Abstract
Background
Few studies have documented rural community pharmacy disaster preparedness.
Objectives
To: (1) describe rural community pharmacies’ preparedness for and responses to COVID-19 and (2) examine whether responses vary by level of pharmacy rurality.
Methods
A convenience sample of rural community pharmacists completed an online survey (62% response rate) that assessed: (a) demographic characteristics; (b) COVID-19 information source use; (c) interest in COVID-19 testing; (d) infection control procedures; (e) disaster preparedness training, and (f) medication supply impacts. Descriptive statistics were calculated and differences by pharmacy rurality were explored.
Results
Pharmacists used the CDC (87%), state health departments (77%), and state pharmacy associations (71%) for COVID-19 information, with half receiving conflicting information. Most pharmacists (78%) were interested in offering COVID-19 testing but needed personal protective equipment and training to do so. Only 10% had received disaster preparedness training in the past five years. Although 73% had disaster preparedness plans, 27% were deemed inadequate for the pandemic. Nearly 70% experienced negative impacts in medication supply. There were few differences by rurality level.
Conclusion
Rural pharmacies may be better positioned to respond to pandemics if they had disaster preparedness training, updated disaster preparedness plans, and received regular policy guidance from professional bodies.
Keywords: Disaster preparedness, Community pharmacies, Rural health, COVID-19
Introduction
Significant health disparities exist in rural communities, which are commonly health professional shortage areas that lack healthcare infrastructure, including hospitals, specialty clinics, and mental health services.1, 2, 3 As one of the most accessible health professionals in rural areas, pharmacists are well-positioned to provide healthcare services to their communities during a pandemic.1 , 4 Indeed, as essential businesses, pharmacies have remained open and continued services via face-to-face, phone, and online interactions.
Professional bodies have outlined how community pharmacies can support a broad, coordinated response to the COVID-19 pandemic, including through: providing factual and reliable COVID-19 information, educating the public on infection control procedures, implementing referral pathways for suspected cases, and maintaining continuity of pharmacy services, including supplying over-the-counter and prescription medications.5 Pharmacies can also serve as sites for delivery of coronavirus testing and, eventually, immunizations.6 Rural pharmacies’ ability to fulfill these functions depends on their level of disaster preparedness. To date, the only study that has explored rural pharmacy disaster preparedness found that rural pharmacies had lower levels of basic preparedness, including emergency power, certified pharmacy immunization staff, and a formal disaster plan.7 This study seeks to add to the limited literature on rural community pharmacy disaster preparedness by documenting their preparedness for and responses to COVID-19.
Methods
Overview. This cross-sectional survey study was conducted with a convenience sample of rural community pharmacies that are part of the Rural Research Alliance of Community Pharmacies (RURAL-CP). RURAL-CP is a multi-state practice-based research network that comprises 100 rural community pharmacies in Alabama, Arkansas, Mississippi, North Carolina, and South Carolina.
RURAL-CP pharmacists received an email describing the study and a link to the 10-min online survey. The survey was distributed on April 3, 2020 and closed on May 15, 2020. Pharmacists received a $25 incentive. IRB-approved exemption was obtained from the first author's institution.
Measures. The survey included 38 questions that assessed pharmacists’: (a) demographic and pharmacy characteristics; (b) use of nine sources of COVID-19 information; (c) interest in COVID-19 testing; (d) infection control procedures; (e) disaster preparedness training and readiness, (f) and medication supply impact. Pharmacy rurality was measured via rural-urban commuting area (RUCA) codes; whereby large rural towns were designated by RUCA codes 4–7, small rural towns as RUCA codes 8–9, and isolated rural towns as RUCA code 10.8
Data analysis. IBM SPSS Statistics Version 25 was used to calculate descriptive statistics. Pearson chi-squared tests were used to examine differences in variables by pharmacy rurality. Coders used Microsoft Excel to categorize and tally responses to open-ended questions.9
Results
Sixty-two pharmacists completed the survey (response rate = 62%; Table 1 ). At the time they completed the survey, only two pharmacists had not had a confirmed case of COVID-19 in their county.
Table 1.
