Abstract
Objective
Our aim was to identify patients with probable anti-NMDA receptor encephalitis among historical medical cases.
Method
A case report published in leading Hungarian-, German- and Italian-language medical journals in the early 1840s was revisited.
Results
In 1830, an 18-year-old, healthy woman suffered epileptic seizures, followed by a 6-day-long state characterized by catalepsy, unresponsiveness, motionless, and light breathing. Her symptoms regularly returned in the following 1.5 years. Meanwhile, a progressively growing huge abdominal tumor appeared. One day, she suddenly started vomiting a large amount of foul-smelling pus mixed with blood, accompanied by bone fragments. Pus mixed blood with some membranous substance was also evacuated through the anus and vagina. After this event, she completely recovered; 1.5 years later, she married and later gave birth to 3 healthy children. The patient remained healthy during the 11-year follow-up.
Conclusions
We suggest that in the description of a paraneoplastic case, an anti-NMDA receptor encephalitis can be dated back as far as to the 19th century, with an especially rare type of resolution: the disappearance of the symptoms after the spontaneous elimination of an ovarian teratoma.
Anti-NMDA receptor encephalitis was discovered by Dalmau et al.1,2 in 2005/2007, although cases were probably described already in 1997.3,4 Moreover, because of revisiting published cases dating back as far as the 19th century, more and more cases are suggested to be of anti-NMDA receptor encephalitis etiology. Merwick et al.5 pointed out that from the case series published by Bickerstaff—in which Bickerstaff encephalitis was described—in one patient, the symptoms were indicative of anti-NMDA receptor encephalitis. In the late 1800s, ovariotomy (Battey's operation) was introduced as a treatment of—among others—“histeroepilepsy.”6 In the course of the recent revisitation of these published cases, symptoms can also be attributed to anti-NMDA receptor encephalitis in more than one patient; this suggestion is also supported by the observation of Battey, namely that “cystic degeneration” was common in the resected ovaries.6 This is the most common autoimmune encephalitis, where 80% of patients are women with a median age of 21.7 Epileptic seizures occur in 76%,8 catatonia-like episodes in 70%,9 whereas hypoventilation in 66% of patients.8 In adult women patients, anti-NMDA receptor encephalitis is associated with ovarian teratoma in 58% of cases.7 Other tumors are rare: in paraneoplastic cases, 94% of the underlying tumor is ovarian teratoma.7
We found an interesting case report published in leading Hungarian-, German- and Italian-language medical journals referring to a presentation at the 3rd Meeting of the Italian Scientists in Florence held in 1841.10–12 We suggest that the description of an anti-NMDA receptor encephalitis can be dated back as far as to the 19th century.
Case
On September 17, 1841, the case was presented by Dr. Odoardo Linoli (figure).10–12 In 1830, an 18-year-old, hitherto healthy female patient suffered epileptic seizures, followed by a strange 6-day-long state characterized by a “catalepsy” pose and an unresponsive motionless state. The only sign of life was a very light breathing. Epileptic seizures and the catalepsy regularly returned in the following 1.5 years. Meanwhile, a progressively growing huge abdominal tumor appeared, which reached the level of the chest on the left side. One day, she suddenly started vomiting a large amount of coffee-colored liquid. Two weeks later, she vomited a foul-smelling pus mixed with blood. This was accompanied by more than 100 bone fragments. Some of these fragments were flat, others were long- or ball-shaped. Pus-mixed blood with some membranous substance was also evacuated through the anus and vagina. After this event, both epileptic seizures and “catalepsy” states disappeared, and she apparently became healthy again; 1.5 years later, she married and later gave birth to 3 healthy children. At the time of Dr. Linoli's presentation (11 years after the disease onset), she was in excellent health. During the discussion, Dr. Linoli argued that the abdominal tumor was probably a “fetal cyst” or “fetus in fetu.” Prof. Carlo Burci—the chairman of the section—suggested that the tumor could have been a “skin cyst,” whereas others speculated that it could have been an extrauterine pregnancy.
