Abstract
Background
The COVID pandemic has challenged the traditional methods used in care of patients with heart failure (HF). Remote management of HF patients has been recommended in order to maintain routine standards of care, but satisfaction with this platform of care is unknown. We set out to address the physician and patient opinion of remote management of HF during COVID-19.
Methods and Results
An observational report of the use of a Structured Telephonic assessment (STA) in stable outpatient HF patients. Physician grading of the STA was complemented by 100 randomly chosen patients to ascertain patient satisfaction and comment. 278 patients underwent a STA. Patient preference for STA was noted in 66%. Convenience was the single most cited reason for this preference (83.3%). The STA was deemed satisfactory by clinicians in 67.6%. The two-leading reasons for clinician dissatisfaction were data gaps providing a barrier to titration (55.6%) and need for clinical exam (18.9%). The annual review appointment visit subtype possessed the highest levels of satisfaction congruence amongst both clinicians and patients.
Conclusion
In summary, this report demonstrates reasonable patient / physician satisfaction with STA, and provides some direction on how this care platform might be sustained beyond the COVID crisis.
Keywords: Heart failure, Telemedicine, COVID-19, Remote patient monitoring
Abbreviations: ARA, Annual review appointment; BP, Blood pressure; DMP, Disease management programme; F2F, Face to Face; GP, General practitioner; HFrEF, Heart failure with reduced ejection fraction; HR, Heart Rate; HRPA, High risk patient appointment; HF, Heart Failure; STA, Structured telephone assessment; VC, Virtual consult; YRS, Years
1. Introduction
Disease management programmes (DMP) are the established platform for delivering community heart failure (HF) care. A significant component of work is patient facing(F2F), involving physician assessment or nurse-delivered education and medication titration. However, telephonic patient contact, remote metric monitoring and the emerging use of virtual consultation (VC) with family practitioners (GPs) represent a growing body of remote patient management [1], [2].
The ongoing COVID pandemic has compromised the delivery of care within DMPs, especially that involving direct patient contact(F2F). Recommendations from bodies such as the European Society of Cardiology [3] and the British HF Association [4] have advised restricting F2F contact, and to provide as much care as possible remotely. Additional commentary has mentioned the opportunity to use this period to address whether applied eHealth strategies used during this time may be of long-term benefit [5]. We set out to address the impact of the COVID-19 pandemic on the functioning of a HF DMP, assessing physician and patient perspectives’ of the switch to predominantly remote care, and using this experience to analyze whether any aspect of the F2F work of a HF unit could successfully be transferred to remote care beyond the Covid-19 crisis.
2. Method
This is a prospective observational report. Our DMP assesses over 100 patients per week through F2F consultation. This service is provided for clinical follow-up post HF discharge, medical review of higher risk patients (HRPA), new patient referrals, annual review appointment (ARA) of patients to update/optimize HF strategy, and regular nurse-led drug titration and self-care education clinics. In addition, we provide 3 VCs per week to consult with GPs on specific HF questions.
With the emergence of the COVID-19 pandemic, and in adherence to local and international advice, we restricted F2F care to post-discharge patients and patients in whom there was concern of clinical deterioration. New patient community referrals were managed by our VC clinic where feasible, and deferred if not appropriate. All other patients due their ARA, HRPA and titration visits were assessed by a structured telephonic assessment (STA). Patients were informed 2 days prior to their originally planned appointment of the change to STA. This allowed patients or family members to prepare questions they would like to raise and to facilitate a family member be present if desired. Patients were requested to have weight books and current medication lists available. All STAs were undertaken by a senior HF fellow and specialist nurse. A staff cardiologist was available to provide opinion where needed.
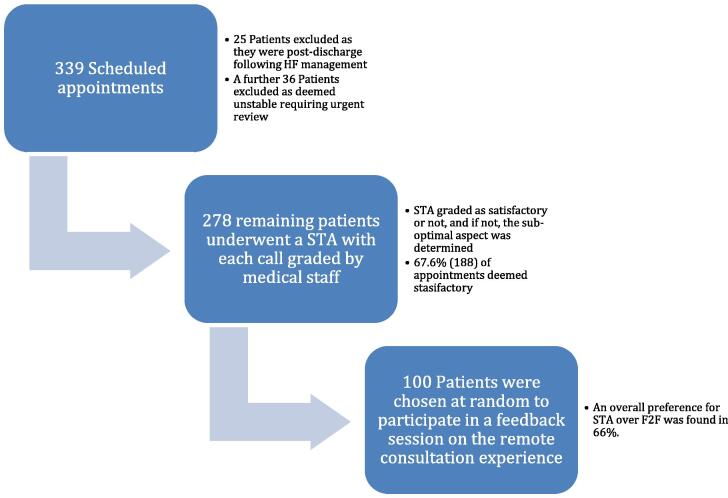
The consultation assessed wellbeing, adherence to self-care underlined, addressed patient concerns and arranged next follow up. Overview of the remote assessment, STA grading and feedback process are outlined in Fig. 1.