Pharmacist characteristics and COVID-19 preparedness (N = 62).
| Variable | Mean (SD) or N (%) |
|---|---|
| Pharmacist characteristics | |
| Age (range: 28–71 years) | 44.1 (10.9) |
| Male gender | 33 (53) |
| White race | 59 (95) |
| Years practiced as pharmacist (range: 1–50) | 20.6 (12.2) |
| Highest pharmacy degree | |
| PharmD | 41 (66) |
| BSPharm | 18 (29) |
| Other | 2 (3) |
| Pharmacy Characteristics | |
| Type | |
| Independent | 55 (89) |
| Grocery chain | 4 (7) |
| National chain | 2 (3) |
| Has drive-through | 32 (52) |
| Is CLIA-waivered siteb | 24 (39) |
| State | |
| Alabama | 17 (27) |
| Arkansas | 9 (15) |
| Mississippi | 6 (10) |
| North Carolina | 17 (27) |
| South Carolina | 13 (21) |
| Ruralitya | |
| Large rural town (RUCA 4–6) | 26 (42) |
| Small rural town (RUCA 7–9) | 23 (37) |
| Isolated rural town (RUCA 10) | 13 (21) |
| COVID-19 information sources | |
| CDC | 54 (84) |
| State health department | 48 (77) |
| State pharmacy association | 44 (71) |
| National pharmacy association | 32 (52) |
| Local news outlet | 25 (40) |
| Local health department | 16 (26) |
| National news/media outlet | 15 (24) |
| School/college of pharmacy | 8 (13) |
| Received conflicting COVID-19 information |
31 (50) |
| Variable |
Mean (SD) or N (%) |
| COVID-19 testing | |
| Can recognize patients who should be tested for COVID-19 | |
| Strongly disagree | 1 (2) |
| Somewhat disagree | 2 (3) |
| Neither agree nor disagree | 9 (15) |
| Somewhat agree | 36 (58) |
| Strongly agree | 14 (23) |
| Knows where to refer patients for COVID-19 testing | |
| Strongly disagree | 5 (8) |
| Somewhat disagree | 3 (5) |
| Neither agree nor disagree | 3 (5) |
| Somewhat agree | 17 (27) |
| Strongly agree | 34 (54) |
| Is interested in offering COVID-19 testing at their pharmacy | |
| Not at all interested | 17 (27) |
| Slightly interested | 19 (31) |
| Fairly interested | 15 (24) |
| Very interested | 11 (18) |
| Disaster Preparedness | |
| Pharmacy is well-prepared to respond to COVID-19 | |
| Strongly disagree | 2 (3) |
| Somewhat disagree | 6 (10) |
| Neither agree nor disagree | 11 (18) |
| Somewhat agree | 33 (53) |
| Strongly agree | 10 (16) |
| Feels prepared as a pharmacist to respond to COVID-19 | |
| Strongly disagree | 2 (3) |
| Somewhat disagree | 3 (5) |
| Neither agree nor disagree | 9 (15) |
| Somewhat agree | 35 (57) |
| Strongly agree | 13 (21) |
| Has participated in an actual emergency response in the past 5 years (other than COVID-19) | 6 (10) |
| Pharmacy has a disaster preparedness plan | |
| Yes | 45 (73) |
| No | 11 (18) |
| Unsure | 6 (10) |
| Believes pharmacy's disaster preparedness plan is adequate for COVID-19 (N = 45) | 33 (73) |
All pharmacies have a rural-urban commuting area (RUCA) code greater than or equal to four.8
CLIA sets federal regulatory standards for all clinical laboratory testing. A CLIA waiver allows for use of simple tests with low risk of incorrect results. Most point-of-care tests are CLIA waived tests.
Information sources. Pharmacists commonly used the CDC (87%), their state health department (77%), and their state pharmacy association (71%) for COVID-19 information. Half of pharmacists received conflicting COVID-19 information, most commonly about the effectiveness of masks at preventing transmission (21%), how the virus is transmitted (11%), and potential treatments (6%). For example, one pharmacist stated, “ACE inhibitors and ARBs have conflicting evidence as to whether they are helpful or harmful. There is also a lot of uncertainty about the use of face masks.” There were no significant differences in use of information sources or receipt of conflicting information by pharmacy rurality.
