Abstract
OBJECTIVE
There is sparse evidence for the association of suitable food substitutions for red and processed meat on the risk of type 2 diabetes. We modeled the association between replacing red and processed meat with other protein sources and the risk of type 2 diabetes and estimated its population impact.
RESEARCH DESIGN AND METHODS
The European Prospective Investigation into Cancer (EPIC)-InterAct case cohort included 11,741 individuals with type 2 diabetes and a subcohort of 15,450 participants in eight countries. We modeled the replacement of self-reported red and processed meat with poultry, fish, eggs, legumes, cheese, cereals, yogurt, milk, and nuts. Country-specific hazard ratios (HRs) for incident type 2 diabetes were estimated by Prentice-weighted Cox regression and pooled using random-effects meta-analysis.
RESULTS
There was a lower hazard for type 2 diabetes for the modeled replacement of red and processed meat (50 g/day) with cheese (HR 0.90, 95% CI 0.83–0.97) (30 g/day), yogurt (0.90, 0.86–0.95) (70 g/day), nuts (0.90, 0.84–0.96) (10 g/day), or cereals (0.92, 0.88–0.96) (30 g/day) but not for replacements with poultry, fish, eggs, legumes, or milk. If a causal association is assumed, replacing red and processed meat with cheese, yogurt, or nuts could prevent 8.8%, 8.3%, or 7.5%, respectively, of new cases of type 2 diabetes.
CONCLUSIONS
Replacement of red and processed meat with cheese, yogurt, nuts, or cereals was associated with a lower rate of type 2 diabetes. Substituting red and processed meat by other protein sources may contribute to the prevention of incident type 2 diabetes in European populations.
Introduction
Type 2 diabetes is a major public health challenge, and its prevalence is projected to increase from 463 million in 2019 to 700 million by 2045 (1). One key modifiable risk factor in the prevention of type 2 diabetes is diet (2). Most dietary recommendations to prevent type 2 diabetes advise that intake of red and processed meat should be limited, mainly based on evidence from cohort studies (3–5), including the multicountry European Prospective Investigation into Cancer (EPIC)-InterAct study (6). However, few studies have quantified the risk associated with replacement of red and processed meat by other food sources of protein (5). Other food sources of protein in European diets include poultry, fish, cheese, yogurt, milk, eggs, legumes, nuts, and cereals (7). A previous study reported that replacing red and processed red meat with poultry, low-fat dairy, whole grains, or nuts was associated with a lower risk of type 2 diabetes in three U.S. cohorts of health professionals (8). This study did not investigate different types of dairy products (cheese, yogurt, milk), eggs, or legumes.
We aimed to investigate the impact of replacing red and processed meat with other food sources of protein (poultry, fish, cheese, yogurt, milk, eggs, legumes, nuts, and cereals) on the development of type 2 diabetes. Moreover, we estimated the population-attributable fraction for replacements associated with lower rates of type 2 diabetes. Lastly, based on previous findings (9,10), we estimated the contribution of body iron storage (serum ferritin) as a potential mediator.
Research Design and Methods
The EPIC-InterAct Study
Study Population
EPIC-InterAct is a case-cohort study nested within the EPIC cohort (11). A detailed description of the study design has previously been published (12). In brief, the EPIC-InterAct study identified type 2 diabetes cases among study participants from eight countries (France, Italy, Spain, the U.K., the Netherlands, Germany, Sweden, and Denmark) included in EPIC with available blood samples (n = 340,234 [3.99 million person-years of follow-up from 1991 to 2007]). After exclusion of prevalent cases of type 2 diabetes at baseline (n = 548), the study included 12,403 verified cases of incident type 2 diabetes and 16,154 participants in a representative subcohort, including, by design, an overlap of 778 incident type 2 diabetes cases. After we excluded participants in the bottom and top 1% of the energy intake–to–requirement ratio (n = 619) and those with missing information on dietary data (n = 736), education (n = 330), physical activity (n = 385), and BMI (n = 197), a total of 15,450 participants in the subcohort and 11,741 type 2 diabetes cases were included in this analysis (Supplementary Fig. 1). All participants gave written informed consent, and the study was approved by the local ethics committees in the participating countries and the Internal Review Board of the International Agency for Research on Cancer.
Dietary Assessment
Habitual dietary intake for the 12 months before entering the study was assessed using self- or interviewer-administered country-specific food-frequency questionnaires (FFQs) or diet history interviews (11,13). Further information on dietary assessment methods and correlation coefficients for protein and food sources of protein from validation studies can be found in Supplementary Table 1. The questionnaires were used to estimate the average daily intake of foods and nutrients. A single 24-h dietary recall was collected from an 8% random sample of participants from each country.
We considered the following food sources of protein: red meat, processed meat, poultry, fish, cheese, yogurt, milk, eggs, nuts, legumes, and cereals. Cereal consumption was included, as this food group was the largest nonanimal food source of protein in EPIC (7). Definitions of individual foods groups are in Supplementary Table 2.
