Abstract
Background
Although rare, human–shark interactions can result in a wide spectrum of injuries. This is the first study to characterize shark-related injuries (SRIs) in Hawai’i.
Methods
This is a retrospective review of the State of Hawai’i Division of Aquatic Resources Shark Incidents List between January 1, 2009 and December 31, 2019. Trauma registry data and medical records of patients treated for SRIs at the only level 1 trauma center in Hawai’i were reviewed.
Results
Sixty-one patients sustained SRIs in the Hawaiian Islands: 25 in Maui, 16 in O’ahu, 12 in Hawai’i, and 8 in Kaua’i. In cases where the shark species could be identified, tiger sharks were the most frequent (25, 41%). Four cases were fatal—all died on scene in Maui with the shark species unknown. Forty-five survivors (79%) received definitive care at regional facilities. Twelve (21%) were treated at the level 1 trauma center, of which two were transferred in for higher level of care. Of the 12 patients, 11 (92%) had extremity injuries, with 3 lower extremity amputations (25%), 2 with vascular injuries (17%), and 5 with nerve injuries (42%). One had an injury to the abdomen. All patients had local bleeding control in the prehospital setting, with 9 (75%) tourniquets and 3 (25%) hemostatic/pressure dressings applied for truncal or proximal extremity injuries. The mean time from injury to emergency department arrival was 63 minutes.
Discussion
Most SRIs are managed at regional facilities, rather than at a level 1 trauma center. Prehospital hemorrhage control is an important survival skill as time to definitive care may be prolonged. For cases treated at the level 1 trauma center, nerve injuries were common and should be suspected even in the absence of major vascular injury. Correlating shark behavior with observed injury patterns may help improve public awareness and ocean safety.
Level of evidence
Level V, epidemiological.
Keywords: bites and stings, hemorrhage
Background
For over half a century, the USA has had the highest number of shark-related injuries (SRIs) of any country in the world. SRI rates have been increasing in higher population countries including the USA and specifically within the region of Hawai’i, but the overall number of SRIs per year still remains low.1 Although rare, human–shark interactions can cause a wide spectrum of injuries. Given this variability of outcomes, one study called for a change in nomenclature away from the loaded phrase of “shark attack” that connotes shark intent and resultant major injuries.2 Therefore, this study will refer to these interactions as “SRIs” to help promote scientific discourse.
Prior studies on SRIs have either used three large independent databases (the Global Shark Attack File (GSAF), the International Shark Attack File (ISAF), or the South African Shark Attack File),3–5 compared shark attack databases with local medical records (Virginia, USA,6 and La Réunion Island, France7), or presented individual case reports in South Africa8 and Mexico/Canada.9 In the few studies that have identified the shark species implicated in SRIs, the majority were caused by the great white shark (Carcharodon carcharias) in South Africa5 and by the bull shark (Carcharhinus leucas) in La Réunion Island, France.7
This is the first study to characterize SRIs in the state of Hawai’i, where the predominant species of shark is the tiger shark (Galeocerdo cuvier).1 Hawai’i is an isolated archipelago of eight major islands in the Pacific Ocean, which poses unique challenges for patient treatment and transport. There is only one level 1 trauma center in the Hawaiian Islands, The Queen’s Medical Center (QMC), located in Honolulu, on the island of O’ahu. The purposes of this study were to (1) determine when and where SRIs occurred in the state of Hawai’i; and (2) describe SRI patterns, interventions, and medical resource utilization in both the prehospital and hospital setting and the outcomes of the patients treated at QMC.
Methods
A retrospective review of the State of Hawai’i Department of Land and Natural Resources Division of Aquatic Resources (DAR) Shark Incidents List between January 1, 2009 and December 31, 2019 was conducted. Both provoked and unprovoked incidents were included. Provoked shark incidents are defined by the ISAF as incidents “when a human initiates interaction with a shark in some way.” Examples of activities that provoke shark incidents include harassing sharks while diving, spearfishing, feeding sharks, and so on.10 Only cases of shark attacks with human injury were included. Twenty-one shark bites of objects such as surfboards in which the victims were unharmed were excluded. All known data associated with each case in the DAR Shark Incidents List were reviewed, including date and time, location, victim’s activity, water clarity, water depth, treatment facility, injury description, and shark species.