Fig. 1.
Overview of Remote assessment and feedback process. After each call medical staff assessed whether the STA was satisfactory or not, and if not, the sub-optimal aspect was determined (Supplement A.).All patients were advised that they could be contacted within 48 h to participate in a feedback session on the remote consultation experience (Supplement B.). 100 patients were chosen at random for this analysis. Abbreviations: HF = Heart Failure; STA = Structured Telephonic assessment.
3. Results
3.1. Baseline Characteristics (Table 1)
Table 1.
Baseline Characteristics.
| Characteristic | Overall N = 278 |
F2F preference N = 34 |
STA preference N = 66 |
|---|---|---|---|
| Mean Age, yrs | 72.8 | 72 | 74.5 |
| Male, n (%) | 159(57.2) | 19(32.4) | 38(57.6) |
| HFrEF, n (%) | 185(66.5) | 20(58.4) | 44(66.7) |
| Ischemic etiology, n (%) | 91(49.2) | 12(60) | 22(50) |
| Comorbidities = 1, n (%) | 38(13.7) | 2(5.8) | 8(12.1) |
| Comorbidities = 2, n (%) | 76(27.3) | 11(32.4) | 16(24.3) |
| Comorbidities = 3, n (%) | 68(24.5) | 11(32.4) | 14(21.2) |
| Comorbidities > 3, n (%) | 96(34.5) | 10(29.4) | 28(42.4) |
| Annual review appointments, n(%) | 107(38.5) | 12(35.3) | 34(51.5) |
| High risk patient appointments (HRPA), n (%) | 127(45.7) | 18(52.9) | 26(39.4) |
| Titration clinic, n (%) | 44(15.8) | 4(11.8) | 6(9.1) |
Abbreviations: F2F = face to face; STA = structured telephone assessment; HFrEF = Heart failure with reduced ejection fraction; HRPA = High risk patient appointments; yrs = years.
A total of 339 patients had scheduled appointments over a 3-week period from March to April 2020. Following exclusion of 61 patients (Fig. 1), the 278 (male 159; 57.2%) remaining appointments were changed to a STA. HF with reduced ejection fraction was the prevalent phenotype, with HRPAs the predominant clinic sub-type. The majority of patients had ≥ 3 comorbidities (Table 1).
3.2. The patient perspective
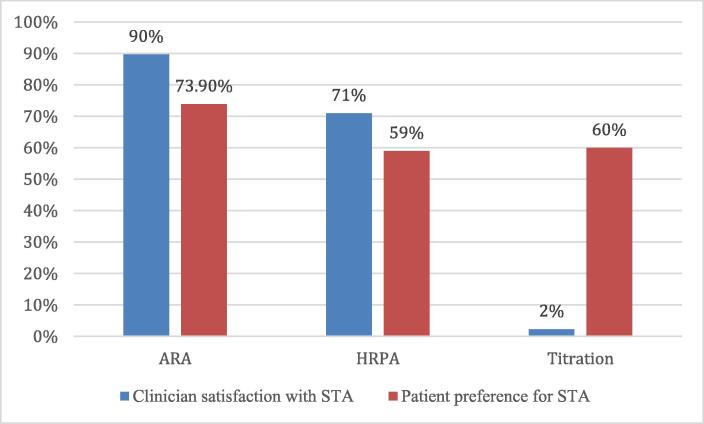
An overall preference for STA over F2F was found in 66%. A similar trend was noted across all consultation subtypes (Fig. 2.). Convenience was the dominant reason for this preference in 83.3% (55/66). Of those who preferred F2F consultations, the primary reasons cited were missing staff/clinician interactions (76.5%, 26/34) and/or omission of physical exam (17.6%, 6/34). Overall, combining both groups, 60% and 42% of patients reported missing staff interactions and the physical exam, respectively. All participants who felt the STA had a negative impact on care preferred F2F consultations.
