases. Mortality rates for Alzheimer disease/dementia increased twice, between weeks ending March 21 and April 11 (APC, 7.3 [95% CI, 2.9-11.8]) and between weeks ending June 6 and July 25 (APC, 1.5 [95% CI, 0.8-2.3]), the latter coinciding with the summer surge in sunbelt states.
Discussion
Although total US death counts are remarkably consistent from year to year, US deaths increased by 20% during March-July 2020. COVID-19 was a documented cause of only 67% of these excess deaths. Some states had greater difficulty than others in containing community spread, causing protracted elevations in excess deaths that extended into the summer. US deaths attributed to some noninfectious causes increased during COVID-19 surges. Excess deaths attributed to causes other than COVID-19 could reflect deaths from unrecognized or undocumented infection with severe acute respiratory syndrome coronavirus 2 or deaths among uninfected patients resulting from disruptions produced by the pandemic. Study limitations include the reliance on provisional data, inaccuracies in death certificates, and assumptions applied to the model.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324(5):510-513. doi: 10.1001/jama.2020.11787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinberger DM, Chen J, Cohen T, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. Published online July 1, 2020. doi: 10.1001/jamainternmed.2020.3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Weekly counts of deaths by state and select causes, 2014-2018. Accessed June 10, 2020. https://data.cdc.gov/NCHS/Weekly-Counts-of-Deaths-by-State-and-Select-Causes/3yf8-kanr
- 4.Centers for Disease Control and Prevention Weekly counts of deaths by state and select causes, 2019-2020. Accessed September 9, 2020. https://data.cdc.gov/NCHS/Weekly-Counts-of-Deaths-by-State-and-Select-Causes/muzy-jte6
- 5.US Census Bureau American Community Survey: table B01003. Accessed May 15, 2020. https://data.census.gov/cedsci/table?q=b01003&g=0100000US.04000.001&tid=ACSDT1Y2018.B01003
- 6.Lee JC, Mervosh S, Harvey B, Matthews AL. See how all 50 states are reopening (and closing again). New York Times Accessed September 11, 2020. https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html