Trauma registry data and medical records of patients treated for SRIs at QMC were reviewed for further clinical details, including patient demographics, treatment provided, and patient outcomes.
Descriptive statistics summarizing patient characteristics were conducted using Microsoft Excel (Redmond, WA, USA).
Results
Sixty-one patients sustained SRIs in the Hawaiian Islands during the study period. The island of Maui had the most SRIs with 25 (table 1). Fifty-three (87%) injuries were unprovoked and 8 (13%) were provoked. The most common activities associated with unprovoked SRIs were surfing (20, 33%) and swimming (14, 23%). The most common activities associated with provoked SRIs were swimming with sharks (4, 6.6%) and spearfishing (2, 3.3%). The majority of cases (57%) occurred in turbid water conditions.
Table 1.
Characteristics of all shark-related injuries in the state of Hawai’i
| Survived, n (%) | 57 (93) |
| Fatal, n (%) | 4 (7)—all on Maui |
| Total | 61 |
| Island, n (%) | |
| Maui | 25 (41) |
| O’ahu | 16 (26) |
| Hawai’i | 12 (20) |
| Kaua’i | 8 (13) |
| Shark species, n (%) | |
| Unknown/data insufficient | 26 (43) |
| Tiger | 25 (41) |
| Cookiecutter | 4 (6.6) |
| Galapagos | 2 (3.3) |
| Requiem | 2 (3.3) |
| Galapagos or sandbar | 1 (1.6) |
| Whitetip reef | 1 (1.6) |
| Water clarity, n (%) | |
| Turbid | 35 (57) |
| Clear | 24 (39) |
| Unknown | 2 (3.3) |
| Activity of unprovoked incident, n (%) | |
| Surfing | 20 (33) |
| Swimming | 14 (23) |
| Snorkeling | 8 (13) |
| Body boarding | 3 (5) |
| Treading water | 2 (3.3) |
| Paddling | 1 (1.6) |
| Stand-up paddle boarding | 1 (1.6) |
| Floating | 1 (1.6) |
| Spearfishing | 1 (1.6) |
| Standing | 1 (1.6) |
| Kite surfing | 1 (1.6) |
| Total | 53 (87) |
| Activity of provoked incident, n (%) | |
| Swimming with sharks | 4 (6.6) |
| Spearfishing | 2 (3.3) |
| Fishing | 1 (1.6) |
| Fishing from kayak | 1 (1.6) |
| Total | 8 (13) |
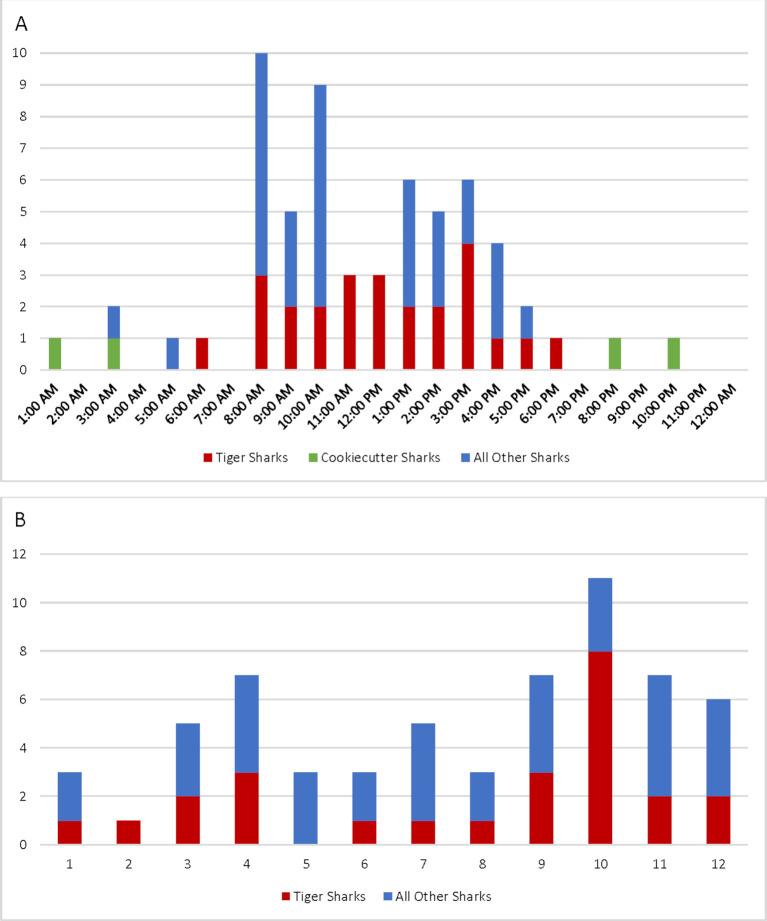
Fifty-three (87%) shark injuries occurred during daylight hours between 08:00 and 17:00 (figure 1A). All four cookiecutter shark injuries occurred during the night between 08:00 and 04:00. Only four injuries (6.6%) occurred during twilight. There were insufficient data to identify the shark species involved in 26 (43%) injuries. In the 35 cases where the species could be identified, tiger sharks were the most frequently involved with 25 (71%). Thirteen of the 25 (52%) tiger shark injuries occurred between September and November, with the most injuries occurring in October (8, 32%) (figure 1B).