Fig. 2.
Clinician and patient satisfaction vs clinic sub type. Abbreviations: ARA = annual review appointment; HRPA = High risk patient appointments; STA = Structured Telephonic assessment.
A hearing impairment was reported in 29%, while 10% self-reported a cognitive impairment. Despite these impediments, only 10% were associated as having a negative impact on the STA result, while only 8% of patients had a family member/ carer present. 28% missed having a family member/ carer involved in the STA. 77% of participants felt in a position to have a family/carer involved in the future. Going forward, 53% of patients felt the STA should be best utilized when they are unwell. Meanwhile, 32% of patients felt the STA should only be used when they are well.
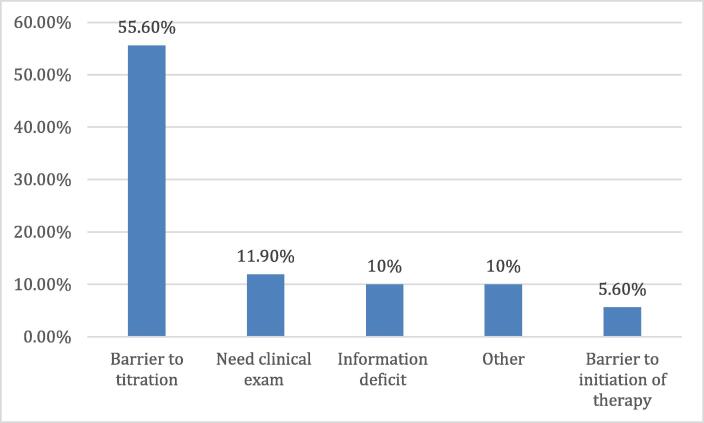
3.3. The clinician perspective
The STA was deemed satisfactory in 67.6% (1 8 8) of appointments. 89.7% (96) of ARA appointments, 71.7% (91) of HRPAs and 2.3% (1) of titration appointments were considered satisfactory by the clinician. The leading reason for clinician dissatisfaction was lack of data resulting in a “barrier to titration” in 55.6%(50) with the other reasons outlined in Fig. 3. Of the STAs where a carer/family member was present, 87.5% were deemed satisfactory by the clinician, improving information deficit dominantly. The best congruence between physician and patient satisfaction was in the ARA cohort, where 56.5% of interactions were satisfactory to both. In total, 2.9% of patients required a F2F visit following their STAs, dominantly because of need for clinical exam.
Fig. 3.
Reasons for Clinicians dissatisfaction.
4. Discussion
The outpatient HF DMP has been the main platform to deliver community HF care [6]. The dominantly F2F service has been significantly disrupted by the COVID-19 pandemic, potentially putting this vulnerable cohort at heightened risk.
Remote care has been increasingly used in community HF management, however the COVID-19 pandemic has challenged established F2F outpatient systems to urgently transfer a large volume of care to a remote platform [3], [4]. The medical suitability and patient acceptance of a wider application of remote care in HF is uncertain [7], [8], but the demands of the present health care environment have necessitated this be tested, potentially providing insight into how we might expand remote care beyond the COVID-19 pandemic
Findings from our observational analysis answer some of these questions. Patient satisfaction was high, driven mainly by convenience. One third of the patient cohort preferred F2F, reflecting reassurance of direct contact and physical examination. Physician assessment was also encouraging, with two-thirds of consultations deemed satisfactory. As anticipated, visits directed at drug titration posed a problem. Interestingly, the lack of physical examination was a meaningful drawback in a minority. Of note, the patient view that the STA would be best deployed for patients feeling unwell is at odds with the physician view. Conventional wisdom would suggest this is the setting where physical examination with additional testing is most required.
These data do provide some insight into how we might expand and improve the role of eHealth for HF services. The ARA visit is an important opportunity to revise self-care and update the treatment plan based on evolution of new therapies and/or alteration in patient metrics (e.g. renal function) in the preceding year. There was an acceptable alignment between patient and physician satisfaction with the STA. This may be a group where remote contact with available updated laboratory studies may be a viable alternative in certain cases to a clinic visit. Patients providing reliable home measures of HR, BP and updated renal function might facilitate remote up-titration in certain cases. Combined, these two visit types represent a significant component of the unit workload and safely transferring some of these appointments to a remote service may have advantages for patients and service capacity [9], [10], [11]. If we had added visual contact to the STA, this may have provided reassurance to the patients/family who miss the F2F element. The visual component may also provide the physician with some additional evidence of patient status [2], [12], [13]. Finally, despite invitation for family involvement only 7% took up this option, yet stated this could be achieved in the majority of future STAs. This may improve both patient and physician satisfaction with the interaction.
