Abstract
A multicentre cross-sectional study was conducted to assess perceived risk and fear of contagion, as well as mental health outcomes among 650 Italian healthcare workers during the COVID-19 outbreak. A relevant proportion of the sample reported symptoms of anxiety, depression, and distress. Female sex, nursing profession, fear of being infected, as well as the time of exposure to the COVID-19 spread and the fact of directly attending infected patients were the main risk factors for developing mental health disturbances. Tailored interventions need to be implemented to reduce psychological burden in healthcare workers, with a particular attention to nurses.
Keywords: Pandemic, Hospital staff, Nurses, Psychological impact
Highlights
-
•
Italian healthcare workers present a significant incidence of psychological symptoms.
-
•
Females and nurses show more psychological symptoms compared to other workers.
-
•
Risk perception and specific working variables explain the incidence of mental symptoms.
-
•
Observed mental burden is higher than in Chinese studies performed in the very first weeks.
Introduction
COVID-19 spread is actually causing an unprecedented psychological stress on people worldwide, and in particular on the nursing and medical workforce, committed to the front line to face one of the most serious disaster of the history in terms of hospitalizations and deaths. In such a dramatic condition, healthcare providers are facing a high risk of contracting the disease, with a growing number of them who already died for it (Hassanian-Moghaddam et al., 2020), as well as an increased risk of developing mental health symptoms such as anxiety, depression, insomnia, work-related stress and post-traumatic stress disorder (Lai et al., 2020).
Despite the fact that COVID-19 spread has started quite recently, there are already some published studies investigating its impact on mental health of healthcare workers in China, India and Malesia, where the pandemic spread originated. Mainly, these results show that physicians, nurses and other staff started manifesting moderate to severe psychological disturbances (Chew et al., 2020; Zhu et al., 2020) already in the immediate wake of the viral epidemic (Kang et al., 2020). Such emotional distress is mainly associated to risk perception, countless death, perceived uncontrollability of the hazard, long work shifts, and working directly with Covid-19 patients. Moreover, also some sociodemographic and working-related factors such as being female (Wu et al., 2009; Chen et al., 2005; Styra et al., 2008; Lu et al., 2020; Zhu et al., 2020), having a longer job seniority (Li et al., 2020; Zhu et al., 2020) and being non-medical healthcare providers (Tan et al., 2020) appear to significantly contribute to the workers' emotional burden. Since there is also a large literature demonstrating the dramatic psychological impact of previous epidemics (i.e. SARS outbreak) (Brooks et al., 2020), further studies are needed to explore factors associated with mental health among health care workers exposed to COVID-2019 in order to develop timely psychological interventions to reduce them (Neto et al., 2020).
Regarding Italy, it has been the first European nation to be affected by COVID-19 with, at the time of this writing, 223,885 cases reported and 31,610 associated fatalities, largely exceeding the numbers in China (WHO, 2020). However, to our knowledge, there is actually only one published study that analyzed the effects of COVID-19 spread on the Italian healthcare providers (Rossi et al., 2020) showing that a substantial proportion of them, and young women in particular, developed mental health issues, including post-traumatic stress disorder (PTSD). In order to further investigate this issue, the aim of this study was to conduct a multicentre cross-sectional in-hospital assessment to evaluate mental health outcomes among different categories of Italian healthcare workers during the second month of the COVID-19 outbreak. Specifically, we explored: a) the workers' perceived risk and fear related to COVID-19 contagion for themselves and their family members, b) the magnitude of symptoms of anxiety, depression, and distress emerged, and c) the potential risk factors associated with mental health symptoms.
Method
Participants
During the COVID-19 outbreak, healthcare professionals from two Italian hospitals (Istituti Clinici Scientifici Maugeri, IRCCS [Maugeri] and Centro Cardiologico Monzino, IRCCS [CCM]) were invited to participate to an online cross-sectional survey conducted using the Qualtrics® platform from April 1st to May 1st 2020. Both these hospitals are located in Lombardy, the Italian region registering the highest number of COVID-19 cases of the entire country (Percudani et al., 2020), and underwent a major reorganization with several units admitting almost exclusively COVID-19 patients.
The present study was approved by the local Scientific Ethics Committee (Maugeri approval number 2411, 26 March 2020; CCM approval number 1238, 17 April 2020) and all participants provided the informed consent to participate. The survey was anonymous, and confidentiality of information was assured. Once started to fill in the survey, subjects could quit it at any time without any consequence.
Instruments
The survey, specifically developed for this study, included the following different domains: (a) socio-demographics (e.g., age, sex, marital status, number of children, presence of elderly parents); (b) work-related information (e.g., place of work, occupation, job seniority, directly attending COVID patients); and (c) the perceived impact of COVID-19 on workplace and on individual working activities (e.g., confidence in Personal Protection Equipment [PPE] measures, and sources of COVID-19 work-related stress). These domains were chosen on the basis of the available literature and on the shared opinions of experts working and caring for COVID-19 patients. Furthermore, participants were asked to answer questions about their own physical (e.g. COVID-19 positivity) and mental health status. In particular, the following psychological domains were investigated:
-
-
Perceived risk and fear of infection related to COVID-19: these two aspects were assessed using four items asking participants to quantify, on a 0–100 slider scale, a) their personal perceived risk of being infected; b) the perceived risk that their family members could be infected; c) their fear of being infected; and d) their fear about the possibility that their family members could be infected.