Figure 1.
(A) Shark-related injuries by time of day. Intervals are from :00 to :59. Example: 06:00 is from 06:00 to 06:59. (B) Shark-related injuries by month.
Four cases (6.6%) were fatal—all died on scene in Maui, with the shark species unknown. Two fatalities sustained proximal upper extremity injuries—one victim was bitten on the right shoulder, underarm, and right side of the face, and the other victim sustained a right arm amputation below the shoulder. One fatality sustained a lower left leg amputation and avulsions to the left arm and hand. For the fourth fatality, it was noted that the victim’s feet were dangling in the water while fishing from a kayak when bitten by a shark; however, no further description of the injury was provided.
Of the 12 patients treated at QMC, the mean age was 36.6 (range 10–58) years and 83% were male. All patients had local bleeding control in the prehospital setting, with 9 (75%) tourniquets and 3 (25%) hemostatic/pressure dressings applied for truncal or proximal extremity injuries. Five (42%) patients had makeshift tourniquets (using a surf leash or clothing) applied by bystanders before commercial tourniquets were applied by first responders. The mean time from injury to initial emergency department (ED) arrival was 63 (range 42–84) minutes.
The nature of injuries treated at QMC is listed in table 2. A single site was injured in seven cases, two sites in four cases, and three sites in one case. Eleven patients (92%) sustained extremity injuries, including three lower extremity amputations (25%). Five patients (42%) sustained nerve injuries, with seven total nerves affected. Two patients (17%) sustained vascular injuries (excluding traumatic and secondary amputations). One patient had an injury to the abdomen that did not violate the peritoneal cavity. The mean Injury Severity Score was 7.08 (range 1–17). Eleven patients (92%) were hospitalized with a mean and median length of stay of 6.25 (range 1–34) days and 3 days (IQR 2–6.5), respectively. Four patients (33%) required transfusion of blood products.
Table 2.