Portion sizes were designated as 200 g/day for milk; 70 g/day for yogurt; 50 g/day for red and processed meat, poultry, fish, eggs, and legumes; 30 g/day for cheese and cereals; and 10 g/day for nuts—all based on previously reported serving sizes or intake ranges from the EPIC-InterAct study (6,14–16). As information on servings was not available for legumes and cereals, we used those in recent meta-analyses (17,18).
Type 2 Diabetes Ascertainment
Multiple sources of information from each EPIC study center were used to ascertain type 2 diabetes cases including self-report and linkage to primary care, secondary care, drug, hospital admission, and mortality data as previously described (12). Cases identified from only one independent source were verified through at least one other source, including medical records. Because cases in Denmark and Sweden were ascertained using local and national diabetes registers, these cases were considered verified. Follow-up was censored at the date of diagnosis, loss to follow-up, death, or 31 December 2007—whichever came first.
Covariate Assessment
Data on lifestyle and medical history were obtained from self-administered questionnaires at baseline including education, physical activity, smoking, and alcohol. Physical activity was classified according to the Cambridge Physical Activity Index. Validity of the index was assessed against objectively measured energy expenditure (19). Height, weight, and waist circumference were measured by trained personnel using standardized protocols during a clinic visit at baseline in all study centers, except Oxford (U.K.) and centers in France, which obtained self-reported measures. Waist circumference was not available in Umeå (Sweden). BMI was calculated as weight in kilograms divided by the square of height in meters. History of prevalent cancer, myocardial infarction, stroke, angina, hypertension, or hyperlipidemia was based on self-report.
At baseline, clinic visit blood samples were collected and stored at −196°C (−150°C in Denmark and −80°C in Sweden) at the coordinating center or local biorepositories. Serum (except for plasma in Umeå) ferritin, as a marker of body iron storage, was analyzed at SHL-Groep, Etten-Leur, the Netherlands, using cobas (Roche Diagnostics, Mannheim, Germany) assays (electrochemiluminescence immunoassay sandwich principle) on a Roche Hitachi Modular P analyzer. The assay range was 0.5–2,000.0 μg/L. Cobas assays were also used to measure hs-CRP (20).
Statistical Analysis
Standard descriptive statistics were used to summarize baseline characteristics for the total subcohort and those with incident type 2 diabetes. We have previously reported the baseline characteristics of the study population across quintiles of meat intake in the subcohort (6).
The modeled associations of replacing red meat with the other protein sources were estimated with Prentice-weighted Cox regression models. The models were fitted separately by country and were used to estimate hazard ratios (HRs) and 95% CIs for the replacement of red and processed meat by other food sources of protein. Then, country-specific estimates were pooled using random-effects meta-analysis, and between-country heterogeneity was quantified using the I2 statistic.
We adjusted for a range of covariates in a series of models. Model 1 adjustments included age (timescale), study center (two to six centers in each country), energy intake (kcal/day [continuous]), sex (stratified by baseline hazard function), education (none, primary school, secondary school, longer including university), physical activity (inactive, moderate inactive, moderately active, active), smoking status (never, former, current, unknown), and alcohol intake (g/day [two continuous terms for a nonlinear relationship based on three-knots restricted cubic spline function]). In model 2, we further adjusted for dietary variables including fruit, vegetables (excluding legumes), sweets, soft drinks, coffee, and tea and intake of other dairy products (e.g., cream desserts and dairy creams) (all in g/day [continuous]). In model 3 (specified as the main model), we further adjusted for BMI (kg/m2 [continuous]). In a further model, we also adjusted for self-reported history of hypertension (yes, no, unknown), self-reported history of dyslipidemia (yes, no, unknown), and waist circumference (cm [continuous]).
The modeled association of each food replacement was estimated as follows using multivariable-adjusted regression. We first obtained regression coefficients (i.e., log HRs) per 1 serving/day for red and processed meat and each of the other food sources of protein (i.e., poultry, fish, cheese, yogurt, milk, eggs, legumes, nuts, and cereals). Then, we calculated the difference between the two coefficients, accounting for their variance and covariance, and exponentiated the difference to estimate the HR for each specific replacement of interest (21). Analyses were also performed excluding participants who consumed <10 g/day red and processed meat. Additionally, replacements of red meat and processed meat were evaluated separately.
To investigate sources of heterogeneity between countries, we performed separate analyses in Northern and Southern Europe. We were not able to differentiate between intake of refined and whole grains; therefore, in an exploratory analysis we stratified the replacement of red and processed meat with cereals by high and low intake of dietary fiber from cereals divided at the median of the subcohort, i.e., 8 g/day. Based on previous findings (6), we also stratified the replacement of red and processed meat with poultry analysis by sex.