-
-
Mental health status: the general mental health status was assessed using the PHQ-4 questionnaire (Patient Health Questionnaire - 4) (Kroenke et al., 2009) that is a validated ultra-brief tool for detecting both anxiety and depressive symptoms. The PHQ-4 consists of the first two items of the Generalized Anxiety Disorder scale (GAD-7) (Spitzer et al., 2006) and the first two items of the longer Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001). Responses are provided on a Likert scale ranging from 0 (=“not at all”) to 3 (=“nearly every day”). A total score ≥ 6 for the PHQ-4, or ≥3 for the two subscales indicates the presence of mild symptoms, while a total score ≥ 9 for the PHQ-4, or ≥5 for the two subscales indicates the presence of severe symptoms (Löwe et al., 2010). Because of its excellent operating characteristics (Kroenke et al., 2009), the PHQ-4 may well substitute for its parent scales (the GAD-7 and PHQ-9), being very useful to assess depression and anxiety in busy clinical and non-clinical settings and conditions, such as the COVID-19 emergency, in which healthcare providers had very few times to complete questionnaires.
-
-
Psychological distress: psychological distress induced by the COVID-19 outbreak was assessed using the Impact of Event Scale-Revised (IES-R) (Creamer et al., 2003) which is a validated 22-item self-report that measures the subjective distress caused by traumatic events. It includes 3 subscales measuring the following dimensions: intrusion, avoidance and hyperarousal. Participants were asked to rate their level of distress using a 5-point Likert scale ranging from 0 (=“not at all”) to 4 (= “often”) referring to the previous seven days. A total score ranging from 0 to 23 indicates the absence of relevant symptoms, from 24 to 32 the presence of mild symptoms, from 33 to 36 the presence of moderate symptoms, and >37 the presence of a severe psychological impact (Creamer et al., 2003; Weiss, 2007).
Statistical analyses
Categorical variables are expressed as absolute values (percentage) while continuous variables are expressed as mean ± standard deviation. Comparisons between healthcare professionals or sex were performed using ANOVA test for continuous variables, while categorical variables were compared using the Chi-square test. To assess difference between the perceived risk or fear of contagion between the respondents and their families, paired t-tests were performed. In order to evaluate the factors independently associated with the different scores obtained from the psychological questionnaires and the related subclasses, multivariable linear regressions with stepwise selection of variables was implemented including all the potential predictors (see Table 1 and Fig. 1 ). The independent contribution of each predictor to the variability of the dependent variables was quantified by the squared partial correlation coefficient.
Table 1.
Characteristics of study participants (N = 650).
| Total (n = 650) | Physicians (n = 177) | Nurses (n = 214) | Other healthcare professionals (n = 217) | Administrative staff (n = 42) | p | |
|---|---|---|---|---|---|---|
| Sociodemographic variables | ||||||
| Age | 44.59 ± 11.1 | 48.75 ± 10.4 | 42.82 ± 10.6 | 43.12 ± 11.3 | 43.43 ± 10.7 | <.001 |
| Sex - Female | 439 (67.5%) | 100 (56.5%) | 172 (80.4%) | 140 (64.5%) | 27 (64.3%) | <.001 |
| Marital status | ||||||
| Single | 93 (14.3%) | 15 (8.5%) | 32 (15%) | 38 (17.5%) | 8 (19%) | .031 |