Nature of shark-related injuries treated at The Queen’s Medical Center
| n=12 | |
| Single site | 7 |
| Multiple sites | 5 |
| Two sites | 4 |
| Three sites | 1 |
| Most severe level of injury per patient | |
| Abrasion/contusion | 0 |
| Skin or soft tissue injury | 1 |
| Tendon/muscle/bone injury | 8 |
| Major vascular injury, includes isolated vascular injuries and amputations | 3 |
| Upper limb injuries, most proximal extent | 8 |
| Hand | 2 |
| Forearm | 3 |
| Elbow | 1 |
| Upper arm | 0 |
| Shoulder | 2 |
| Lower limb injuries, most proximal extent | 9 |
| Thigh | 5 |
| Lower leg | 4 |
| Foot | 0 |
| Abdomen | 1 |
| Vascular injury* | |
| Ulnar artery† | 1 |
| Anterior tibial artery‡ | 1 |
| Amputation/disarticulation | |
| Below the knee† | 2 |
| Above the knee | 1 |
| Nerve injury* | |
| Ulnar nerve | 2 |
| Radial nerve | 2 |
| Median nerve | 1 |
| Lateral antebrachial cutaneous nerve | 1 |
| Peroneal nerve | 1 |
| Shark-induced trauma level, n (%) | |
| Level 5 | 1 (8.3) |
| Level 4 | 3 (25) |
| Level 3 | 4 (33) |
| Level 2 | 4 (33) |
| Level 1 | 0 (0) |
*Excluding traumatic and secondary amputation.
†One patient had a traumatic BKA and ulnar artery injury (see figure 3).
‡One patient had ipsilateral anterior and posterior tibial artery injuries. Revascularization was unsuccessful and necessitated secondary BKA. The contralateral leg had an anterior tibial artery injury (see figure 2).
BKA, below knee amputation.
Injuries were classified with the Shark-Induced Trauma (SIT) Scale (table 2).4 This score includes measurement of the initial blood pressure, the location and depth of the injury, the impairment from the injury, and the complexity of the required treatment. Level 5 injuries are the most severe with fatality likely—in our study, the single level 5 patient was the only one who required intensive care unit care for 7 days. The most frequent injury levels were levels 2 and 3, with 33% each. Clinical photos with examples of each injury level treated at QMC are demonstrated in figures 2–3.
Figure 2.
(A) Level 2 injury from cookiecutter shark bite to the left posterior shoulder. Distinctive “punched-out” bite pattern pathognomonic of a cookiecutter shark. Underwent operative debridement and wound closure. (B) Level 3 injury from a tiger shark to the left lower extremity (LLE). Obvious bite marks to the thigh with shark dentition pattern evident. Sustained traumatic arthrotomy of the knee, complete biceps femoris tendon laceration, and complete laceration of the common peroneal nerve. Underwent two operative debridements, repair of tendon, and delayed primary repair of the peroneal nerve. (C) Level 5 injury from a tiger shark. Bilateral tibiotalar joint dislocations with extensive soft tissue injuries. Right lower extremity (RLE) with anterior and posterior tibial artery injuries. LLE with anterior tibial artery injury only. Revascularization of RLE attempted but graft occluded and the patient underwent secondary below knee amputation of RLE the next day. Left lower extremity salvaged with transtibiocalcaneal pins, multiple tendon repairs, four operative debridements, and latissimus/serratus free flap with split-thickness skin graft placed 9 days after injury. Pseudomonas aeruginosa cultured from LLE wound 5 days after injury and treated with cefepime and surgical debridement.
Figure 3.
Level 4 injury from a tiger shark. (A, B) Traumatic below knee amputation (BKA) of the right lower extremity (RLE). (C, D) Deep lacerations to the right upper extremity (RUE) with traumatic wrist arthrotomy and lacerated median nerve, ulnar nerve, ulnar artery, and multiple tendons. After undergoing operative debridement of RUE and RLE and provisional revision amputation of RLE, the patient was transferred to The Queen’s Medical Center for hand surgeon expertise. All injured structures of RUE were repaired. A total of four operative debridements were performed to RLE prior to transfer to mainland for complex wound coverage of BKA site.