One of the mechanisms by which a high intake of red and processed meat may be associated with development of type 2 diabetes is through its high content of heme iron (22). We compared substitution models with and without adjustment for ferritin, a marker of body iron storage, using a one-sided Wald test (23), separately for model 2 and 3 (without and with adjustment for BMI, respectively) among those with measured ferritin levels. Because ferritin is an acute-phase reactant and could therefore be elevated due to systemic inflammation, we additionally adjusted model 3 for hs-CRP, a marker of systemic inflammation (24). To quantify the extent to which ferritin explained the lower incidence rate (IR) arising from each replacement, we calculated: (HRreplacement not adjusted − HRreplacement adjusted for ferritin) / (HRreplacement not adjusted − 1). A bootstrapping procedure (1,000 replicates) was used to derive 95% CIs.
In sensitivity analyses, we 1) excluded participants with cancer, myocardial infarction, stroke, angina, and self-reported hypertension and/or hyperlipidemia at baseline; 2) excluded cases that occurred during the first 2 years of observation, due to concerns about reverse causation; 3) excluded individuals with HbA1c levels ≥6.5% (equivalent to 48 mmol/mol) measured at the baseline visit; and 4) applied regression calibration to all dietary intakes due to possible measurement error in self-reported dietary intakes. We regressed intakes from the 24-h dietary recalls on those from the FFQs in a multivariable-adjusted linear mixed model with country as a random effect. The HRs were then corrected by dividing the log HRs by the regression dilution ratio. Uncertainty in the calibration model was accounted for by sampling a set of five values using a multiple imputation approach. Corrected log HRs and SEs were calculated and pooled using Rubin’s rules (25). 5) We also estimated replacements per 5 g protein from each source of protein.
We estimated the population attributable fraction for the modeled replacements associated with a lower hazard of type 2 diabetes in the subcohort, under the assumption of causality, to investigate how much of the incidence of type 2 diabetes could be preventable by replacing red and processed meat with another protein source. The population attributable fraction was calculated as the difference between the predicted IR for the overall subcohort and the predicted IR for the relevant replacements divided by the overall IR (i.e., [IRsubcohort − IRreplacement] / [IRsubcohort]). All IRs were adjusted for model 3 covariates, and 95% CIs were derived using a bootstrap procedure with 1,000 replications. All analyses were performed in Stata 15.1 (StataCorp, College Station, TX).
Results
The median follow-up time was 12.3 years. Table 1 shows the baseline characteristics of the subcohort and those with type 2 diabetes. Participants with type 2 diabetes were older and more likely to be men, have a lower education level, be physically inactive, smoke, and have a higher BMI and higher levels of serum ferritin compared with subcohort participants. Those with type 2 diabetes had a slightly higher intake of red and processed meat and soft drinks and a lower intake of yogurt, sweets, and fruits.
Table 1.
Baseline characteristics of the EPIC-InterAct case-cohort study (n = 26,460)
| Subcohort | Participants with type 2 diabetes | |
|---|---|---|
| (n = 15,450) | (n = 11,741) | |
| Characteristics | ||
| Age, years | 53 (47–59) | 56 (50–61) |
| Women, % | 62 | 50 |
| Lower education level, % | 41 | 51 |
| Physically inactive, % | 24 | 30 |
| Smoker, % | 26 | 28 |
| BMI, kg/m2 | 26 (23–28) | 29 (26–32) |
| Foods, g/day | ||
| Red and processed meat | 74 (46–108) | 84 (53–121) |
| Red meat | 38 (19–65) | 43 (23–71) |
| Processed meat | 28 (15–49) | 32 (17–56) |
| Poultry | 16 (7–31) | 16 (7–32) |
| Fish | 29 (15–52) | 32 (16–55) |
| Cheese | 28 (14–51) | 26 (12–49) |
| Yogurt | 26 (0–97) | 20 (0–88) |
| Milk | 165 (45–301) | 170 (47–321) |
| Eggs | 15 (7–25) | 16 (7–28) |
| Legumes | 5 (0–23) | 4 (0–20) |
| Nuts | 1 (0–3) | 0 (0–2) |
| Cereals | 197 (140–273) | 197 (137–273) |
| Other dairy | 6 (0–24) | 5 (0–21) |
| Sweets | 71 (40–112) | 65 (35–110) |
| Soft drinks | 3 (0–66) | 10 (0–92) |
| Fruit | 193 (103–315) | 182 (96–307) |
| Vegetables (excluding legumes) | 155 (101–239) | 149 (95–234) |
| Coffee | 270 (90–525) | 287 (90–536) |
| Tea | 3 (0–197) | 0 (0–119) |
| Nutrients | ||
| Total energy intake, kcal/day | 2,057 (1,679–2,515) | 2,084 (1,685–2,575) |
| Alcohol, g/day* | 8 (2–20) | 8 (2–22) |
| Alcohol abstainers, % | 8 | 10 |
| Dietary fiber, g/day | 22 (17–27) | 22 (19–27) |
| Serum ferritin, µg/L | 82 (39–156) | 132 (65–242) |
Data are median (interquartile range) unless otherwise indicated.