| In a relationship | 146 (22.5%) | 35 (19.8%) | 58 (27.1%) | 46 (21.2%) | 7 (16.7%) | |
| Engaged or married | 335 (51.5%) | 110 (62.1%) | 95 (44.4%) | 112 (51.6%) | 18 (42.9%) | |
| Divorced or separated | 58 (8.9%) | 14 (7.9%) | 20 (9.3%) | 16 (7.4%) | 8 (19%) | |
| Widower | 5 (0.8%) | 2 (1.1%) | 2 (0.9%) | 1 (0.5%) | 0 (0%) | |
| Other | 13 (2%) | 1 (0.6%) | 7 (3.3%) | 4 (1.8%) | 1 (2.4%) | |
| Children - Yes | 380 (58.5%) | 118 (66.7%) | 118 (55.1%) | 124 (57.1%) | 20 (47.6%) | .045 |
| Parents > 65 years - Yes | 440 (67.7%) | 128 (72.3%) | 148 (69.2%) | 135 (62.2%) | 29 (69%) | |
| Working-related variables | ||||||
| Work place - Maugeri | 453 (69.7%) | 126 (71.2%) | 145 (67.8%) | 171 (78.8%) | 11 (26.2%) | <.001 |
| Work place - CCM | 197 (29.2%) | 51 (28.8%) | 69 (32.2%) | 46 (21.2%) | 31 (73.8%) | |
| Job seniority | .139 | |||||
| >20 years | 321 (49.4%) | 91 (51.4%) | 110 (51.4%) | 99 (45.69%) | 21 (50%) | |
| <20 and >10 years | 160 (24.6%) | 53 (29.9%) | 45 (21%) | 52 (24%) | 10 (23.8%) | |
| <10 years | 169 (26%) | 33 (18.6%) | 59 (27.6%) | 66 (30.4%) | 11 (26.2%) | |
| COVID-19-related variables | ||||||
| Directly attending COVID patients Yes | 395 (60.8%) | 115 (65%) | 136 (63.6%) | 123 (56.7%) | 21 (50%) | .135 |
| Workers positive to COVID-19 | <.001 | |||||
| Never tested | 288 (44.3%) | 62 (35%) | 88 (41.1%) | 107 (49.4%) | 31 (73.8%) | |
| Tested, but negative | 336 (51.7%) | 107 (60.5%) | 115 (53.7%) | 104 (47.9%) | 10 (23.8%) | |
| Yes, in the past | 21 (3.2%) | 5 (2.8%) | 11 (5.1%) | 4 (1.8%) | 1 (2.4%) | |
| Yes, actually | 5 (0.8%) | 3 (1.7%) | 0 (0%) | 2 (0.9%) | 0 (0%) | |
| Impact of COVID-19 on working activities | <.001 | |||||
| Not at all | 37 (5.7%) | 9 (5.1%) | 7 (3.3%) | 16 (7.4%) | 5 (11.9%) | |
| A little bit | 118 (18.2%) | 35 (19.8%) | 28 (13.1%) | 47 (21.7%) | 8 (19%) | |
| Moderately | 156 (24%) | 44 (24.9%) | 39 (18.2%) | 65 (30%) | 8 (19%) | |
| A lot | 200 (30.8%) | 63 (35.6%) | 76 (35.5%) | 51 (23.59%) | 10 (23.8%) | |
| Absolutely yes | 139 (21.4%) | 26 (14.7%) | 64 (29.9%) | 38 (17.5%) | 11 (26.2%) | |
| From how long | .575 | |||||
| <1 week | 5 (0.8%) | 1 (0.6%) | 2 (0.9%) | 2 (0.9%) | 0 (0%) | |
| >1 and <2 weeks | 14 (2.2%) | 3 (1.7%) | 3 (1.4%) | 8 (3.7%) | 0 (0%) | |
| >2 and <3 weeks | 41 (6.3%) | 11 (6.2%) | 18 (8.4%) | 11 (5.1%) | 1 (2.4%) | |
| >3 weeks | 590 (90.7%) | 162 (91.5%) | 191 (89.3%) | 196 (90.3%) | 41 (97.6%) | |
| Availability of PPE | .601 | |||||
| Not at all | 35 (5.4%) | 7 (4.0%) | 13 (6.1%) | 13 (6.0%) | 2 (4.8%) | |
| A little bit | 189 (29.1%) | 50 (28.2%) | 56 (26.2%) | 66 (30.4%) | 17 (40.5%) | |
| Enough | 274 (42.2%) | 76 (42.9%) | 95 (44.4%) | 92 (42.4%) | 11 (26.2%) | |
| A lot | 131 (20.2%) | 35 (19.8%) | 44 (20.6%) | 41 (18.9%) | 11 (26.2%) | |
| Absolutely yes | 21 (3.2%) | 9 (5.1%) | 6 (2.8%) | 5 (2.3%) | 1 (2.4%) | |
| Work shift during COVID-19 emergency - Yes | 319 (49.1%) | 92 (28.8%) | 164 (76.6%) | 54 (24.9%) | 9 (21.4%) | <.001 |
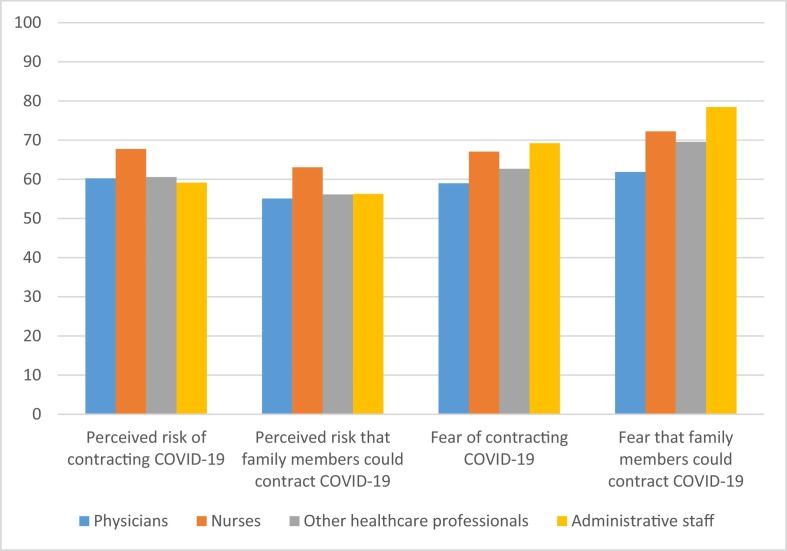
Fig. 1.
Perceived risk and fear for themselves and for family members about COVID-19 contagion among the different categories of healthcare workers.
The significance level was p < .05 (two-tailed) except for the multivariable analysis, where a more conservative p < .01 was chosen, in order to account for multiple testing. All the analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, US).