Two patients received wound treatment in the ED and 10 patients were treated in the operating room. Of the 10 patients requiring surgery, 6 (60%) were treated with a single operation. Four patients (40%) had multiple operations done in tandem or succession. Hand surgeons operated on the majority of surgical patients (6), followed by orthopedics (5), trauma (5), vascular surgery (1), plastic surgery (1), and otolaryngology who provided free flap coverage (1). Five patients (50%) had six microsurgical operations during their index hospitalization—three patients had nerve repairs, one patient had nerve and artery repairs, and one patient had a vascular repair and free flap coverage of a wound. Three patients (25%) were discharged with plans for future surgical intervention. One patient was transferred to a mainland hospital for complex wound flap coverage, one had delayed nerve reconstruction, and one had removal of temporary pin fixation. There were no unplanned readmissions within 30 days of discharge.
All 12 patients were administered antibiotic prophylaxis with multiple-agent regimens that included doxycycline. All doses of doxycycline were 100 mg administered every 12 hours, but the duration of prophylactic dosing ranged from 3 to 14 days and the route of administration (oral or intravenous) varied. There was only one wound infection in this case series, Pseudomonas aeruginosa, in a patient with extensive soft tissue loss (figure 2C). Antibiotic coverage was changed to cefepime per bacterial sensitivities for treatment. After further debridement, the patient underwent successful free flap coverage of the large lower extremity wound.
Discussion
The death rate for all SRIs in Hawai’i during this study period was 6.6%, which is lower than the rates reported in South Africa from 1980 to 1999 (11.6%),5 in Australia from 2000 to 2009 (9.9%),11 and in La Réunion Island from 2000 to 2016 (38%).7 The difference in mortality rates is likely multifactorial. One explanation could be that different shark species are present in each region causing different severities of injury. The great white shark in South Africa5 and Australia11 and the bull shark on La Réunion Island7 were the species implicated in most fatalities. Although tiger sharks are the most abundant species in Hawai’i’s waters, the shark species involved in the four fatal cases is/are unknown. A prior review of the GSAF from 1900 to 2014 demonstrated that tiger sharks were the only shark species associated with an increased risk of fatal attacks,3 but there were no fatalities in this study knowingly attributed to tiger sharks. All four fatalities died on scene in Maui. It is unclear why these victims died from the injuries, whereas the amputations and proximal injuries in our case series survived. Further clinical data in these cases are necessary to elucidate possible reasons for fatality.
All 12 patients treated at the level 1 trauma center in this case series survived. Prior SRI studies have demonstrated that hemorrhage and hypovolemic shock are the principal causes of death among shark-related fatalities.5 7 8 All patients in this case series received local bleeding control measures (tourniquet or hemostatic/pressure dressing) and fluid resuscitation by first responders prior to hospital arrival. Prehospital control of blood loss is particularly important given the prolonged times from injury to ED arrival (mean of 63 minutes) as SRIs occurred either in remote parts of the islands or out on the open water (as in the cases of cookiecutter shark-related injuries). All patients with SIT level 4 and 5 injuries, the highest injury severity levels, also had makeshift tourniquets applied by bystanders prior to first responder arrival. Treatment of SRIs must start in the prehospital setting using Stop the Bleed techniques,12 and contributions from good samaritan bystanders cannot be overestimated. Perhaps targeting the Stop the Bleed course toward the public at risk and providing bleeding control kits at beaches might help prevent death and hemorrhage from future SRIs.
Once patients arrive in the hospital setting, treatments to help prevent wound infection must be undertaken. Larger wounds are often contaminated with sand and contain devitalized soft tissue which requires appropriate surgical debridement. Antibiotic prophylaxis must also be considered. Antibiotic prophylaxis against Vibrio species is recommended for SRIs as they are the most common bacteria found in marine waters13 and have been cultured from the teeth of a great white shark.14 Vibrio vulnificus wound infections can range from relatively mild cases to severe and rapidly progressive cellulitis and myositis.15 The Centers for Disease Control and Prevention recommends treating V. vulnificans infections with a regimen such as doxycycline 100 mg orally or intravenously two times a day for 7 to 14 days with a third-generation cephalosporin, but there are no clear guidelines for infection prophylaxis.16 All patients treated at QMC received antibiotic prophylaxis with multiple-agent regimens including doxycycline 100 mg either intravenously or orally of varying duration for coverage against Vibrio spp. There was only one wound infection, P. aeruginosa, diagnosed by wound culture during hospitalization. There were no Vibrio spp infections in this case series.