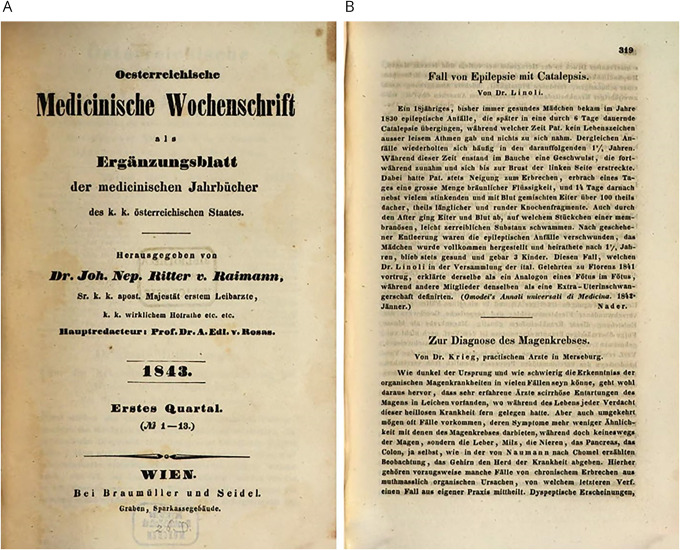
Figure. Case presentation.
The title page of the Österreichische Medizinische Wochenschrift from 1843 (A) and the case presentation in German (B). Available at the Bayerische Staatsbibliothek München, H.misc. 33 t-16, S. 244, urn:nbn:de:bvb:12-bsb10737557-2.
Discussion
The medical language in the first half of the 19th century was certainly different from today. The reliability of the description is enhanced by the fact that the case has been described in 3 different languages in the 1840s.10–12 The case was presented by Odoardo Linoli (1801–1886), a well-known surgeon from Pietrasanta,13 and discussed by Carlo Burci,14 who was the professor of surgery at the University of Pisa, indicating that the case was observed and discussed by the most prestigious professionals of that time.
We tried to interpret this case report according to today's medical concepts. Although catatonia was not described as such until 1874, the described motionless and unresponsive state accompanied by catalepsy meet the criteria of a catatonia.15 Another issue is the type of the described huge abdominal tumor that contained bone fragments.
According to Dr. Linoli's interpretation, it was a “fetus in fetu.” Fetus in fetu is extremely rare in adulthood16 and should contain vertebral axis or limbs, otherwise it should classify as teratoma.17 Dr. Burci suggested that the tumor was a “skin cyst.” According to today's nomenclature, dermoid cyst (i.e., skin-like cyst) is a synonym for teratoma. The presence of bone is not unusual in teratoma.18 Based on the presence of bone, a teratoma was diagnosed during a paleopathological examination of a female skeleton from the late Roman age.19
Ovarian teratomas without treatment can reach a huge size, some of them can be up to 30 cm in diameter.18 Not only the size, localization, and the presence of bone but also the strange elimination of the tumor through the gastrointestinal system and vagina may also support the concept of teratoma. Teratomas (dermoid cysts) can perforate into the adjacent organs including bowel and vagina.20–23 For example, Flood et al.22 reported a 23-year-old woman who discovered teeth-like structures in her underwear, which were the contents of an ovarian teratoma excreted in the vagina through a fistula. Mitui et al.23 reported a 72-year-old woman whose diarrhea, in which she found hair, was caused by an ovarian teratoma perforating into the bowels.
Summarizing our interpretation, a young woman had newly onset seizures, followed by catatonia-like symptoms and hypoventilation. This was associated with an abdominal tumor, which was probably a teratoma. The symptoms disappeared after the spontaneous elimination of the tumor, and the patient remained healthy during the 11-year follow-up.