Results
Participants' characteristics
In this cross-sectional survey, we retrieved a total of 770 questionnaires. Of which, 73 questionnaires were excluded for the irrational completion time, and 47 incomplete questionnaires were also eliminated. The remaining 650 questionnaires were completed eligibly, giving an overall response rate of 84.4%.
The respondents included 177 physicians, 214 nurses, 217 other healthcare professionals (psychologists, physiotherapists, dieticians, and speech therapists), and 42 administrative staff (including the logistics). The detailed demographic characteristics are presented in Table 1. The largest proportion of female respondents was found in the nurses group (80.4%), while the physicians were those with the highest age (mean = 48.75 ± 10.4 years). Almost half of all workers had a job seniority longer than 20 years (49.4%).
Regarding data related to the COVID-19 emergency, at the time of assessment 60.8% of all responders were working in units with COVID patients. Half of responders (51.7%) were tested for COVID-19 and were negative. Most of those tested were physicians (60.5%). Among those never tested, 20.3% were worried to be positive.
Many physicians (50.3%) and nurses (65.4%) declared that the COVID-19 emergency had a high impact on their everyday working activities. Among them, 29.9% of nurses and only 14.7% of physicians affirmed that the impact was extremely high. For the 90.7% of all responders the COVID-19 impact was present from more than 3 weeks.
We also asked responders to evaluate the availability of PPE in their working places, finding that 34.5% of them declared that available PPE were not enough.
Measures adopted to protect family members and perceived risk and worries about contagion
Starting from the beginning of the COVID-19 spread, 9.3% of responders who used to live with their relatives decided to move in a separate apartment, 9.0% isolated themselves from their relatives when came back home, and 36.9% started to use PPE at home in order to protect people living with them. The remaining responders decided to not use any kind of precautions at home because they did not have the possibility to do it (for example, the apartment was too small to stay separate from their relatives) (17.6%) or because they thought it was not necessary (13.3%).
In general, healthcare workers thought they were more at risk (M = 62.87, SD = 24.20) than their family members who lived with them (M = 58.22, SD = 27.90) to contract the virus (t(428) = 2.34, p = .02). On the contrary, they were more worried about possible contagion for their family members (M = 69.76, SD = 28.91) than for themselves (M = 66.33, SD = 29.18) (t(443) = −2.87, p = .004). Significant differences were also found among different categories of healthcare providers both in the perceived risk and in the fear of contagion for themselves and for their family members. Regarding the perceived risk of being infected, there was a statistically significant difference between groups of healthcare providers as determined by one-way ANOVA (F(3,561) = 4.104, p = .007). In particular, a Tukey post hoc test revealed that nurses (M = 67.73 ± 24.20) felt themselves more at risk of contracting the virus than physicians (M = 60.25 ± 25.55) (p = .02) and other healthcare workers (M = 60.57 ± 22.06) (p = .02). On the contrary, no statistically significant differences were found among the different groups regarding the perceived risk that family members could be infected (p = .06).
Regarding the fear of being infected, different groups did not show any significant difference (F(3,572) = 2.739, p = .06). On the contrary, nurses (M = 67.07 ± 29.54) (p = .02) and administrative staff (M = 69.19 ± 28.78) (p = .04) were more worried than physicians (M = 58.99 ± 29.76) about the possibility that their family members could become infected (F(3,474) = 4.325, p = .005) (see Fig. 1).
No significant differences were found between the different categories of healthcare workers and the precautions adopted at home (X2 (15, N = 547) = 19.724, p = .183).
Perceived effects of COVID-19 on the working routine
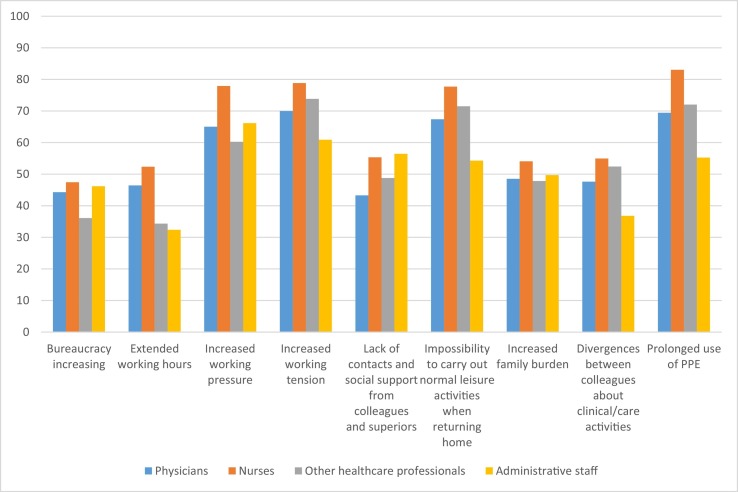
As described above, most of responders declared that the COVID-19 spread had a significant impact on their everyday workload (see Table 1). The main reasons why this happened are reported in Fig. 2 .
Fig. 2.
Main reasons that, according to the different categories of workers, were responsible of the impact of COVID-19 on the daily working activity. Note that the variable named “Working pressure” refers to the increased number of work-related requests occurred during the COVID-19 emergency, while the variable “Working tension” regards the increased tension in the working climate.