The severity of injuries treated at QMC was likely higher than those treated at other facilities in Hawai’i due to its designation as a level 1 trauma center with high availability of surgical specialists. Nerve injuries were common in the cases treated at QMC and should be suspected even in the absence of major vascular injury. Half of the surgical patients with SRIs at QMC required microsurgery, including the two patients transferred to QMC from outer islands for hand surgeon expertise. Coordinating surgical care between specialties to perform operations in tandem or succession helped to minimize operation time and anesthesia events for patients. The majority of SRIs were otherwise managed at regional facilities. Further study evaluating the clinical data from patients with SRI treated at other facilities is warranted for a more comprehensive understanding of SRI patterns and medical intervention in Hawai’i.
Understanding shark habitats and behavior can shed light on SRI incident patterns in Hawai’i. Maui had almost 1.5 times the amount of SRIs compared with O’ahu despite the human population of O’ahu being six times larger.17 A study of electronically tagged tiger sharks demonstrated that tiger sharks have a high affinity for the insular shelf habitat around Maui. Most Maui-tagged sharks tended to stay near Maui in a smaller home range, whereas Oahu-tagged sharks undertook seasonal migrations to Maui. Tiger shark home ranges around Maui are also closer to high-use ocean recreation sites compared with those on O’ahu.18 These patterns may help explain why Maui has had more SRIs than other Hawaiian Islands.
The highest number of tiger shark injuries occurred in the fall, particularly in October. This was to be expected as Hawaiian oral tradition warns, “When the wiliwili tree blooms” in the fall, “the sharks bite.”19 Tiger shark pupping season, which is typically around September to October,20 could be one explanation for this increase in injuries despite fewer people being in the water in the fall.21 An estimated 25% of mature female sharks appear to migrate from the remote French Frigate Shoals atoll to the main Hawaiian Islands during late summer/early fall, potentially to give birth.22 These female sharks with lower energy reserves could then bite something, such as a human, that they normally would not bite. Ocean users should proceed with extra caution during the fall months in Hawai’i.
Although it is recommended to stay out of the water at dawn, dusk, and night, SRIs can occur at any time of day (figure 1A). It is unclear if fewer shark bites occur during twilight hours only because there are fewer people in the water. A unique subset of SRIs from cookiecutter sharks (Isistius spp) occurred overnight. Cookiecutter sharks have unique feeding habits that leave pathognomonic circular wounds that resemble the cut-out of a cookie cutter (figure 2A). These injuries were all sustained by long-distance swimmers swimming the Ka’iwi Channel between the islands of O’ahu and Moloka’i at night to avoid excessive sunburn, which corresponds with the nocturnal surface feeding activity of cookiecutter sharks.23
Although SRIs can be devastating, the risk of sustaining an SRI in Hawai’i is extremely low. For example, in 2018, there were three SRIs for an estimated 1.6 million people (de facto resident and visitor population) present on the islands.17 Ocean users still need to be mindful that they are entering the natural habitat of many potentially dangerous creatures. Awareness of seasonal injury patterns and shark safety tips (box 1) can help the public make a better informed decision of their ocean use.
Box 1. Ten safety tips to reduce the risk of shark-related injuries24.
Swim, surf, or dive with other people, and do not move too far away from assistance.
Stay out of the water at dawn, dusk, and night, when some species of sharks may move inshore to feed. But be aware that tiger sharks are known to bite people at all times of the day.
Do not enter the water if you have open wounds or are bleeding in any way. Sharks can detect blood and body fluids in extremely small concentrations.
Avoid murky waters, harbor entrances, and areas near stream mouths (especially after heavy rains), channels, or steep dropoffs. These types of waters are known to be frequented by sharks.