Only in consumers, n = 14,264 in subcohort and n = 10,626 in participants with type 2 diabetes.
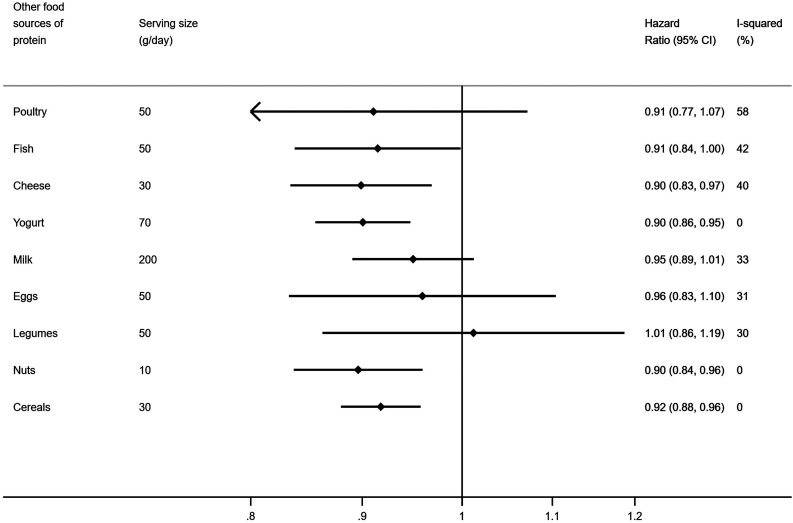
Modeled replacement of red and processed meat with cheese, yogurt, nuts, or cereals was associated with lower hazard of type 2 diabetes (Fig. 1 and Supplementary Fig. 2). Replacing red and processed meat with fish also suggested a lower rate of type 2 diabetes (HR 0.91, 95% CI 0.84–1.00; P = 0.046), and a similar point estimate was observed for poultry but with wider CIs (0.91, 0.77–1.07). Replacing red and processed meat with milk, eggs, or legumes was not significantly associated with type 2 diabetes risk. Additional adjustment for BMI attenuated most of the associations with type 2 diabetes, particularly the replacement of red and processed meat with legumes (model 2, 0.88, 0.80–0.96, and model 3, 1.01, 0.86–1.19). Patterns of associations similar to those in the main analysis were observed after exclusion of those with very low consumption of red and processed meat (n = 739) (data not shown) and when red meat and processed meat were replaced separately (Supplementary Fig. 3). Replacing processed meat with fish was associated with a lower hazard of type 2 diabetes (0.82, 0.71–0.94), whereas replacing red meat with fish was not (0.95, 0.86–1.04).
Figure 1.
The estimated association of replacing red and processed meat (per 50 g/day) with other food sources of protein and the incidence of type 2 diabetes in the EPIC-InterAct case-cohort study (n total = 26,460, n cases of type 2 diabetes = 11,741). Country-specific estimates were obtained and combined using random effects meta-analysis. Adjustment for age (underlying timescale), sex, center, education, physical activity, smoking status, total energy intake, alcohol consumption, fruit, vegetables, sweets, soft drinks, coffee, tea, other dairy products, and BMI.
There was heterogeneity between countries for the replacement of red and processed meat with poultry or fish (Supplementary Fig. 2). This was not explained by European region (i.e., north and south Europe) (Supplementary Fig. 4). Stratification by sex for the replacement of red and processed meat with poultry showed associations in different directions for men and women (men, 0.74, 0.59–0.93, and women 1.16, 0.89–1.52; P for interaction 0.04). After stratification of the replacement of red and processed meat with cereals by high or low cereal fiber, we found no substantial differences between strata (Supplementary Fig. 5).
Adjustment for ferritin attenuated the estimated HRs for all replacement analyses, with and without adjustment for BMI (Supplementary Table 3). Further adjustment for hs-CRP did not change the results (data not shown). Of the lower IR observed for replacement of red and processed meat with cheese, yogurt, nuts, and cereals, 22.1–31.8% was explained by serum ferritin (Fig. 2).
Figure 2.
Estimated % of the association between replacement of red and processed meat with other food sources of protein and risk of type 2 diabetes that is explained by serum ferritin (n total = 24,611, n cases of type 2 diabetes = 10,769). CIs were derived from a bootstrap procedure using 1,000 replicates. HRs on which these estimates are based were estimated from Prentice-weighted Cox regression models with adjustment for age (underlying timescale), sex, center, country, education, physical activity, smoking status, total energy intake, alcohol consumption, fruit, vegetables, sweets, soft drinks, coffee, tea, other dairy products, and BMI. Serving sizes were 70 g/day for yogurt, 50 g/day for red and processed meat, 30 g/day for cheese and cereals, and 10 g/day for nuts. Estimated % of association explained was calculated as follows: [(HRwithout − HRwith) / (HRwithout − 1)] ∗ 100.