COVID-19 testing. Most pharmacists (81%) agreed they could recognize patients who should be tested for COVID-19 (Table 1). However, only 54% strongly agreed that they knew where to refer patients for testing. Many (73%) were interested in offering COVID-19 testing at their pharmacies, but reported needing personal protective equipment (PPE) (n = 32), training on how to administer and bill for tests (n = 17), and testing supplies (n = 13) to offer testing. State policies (such as statewide standing orders), staff, and a safe space to test were also mentioned as needed resources to implement testing. In one pharmacist's own words, “I would need training and the capability to legally administer and bill for the tests. I would also need better access to PPE.” There were no significant differences in COVID-19 testing variables by pharmacy rurality.
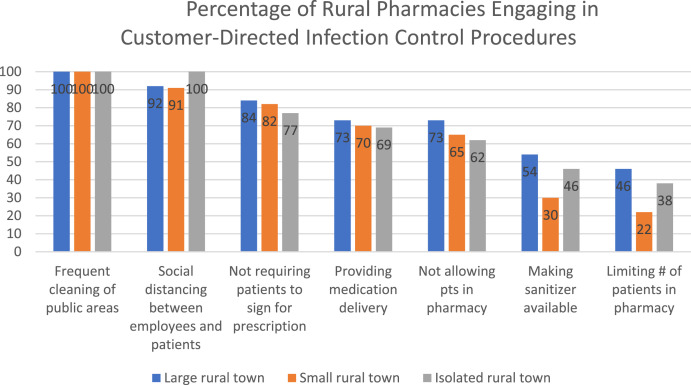
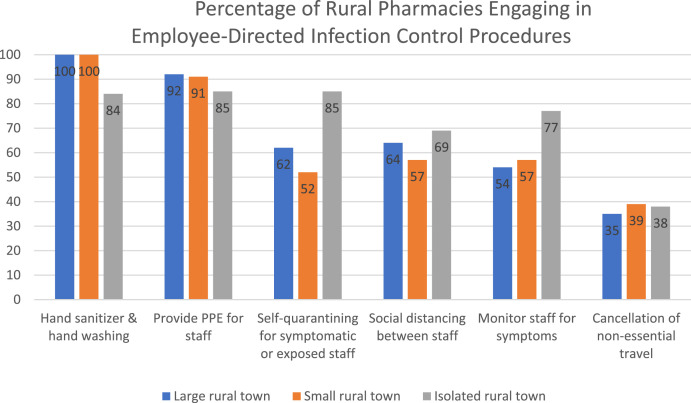
Infection control procedures. Most pharmacies had implemented several customer (Fig. 1 ) and staff (Fig. 2 ) infection control measures. All pharmacies had implemented frequent cleaning of public areas, and most emphasized frequent staff use of hand sanitizer/hand washing (97%) and social distancing (94%). For customers, pharmacies were least likely to have an isolated area for suspected COVID-19 patients (7%) or provide masks to asymptomatic patients (2%). For staff, pharmacies were least likely to cancel non-essential staff travel (37%) or update sick leave policies (25%). Isolated rural pharmacies were significantly less likely to emphasize frequent hand washing or use of hand sanitizer than pharmacies in larger rural towns (ᵡ2 (2) = 7.79, p = 0.02).
Fig. 1.
Percentage of rural pharmacies engaging in customer-directed infection control procedures.
Fig. 2.
Percentage of rural pharmacies engaging in employee-directed infection control procedures.
Disaster preparedness. Most pharmacists felt personally prepared to respond to COVID-19 (78%), but fewer (69%) agreed that their pharmacy was well-prepared. Only six pharmacists (10%) had participated in public health disaster training in the past five years. Those trainings primarily focused on natural disasters (e.g., hurricanes) or fires/burglaries. The majority of pharmacists (94%) were interested in participating in formal emergency preparedness training.
Most pharmacies (73%) reported having disaster preparedness plans. Among these pharmacies, 27% believed their plan was inadequate for COVID-19. Inadequacies described related to the current plan's focus on physical or weather threats rather than infectious disease. For example, one pharmacist responded: “We need a formal plan to split the workforce if some test positive or are placed in quarantine. Who would work if both pharmacists are out? We have devised a plan but not put it into a formal plan.” Pharmacists thought plans should be adjusted to: (a) address adequate supply of PPE, (b) include procedures to protect against medication shortages, (c) describe infection control procedures, and (d) address workforce planning. There were no significant differences in disaster preparedness variables by pharmacy rurality.