According to a recent position study, new-onset seizures and altered mental status (unresponsive state) with subacute onset meet the criteria for “possible autoimmune encephalitis.”24 Epileptic seizures, altered mental status, abnormal posturing, and hypoventilation meet the symptoms criteria for “possible anti-NMDA receptor encephalitis.”24 The young age and female sex as well as the presence of ovarian teratoma also strengthen our assumption that Dr. Linoli's case study might be the first description of anti-NMDA receptor encephalitis.
In paraneoplastic anti-NMDA receptor encephalitis, the symptoms usually resolve after tumor removal, may that be either ovarian or extraovarian.7,25 Regarding Dr. Linoli's patient, the symptoms were present when the tumor was present and disappeared after the tumor also disappeared. Thus, we state that the description of a paraneoplastic story can be dated back as far as to 1830, ahead of the description of Trousseau's syndrome in 1865.26
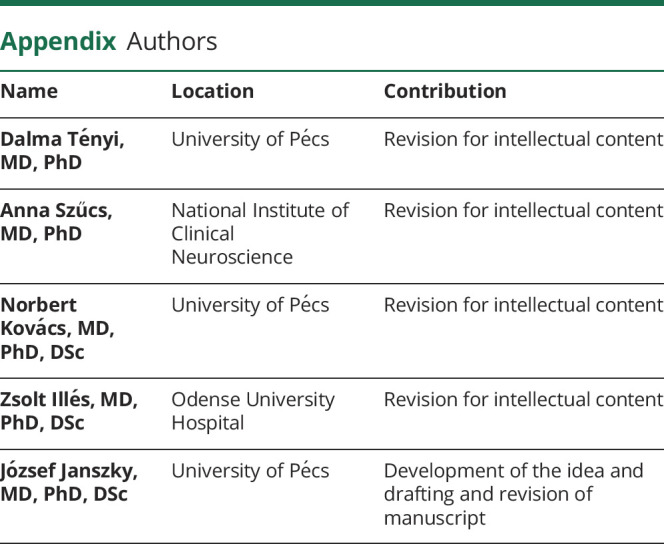
Appendix. Authors
Study funding
Study funded by the Hungarian Brain Research Program (2017-1.2.1-NKP-2017-00002), NKFIH EFOP-3.6.2-16-2017-00008 government-based funds. Our research was partly financed by the Higher Education Institutional Excellence Program of the Ministry of Human Capacities in Hungary, within the framework of the 5th thematic program of the University of Pécs, Hungary (20765/3/2018/FEKUSTRAT). The study was furthermore supported by the University of Pécs Medical School.
Disclosure
None of the authors report anything to disclose. Go to Neurology.org/NN for full disclosures.
References
- 1.Dalmau J, Tüzün E, Wu HY, et al. . Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 2007;61:25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vitaliani R, Mason W, Ances B, Zwerdling T, Jiang Z, Dalmau J. Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann Neurol 2005;58:594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nokura K, Yamamoto H, Okawara Y, Koga H, Osawa H, Sakai K. Reversible limbic encephalitis caused by ovarian teratoma. Acta Neurol Scand 1997;95:367–373. [DOI] [PubMed] [Google Scholar]
- 4.Okamura H, Oomori N, Uchitomi Y. An acutely confused 15-year-old girl. Lancet 1997;350:488. [DOI] [PubMed] [Google Scholar]
- 5.Merwick A, Dalmau J, Delanty N. Insights into antibody-associated encephalitis—Bickerstaff's 1950's papers revisited. J Neurol Sci 2013;334:167–168. [DOI] [PubMed] [Google Scholar]
- 6.Komagamine T, Kokubun N, Hirata K. Battey's operation as a treatment for hysteria: a review of a series of cases in the nineteenth century. Hist Psychiatry 2020;31:55–66. [DOI] [PubMed] [Google Scholar]
- 7.Titulaer MJ, McCracken L, Gabilondo I, et al. . Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 2013;12:157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dalmau J, Gleichman AJ, Hughes EG, et al. . Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008;7:1091–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Espinola-Nadurille M, Flores-Rivera J, Rivas-Alonso V, et al. . Catatonia in patients with anti-NMDA receptor encephalitis. Psychiatry Clin Neurosci 2019;73:574–580. [DOI] [PubMed] [Google Scholar]