Across all sensitivity analyses, a pattern of associations was observed similar to that observed in the main analysis (Supplementary Fig. 6) except for replacement with 5 g protein/day from cereals, which was not associated with diabetes risk (HR 0.99, 95% CI 0.94–1.04) (Supplementary Fig. 7). The population attributable fraction for the modeled replacement of 1 serving/day of red and processed meat with 1 serving/day of cheese, yogurt, or nuts was 7.5–8.8% of participants with type 2 diabetes in our study (Table 2). For cereals, the CI was wide and included zero.
Table 2.
Population attributable fraction for type 2 diabetes calculated in the subcohort (n total = 15,450) of the InterAct study
| Other food sources of protein to replace red and processed meat with* | Population attributable fraction (95% CI)† |
|---|---|
| Cheese | 8.8% (3.1 to 13.6) |
| Yogurt | 8.3% (3.3 to 12.7) |
| Nuts | 7.5% (3.3 to 11.3) |
| Cereals | 17.1% (−6.7 to 33.3) |
Serving sizes were 200 g/day for milk; 70 g/day for yogurt; 50 g/day for red and processed meat, poultry, fish, eggs, and legumes; 30 g/day for cheese and cereals; and 10 g/day for nuts.
CIs were derived from a bootstrap procedure of the difference between the predicted IR for the overall subcohort and the predicted IR for the relevant replacements divided by the overall IR using 1,000 replicates.
Conclusions
In this large case-cohort study across eight European countries, we used substitution modeling and estimated that replacing red and processed meat with cheese, yogurt, nuts, or cereals was significantly associated with a lower rate of type 2 diabetes, whereas replacing red and processed meat with poultry, fish, milk, eggs, or legumes was not. Mediation analysis suggested that these associations were partially mediated by body iron storage as assessed by serum ferritin levels. If we assume causality, 7.5–8.8% of the observed cases of type 2 diabetes could have been prevented if all participants replaced 1 serving/day of red and processed meat with 1 serving/day of cheese, yogurt, or nuts.
This prospective case-cohort study included individuals from geographically diverse populations across Europe. Because of specification of modeled food substitutions, the results allow a clear interpretation for public health and healthful selection of other protein sources as alternatives to red and processed meat for the primary prevention of type 2 diabetes. The serving sizes in grams per day were based on previous literature and study intake ranges. The difference in energy content between the substituted foods may leave an unspecified energy substitution (for instance, the energy difference between 50 g red meat and 30 g cheese) that must be compensated for by other foods not in the model. However, serving size information in grams per day is likely to be more readily understood than information in units of energy percent or kilocalories per day. All replacements may not be applicable to a single meal setting; rather, replacements may be applicable to longer-term average replacements in the habitual diet. For instance, replacing 50 g red meat with 10 g nuts in a single meal may not be realistic. Dietary intake information was obtained from cohort-specific semi-quantitative FFQs or diet history interviews across eight different European countries. This provided greater variation in intakes than in studies that included participants from a single country. Still, intake of nuts was generally low, which highlights the importance of a cautious interpretation.
A limitation of the current study is that the food substitutions were inferred based on a statistical model that compared individuals with different average intakes while no one actively changed their diet. Conducting randomized controlled trials of foods for long-term health end points such as type 2 diabetes is not practical, and in their absence, well-conducted prospective studies that not only assess associations of food intake but also model food substitutions can be helpful. We also acknowledge the limitation of our use of a single measure of diet and covariates, and we were not able to examine changes over time. Nevertheless, our results are consistent with those from studies modeling repeated measures of red and processed meat intake as either average intake or dietary changes (8,26). Self-reported dietary measures are prone to error. While we observed similar patterns of associations after regression calibration against a single 24-h recall, errors due to self-reporting, covariate measurement errors, and confounding due to unmeasured factors may bias our findings in either direction. Type 2 diabetes cases were verified in our study, and the risk of misclassification was low. Analysis excluding undiagnosed diabetes at baseline showed similar patterns of associations.
There is limited evidence from prospective studies about the effects of replacing red and processed meat with other protein sources on incident type 2 diabetes. Pan et al. (8) found that replacing red and processed red meat with nuts, low-fat dairy, whole grains, poultry, and fish was associated with a lower risk of type 2 diabetes. We found that the HRs for replacing red and processed meat with fish or poultry were similar in magnitude to the estimates for cheese, yogurt, nuts, and cereals but with wider CIs and not statistically significant. When replacing processed meat with fish, but not when replacing unprocessed red meat with fish, we observed a lower rate of type 2 diabetes. Also, we found that replacing red and processed meat with poultry was associated with a lower diabetes rate in men but not in women. The reasons for these differences by sex are unclear, but we may speculate that differences in preparation methods and types of red and processed meat as well as poultry and fish consumed by men and women in different countries may contribute, though we were unable to test this in our study. We found that replacing red and processed meat with fermented dairy products, such as yogurt and cheese, but not with milk, was associated with a lower rate of type 2 diabetes. Neither prior reports from U.S.-based cohorts (8) nor our current study is able to clarify whether the type of dairy product (such as fermented or not) or specifically its nutrient content is more important for type 2 diabetes risk.