Medication supply impacts. Sixty-nine percent of pharmacies had been affected by early refills and 90-day supply prescriptions, including drug shortages/inability to fill prescriptions (n = 16), increased demand for prescriptions (n = 12), increased workload (n = 7), and cash flow shortages due to the time-period between ordering a 90-day supply and being reimbursed (n = 6). Pharmacists noted the following medications were difficult to obtain: hydroxychloroquine (n = 45), antibiotics including azithromycin (n = 27), respiratory inhalers (n = 24), diabetes medications (n = 8), over-the-counter pain and fever medications (n = 7), and other over-the-counter products like zinc and Vitamin C (n = 7). Pharmacists also noted PPE and isopropanol shortages.
Half of pharmacists (n = 31) reported that individuals had attempted to fill speculated prophylactic treatments for COVID-19 (e.g., chloroquine, hydroxycholorquine, azithromycin), of which 18 (29%) refused to fill. Over time, an evolution of filling behavior was apparent whereby pharmacists initially filled speculated prophylactic prescriptions for hydroxycholorquine and azithromycin, but after state boards of pharmacy released guidance about filling, the pharmacists would then refuse to fill those prescriptions citing guidance from those organizations. A few pharmacists also noted suspicious orders, including an abnormal increase in the number of people who had been diagnosed with lupus. There were no differences in medication supply impact variables by pharmacy rurality.
Discussion
This study adds new insights into rural pharmacies’ pandemic preparedness and responses. Although most pharmacies had disaster preparedness plans, more than a quarter were deemed by the pharmacists to be inadequate for COVID-19. Plans that were developed before the pandemic often focused on physical threats, which made them deficient for addressing the unique challenges of a pandemic, such as ordering PPE and planning for staff quarantining and shortages. Additionally, few pharmacists had received disaster preparedness training, even though the overwhelming majority were interested in participating in such training. These findings underscore the importance of training pharmacists in rural communities in disaster preparedness.
Because many rural pharmacies are geographically isolated and travel to participate in trainings can be cost- and time-prohibitive, creating mobile teams that visit pharmacists' communities to offer disaster preparedness training and help adapt disaster preparedness plans could increase training participation. Furthermore, because some rural areas do not have access to reliable high-speed Internet, mobile teams would be particularly important for these hard-to-reach pharmacies. There was only one difference between pharmacies’ preparedness and responses to COVID-19 based on level of rurality, suggesting that, overall, there may not be a strong need to tailor disaster preparedness training on that basis.
Several factors influenced rural pharmacies' ability to contribute to a broad, coordinated community response to COVID-19. First, receiving conflicting information about mask effectiveness and potential treatments could negatively impact pharmacies' ability to provide factual and reliable COVID-19 information to customers and educate the public on infection control procedures. Pharmacists used a variety of high-quality information sources (e. g., CDC, health departments) but need continued informational support from these organizations to convey up-to-date reliable information to the public. As recommendations for COVID-19 testing and treatment continue to evolve, pharmacists may also need to address their customers’ scientific literacy by explaining how previous coronavirus recommendations can be supplanted by newer recommendations as the body of high-quality scientific evidence grows.
Second, medication shortages negatively impacted rural pharmacies' ability to maintain continuity of pharmacy services and supply the public with essential medications, including antibiotics, speculated COVID-19 treatments, chronic disease medications, and over-the-counter products. Again, policy guidance from professional organizations can help pharmacies mitigate increased public demand for medications and supplies. In particular, receiving early guidance on how to prioritize the distribution of high-demand products and manage patients' desire to obtain excess supplies of maintenance medications would help pharmacists better serve the public's health to ensure that the highest need individuals are the first to received limited medications and supplies. Also, caution should be taken when recommendations are made to the public to obtain an excess supply of their maintenance medications without first preparing for the negative impact on drug supply (i.e., panic buying).