Do not wear high-contrast clothing or shiny jewelry. Sharks see contrast very well.
Refrain from excessive splashing; keep pets, which swim erratically, out of the water. Sharks are known to be attracted to such activity.
Do not enter the water if sharks are known to be present and leave the water quickly and calmly if one is sighted. Do not provoke or harass a shark, even a small one.
If fish or turtles start to behave erratically, leave the water. Be alert to the presence of dolphins, as they are prey for some large sharks.
Remove speared fish from the water or tow them a safe distance behind you. Do not swim near people fishing or spearfishing. Stay away from dead animals in the water.
Swim or surf at beaches patrolled by lifeguards and follow their advice.
Acknowledgments
The authors would like to thank Randy Honebrink with the Hawai’i DLNR DAR for his assistance with data collection and his shark expertise. The authors also appreciate the collaboration between The Queen’s Medical Center and Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality.
Footnotes
Presented at: This paper was presented as a poster presentation at the 79th Annual Meeting of AAST and Clinical Congress of Acute Care Surgery.
Contributors: Drafting of the article: VAS. Study conception and design: all authors. Acquisition of data: VAS, KN. Regulatory support: KN. Analysis and interpretation of data: all authors. Critical revision: all authors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: ERH reports research funding from the Patient-Centered Outcomes Research Institute (PCORI), the Agency for Healthcare Research and Quality (AHRQ), the NIH/NHLBI, the DOD/Army Medical Research Acquisition Activity, and the Henry M Jackson Foundation for the Advancement of Military Medicine (HJF). ERH receives royalties from Lippincott Williams & Wilkins for a book, Avoiding Common ICU Errors. ERH was a paid speaker for the Vizient Hospital Improvement Innovation Network (HIIN) VTE Prevention Acceleration Network. The other authors (VAS, MSH, JK, KN, SF) have no conflicts of interest.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the Research and Institutional Review Committee of The Queen’s Medical Center (approval ID# RA-2020-001). This retrospective study was approved with a waiver of informed consent as all medical care had already been provided and subjects were not impacted.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1.Midway SR, Wagner T, Burgess GH. Trends in global shark attacks. PLoS One 2019;14:e0211049–13. 10.1371/journal.pone.0211049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neff C, Hueter R, Science HR. Science, policy, and the public discourse of shark “attack”: a proposal for reclassifying human–shark interactions. J Environ Stud Sci 2013;3:65–73. 10.1007/s13412-013-0107-2 [DOI] [Google Scholar]
- 3.Ricci JA, Vargas CR, Singhal D, Lee BT. Shark attack-related injuries: epidemiology and implications for plastic surgeons. J Plast Reconstr Aesthet Surg 2016;69:108–14. 10.1016/j.bjps.2015.08.029 [DOI] [PubMed] [Google Scholar]
- 4.Lentz AK, Burgess GH, Perrin K, Brown JA, Mozingo DW, Lottenberg L. Mortality and management of 96 shark attacks and development of a shark bite severity scoring system. Am Surg 2010;76:101–6. 10.1177/000313481007600120 [DOI] [PubMed] [Google Scholar]
- 5.Woolgar JD, Cliff G, Nair R, Hafez H, Robbs JV. Shark attack: review of 86 consecutive cases. J Trauma 2001;50:887–91. 10.1097/00005373-200105000-00019 [DOI] [PubMed] [Google Scholar]
- 6.Tomberg RJ, Cachaper GA, Weingart GS. Shark related injuries: a case series of emergency department patients. Am J Emerg Med 2018;36:1645–9. 10.1016/j.ajem.2018.06.059 [DOI] [PubMed] [Google Scholar]
- 7.Ballas R, Saetta G, Peuchot C, Elkienbaum P, Poinsot E. Clinical features of 27 shark attack cases on La Réunion island. J Trauma Acute Care Surg 2017;82:952–5. 10.1097/TA.0000000000001399 [DOI] [PubMed] [Google Scholar]
- 8.Caldicott DGE, Mahajani R, Kuhn M. The anatomy of a shark attack: a case report and review of the literature. Injury 2001;32:445–53. 10.1016/S0020-1383(01)00041-9 [DOI] [PubMed] [Google Scholar]
- 9.Roy M, Plant MA, Snell L. A shark attack treated in a tertiary care centre: case report and review of the literature. Arch Plast Surg 2018;45:80–4. 10.5999/aps.2016.01991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.International Shark Attack File Yearly Worldwide Shark Attack Summary. https://www.floridamuseum.ufl.edu/shark-attacks/yearly-worldwide-summary/ (Published 2020. Accessed June 5, 2020).