To our knowledge, no previous study has investigated the association of replacing red and processed meat with eggs or legumes and the development of type 2 diabetes. Other cohort studies, that have not specified food substitutions, have suggested that intake of eggs was not associated with risk of type 2 diabetes in Europe or Asia but positively associated with risk in the U.S., with significant heterogeneity by region (27). Legume intake was not associated with type 2 diabetes in a recent umbrella review of meta-analyses (5), although the definitions of legumes varied substantially across studies, which is also the case across our study centers. Overall, due to the low intake of legumes in some countries, most estimates were, however, imprecise and further research is needed.
There is consistent evidence from cohort studies linking whole grains to a lower risk of type 2 diabetes (18), but in the current study, we were not able to differentiate between the intake of refined and whole grains. In an exploratory analysis stratifying the study population by cereal fiber, we found no substantial differences between strata. This could be a reflection of the absence of an association between refined grain and type 2 diabetes in this study, as in some other populations (18). When replacing 5 g protein from red and processed meat with 5 g protein from cereals, we found no association, suggesting that other nutrients in cereals, like dietary fiber, may drive the observed association. Our results extend the previous findings in the U.S. study to a European population and highlight that some, but not all, food sources of protein may be beneficial for type 2 diabetes risk as alternatives to red and processed meat. A caveat to this is that the point estimates for poultry and fish were similar to the other replacement foods, but with less precision.
In this study, we were able to investigate whether body iron stores, measured as serum ferritin, could mediate the association of replacing red meat with other sources of protein. Our results suggest that ferritin may explain up to 31.8% of the observed associations, although the associations were, in general, weak. This result is in line with a previous finding that serum ferritin may partly mediate the association between intake of red meat and risk of type 2 diabetes in the EPIC-Potsdam study (9). There are, however, alternative explanations for the potential benefits of substituting red meat with other protein sources. BMI could be regarded as a mediator. We found that most of our estimates were attenuated after adjustment for BMI, as was also observed in a large Chinese cohort (28), and higher consumption of red and processed meat has also been associated with weight gain in the EPIC study (29). We only had a single measure of BMI and could not study weight change, but we prespecified including baseline BMI as a potential confounder. Advanced glycation end products formed during the preparation of red and processed meat may increase body weight, inflammation, and insulin resistance (30,31). Nitrates and nitrites, which are commonly found in processed meat, can be converted to nitrosamines, which have been linked with insulin resistance and may be toxic to pancreatic β-cells (30). Negative effects from preparation methods of other meat products, such as poultry or fish, might explain why these replacements were not associated with a lower risk of type 2 diabetes. Fermented dairy products like cheese and yogurt contain odd-chain fatty acids, ruminant trans fatty acids, and probiotic bacteria, all of which have been hypothesized to have beneficial effects on glucose metabolism (32,33). Cereals, in our study consisting of both refined and whole grains, may lower diabetes risk primarily through the intake of whole grains high in dietary fiber and phytochemicals with benefits on the production of short-chain fatty acids, improved insulin sensitivity, and glucose control and anti-inflammatory effects (34).
Under the assumption of causal effects, stable dietary intakes, and linear IRs, our estimate of the population attributable fraction suggested that 7.5% (95% CI 3.3–11.3) to 8.8% (3.1–13.6) of observed type 2 diabetes cases could have been prevented if the population had replaced 1 serving/day of red and processed meat with 1 serving/day of cheese, yogurt, or nuts. This is relevant for public health. Our study paid close attention to accounting for a range of potential confounding factors and addressed a number of potential biases. Our study was undertaken in meat-consuming European populations, and the results cannot, therefore, necessarily be generalized to non-European populations with different dietary habits. Although studies suggest that red and processed meat intake is positively associated with the development of type 2 diabetes (6), this may also depend on the consumption levels of other foods consumed in the diet, such as fiber- or calcium-rich foods, and whether red and processed meats are consumed within an overall healthy diet (35).
In conclusion, this study suggests that the replacement habitually of 1 serving/day of red and processed meat with 1 serving/day of cheese, yogurt, nuts, or cereals may be associated with a lower rate of development of type 2 diabetes. Replacing red and processed meat with other sources of protein may have a public health impact for the prevention of type 2 diabetes.