Rural pharmacies had implemented a number of infection control measures for both customers and staff. There was near universal implementation of frequent cleaning of the pharmacy and social distancing between staff and employees. Additionally, the vast majority of pharmacies provided staff with PPE. Areas for improvement included self-quarantining of potentially exposed or symptomatic employees, monitoring of staff symptoms, and providing customers with hand sanitizer. It is possible that more pharmacies have implemented these infection control precautions since completing the survey in April. However, pharmacies also noted lack of PPE and sanitizer, which could impede their ability to implement these precaution measures. Additionally, the availability of floaters or temporary staff is limited in rural areas, so options for adequately staffing the pharmacy when an employee is out are more limited.
Approximately half of rural pharmacists strongly agreed that they know where to refer patients for testing, which suggests that rural pharmacies’ ability to implement referral pathways for suspected COVID-19 patients could be improved. Rural health departments and other healthcare organizations should make sure they include pharmacies when they communicate about test site availability. Many rural pharmacies were willing to serve as testing sites, but reported needing PPE, testing supplies, and training to offer coronavirus testing. With over 68,000 pharmacies in the U.S.4, rural pharmacies are logical locations for testing and immunizations. However, federal and/or state governments will need to enact legislation, such as statewide standing orders, to allow pharmacists to provide and bill for these services.
Limitations. Several study limitations should be noted. First, using a convenience sample of rural pharmacies in five southeastern states limits generalizability; rural pharmacies in other regions may have responded differently. Second, pharmacists who responded to this survey may differ from non-respondents in that they may have been more affected by COVID-19. Additionally, most surveys were completed in April 2020 and pharmacists’ opinions about COVID-19 impacts and responses may change over time. Last, the exploratory analysis of differences by rurality was limited by a small sample size, even though one significant difference in infection control procedures was detected.
Conclusion
Rural pharmacies could better respond to pandemics if they had the appropriate disaster preparedness training, updated disaster preparedness plans that addressed infectious disease, and received regular policy and informational guidance from professional bodies and state and national health organizations.
Funding support
The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR002489 and the Eshelman Institute for Innovation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Dr. Curran was supported by the Translational Research Institute (TRI), UL1 TR003107, through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH).
Declaration of competing interest
The authors declare no relevant conflicts of interest or financial relationships.
References
- 1.Knapp K.K., Paavola F.G., Maine L.L., Sorofman B., Politzer R.M. Availability of primary care providers and pharmacists in the United States. J Am Pharmaceut Assoc. 1996;39(2):127–135. doi: 10.1016/s1086-5802(16)30486-7. 1999. [DOI] [PubMed] [Google Scholar]
- 2.Lin S.-J. Access to community pharmacies by the elderly in Illinois: a geographic information systems analysis. J Med Syst. 2004;28(3):301–309. doi: 10.1023/b:joms.0000032846.20676.94. [DOI] [PubMed] [Google Scholar]
- 3.Casey M.M., Klingner J., Moscovice I. Pharmacy services in rural areas: is the problem geographic access or financial access? J Rural Health. 2002;18(3):467–477. doi: 10.1111/j.1748-0361.2002.tb00911.x. [DOI] [PubMed] [Google Scholar]
- 4.Qato D.M., Zenk S., Wilder J., Harrington R., Gaskin D., Alexander G.C. The availability of pharmacies in the United States: 2007–2015. PloS One. 2017;12(8) doi: 10.1371/journal.pone.0183172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cadogan C.A., Hughes C.M. On the frontline against COVID-19: community pharmacists' contribution during a public health crisis. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.015. Epub ahead of print: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hedima E.W., Adeyemi M.S., Ikunaiye N.Y. Community pharmacists: on the frontline of health service against COVID-19. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.013. Epub ahead of print: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henkel P.J., Marvanova M. Basic disaster preparedness of rural community pharmacies in 5 states. Disaster Med Public Health Prep. 2019:1–6. doi: 10.1017/dmp.2019.57. [DOI] [PubMed] [Google Scholar]
- 8.United States Department of Agriculture Rural-urban commuting area codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx Updated October 12, 2016. Accessed February 28, 2019.
- 9.Strauss A., Corbin J. Thousand Oaks, CA: Sage. 1998. Basics of qualitative research: procedures and techniques for developing grounded theory. [Google Scholar]