- 11.West JG. Changing patterns of shark attacks in Australian waters. Mar. Freshwater Res. 2011;62:744–54. 10.1071/MF10181 [DOI] [Google Scholar]
- 12.American College of Surgeons Stop the Bleed. https://www.stopthebleed.org/ (Accessed June 5, 2020).
- 13.Howard RJ, Bennett NT, Malangoni MA, Meyer AA, Deitch EA, Pruitt BA. Infections caused by halophilic marine Vibrio bacteria. Ann Surg 1993;217:525–31. 10.1097/00000658-199305010-00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buck JD, Spotte S, Gadbaw JJ. Bacteriology of the teeth from a great white shark: potential medical implications for shark bite victims. J Clin Microbiol 1984;20:849–51. 10.1128/JCM.20.5.849-851.1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morris JG, Black RE. Cholera and other vibrioses in the United States. N Engl J Med 1985;312:343–50. 10.1056/NEJM198502073120604 [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention Management of Vibrio Vulnificus Wound Infections. Vibrio Species Causing Vibriosis. https://www.cdc.gov/vibrio/healthcare.html#wounds (Accessed July 16, 2020).
- 17.Hawaii State Department of Business Economic Development and Tourism’s Research and Economic Analysis Division The State of Hawaii Data Book: A Statistical Abstract.;. 2018. http://files.hawaii.gov/dbedt/economic/databook/db2018/DB2018_final.pdf.
- 18.Meyer CG, Anderson JM, Coffey DM, Hutchinson MR, Royer MA, Holland KN. Habitat geography around Hawaii’s oceanic islands influences tiger shark (Galeocerdo cuvier) spatial behaviour and shark bite risk at ocean recreation sites. Sci Rep 2018;8:1–18. 10.1038/s41598-018-23006-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pukui MK, Varez D, Pope B. ’Olelo No’eau : Hawaiian Proverbs & Poetical Sayings. Press BM, ed 6Th, 1997. [Google Scholar]
- 20.Whitney NM, Crow GL. Reproductive biology of the tiger shark (Galeocerdo Cuvier) in Hawaii. Mar Biol 2007;151:63–70. 10.1007/s00227-006-0476-0 [DOI] [Google Scholar]
- 21.State of Hawaii Division of Aquatic Resources Hawai’i Sharks Incident Graphs. https://dlnr.hawaii.gov/sharks/shark-incidents/incident-graphs/ (Accessed September 10, 2019).
- 22.Papastamatiou YP, Meyer CG, Carvalho F, Dale JJ, Hutchinson MR, Holland KN. Telemetry and random-walk models reveal complex patterns of partial migration in a large marine predator. Ecology 2013;94:2595–606. 10.1890/12-2014.1 [DOI] [PubMed] [Google Scholar]
- 23.Honebrink R, Buch R, Galpin P, Burgess GH. First Documented Attack on a Live Human by a Cookiecutter Shark (Squaliformes, Dalatiidae: Isistius sp.). Pacific Science 2011;65:365–74. 10.2984/65.3.365 [DOI] [Google Scholar]
- 24.State of Hawaii Division of Aquatic Resources Safety Tips. https://dlnr.hawaii.gov/sharks/shark-safety/safety-tips/ (Accessed June 5, 2020).