Article Information
Acknowledgments. The authors thank all EPIC participants and staff for their contribution to the study and Nicola Kerrison, MRC Epidemiology Unit, University of Cambridge School of Clinical Medicine, Cambridge, U.K., for data management.
Funding. Funding for the InterAct project was provided by the European Union Sixth Framework Programme (grant no. LSHM_CT_2006_037197). Additionally, InterAct investigators acknowledge funding from the following agencies: N.J.W. and N.G.F. acknowledge funding from the MRC Epidemiology Unit (MC_UU_12015/1 and MC_UU_12015/5) and NIHR Biomedical Research Centre Cambridge: Nutrition, Diet, and Lifestyle Research Theme (IS-BRC-1215-20014). M.S. and F.I. report core MRC Unit support through the Nutritional Epidemiology Programme (MC_UU_12015/5). M.B.S. acknowledges funding by the German Ministry of Education and Research (BMBF) and the State of Brandenburg (DZD grant 82DZD00302). M.G. acknowledges funding by the Regional Government of Navarre. V.S. was supported by Programma VALERE, University of Campania Luigi Vanvitelli.
The funding sources did not participate in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. The EPIC-InterAct study was coordinated by N.J.W., S.J.S., and N.G.F. with N.J.W. as chief investigator. D.B.I., M.S., F.I., K.O., and N.G.F. conceived the research question. D.B.I., M.S., F.I., K.O., M.B.S., B.B., M.G., and N.G.F. designed the analysis plan. D.B.I. performed the data analysis. M.S., F.I., and S.J.S. provided statistical supervision. D.B.I. drafted the manuscript with supervision from N.G.F. All authors interpreted the results and critically revised the article for important intellectual content and gave final approval of the version to publish. N.G.F. and N.J.W. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Where authors are identified as personnel of the International Agency for Research on Cancer, World Health Organization, the authors alone are responsible for the views expressed in this article, and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer, World Health Organization.
N.G.F. and N.J.W. made equal contributions.
This article contains supplementary material online at https://doi.org/10.2337/figshare.12732920.
References
- 1.Saeedi P, Petersohn I, Salpea P, et al. . Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 2019;157:107843. [DOI] [PubMed] [Google Scholar]
- 2.Hemmingsen B, Gimenez-Perez G, Mauricio D, Roqué I Figuls M, Metzendorf MI, Richter B. Diet, physical activity or both for prevention or delay of type 2 diabetes mellitus and its associated complications in people at increased risk of developing type 2 diabetes mellitus. Cochrane Database Syst Rev 2017;12:CD003054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dyson PA, Twenefour D, Breen C, et al. . Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med 2018;35:541–547 [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association 3. Prevention or delay of type 2 diabetes: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S29–S33 [DOI] [PubMed] [Google Scholar]
- 5.Neuenschwander M, Ballon A, Weber KS, et al. . Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ 2019;366:l2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bendinelli B, Palli D, Masala G, et al.; InterAct Consortium . Association between dietary meat consumption and incident type 2 diabetes: the EPIC-InterAct study. Diabetologia 2013;56:47–59 [DOI] [PubMed] [Google Scholar]
- 7.Halkjaer J, Olsen A, Bjerregaard LJ, et al. . Intake of total, animal and plant proteins, and their food sources in 10 countries in the European Prospective Investigation into Cancer and Nutrition. Eur J Clin Nutr 2009;63(Suppl. 4):S16–S36 [DOI] [PubMed] [Google Scholar]
- 8.Pan A, Sun Q, Bernstein AM, et al. . Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr 2011;94:1088–1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wittenbecher C, Mühlenbruch K, Kröger J, et al. . Amino acids, lipid metabolites, and ferritin as potential mediators linking red meat consumption to type 2 diabetes. Am J Clin Nutr 2015;101:1241–1250 [DOI] [PubMed] [Google Scholar]
- 10.Yeap BB, Divitini ML, Gunton JE, et al. . Higher ferritin levels, but not serum iron or transferrin saturation, are associated with type 2 diabetes mellitus in adult men and women free of genetic haemochromatosis. Clin Endocrinol (Oxf) 2015;82:525–532 [DOI] [PubMed] [Google Scholar]
- 11.Riboli E, Hunt KJ, Slimani N, et al. . European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 2002;5:1113–1124 [DOI] [PubMed] [Google Scholar]
- 12.Langenberg C, Sharp S, Forouhi NG, et al.; InterAct Consortium . Design and cohort description of the InterAct Project: an examination of the interaction of genetic and lifestyle factors on the incidence of type 2 diabetes in the EPIC Study. Diabetologia 2011;54:2272–2282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Margetts BM, Pietinen P. European Prospective Investigation into Cancer and Nutrition: validity studies on dietary assessment methods. Int J Epidemiol 1997;26(Suppl. 1):S1–S5 [DOI] [PubMed] [Google Scholar]
