Psychological stress is a known general health risk potentially increasing the risk of type 1 diabetes. Consistent with this hypothesis, there were reports of a higher incidence of type 1 diabetes after other stressful catastrophic events, e.g., the Chernobyl incident in 1986 or the Los Angeles earthquake in 1994 (1,2). Over the past few months, coronavirus disease 2019 (COVID-19) and subsequent social distancing have affected biological, psychological, economic, and social aspects of life. Social distancing during the lockdown could be perceived as a stressful situation for children and adolescents, who could not attend kindergarten or school and were unable to pursue hobbies like sports or meeting friends. Perceived stress caused by feelings of isolation may have increased the risk of type 1 diabetes (3). Since type 1 diabetes is also associated with viral infections (4), explaining, for example, the higher type 1 diabetes incidence during winter months, COVID-19 infection may have caused an increase of type 1 diabetes manifestations by affecting immune regulation or by directly damaging pancreatic β-cells (5). On the contrary, during the lockdown period between March and May 2020 in Germany, the incidence of type 1 diabetes could also have decreased, since people were less exposed to common infections.
We aimed to assess a possible change in pediatric type 1 diabetes incidence during the COVID-19 lockdown.
Out of 217 German pediatric diabetes centers participating in the Diabetes-Prospective Follow-up registry (DPV), 216 centers provided us with information about incident type 1 diabetes cases. We included pediatric type 1 diabetes patients with onset age between 6 months and <18 years diagnosed between 13 March and 13 May in each year between 2011 and 2020, corresponding to the lockdown period in Germany in 2020. For each year, we related the number of cases to the respective patient-years at risk—obtained from the Federal Statistical Office—to estimate the incidence per 100,000 patient-years with 95% CI. Applying Poisson regression, we predicted the type 1 diabetes incidence for 2020 based on data from 2011–2019 and compared these with the observed incidence. Additionally, we stratified the analyses by sex and age-group (<6, 6 to <12, 12 to <18 years).
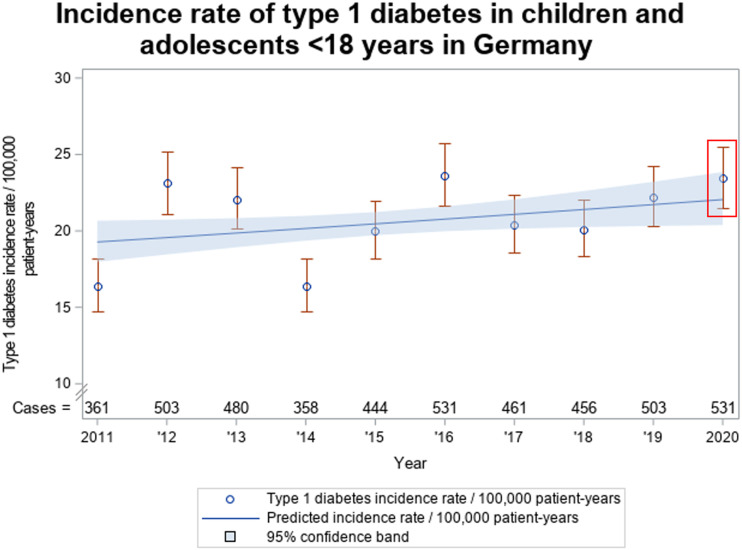
Overall, the type 1 diabetes incidence increased from 16.4 [95% CI 14.7–18.2] in 2011 to 22.2 [20.3–24.2] in 2019 (P = 0.04). The incidence in 2020, based on 532 cases among 13.6 million subjects <18 years, was 23.4 [21.5–25.5] and did not differ significantly from the prediction (22.1 [20.4–23.9]) (Fig. 1). Stratifying by age-group or sex, we also found no significant differences between observed and estimated incidence in 2020. However, we observed a nonsignificantly higher incidence in males in 2020 (28.1 [25.1–31.3]) compared with the predicted incidence of 23.1 [20.8–25.7]. In females, the observed incidence in 2020 was lower than the predicted incidence (18.6 [16.2–21.4] vs. 20.9 [18.6–23.5]).
Figure 1.
Type 1 diabetes incidence of patients <18 years during the period 13 March to 13 May (corresponding to the German lockdown period in 2020) in the years 2011 to 2020.
The type 1 diabetes incidence in 2020 follows the increasing trend observed between 2011 and 2019 without up- or downward deviation, indicating no short-term influence of the COVID-19 pandemic. Thus, strong direct diabetogenic effects seem very unlikely, but weak effects cannot be excluded given the relatively low COVID-19 infection rate in Germany. It remains unclear whether elevated stress levels and reduced infection rates outweigh each other regarding effects on the onset of type 1 diabetes in children and adolescents or whether they have no measurable impact on incidence. However, there may be a delay between immunologic factors or infections and the onset of type 1 diabetes. It is therefore crucial to conduct long-term follow-up studies to investigate possible associations between the COVID-19 pandemic and the incidence of type 1 diabetes.
Article Information
Acknowledgments. The authors thank Katharina Fink and Alexander Eckert (both at Ulm University) for the DPV data management.
Funding. This work was supported by the German Center for Diabetes Research (DZD) funded by the Federal Ministry of Education and Research (FKZ 82DZD14A02). The German Diabetes Association (DDG) and the Robert Koch Institute (RKI) provided further financial support for the DPV registry.
Duality of Interest. K.M. has received Medtronic personal educational fees of <1500 € (without conflicts regarding this article). No other potential conflicts of interest relevant to this article were reported.
Author Contributions. S.R.T. and J.R. researched data and wrote the manuscript. C.K., J.Z., F.R., J.H., K.M., A.P., and T.K. contributed data and reviewed and edited the manuscript. R.W.H. conceptualized the study and reviewed and edited the manuscript. All authors have read and approved the final manuscript. R.W.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this work were presented in abstract form at the International Society for Pediatric and Adolescent Diabetes (ISPAD) 46th Annual Conference, 15–17 October 2020.
Footnotes
See accompanying articles, pp. 2631, 2870, and e170.
This article is part of a special article collection available at https://care.diabetesjournals.org/collection/diabetes-and-COVID19.
S.R.T. and J.R. share first authorship.
References
- 1.Kaufman FR, Devgan S. An increase in newly onset IDDM admissions following the Los Angeles earthquake. Diabetes Care 1995;18:422. [DOI] [PubMed] [Google Scholar]
- 2.Zalutskaya A, Bornstein SR, Mokhort T, Garmaev D. Did the Chernobyl incident cause an increase in type 1 diabetes mellitus incidence in children and adolescents? Diabetologia 2004;47:147–148 [DOI] [PubMed] [Google Scholar]
- 3.Sharif K, Watad A, Coplan L, Amital H, Shoenfeld Y, Afek A. Psychological stress and type 1 diabetes mellitus: what is the link? Expert Rev Clin Immunol 2018;14:1081–1088 [DOI] [PubMed] [Google Scholar]
- 4.Filippi CM, von Herrath MG. Viral trigger for type 1 diabetes: pros and cons. Diabetes 2008;57:2863–2871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang L, Han Y, Nilsson-Payant BE, et al. A human pluripotent stem cell-based platform to study SARS-CoV-2 tropism and model virus infection in human cells and organoids. Cell Stem Cell 2020;27:125–136.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]