- 10.Linoli O. Fall von Epilepsie mint Katalepsie [A case of epilepsy with catalepsy, German]. Österreichische Medizinische Wochenschrift 1843;12:319 Available at (free access): opacplus.bsb-muenchen.de/Vta2/bsb10086743/bsb:5976959?page=325. Accessed June 23, 2020. [Google Scholar]
- 11.Third Meeting of Italian Scientists in Florence. Annali Universali di Medicina 1842;40:17–20. Available at (free access): archive.org/details/s12id13209690/page/17. Accessed June 23, 2020. [Google Scholar]
- 12.Bugát P, Flór F. Kivonatok idegen lapokbul és munkákbul. Kór- és gyógytudomány. Nehézkor dermengéssel. [Extracts from foreign works. Pathology and medicine. Epilepsy with catalepsy, Hungarian] Orvosi Tár 1843;17:295 Available at (free access): library.hungaricana.hu/hu/view/ORSZ_ORVO_OT_1843_04/. Accessed June 23, 2020. [Google Scholar]
- 13.Wikipedia article. Available at: treccani.it/enciclopedia/odoardo-linoli_(Dizionario-Biografico)/. Accessed June 12, 2020.
- 14.Wikipedia article. Available at: it.wikipedia.org/wiki/Carlo_Burci. Accessed June 12, 2020.
- 15.Tandon R, Heckers S, Bustillo J, et al. . Catatonia in DSM-5. Schizophr Res 2013;150:26–30. [DOI] [PubMed] [Google Scholar]
- 16.Kumar A, Paswan SS, Kumar B, Kumar P. Fetus in fetu in an adult woman. BMJ Case Rep 2019;12:e230835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willis RA. The structure of teratoma. J Pathol Bacteriol 1935;40:1–36. [Google Scholar]
- 18.Caruso PA, Marsh MR, Minkowitz S, Karten G. An intense clinicopathologic study of 305 teratomas of the ovary. Cancer 1971;27:343–348. [DOI] [PubMed] [Google Scholar]
- 19.Armentano N, Subirana M, Isidro A, Escala O, Malgosa A. An ovarian teratoma of late Roman age. Int J Paleopathol 2012;2:236–239. [DOI] [PubMed] [Google Scholar]
- 20.von-Walter AR, Nelken RS. Benign cystic ovarian teratoma with a fistula into the small and large bowel. Obstet Gynecol 2012;119:434–436. [DOI] [PubMed] [Google Scholar]
- 21.Zarain García F. Teratoma quístico del ovario con absceso y fístula a vagina (Cystic teratoma of the ovary with abscess and fistula in the vagina [in Spanish]). Ginecol Obstet Mex 1974;36:49–53. [PubMed] [Google Scholar]
- 22.Flood K, Breathnach F, Gleeson N. An unusual presentation of a dermoid cyst. J Obstet Gynaecol 2010;30:72–73. [DOI] [PubMed] [Google Scholar]
- 23.Mitui AH, Fujita R, Sugata F, Kienebuchi M, Suzuki K, Sagawa F. A case of ovarian dermoid cyst with malignant transformation perforated into the rectosigmoid colon and small intestine. Endoscopy 1983;15:331–333. [DOI] [PubMed] [Google Scholar]
- 24.Graus F, Titulaer MJ, Balu R, et al. . A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 2016;15:391–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kümpfel T, Gerdes LA, Heck C, Prüss H. Delayed diagnosis of extraovarian teratoma in relapsing anti-NMDA receptor encephalitis. Neurol Neuroimmunol Neuroinflamm 2016;3:e250 doi: 10.1212/NXI.0000000000000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Darnell RB, Posner JB. Paraneoplastic Syndromes. Oxford/New York: Oxford University Press; 2011. [Google Scholar]