- 14.Sluijs I, Forouhi NG, Beulens JWJ, et al.; InterAct Consortium . The amount and type of dairy product intake and incident type 2 diabetes: results from the EPIC-InterAct Study. Am J Clin Nutr 2012;96:382–390 [DOI] [PubMed] [Google Scholar]
- 15.Patel PS, Forouhi NG, Kuijsten A, et al.; InterAct Consortium . The prospective association between total and type of fish intake and type 2 diabetes in 8 European countries: EPIC-InterAct Study. Am J Clin Nutr 2012;95:1445–1453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buijsse B, Boeing H, Drogan D, et al.; InterAct Consortium . Consumption of fatty foods and incident type 2 diabetes in populations from eight European countries. Eur J Clin Nutr 2015;69:455–461 [DOI] [PubMed] [Google Scholar]
- 17.Schwingshackl L, Hoffmann G, Lampousi AM, et al. . Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol 2017;32:363–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol 2013;28:845–858 [DOI] [PubMed] [Google Scholar]
- 19.Wareham NJ, Jakes RW, Rennie KL, et al. . Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr 2003;6:407–413 [DOI] [PubMed] [Google Scholar]
- 20.Podmore C, Meidtner K, Schulze MB, et al. . Association of multiple biomarkers of iron metabolism and type 2 diabetes: the EPIC-InterAct study. Diabetes Care 2016;39:572–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song M, Giovannucci E. Substitution analysis in nutritional epidemiology: proceed with caution. Eur J Epidemiol 2018;33:137–140 [DOI] [PubMed] [Google Scholar]
- 22.Simcox JA, McClain DA. Iron and diabetes risk. Cell Metab 2013;17:329–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffmann K, Pischon T, Schulz M, Schulze MB, Ray J, Boeing H. A statistical test for the equality of differently adjusted incidence rate ratios. Am J Epidemiol 2008;167:517–522 [DOI] [PubMed] [Google Scholar]
- 24.Rajpathak SN, Crandall JP, Wylie-Rosett J, Kabat GC, Rohan TE, Hu FB. The role of iron in type 2 diabetes in humans. Biochim Biophys Acta 2009;1790:671–681 [DOI] [PubMed] [Google Scholar]
- 25.Fibrinogen Studies Collaboration Correcting for multivariate measurement error by regression calibration in meta-analyses of epidemiological studies. Stat Med 2009;28:1067–1092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan A, Sun Q, Bernstein AM, Manson JE, Willett WC, Hu FB. Changes in red meat consumption and subsequent risk of type 2 diabetes mellitus: three cohorts of US men and women. JAMA Intern Med 2013;173:1328–1335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wallin A, Forouhi NG, Wolk A, Larsson SC. Egg consumption and risk of type 2 diabetes: a prospective study and dose-response meta-analysis. Diabetologia 2016;59:1204–1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Du H, Guo Y, Bennett DA, et al.; China Kadoorie Biobank collaborative group . Red meat, poultry and fish consumption and risk of diabetes: a 9 year prospective cohort study of the China Kadoorie Biobank. Diabetologia 2020;63:767–779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vergnaud AC, Norat T, Romaguera D, et al. . Meat consumption and prospective weight change in participants of the EPIC-PANACEA study. Am J Clin Nutr 2010;92:398–407 [DOI] [PubMed] [Google Scholar]
- 30.Kim Y, Keogh J, Clifton P. A review of potential metabolic etiologies of the observed association between red meat consumption and development of type 2 diabetes mellitus. Metabolism 2015;64:768–779 [DOI] [PubMed] [Google Scholar]
- 31.Cordova R, Knaze V, Viallon V, et al. . Dietary intake of advanced glycation end products (AGEs) and changes in body weight in European adults. Eur J Nutr. 7 November 2019 [Epub ahead of print]. DOI: 10.1007/s00394-019-02129-8 [DOI] [PubMed] [Google Scholar]
- 32.Fernandez MA, Marette A. Novel perspectives on fermented milks and cardiometabolic health with a focus on type 2 diabetes. Nutr Rev 2018;76(Suppl. 1):16–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Imamura F, Fretts A, Marklund M, et al.; InterAct Consortium; Fatty Acids and Outcomes Research Consortium (FORCE) . Fatty acid biomarkers of dairy fat consumption and incidence of type 2 diabetes: a pooled analysis of prospective cohort studies. PLoS Med 2018;15:e1002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Della Pepa G, Vetrani C, Vitale M, Riccardi G. Wholegrain intake and risk of type 2 diabetes: evidence from epidemiological and intervention studies. Nutrients 2018;10:E1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Connor LE, Paddon-Jones D, Wright AJ, Campbell WW. A Mediterranean-style eating pattern with lean, unprocessed red meat has cardiometabolic benefits for adults who are overweight or obese in a randomized, crossover, controlled feeding trial. Am J Clin Nutr 2018;108:33–40 [DOI] [PMC free article] [PubMed] [Google Scholar]