It should be noted that this study does not report on the impact of this change on clinical events. Going forward, with any systematic change, follow-up of events needs to be central to ensure quality of care is either unaltered or improved, and is already in development in our unit. In addition, the answers provided in this report may have been altered by the impact of the ongoing COVID-19 crisis. However, metanalysis and systemic reviews have demonstrated that compared to usual care, STA and telemonitoring significantly reduced death and hospitalization due to heart failure [14], [15], [16]. In the data that has evaluated the cost effectiveness of HF management, significant economic viability of telehealth care programmes have been demonstrated, with savings estimated at between $5000 and >$50,000 per year per patient, according to the HF stage and study setting [17], [18], [19]. Due to the heterogenous nature of both the trials and the analysis, further research is required to quantify the cost effectiveness of the sub-types of telemedicine to establish the most cost-effective.
5. Conclusion
In summary, this single unit observational report reviews the impact of the COVID-19 pandemic on routine community HF care provided through a DMP. It underlines that changing to a dominantly remote platform, while not ideal for all interactions, did have a high acceptance rate for patient and medical staff. The lessons from this experience may help evolve the use of eHealth strategies in HF care in the future.
Funding
No funding received
Originality statement
All material enclosed in this prospective observational report titled “Changing to remote management of a community heart failure population during COVID-19 – Clinician and Patient perspectives” is original to this submission.
Author contributions
BK, JG, MB and KM conceptualized, drafted and wrote the final manuscript. CH, ML and RP reviewed and edited the final draft while BK and RP were involved in data curation. BK performed the statistical analysis.
All authors have approved the final article.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ponikowski P., Voors A.A., Anker S.D., Bueno H., Cleland J.G.F., Coats A.J.S. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. [Internet]. 2016 Jul 14;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 2.Gallagher J., James S., Keane C., Fitzgerald A., Travers B., Quigley E. Heart Failure Virtual Consultation: bridging the gap of heart failure care in the community - A mixed-methods evaluation. ESC Hear Fail [Internet]. 2017 Aug;4(3):252–258. doi: 10.1002/ehf2.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.European Society of Cardiology. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic [Internet]. 2020 [cited 2020 May 24]. p. 1–119. Available from: https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance#p06.
- 4.Brisitsh Society For Heart Failure. Retention of Essential Heart Failure Services during COVID-19 Pandemic A Position Statement from the British Society for Heart Failure [Internet]. 2020 [cited 2020 May 24]. Available from: https://www.bsh.org.uk/resources/.
- 5.Cowie MR. COVID-19 digital health swings into action [Internet]. [cited 2020 May 24]. Available from: https://www.escardio.org/Education/COVID-19-and-Cardiology/covid-19-digital-health-swings-into-action.