Psychological outcomes
Data obtained from psychological questionnaires showed that, in general, women presented higher scores than men, while physicians presented lower scores than the other workers in all the investigated domains (see Table 2 ).
Table 2.
Comparison of the prevalence of anxiety, depression and distress among the different categories of healthcare workers, and between males and females.
| N tot (%) | Physicians (n = 177) | Nurses (n = 214) | Other healthcare professionals (n = 217) | Administrative staff (n = 42) | X2 | p value | Males | Females | X2 | p value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PHQ-4 | 11.287 | .080 | 20.583 | <.001 | |||||||
| <6 No symptoms |
496 (76.3) | 143 (80.8) | 151 (70.6) | 171 (78.8) | 31 (73.8) | 184 (87.2) | 312 (71.1) | ||||
| ≥6 Mild symptoms |
87 (13.4) | 25 (14.1) | 33 (15.4) | 23 (10.6) | 5 (11.9) | 16 (7.6) | 71 (16.2) | ||||
| ≥9 Severe symptoms |
67 (10.3) | 9 (5.1) | 30 (14.0) | 23 (10.6) | 5 (11.9) | 11 (5.2) | 56 (12.8) | ||||
| GAD-2_Anxiety | 13.821 | .032 | 18.109 | <.001 | |||||||
| <3 No symptoms |
457 (70.3) | 137 (77.4) | 136 (63.6) | 157 (72.4) | 27 (64.3) | 171 (81) | 286 (65.1) | ||||
| ≥3 Mild symptoms |
116 (17.8) | 27 (15.3) | 50 (23.4) | 30 (13.8) | 9 (21.4) | 27 (12.8) | 89 (20.3) | ||||
| ≥5 Severe symptoms |
77 (11.8) | 13 (7.3) | 28 (13.1) | 30 (13.8) | 9 (21.4) | 13 (6.2) | 64 (14.6) | ||||
| PHQ-2_Depression | 1.602 | .024 | 17.670 | <.001 | |||||||
| <3 No symptoms |
502 (77.2) | 144 (81.4) | 148 (69.2) | 178 (82.0) | 32 (76.2) | 184 (87.2) | 318 (72.4) | ||||
| ≥3 Mild symptoms |
104 (16.0) | 26 (14.7) | 43 (20.1) | 28 (12.9) | 7 (16.7) | 19 (9.0) | 85 (19.4) | ||||
| ≥5 Severe symptoms |
44 (6.8) | 7 (4.0) | 23 (10.7) | 11 (5.1) | 3 (7.1) | 8 (3.8) | 36 (8.2) | ||||
| IES-R | 23.333 | <.001 | |||||||||
| 0–23 No symptoms |
356 (55.1) | 120 (67.8) | 87 (41.0) | 127 (59.1) | 22 (52.4) | 144 (68.6) | 212 (48.6) | ||||
| 24–32 Mild symptoms |
104 (16.1) | 21 (11.9) | 43 (20.3) | 31 (14.4) | 9 (21.4) | 22 (10.5) | 82 (18.8) | ||||
| 33–36 Moderate symptoms |
36 (5.6) | 9 (5.1) | 13 (6.1) | 10 (4.7) | 4 (9.5) | 10 (4.8) | 26 (6.0) | ||||
| >37 Severe symptoms |
150 (23.2) | 27 (15.3) | 69 (32.5) | 47 (21.9) | 7 (16.7) | 34 (22.7) | 116 (26.6) |
Risk factors on mental health outcomes
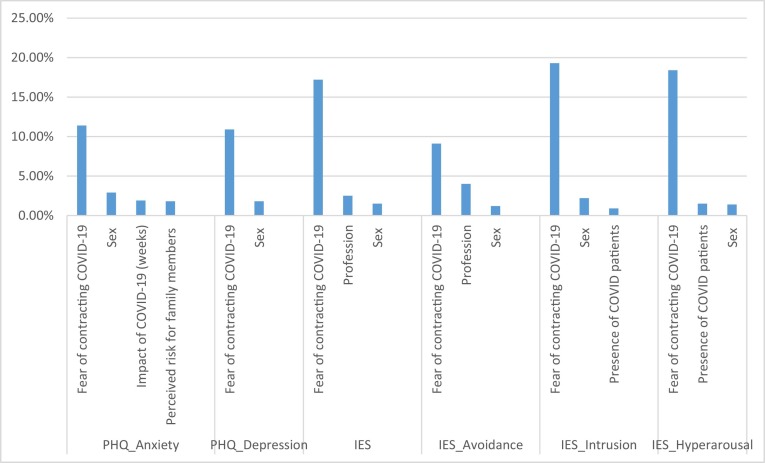
A series of multivariable regression analyses, including all the variables presented in Table 1 and Fig. 1 were conducted in order to predict which factors better explain the incidence of psychological disorders in the healthcare staff. In the tables only the variables of the stepwise selection model were reported (see Fig. 3 ).
Fig. 3.
Partial R square (%) indicating the sources of variability for the different psychological variables.
Anxiety and depression
The regression analysis showed that male health care professionals experienced significantly less severe anxiety symptoms than their female colleagues (β = −0.25; p < .0001). The number of weeks COVID-19 has been impacting on health care professionals work positively associated with anxiety symptoms (β = 0.20; p = .0012). Furthermore, also the fear of contracting COVID-19 increased the severity of anxiety symptoms (β = 0.01; p < .0001). Finally, healthcare professionals' anxiety symptoms positively associated with their perceived probability of being the source of contagion for those who lived with them (β = 0.004; 1; p = .0018) (see Table 3 ).
Table 3.
GLM for anxiety symptoms.
| GAD-2 | β | SE | t | Pr > |t| |
|---|---|---|---|---|
| Sex (man) | −0.25 | 0.06 | −4.05 | <0.0001 |
| How likely do you think the people who live with you will contract Covid-19? | 0.004 | 0.001 | 3.15 | 0.0018 |
| How many weeks has the Covid-19 emergency impacted on your daily workload? | 0.20 | 0.06 | 3.26 | 0.0012 |
| How much are you frightened by the possibility of contracting the Covid-19? | 0.01 | 0.00 | 7.99 | <0.0001 |
Similarly, men experienced significantly less severe depressive symptoms than their female colleagues (β = −0.45; p < .0001) and, in general, health care professionals depressive symptoms positively associated with the fear of contracting COVID-19 (β = 0.02; p = .0006) (see Table 4 ).
Table 4.
GLM for depressive symptoms.
| PHQ-2 | β | SE | t | Pr > |t| |
|---|---|---|---|---|
| Sex (man) | −0.45 | 0.13 | −3.45 | 0.0006 |
| How much are you frightened by the possibility of contracting the Covid-19? | 0.02 | 0.00 | 8.54 | <0.0001 |
Psychological distress
The regression analysis showed that male health care professionals seemed to have less suffered the pandemic impact than their female colleagues (β = −0.45; p = .0008). Furthermore, it seemed that nurses have suffered the impact of the pandemic more than both physicians (β = −0.66; p ≤ .0001) and other health professionals (β = −0.52; p = .0007) (see Table 5 ).
Table 5.
GLM for psychological distress. Job reference category Nurses.
| β | SE | t | Pr > |t| | |
|---|---|---|---|---|
| Sex (man) | −0.45 | 0.13 | −3.38 | 0.0008 |
| How much are you frightened by the possibility of contracting the Covid-19? | 0.03 | 0.00 | 11.47 | <0.0001 |
| Job (physicians) | −0.66 | 0.16 | −4.06 | <0.0001 |
| Job (other health care professionals) | −0.52 | 0.15 | −3.42 | 0.0007 |
| Job (technical and administrative staff) | −0.48 | 0.27 | −1.79 | 0.0738 |
Table 5a, Table 5b, Table 5c show results obtained from the IES-R subscales (Avoidance, Intrusion, Hyperarousal).
Table 5a.
GLM for subscales of psychological distress: Avoidance. Job reference category Nurses.
| β | SE | t | Pr > |t| | |
|---|---|---|---|---|
| Sex (man) | −0.09 | 0.03 | −2.84 | 0.0047 |
| How much are you frightened by the possibility of contracting the Covid-19? | 0.004 | 0.001 | 7.96 | <0.0001 |
| Job (physicians) | −0.209 | 0.04 | −5.14 | <0.0001 |
| Job (other health care professionals) | −0.133 | 0.04 | −3.53 | 0.0005 |
| Job (technical and administrative staff) | −0.128 | 0.067 | −1.92 | 0.0549 |
Table 5b.
GLM for subscales of psychological distress: Intrusion.
| β | SE | t | Pr > |t| | |
|---|---|---|---|---|
| Sex (man) | −0.136 | 0.03 | −4.12 | <0.0001 |
| How much are you frightened by the possibility of contracting the Covid-19? | 0.006 | 0.001 | 12.08 | <0.0001 |
| Directly attending COVID patients (no) | −0.084 | 0.03 | −2.65 | 0.0083 |
Table 5c.
GLM for subscales of Psychological Distress: Hyperarousal.
| β | SE | t | Pr > |t| | |
|---|---|---|---|---|
| Sex (man) | −0.114 | 0.03 | −3.27 | 0.0011 |
| How much are you frightened by the possibility of contracting the Covid-19? | 0.007 | 0.00 | 11.66 | <0.0001 |
| Directly attending COVID patients (no) | −0.112 | 0.03 | −3.35 | 0.0008 |
Discussion
The present multicentre cross-sectional study was conducted in Italy during the second month of the COVID-19 pandemic. Chronologically, Italy has been the second nation, after China, seriously affected by the COVID-19 emergency that has required rapid changes in the entire healthcare system and an extraordinary workload for all the healthcare professionals. The sudden and violent spread of the virus has also induced a serious emotional load mainly due to the fear of contagion and the high number of victims occurred in a very short time. In such a critical condition, we investigated the workers' perception about the Covid-19 related-risks, the magnitude of symptoms of anxiety, depression and distress emerged, and the potential risk factors associated with mental health symptoms.