- 6.McDonagh T.A., Blue L., Clark A.L., Dahlström U., Ekman I., Lainscak M. European Society of Cardiology Heart Failure Association Standards for delivering heart failure care. Eur. J. Heart Fail [Internet]. 2011 Mar;13(3):235–241. doi: 10.1093/eurjhf/hfq221. [DOI] [PubMed] [Google Scholar]
- 7.Seuren LM, Wherton J, Greenhalgh T, Cameron D, A’Court C, Shaw SE. Physical Examinations via Video for Patients With Heart Failure: Qualitative Study Using Conversation Analysis. J Med Internet Res [Internet]. 2020 Feb 20;22(2):e16694. Available from: https://www.jmir.org/2020/2/e16694 [DOI] [PMC free article] [PubMed]
- 8.Wherton J, Shaw S, Papoutsi C, Seuren L, Greenhalgh T. Guidance on the introduction and use of video consultations during COVID-19: important lessons from qualitative research. BMJ Lead [Internet]. 2020 May 18;leader-2020-000262. Available from: http://bmjleader.bmj.com/lookup/doi/10.1136/leader-2020-000262
- 9.Akobeng AK, O’Leary N, Vail A, Brown N, Widiatmoko D, Fagbemi A, et al. Telephone Consultation as a Substitute for Routine Out-patient Face-to-face Consultation for Children With Inflammatory Bowel Disease: Randomised Controlled Trial and Economic Evaluation. EBioMedicine [Internet]. 2015 Sep;2(9):1251–6. Available from: http://dx.doi.org/10.1016/j.ebiom.2015.08.011 [DOI] [PMC free article] [PubMed]
- 10.Gorodeski EZ, Moennich LA, Riaz H, Tang WHW. Virtual Visits Versus In-Person Visits and Appointment No-Show Rates. J Card Fail [Internet]. 2019 Nov;25(11):939. Available from: https://doi.org/10.1016/j.cardfail.2019.11.008
- 11.Ruiz-Pérez I, Bastos Á, Serrano-Ripoll MJ, Ricci-Cabello I. Effectiveness of interventions to improve cardiovascular healthcare in rural areas: a systematic literature review of clinical trials. Prev Med (Baltim) [Internet]. 2019 Feb;119(December 2018):132–44. Available from: https://doi.org/10.1016/j.ypmed.2018.12.012 [DOI] [PubMed]
- 12.Abnousi F, Kang G, Giacomini J, Yeung A, Zarafshar S, Vesom N, et al. A novel noninvasive method for remote heart failure monitoring: the EuleriAn video Magnification apPLications In heart Failure studY (AMPLIFY). npj Digit Med [Internet]. 2019 Dec 21;2(1):80. Available from: http://dx.doi.org/10.1038/s41746-019-0159-0 [DOI] [PMC free article] [PubMed]
- 13.Thibodeau J.T., Drazner M.H. The Role of the Clinical Examination in Patients With Heart Failure. JACC Hear Fail [Internet]. 2018 Jul;6(7):543–551. doi: 10.1016/j.jchf.2018.04.005. https://linkinghub.elsevier.com/retrieve/pii/S221317791830283X [DOI] [PubMed] [Google Scholar]
- 14.Kotb A, Cameron C, Hsieh S, Wells G. Comparative Effectiveness of Different Forms of Telemedicine for Individuals with Heart Failure (HF): A Systematic Review and Network Meta-Analysis. Wu W-CH, editor. PLoS One [Internet]. 2015 Feb 25;10(2):e0118681. Available from: https://dx.plos.org/10.1371/journal.pone.0118681 [DOI] [PMC free article] [PubMed]
- 15.Inglis S.C., Clark R.A., Dierckx R., Prieto-Merino D., Cleland J.G.F. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Heart [Internet] 2017 Feb 15;103(4):255–257. doi: 10.1136/heartjnl-2015-309191. [DOI] [PubMed] [Google Scholar]
- 16.Kruse CS, Soma M, Pulluri D, Nemali NT, Brooks M. The effectiveness of telemedicine in the management of chronic heart disease – a systematic review. JRSM Open [Internet]. 2017 Mar;8(3):205427041668174. Available from: http://journals.sagepub.com/doi/10.1177/2054270416681747 [DOI] [PMC free article] [PubMed]
- 17.Vestergaard A.S., Hansen L., Sørensen S.S., Jensen M.B., Ehlers L.H. Is telehealthcare for heart failure patients cost-effective? An economic evaluation alongside the Danish TeleCare North heart failure trial. BMJ Open [Internet]. 2020;10(1):e031670. doi: 10.1136/bmjopen-2019-031670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu S.X., Xiang R., Lagor C., Liu N., Sullivan K. Economic Modeling of Heart Failure Telehealth Programs: When Do They Become Cost Saving? Int. J. Telemed. Appl. [Internet]. 2016:1–9. doi: 10.1155/2016/3289628. http://www.hindawi.com/journals/ijta/2016/3289628/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiménez-Marrero S., Yun S., Cainzos-Achirica M., Enjuanes C., Garay A., Farre N. Impact of telemedicine on the clinical outcomes and healthcare costs of patients with chronic heart failure and mid-range or preserved ejection fraction managed in a multidisciplinary chronic heart failure programme: A sub-analysis of the iCOR randomized. J. Telemed. Telecare [Internet]. 2020 Jan 7;26(1–2):64–72. doi: 10.1177/1357633X18796439. http://journals.sagepub.com/doi/10.1177/1357633X18796439 [DOI] [PubMed] [Google Scholar]