Perceived risk and fear of infection for themselves and family members
Regarding the perceived risk of being infected, healthcare workers thought they were more at risk than their family members to contract the virus. This was expected, considering that they spent their working time in a hospital, while their relatives did not. Opposite results came from data about the fear of contagion, showing that they were more worried for their family members than for themselves. These results are in line with those reported by Dai et al. (n.d.) who found that, in the early stage of COVID-19 epidemic, healthcare workers were worried about getting infected (40%), but were even more worried about the risk to infect colleagues (72.5%) and family members (63.9%). It is possible that healthcare workers act a sort of defensive strategy that leads to shifting their own fears into the most intimate people, which thus be controlled and kept away through altruistic and protective behaviours (such as the protective measures taken at home – see below) that are known to be beneficial for people experiencing a psychological suffering (Kang et al., 2020).
Moreover, analysing the different categories of workers involved in the study, we noticed that, according to Dai et al. (n.d.), nurses perceived a higher risk of being infected compared to physicians and other healthcare workers, and were more worried about the possibility that their family members could be infected. This may be due by the fact that nurses work closer to the patients than physicians and other workers do, carrying out activities that often require repetitive and long-lasting contact with them. This, added to the fact that they received fewer swabs compared to physicians, objectively increases their probability of being infected and becoming potential carrier of the virus, maybe asymptomatic, causing transmission among relatives (Chew et al., 2020).
Despite these differences in risk perception and fear of contagion, we did not find any significant differences among workers regarding the anti-contagion precautions adopted at home which suggests a generalized will to protect their relatives in the way that was the most feasible for them.
Effects of COVID-19 on the hospital working routine
Most of responders perceived that their working routine was moderate or significantly modified by the COVID-19 spread, mainly because of the prolonged use of PPE, the increased working tension, the impossibility to carry out normal leisure activities after work and the increased working pressure.
The COVID-19 spread has dramatically affected the entire health care system, while the working life of healthcare professionals has been highly disrupted. This was mainly due to the introduction of new policies and processes that have significantly changed the normal routine, often generating rigid and mechanical procedures with consequent negative effects on working pressure and tension. At the same time, the high level of contagiousness of the virus and the consequent lockdown imposed by the Italian authorities have eliminated the possibility of promoting the work –life balance (Yester, 2019) spending free time with family and friends and practicing hobbies and leisure activities after work, inducing a severe deprivation of social support that is a relevant protective factor for mental health (Adriaenssens et al., 2015).
It is also interesting to notice that the prolonged use of PPE was considered the first element negatively impacting the responders' working activity since it causes an inevitable physical fatigue, due to the difficult of moving, the increase in body temperature and the limitation in the essential physical needs (and even pain, sometimes). Furthermore, PPE induce a severe mental stress related to the impossibility of getting rid of their “shell”, including feeling of oppression, constraint up to symptoms of claustrophobia and difficult relationships with colleagues.
COVID-19 and mental health outcomes
Overall, 29.6%, 22.8%, and 44.9% of all participants reported symptoms of moderate to severe anxiety, depression, and distress, respectively, indicating a significant incidence of psychological symptoms in the responders' sample (see Table 2). These data indicate a general higher burden of psychological symptoms in the Italian workers compared to those found by the first Chinese studies (Chew et al., 2020), but a similar incidence if compared with the later ones (Lai et al., 2020). This may explained by the fact that the more time passes from the beginning of pandemic to data collection, the higher is the incidence of distress symptoms that are known to worsen in the long-term. Moreover, according to our data and in line with the existing literature (Kisely et al., 2020; Lai et al., 2020; Wong et al., 2005), female sex and nursing profession appeared as relevant risk factors for developing more severe psychological symptoms. With regard to sex differences, it is well know that men are used to adopt coping strategies such as rationalization, which lead to a greater emotional distance from patients and therefore to a lower emotional distress, while women usually manifest high levels of personal, emotional and psychological involvement, that inevitably leads to a greater psychological burden (Meléndez et al., 2012). On the other hand, in relation to the professional category, mental suffering induces identifying mechanisms, especially on nurses who use to take care of patients for a longer time compared to other professionals, often without the adequate protections (Mok et al., 2005). Moreover, nurses are also often exposed to the patients' mental suffering, especially when relatives and caregivers are not allowed to do it due to the restrictions caused by the epidemic/pandemic spread.
Results from multivariate analyses show that other than sex and profession, the fear of being infected was the main source of psychological burden in our sample. This is certainly due to the responders' worries of contracting a dangerous illness, but maybe also to the fear of becoming a carrier of the virus, causing transmission among fellow healthcare workers and their own families (Kisely et al., 2020). Also results of two previous studies conducted during the current COVID-19 outbreak (Wang et al., 2020) and the previous Ebola crisis (Matua & Van Der Wal, 2015) found a sense of intense fear, stigmatization and ostracism when healthcare workers displayed physical symptoms suggestive of the virus infection, which often leads to negative psychological pain (Nezlek et al., 2012; Troyer et al., 2020). Moreover, we found that the duration of the COVID-19 impact, as perceived by workers, determined the level of anxiety, probably due to the prolonged exposure to the new stressful condition, while being a nurse specifically determined the level of distress and avoidance (intended as the attempt to escape thoughts or feelings related to the COVID-19 experience). Finally, we found that, regardless any other confounding variable, directly attending COVID patients had a significant impact on intrusive thoughts and hyperarousal related to the COVID-19 pandemic, maybe, once again, because of the fear of contagion and/or because of the daily workers' exposure to the dramatic effects of the COVID-19 spread.
In conclusion, our data represent a significant evidence of the impact of COVID-19 on the Italian healthcare workers' mental burden, and clearly show that hailing them as “heroes” is not sufficient to protect them from the negative psychological consequences that may be generated by a pandemic spread. In our opinion, these data should be urgently taken into consideration not only by mental health professionals, that are called to find effective approaches to support frontline workers, such as those recently suggested by WHO (WHO, 2020a), but also by Italian policy makers that are expected to set up new policies to protect them from unacceptable conditions such as shortages in critical protective equipment or inadequate economic treatments, especially in regard of those categories that appear to be at higher risk (i.e. females and nurses).
Acknowledgments
Acknowledgment
This work was supported in part by the “Ricerca Corrente” scheme of the Italian Ministry of Health, Italy.
Declaration of competing interest
None.
References
- Adriaenssens J., De Gucht V., Maes S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. International Journal of Nursing Studies. 2015 doi: 10.1016/j.ijnurstu.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C.S., Wu H.Y., Yang P., Yen CF. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatric Services. 2005;56(1):76–79. doi: 10.1176/appi.ps.56.1.76. PMID: 15637196. [DOI] [PubMed] [Google Scholar]
- Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H.…Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behaviour Research and Therapy. 2003 doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Dai, Y., Hu, G., Xiong, H., Qiu, H., & Yuan, X. (n.d.). Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. doi: 10.1101/2020.03.03.20030874. [DOI]
- Hassanian-Moghaddam H., Zamani N., Kolahi A.A. COVID-19 pandemic, healthcare providers’ contamination and death: An international view. Critical Care. 2020;24(1) doi: 10.1186/s13054-020-02938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., Yao L., Bai H., Cai Z., Xiang Yang B., Hu S., Zhang K., Wang G., Ma C., Liu Z. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ. 2020:369. doi: 10.1136/bmj.m1642. (Published 05 May 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001 doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics. 2009 doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N.…Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Miao J., Wang H., Xu S., Sun W., Fan Y.…Wang W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: A cross-sectional study. Journal of Neurology, Neurosurgery & Psychiatry. 2020;91:895–897. doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research. 2020 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K., Schneider A., Brähler E. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders. 2010 doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- Matua G.A., Van Der Wal D.M. Living under the constant threat of ebola: A phenomenological study of survivors and family caregivers during an ebola outbreak. Journal of Nursing Research. 2015 doi: 10.1097/jnr.0000000000000116. [DOI] [PubMed] [Google Scholar]
- Meléndez J.C., Mayordomo T., Sancho P., Tomás J.M. Coping strategies: Gender differences and development throughout life span. The Spanish Journal of Psychology. 2012 doi: 10.5209/rev_sjop.2012.v15.n3.39399. [DOI] [PubMed] [Google Scholar]
- Mok E., Chung B.P.M., Chung J.W.Y., Wong T.K.S. An exploratory study of nurses suffering from severe acute respiratory syndrome (sars) International Journal of Nursing Practice. 2005 doi: 10.1111/j.1440-172X.2005.00520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neto M.L.R., Almeida H.G., Esmeraldo J.D.a., Nobre C.B., Pinheiro W.R., de Oliveira C.R.T.…da Silva C.G.L. When health professionals look death in the eye: The mental health of professionals who deal daily with the 2019 coronavirus outbreak. In Psychiatry Research. 2020 doi: 10.1016/j.psychres.2020.112972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezlek J.B., Wesselmann E.D., Wheeler L., Williams K.D. Ostracism in everyday life. Group Dynamics. 2012 doi: 10.1037/a0028029. [DOI] [PubMed] [Google Scholar]
- Percudani M., Corradin M., Moreno M., Indelicato A., Vita A. Mental health services in Lombardy during COVID-19 outbreak. Psychiatry Research. 2020 doi: 10.1016/j.psychres.2020.112980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., Rossi A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Network Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006 doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Styra R., Hawryluck L., Robinson S., Kasapinovic S., Fones C., Gold WL. Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. Journal of Psychosomatic Research. 2008;64(2):177–183. doi: 10.1016/j.jpsychores.2007.07.015. PMID: 18222131; PMCID: PMC7094601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L.…Tam W. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D.S. Cross-cultural assessment of psychological trauma and PTSD. Springer; 2007. The impact of event scale: Revised; pp. 219–238. [Google Scholar]
- WHO A guide to preventing and addressing social stigma. 2020. https://www.who.int/docs/default-source/coronaviruse/covid19-stigma-guide.pdf
- WHO WHO Coronavirus disease (COVID-2019) situation report 117. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Wong T.W., Yau J.K.Y., Chan C.L.W., Kwong R.S.Y., Ho S.M.Y., Lau C.C.…Lit C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. European Journal of Emergency Medicine. 2005 doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X.…Hoven CW. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. PMID: 19497162; PMCID: PMC3780353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yester M. Work-life balance, burnout, and physician wellness. The Health Care Manager. 2019 doi: 10.1097/HCM.0000000000000277. [DOI] [PubMed] [Google Scholar]
- Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G.…Wang W. COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. MedRxiv. 2020 doi: 10.1101/2020.02.20.20025338. [DOI] [Google Scholar]